Abstract
Aims
To assess if low occupational class was an independent predictor of Type 2 diabetes in men in Sweden over a 35-year follow-up, after adjustment for both conventional risk factors and psychological stress.
Methods
A random population-based sample of 6874 men aged 47–56 years without a history of diabetes was divided into five occupational classes and the men were followed from 1970 to 2008. Diabetes cases were identified through the Swedish inpatient and death registers. Subdistribution hazard ratios (SHRs) and 95% CIs from competing risk regressions, cumulative incidence and conditional probabilities were calculated, after accounting for the risk of death attributed to other causes.
Results
A total of 907 (13%) men with diabetes were identified over 35 years with a median follow-up of 27.9 years. The cumulative incidence of diabetes, when taking into account death as a competing event, was 11% in high officials, 12% in intermediate non-manual employees, 14% in assistant non-manual employees, 14% in skilled workers, and 16% in unskilled and semi-skilled workers. Men with unskilled and semi-skilled manual occupations had a significantly higher risk of diabetes than high officials (reference) after adjustment for age, BMI, hypertension, smoking and physical activity (SHR 1.39, 95% CI 1.08–1.78). Additional adjustment for self-reported psychological stress did not attenuate the results.
Conclusions
A low occupational class suggests a greater risk of Type 2 diabetes, independently of conventional risk factors and psychological stress.
Introduction
The rapid rise of diabetes worldwide poses one of the major public health challenges of the 21st century [1]. In the Western world Type 2 diabetes disproportionately affects people with lower socio-economic status (SES) [2–8]. The traditional risk factors of diabetes, such as obesity, low physical activity, unhealthy diet and smoking, are often more prevalent in lower SES groups, particularly in high-income countries, and these risk factors explain some of the observed SES inequalities in people with diabetes [4,5,7,9]. Psychological stress is also known to increase the risk of diabetes [10,11], for which possible mechanisms are alterations of the hypothalamic–pituitary–adrenal axis activity leading to abdominal obesity [12], or which could be mediated through unhealthy behaviours. Psychological stressors have been shown to be reported more frequently in lower SES groups [9], but most of the studies on the relationship between SES and diabetes are not adjusted for psychological stress [3]. Furthermore, the few studies that have been conducted on SES and the risk of diabetes in Swedish populations are limited because they were either cross-sectional [9], were in women only [13], adjusted for only a limited number of conventional risk factors, or had short follow-up periods [14]. Knowledge of existing inequalities in the risk of diabetes is important for directing preventive actions and screening more effectively. The present study aimed to assess if SES defined by occupation was an independent predictor of Type 2 diabetes in men over a 35-year follow-up period, while taking psychological stress into account, as well as other known conventional risk factors for diabetes.
What's new?
Studies with a follow-up of 15 years have shown that Type 2 diabetes disproportionately affects people with a lower socio-economic status.
With the world's aging population, it is important to determine if risk factors persist into older age groups.
In contrast to many other studies, we adjusted the analysis, not only for conventional risk factors, but also for psychological stress and competing risk of death.
The present study shows that low occupational class at mid-life remains an independent predictor for Type 2 diabetes after a 35-year follow-up.
Subjects and methods
Study population
The multifactor Primary Prevention Study was a population-based cohort study of middle-aged men, established in 1970 in Gothenburg [15]. All men in Gothenburg born in the period 1915–1925 (except for men born in 1923, who took part in another study) were randomly divided into one of three equally large groups consisting of ∼10 000 men each. Two of the groups were control groups and one group was the intervention group. The present study is based on data from the intervention group. Participants in the intervention group were offered a medical examination to identify and treat risk factors. The intervention criteria in the study were antihypertensive treatment if systolic blood pressure was > 175 mm Hg or if diastolic blood pressure was >115 mm Hg, dietary advice if serum cholesterol levels were > 260 mg per 100 ml (=6.8 mmol/1), and referral to anti-smoking clinics for participants who smoked ≥15 cigarettes per day. Treatment was offered at specialist clinics. At the follow-up after 12 years, there was no difference in cardiovascular disease outcome or all-cause mortality between the intervention and two control groups [15]; therefore, despite the fact that the men took part in an intervention study, the study cohort may be regarded as representative of the general middle-aged male population of Gothenburg during this period. All participants gave their informed consent to participate in the study. The study was approved by the Ethics Committee for Medical Research at the University of Gothenburg, and complied with the Helsinki Declaration principles.
Of the 10 004 men randomized to the intervention group, 7494 of the men (75% of the sample) participated in the baseline screening examination and completed a postal questionnaire before this. Two of the questions in the questionnaire were: ‘Has a physician ever told you that you have had diabetes?’ and ‘Have you ever had myocardial infarction/bleeding of the brain/thrombosis of the brain?’. According to this self-report, 238 men had a history of diabetes, myocardial infarction or stroke at baseline, and were excluded from the study. Another 382 of the 7256 men could not be classified according to the Swedish socio-economic classification system, the Socio-Economic Index (described below), resulting in a final total of 6874 men included in the present study. The main reason for not having an Socio-Economic Index classification was early retirement.
Occupational class
The participants were classified into the following five occupational classes and coded according to the Swedish socio-economic classification system [16]: (1) unskilled and semi-skilled workers; (2) skilled workers; (3) foremen in industrial production and assistant non-manual employees; (4) intermediate non-manual employees; and (5) employed and self-employed professionals, higher civil servants and executives.
Other covariates
Information on smoking habits, physical activity, antihypertensive treatment and self-perceived psychological stress was collected from the postal questionnaire. Smoking status was defined as non-smoker, former smoker of > 1 month's duration and current smoker. Physical activity during leisure time was divided into sedentary, moderate and regular exercise. Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, or receiving antihypertensive medication. Self-perceived psychological stress was assessed by a single question in the questionnaire defining stress as feeling tense, irritable, filled with anxiety or having sleeping difficulties as a result of conditions at work or at home. The alternative responses were on a six-point scale as follows: 1: never experienced stress; 2: some period of stress ever; 3: some period of stress in the past 5 years; 4: several periods of stress in the past 5 years; 5: permanent stress in the past year; and 6: permanent stress over the past 5 years. The six-point scale was then merged into three categories: no or little stress (scale point 1–2); periodic stress (scale points 3–4); and permanent stress (scale points 5–6) [17]. The stress question was first developed and used in the present study and has later been used in large international studies (e.g. the INTERHEART [18] and INTERSTROKE studies [19]).
At the baseline screening examination, weight was measured to the nearest 0.1 kg and height to the nearest 0.01 m. BMI (weight in kg divided by measured height in m2) was categorized as <25 (normal), 25–30 (overweight) and >30 kg/m2 (obese). Blood pressure was measured using a mercury manometer, with the subject seated after 4–5 min rest, and was measured to the nearest 2 mmHg.
The proportion of missing data was 5.7% (n =393) for the psychological stress variable and ≤1.1% for all the other covariates.
Diagnosis of diabetes
By using their unique personal identification numbers, the men were followed from the date of their baseline examination until 31 December 2008, or until death. The Swedish national register on cause of death and the Swedish hospital discharge register were used to identify men diagnosed with diabetes during follow-up. The hospital discharge register has operated on a nationwide basis since 1987, but all discharges from Gothenburg hospitals have been entered in the national register since 1970 (except in 1976 owing to a legislative change for that year). The International Classification of Disease (ICD) codes listed on the registries were used to identify diabetes cases during the follow-up period, either as a principal or as a secondary diagnosis. ICD-8 was in use from 1968 to 1986, ICD-9 from 1987 to 1996, and ICD-10 from 1997 until the present. In the present study, the following ICD codes were used to identify diagnosis of diabetes: 250 (ICD-8), 250 (ICD-9), or E10–E14 (ICD-10). ICD-8 and ICD-9 do not differentiate between Type 1 and Type 2 diabetes. This procedure was reviewed and approved by our institutional Ethics Committee.
Statistical analysis
The descriptive statistics at baseline are presented as frequencies and percentages for categorical variables, or mean value with standard deviation (sd) for continuous variables. Trends in distribution of baseline characteristics along the occupational classes were analysed using the Cochran–Armitage trend test for categorical variables and the anova linear trend test for continuous variables. All P values were two-sided and values <0.05 were considered to indicate statistical significance. For each occupational class, as well as for the whole study population, we calculated the age-adjusted diabetes incidence rates per 100 000 person-years. Time at risk was calculated from the baseline examination between January 1970 and March 1973 to the first hospitalization with a diagnosis of diabetes (as a principal or secondary diagnosis), to death or to 31 December 2008. We used competing risk regression [20] to model the risk for diabetes, with death as a competing event in association with occupational class, controlling for potential confounders. Subdistribution hazard ratios (SHRs) and associated 95% CIs for diabetes were estimated for this procedure. The highest occupational class (high officials) was used as a reference. To account for the non-proportionality of hazard ratios [21], these were time-averaged properly according to Schemper et al. [22]. The first regression model was adjusted for age only. The final model was adjusted for age, BMI, hypertension, smoking, physical activity and psychological stress. A dummy variable was constructed for the men with missing data on stress (5.7%, n=395) and entered into the model. Curves displaying the cumulative incidence of diabetes and death across occupational classes, as well as curves displaying the conditional probability [23] of diabetes in different occupational classes are shown (estimated as conditional probability = cumulative incidence of diabetes/1-cumulative incidence of death). All statistical analyses were performed using sas software version 9.3 (SAS institute, Cary, NC, USA) and Statistical package R version 3.00.
Results
The mean age of the men at baseline was 51.6 ± 2.3 years. During a 35-year follow-up (median follow-up, 27.9 years), 907 (13%) of the 6874 men were diagnosed with diabetes according to the Swedish hospital discharge register (874 cases) or the Swedish national register of cause of death (33 cases). The crude incidence of diagnosed diabetes was 506 cases per 100 000 person-years.
Baseline characteristics by different occupational classes are shown in Table 1. The classic risk factors for diabetes were more pronounced in the lower occupational classes as expected. The men in these occupational classes had a significantly higher BMI, were more obese, had a higher blood pressure and rate of smoking, and a more sedentary lifestyle than those in the higher occupational classes. The men in the lower occupational classes also reported more permanent stress than those in the higher occupational classes.
Table 1.
Baseline characteristics according to occupational class
| Characteristics | All, N = 6874 | High officials, professionals, n = 793 | Intermediate, non-manual employees, n = 1231 | Assistant non-manual employees, n = 1348 | Skilled workers, n = 1871 | Unskilled and semiskilled workers, n = 1631 | P* |
|---|---|---|---|---|---|---|---|
| Mean (sd) age, years, | 51.6 (2.3) | 51.6 (2.3) | 51.5 (2.3) | 51.5 (2.2) | 51.7 (2.2) | 51.5 (2.3) | 0.40 |
| Mean (sd) BMI, kg/m² | 25.5 (3.2) | 25.3 (3.0) | 25.4 (3.1) | 25.4 (3.1) | 25.6 (3.1) | 25.7 (3.4) | 0.01 |
| Obesity: BMI ≥30 kg/m², % (n) | 7.7 (532) | 6.7 (53) | 6.9 (85) | 7.3 (99) | 7.8 (146) | 9.1 (149) | 0.012 |
| Mean (sd) height, cm | 175.7 (6.3) | 178.0 (6.1) | 176.7 (6.2) | 175.9 (6.3) | 174.5 (6.1) | 174.8 (6.4) | <0.001 |
| Mean (sd) systolic blood pressure, mmHg | 149 (22) | 145 (21) | 148 (21) | 149 (22) | 150 (22) | 148 (22) | <0.001 |
| Mean (sd) diastolic blood pressure, mmHg | 95 (13) | 93 (13) | 94 (13) | 95 (13) | 95 (13) | 94 (13) | 0.022 |
| Hypertension, % (n) | 70.0 (4802) | 63.1 (500) | 69.4 (854) | 72.5 (976) | 71.7 (1340) | 69.7 (1132) | 0.006 |
| Current smokers, % (n) | 50.1 (3444) | 47.2 (374) | 45.9 (565) | 49.8 (671) | 51.1 (957) | 53.8 (877) | <0.001 |
| Sedentary, % (n) | 25.3 (1716) | 20.1 (159) | 18.4 (226) | 22.8 (308) | 28.4 (532) | 30.1 (491) | <0.001 |
| Permanent stress†, % (n) | 14.9 (966) | 13.9 (110) | 11.5 (141) | 13.9 (187) | 15.0 (281) | 15.1 (247) | 0.020 |
P value for trends in distribution of baseline characteristics.
Self-perceived psychological stress category 3 = permanent stress.
Table 2 shows the SHRs from the competing risk regression models. There was a tendency of a higher risk of diabetes in the lower occupational classes. The lowest occupational class (unskilled and semiskilled workers) had a significantly greater risk of diabetes with an age-adjusted SHR of 1.48 (95% CI 1.16–1.89) compared with high officials (reference). SHRs were attenuated in the multivariable adjusted model after adjusting for conventional risk factors for diabetes and psychological stress, but a significantly higher risk was still observed in unskilled and semiskilled workers (SHR 1.39; 95% CI 1.08–1.78). We also estimated the multiple adjusted SHR, excluding psychological stress, and found that the SHR was still 1.39 (95% CI 1.09–1.78) for unskilled and semiskilled workers.
Table 2.
Age and multivariable-adjusted subdistribution hazard ratios and 95% CIs of the incidence of diabetes in different occupational classes over a 35-year follow-up period
| Occupational class | Number at risk | Diabetes cases, n | Observation years | Diabetes cases per 100 000 person-years | Age adjusted SHR (95% CI) | Multivariable adjusted* SHR (95% CI) |
|---|---|---|---|---|---|---|
| High officials, professionals | 793 | 88 | 22 485 | 391 | Ref | Ref |
| Intermediate, non-manual employees | 1231 | 139 | 34 001 | 409 | 1.05 (0.80–1.37) | 0.98 (0.75–1.29) |
| Assistant non-manual employees | 1348 | 171 | 34 475 | 496 | 1.21 (0.92–1.58) | 1.18 (0.90–1.54) |
| Skilled workers | 1871 | 255 | 48 145 | 530 | 1.28 (1.01–1.64) | 1.18 (0.93–1.51) |
| Unskilled and semiskilled workers | 1631 | 254 | 40 278 | 630 | 1.48 (1.16–1.89) | 1.39 (1.08–1.78) |
Adjusted for age, BMI, hypertension, smoking, physical activity and self-perceived psychological stress. SHR, subdistribution hazard ratio.
Figure 1 shows the cumulative incidence curves of diabetes and mortality across the occupational classes. The cumulative incidence of diabetes, when taking into account death as a competing event, was 16% in unskilled and semiskilled workers, 14% in skilled workers, 14% in assistant non-manual employees, 12% in intermediate non-manual employees, and 11% in high officials. Mortality among the men who were not diagnosed with diabetes was inversely related to occupational class, with unskilled and semiskilled workers having the highest cumulative risk of death (65%) and men with high official positions having the lowest risk (53%; Fig. 1).
FIGURE 1.
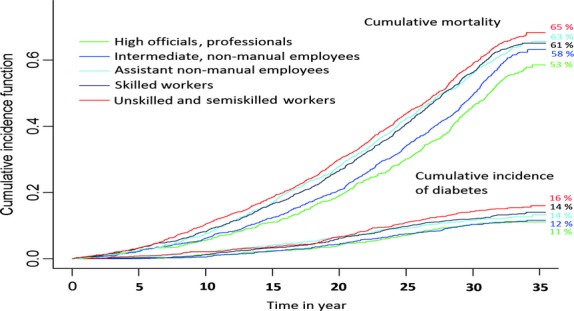
Cumulative incidence curves of diabetes and mortality across the occupational classes.
Figure 2 shows the conditional probability of diabetes according to different occupational classes by taking death attributable to other causes into account. The conditional probability of diabetes was 43% for unskilled and semiskilled workers, 35% for skilled workers, 31% for assistant non-manual employees, 26% for intermediate non-manual employees, and 23% for high officials.
FIGURE 2.
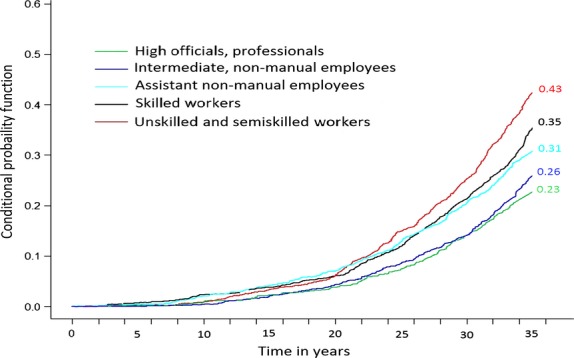
Conditional probability of diabetes according to different occupational classes, taking death attributable to other causes into account.
Discussion
In the present study, low occupational class was a significant predictor for diagnosed diabetes during a 35-year follow-up. The higher risk of diabetes in the lowest occupational class remained significant even after adjustment for several well-known risk factors for diabetes. A tendency towards a greater incidence among assistant non-manual employees and skilled workers was observed, but this was not significant. These findings are consistent with other studies [3,4,24], whereas other studies only found an association with education and not occupation [5]. The present study showed that there is inequality in the incidence of diabetes between different occupational classes among Swedish men, and this persists after a prolonged follow-up of 35 years. This finding is consistent with the results from a cross-sectional study [9] and a longitudinal study of women [13].
The most commonly used proxy for SES that has shown the strongest association with incident diabetes is education [3,25]. Even though education tends to lead to a higher occupation and income, different indicators of SES reflect different aspects of life, and they cannot be used interchangeably [26]. Occupation was the only indicator of SES in the present study and we had no data on education. Because most studies have reported a higher correlation for diabetes with education than with occupation [3,25], we could potentially have found a stronger association if SES had been based on education instead.
An explanation for the greater risk of diabetes in lower SES groups has been investigated in many studies. Conventional risk factors account for a large part of this greater risk, with approximately one third of the effect if measured at baseline only [5] and up to ∼50% if measured repeatedly [4].
Psychological stress is a known risk factor for diabetes [10] and lower SES groups have been shown to report a higher psychological burden [9]; therefore, stress and other psychological factors have been suggested as an explanation for the difference in risk of diabetes according to SES. Based on data from the present study population we have previously shown that permanent stress is independently associated with a higher risk of Type 2 diabetes [17]; however, in the present study, we did not find that psychological stress explained the difference in risk of diabetes across the occupational classes. Even so, psychological factors are difficult to define and complex to measure. In the present study, the measurement of stress was based on one question, which might be perceived as a crude measure; however, the same question was used in large international studies (e.g. the INTERHEART [18] and INTERSTROKE [19] studies), and it was found to be associated with other measures representing various forms of psychological stress across the ethnically diverse population of the INTERHEART study [18], being strongly correlated with other measures of stress including loss of control, stressful life events and financial stress. The INTERSTROKE study is the first large case–control study of risk factors for stroke. The study, with participants from 22 countries, found a significant association between stress and risk of all stroke across regions [19]. Although assessment of stress was based on one item, collectively, these results indicate the robustness of our measure of stress and of the other related psychological components it may comprise. Some studies have found that psychological factors can explain some of the difference in diabetes incidence between different SES groups [8], whereas others have found an association only for men [24] or for women [9]. Given the many different methods of measuring stress, slightly divergent findings are not surprising. Psychological stress related to SES could mediate its effect on diabetes incidence through unhealthy behaviours and through raised cortisol levels [12], but this was beyond the scope of the present study.
Moderate alcohol consumption has been shown to reduce the risk of Type 2 diabetes [27]. We did not adjust our analysis for alcohol consumption. The only information on alcohol in the present study was data on alcohol abuse from official registers (Swedish Board of Social Welfare for medical or legal problems attributed to alcohol). It is likely, however, that the risk of being registered is also socially patterned. Stringhini et al. [4] found in their study that alcohol had a negligible role in explaining the socio-economic difference in the risk of diabetes, so it seems unlikely that adjustment for alcohol consumption would have affected our estimates to any great extent.
Another potential explanation for the difference in diabetes incidence, which was not assessed in the present study, are early life factors. Prenatal or perinatal circumstances, such as low birth weight and preterm birth, may lead to insulin resistance and Type 2 diabetes later in life [28]. In the present study, men in the higher occupational classes were taller, similar to findings in other studies [29]. Height could reflect nutritional status during childhood, which can affect the risk of future diabetes [30]. We did not have any information regarding childhood SES of the participants, but because it is common for a child to adopt a similar SES to his/her parents [31], a substantial proportion of men in the higher occupational classes may also have had a high childhood SES. Low childhood SES has been argued to be responsible for some of the difference in diabetes incidence observed with regard to adult SES [32], but the findings are not consistent [33]. Physiological factors and dietary factors not detected in studies might also explain some of the remaining inequality in the risk of diabetes between different socio-economic status groups.
Strengths and limitations
The strengths of the present study include its large number of unselected men from the general population, its prospective longitudinal design, the extended follow-up, and the large number of diabetes cases (907 cases, 13%). Nevertheless, there are a number of limitations that must be considered. At baseline screening, there were no measurements of blood glucose or oral glucose tolerance test results. Type 2 diabetes can exist asymptomatically in a person for several years, therefore, some of the participants might have had undetected diabetes at study entry. These putative cases might be more frequent in lower occupational classes and could thus partly constitute the observed higher incidence. Nevertheless, the majority of diabetes cases were detected at least a decade after the baseline examination (816/907, 90%), and it is therefore unlikely that undiagnosed cases at baseline would affect the significance of an increased risk of diabetes for unskilled and semiskilled workers. We defined diabetes as a discharge from hospital with the diagnosis of diabetes, or as having a death certificate with the diagnosis of diabetes. Type 2 diabetes is often managed in primary healthcare, and someone who never attended hospital would not be detected; however, the majority of the men included in the study did attend hospital at some point (6498/6874, 94.5%), and most of them visited several times. We believe that most cases are captured since diabetes influences many other health conditions and therefore is likely to be registered at some point. At the end of the study, 98.1% (6743/6874) of the men were registered in one of the two registers. The absence of primary care data most likely explains why we found a comparatively low proportion of diabetes cases in the first 10 years compared with other studies [4,5], and accordingly, a ‘detection delay’. Older ICD versions (ICD-8 and ICD-9) do not differentiate between Types 1 and 2 diabetes. After middle age, the absolute majority of new diabetes cases are Type 2 and we do not believe that this potential misclassification would have greatly affected our estimates, if at all. Some covariates in the present study might be considered to be somewhat crude, and our findings could have been affected by residual confounders; however, other studies with more accurate measurements of some variables (e.g. physical activity with hours per week [4,5]) still found an independent association between SES and diabetes incidence. These potential confounders are therefore unlikely to have affected the significance of our findings. Finally, we only had baseline information on all of the covariates. Many of the covariates are time-dependent and fluctuations occur, so we might not have included the total effect of covariates on the association between occupational class and diabetes incidence.
In conclusion, the present cohort study in middle-aged Swedish men shows that low occupational class is an independent predictor of Type 2 diabetes. Conventional diabetes risk factors explain the difference to some extent, while additional adjustment for psychological stress does not alter the results. Further longitudinal studies on SES and incident diabetes with more refined measures of stress and other psychosocial factors are advisable to determine the role of these and other factors as mediators of the greater risk of Type 2 diabetes related to lower SES in Western developed countries.
Funding sources
The study was supported by grants from the Bank of Sweden Tercentenary Fund, the Swedish Heart and Lung Foundation, the Swedish Council for Working Life and Social Research (Epilife), the Swedish Research Council and the Gothenburg Medical Society.
Competing interests
None declared.
References
- 1.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.Dasgupta K, Khan S, Ross NA. Type 2 diabetes in Canada: concentration of risk among most disadvantaged men but inverse social gradient across groups in women. Diabet Med. 2010;27:522–531. doi: 10.1111/j.1464-5491.2010.02982.x. [DOI] [PubMed] [Google Scholar]
- 3.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40:804–818. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 4.Stringhini S, Tabak AG, Akbaraly TN, Sabia S, Shipley MJ, Marmot MG, et al. Contribution of modifiable risk factors to social inequalities in type 2 diabetes: prospective Whitehall II cohort study. BMJ. 2012;345:e5452. doi: 10.1136/bmj.e5452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams ED, Tapp RJ, Magliano DJ, Shaw JE, Zimmet PZ, Oldenburg BF. Health behaviours, socioeconomic status and diabetes incidence: the Australian Diabetes Obesity and Lifestyle Study (AusDiab) Diabetologia. 2010;53:2538–2545. doi: 10.1007/s00125-010-1888-4. [DOI] [PubMed] [Google Scholar]
- 6.Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res Clin Pract. 2005;68:230–236. doi: 10.1016/j.diabres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Sacerdote C, Ricceri F, Rolandsson O, Baldi I, Chirlaque MD, Feskens E, et al. Lower educational level is a predictor of incident type 2 diabetes in European countries: The EPIC-InterAct study. Int J Epidemiol. 2012;41:1162–1173. doi: 10.1093/ije/dys091. [DOI] [PubMed] [Google Scholar]
- 8.Dinca-Panaitescu M, Dinca-Panaitescu S, Raphael D, Bryant T, Pilkington B, Daiski I. The dynamics of the relationship between diabetes incidence and low income: longitudinal results from Canada's National Population Health Survey. Maturitas. 2012;72:229–235. doi: 10.1016/j.maturitas.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Agardh EE, Ahlbom A, Andersson T, Efendic S, Grill V, Hallqvist J, et al. Explanations of socioeconomic differences in excess risk of type 2 diabetes in Swedish men and women. Diabetes Care. 2004;27:716–721. doi: 10.2337/diacare.27.3.716. [DOI] [PubMed] [Google Scholar]
- 10.Pouwer F, Kupper N, Adriaanse MC. Does emotional stress cause type 2 diabetes mellitus? A review from the European Depression in Diabetes (EDID) Research Consortium. Discov Med. 2010;9:112–118. [PubMed] [Google Scholar]
- 11.Eriksson AK, van den Donk M, Hilding A, Ostenson CG. Work stress, sense of coherence, and risk of type 2 diabetes in a prospective study of middle-aged Swedish men and women. Diabetes Care. 2013;36:2683–2689. doi: 10.2337/dc12-1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosmond R, Bjorntorp P. The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med. 2000;247:188–197. doi: 10.1046/j.1365-2796.2000.00603.x. [DOI] [PubMed] [Google Scholar]
- 13.Cabrera C, Helgesson O, Wedel H, Björkelund C, Bengtsson C, Lissner L. Socioeconomic status and mortality in Swedish women: opposing trends for cardiovascular disease and cancer. Epidemiology. 2001;12:532–536. doi: 10.1097/00001648-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Norberg M, Stenlund H, Lindahl B, Andersson C, Eriksson JW, Weinehall L. Work stress and low emotional support is associated with increased risk of future type 2 diabetes in women. Diabetes Res Clin Pract. 2007;76:368–377. doi: 10.1016/j.diabres.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Wilhelmsen L, Berglund G, Elmfeldt D, Tibblin G, Wedel H, Pennert K, et al. The multifactor primary prevention trial in Goteborg. Sweden. Eur Heart J. 1986;7:279–288. doi: 10.1093/oxfordjournals.eurheartj.a062065. [DOI] [PubMed] [Google Scholar]
- 16.Statistics S. [Socioekonomisk indelning (SEI) 1983. Meddelande i samordingsfrågor 1982:4 (Swedish socio-economic classification SEI) Reports on statistical coordination, in Sweden with an english summary]
- 17.Novak M, Bjorck L, Giang KW, Heden-Ståhl C, Wilhelmsen L, Rosengren A. Perceived stress and incidence of Type 2 diabetes: a 35-year follow-up study of middle-aged Swedish men. Diabet Med. 2013;30:e8–e16. doi: 10.1111/dme.12037. [DOI] [PubMed] [Google Scholar]
- 18.Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 19.O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 20.Fine JP, Gray RJ. A proportional Hazards Model for the Subdistribution of a Competing risk. J Am Statis Assoc. 1999;94:496–509. [Google Scholar]
- 21.Kohl M, Heinze G. 2012. PSHREG: A SASr macro for proportional and nonproportional substribution hazards regression with competing risk data: Vienna.
- 22.Schemper M, Wakounig S, Heinze G. The estimation of average hazard ratios by weighted Cox regression. Statistics in medicine. 2009;28:2473–2489. doi: 10.1002/sim.3623. [DOI] [PubMed] [Google Scholar]
- 23.Pintilie M. 2006. Competing risks: a practical perspective: Wiley.com.
- 24.Kumari M, Head J, Marmot M. Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Arch Intern Med. 2004;164:1873–1880. doi: 10.1001/archinte.164.17.1873. [DOI] [PubMed] [Google Scholar]
- 25.Maty SC, Everson-Rose SA, Haan MN, Raghunathan TE, Kaplan GA. Education, income, occupation, and the 34-year incidence (1965-99) of Type 2 diabetes in the Alameda County Study. Int J Epidemiol. 2005;34:1274–1281. doi: 10.1093/ije/dyi167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geyer S, Hemstrom O, Peter R, Vagero D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health. 2006;60:804–810. doi: 10.1136/jech.2005.041319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28:719–725. doi: 10.2337/diacare.28.3.719. [DOI] [PubMed] [Google Scholar]
- 28.Kaijser M, Bonamy AK, Akre O, Cnattingius S, Granath F, Norman M, et al. Perinatal risk factors for diabetes in later life. Diabetes. 2009;58:523–526. doi: 10.2337/db08-0558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peck MN, Lundberg O. Short stature as an effect of economic and social conditions in childhood. Soc Sci Med. 1995;41:733–738. doi: 10.1016/0277-9536(94)00379-8. [DOI] [PubMed] [Google Scholar]
- 30.van Abeelen AF, Elias SG, Bossuyt PM, Grobbee DE, van der Schouw YT, Roseboom TJ, et al. Famine exposure in the young and the risk of type 2 diabetes in adulthood. Diabetes. 2012;61:2255–2260. doi: 10.2337/db11-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuh DB-SY, editor. 2007. A life course approach to chronic disease epidemiology Oxford University press.
- 32.Maty SC, Lynch JW, Raghunathan TE, Kaplan GA. Childhood socioeconomic position, gender, adult body mass index, and incidence of type 2 diabetes mellitus over 34 years in the Alameda County Study. Am J Public Health. 2008;98:1486–1494. doi: 10.2105/AJPH.2007.123653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agardh EE, Ahlbom A, Andersson T, Efendic S, Grill V, Hallqvist J, et al. Socio-economic position at three points in life in association with type 2 diabetes and impaired glucose tolerance in middle-aged Swedish men and women. Int J Epidemiol. 2007;36:84–92. doi: 10.1093/ije/dyl269. [DOI] [PubMed] [Google Scholar]


