Abstract
Aim:
To compare the effect of honey, chlorhexidine mouthwash and combination of xylitol chewing gum and chlorhexidine mouthwash on the dental plaque level.
Materials and Methods:
Ninety healthy dental students, both male and female, aged between 21 to 25 years participated in the study. The subjects were randomly divided into three groups, i.e. the honey group, the chlorhexidine gluconate mouthwash group and the combination of xylitol chewing gum and chlorhexidine (CHX) mouthwash group. The data was collected at the baseline, 15th day and 30th day; the plaque was disclosed using disclosing solution and their scores were recorded at six sites per tooth using the Quigley and Hein plaque index modified by Turesky-Gilmore-Glickman. Statistical analysis was carried out later to compare the effect of all the three groups. P ≤ 0.05 was considered as statistically significant.
Results:
Our result showed that all the three groups were effective in reducing the plaque but post-hoc LSD (Least Significant Difference) showed that honey group and chlorhexidine + xylitol group were more effective than chlorhexidine group alone. The results demonstrated a significant reduction of plaque indices in honey group and chlorhexidine + xylitol group over a period of 15 and 30 days as compared to chlorhexidine.
Keywords: Chlorhexidine, honey, plaque index, xylitol
INTRODUCTION
Removal of supragingival plaque is the mainstay in the maintenance of a healthy periodontium. Dental plaque is associated with the most prevalent oral diseases like dental caries and periodontal diseases. The removal of plaque is a determining component in the prevention and treatment of these diseases. The use of mechanical agents is a simple and cost-effective method that has been demonstrated to be efficient in the control of gingivitis.[1,2,3] High percentage of individuals all over world do not practice an acceptable standard of mechanical plaque removal due to lack of dexterity in performing oral hygiene methods. Therefore, several anti-plaque agents are being available in the market. With the rise in bacterial resistance to antibiotics, there is much interest in the development of herbal antimicrobials.
The most effective anti plaque agent till date is chlorhexidine.[4,5] Many of the currently available mouthrinses including chlorhexidine do have drawbacks, such as alteration in taste sensation and staining of teeth. In order to overcome such side effects the WHO has advised to investigate the possible use of natural products (herb and plant extracts).[6,7,8]
Xylitol present in chewing gum inhibits bacterial growth through two mechanisms: Direct inhibition of the glycolytic route resulting from the xylitol 5-phosphate derivative and/or indirect inhibition resulting from the competition for the HPr-P (phosphorylated phosphocarrier protein) carrier between glucose and xylitol. Chlorhexidine disrupts the cell membrane of targeted bacteria and cause leakage of its cytoplasmatic constituents.[9]
Honey is defined as a sweet liquid substance produced by bees that have been used as a source of nutrients as well as medicine since ancient times.[10,11] Honey can be kept for long periods of time without spoiling, because of its high osmotic pressure and anti bacterial property. It has been shown to have broad antimicrobial activity and thus inhibit the growth of a wide range of bacteria, fungi, protozoa, and viruses. Hydrogen peroxide is generated on the slow dilution of unprocessed honey. Several chemicals had been demonstrated in honey with different antibacterial activity. According to recent research blood lymphocytes is also stimulated by action of honey.[12,13]
Hence, the present study was undertaken with an aim to compare the effect of honey, chlorhexidine gluconate mouthwash (0.2%) and combination of xylitol chewing gum and chlorhexidine gluconate mouthwash (0.2%) on the dental plaque levels.
MATERIALS AND METHODS
This single blind (Investigator was blinded to the group allocation) randomized control trial; three group parallel study was conducted in the Department of Public Health Dentistry on 90, both male and female, volunteered students of Teerthanker Mahaveer Dental College and Research center. Protocol was approved by the Institutional Review Board (IRB) of Teerthanker Mahaveer University. All subjects signed an IRB approved consent form. Pilot study was done on five patients in each group to check the feasibility of the study; results are not included in the present study.
Inclusion and exclusion criteria
The students with no history of any dental treatment, antibiotic or anti-inflammatory drug therapy for the past three months were included in the study. Students with any of history systemic diseases/conditions, fibrotic gingival enlargement and smoking were excluded from the study. Participants with good general health, a baseline plaque score greater than 1.5 and a baseline DMFT (Decayed, Missing, Filled Tooth) index of 3 to 5 were included in the study. Those volunteers who had used antibiotics or mouthwash for five consecutive days or corticosteroids in the past 30 days were excluded from the study. Those subjects who had a history of sensitivity to any mouthwash or used removable prostheses or an orthodontic appliance were excluded from the study. Also, those who had undergone professional measures to remove plaque and calculus in the past 15 days, and did not give consent for clinical trial were excluded.
The data was collected at the baseline, 15th day, and 30th day. The plaque was disclosed using disclosing solution (containing erythrosine dye) and their scores were recorded using the Quigley and Hein plaque index modified by Turesky-Gilmore-Glickman. Disclosing agent was applied with the help of cotton pellet on the buccal and lingual aspect of the tooth. The colored area on the buccal/lingual surface of the teeth was measured to note the amount of plaque present on the surface. Subjects were randomly divided into three groups, i.e. the honey group, the chlorhexidine group (0.2%) and the combination of chlorhexidine (0.2%) and xylitol chewing gum group. A total of 90 volunteers were randomly allocated into the three study groups through computer-generated random numbers. Random allocation of experimental oral hygiene aid was done using the lottery method. Individuals were identified by code numbers throughout the study. The procedure of applying honey and rinsing with mouthwash was done daily under the observation of instructor.
Group I (Honey group): The subjects were trained to apply the honey gently into the gingival sulcus of all the teeth, wait for 5 min and then repeat the procedure twice. The honey was applied twice a day after meals.
Group II (Chlorhexidine group): The subjects were asked to rinse their mouth with 10 ml solution of 0.2% chlorhexidine mouthwash twice a day for 60 seconds. After reaching the exact-rinsing time, the subjects had to expectorate the mouth wash.
Group III (CHX and Xylitol): In this group, the subjects were instructed to chew the sugarless xylitol chewing gum for 5 minutes, thrice a day after meals and the subjects were also asked to rinse their mouth with 10 ml solution of 0.2% chlorhexidine mouthwash twice a day for 60 seconds. After reaching the exact-rinsing time of 60 seconds, the subjects had to expectorate the mouth wash.
Patients were instructed not to rinse the mouth with water or other mouthwashes or eat after the use of experimental material for half an hour.
After 15 days and 30 days, the plaque was disclosed using disclosing solution and the scores were recorded using the Quigley and Hein plaque index modified by Turesky-Gilmore-Glickman.[14] All measurements were carried out using the same disclosing solution under the same circumstances.[15] The students did not discontinue with their routine oral hygiene practices.
RESULTS
All the participants completed the study. Descriptive baseline statistics are represented in Table 1. Table 2 depicts mean ± SD (Standard Deviation) and percentage change in plaque scores for the Group I, II and III. ANOVA (Analysis of Variance) was used to analyze the reduction in plaque in the three groups. ANOVA [Table 3] was carried out to assess the intra- and inter-group variations for plaque. There was no difference in the baseline value in plaque P > 0.05. There was a significant decrease in the plaque in all the three groups at 15 days and 30 days (P < 0.05) [Table 3]. There was progressive decrease in the plaque score at 5% level of significance. Chlorhexidine + xylitol group showed maximum decrease as compared to honey group but difference was not statistically significant [Table 4]. There was statistical difference between honey group and chlorhexidine group. Honey resulted in better antiplaque agent than chlorhexidine. Multiple comparisons were obtained by post-hoc LSD [Table 4]. The difference in the decrease in plaque (P = 0.778 at 15 days and P = 0.684 at 30 days) between Group I and Group III was not statistically significant. However, the difference between honey group and the chlorhexidine group and chlorhexidine and chlorhexidine + xylitol group was significant (P < 0.05). Data shows that honey is better antiplaque agent than chlorhexidine but is statistically equivalent to combination of chlorhexidine and xylitol [Figure 1].
Table 1.
Baseline background of the subjects
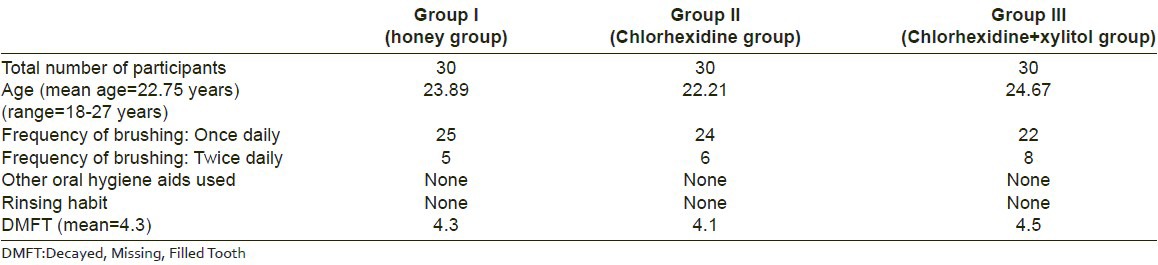
Table 2.
Plaque score at baseline, after 15 days and after 30 days
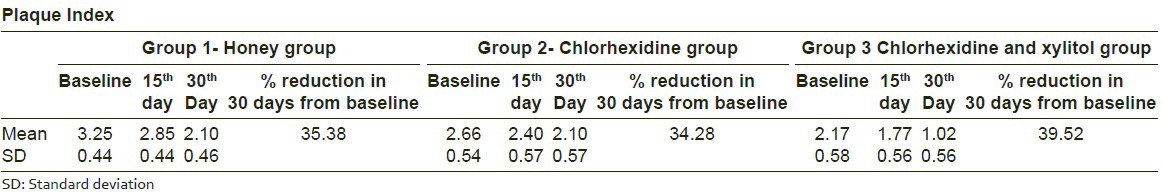
Table 3.
ANOVA of the three study groups
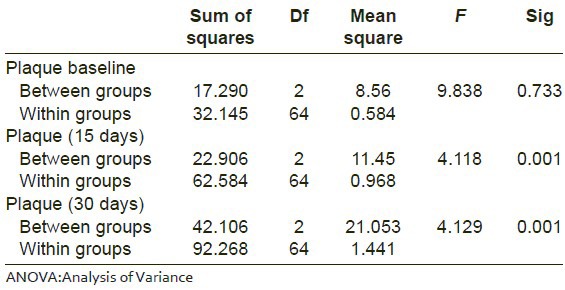
Table 4.
Post-hoc LSD test for multiple comparison
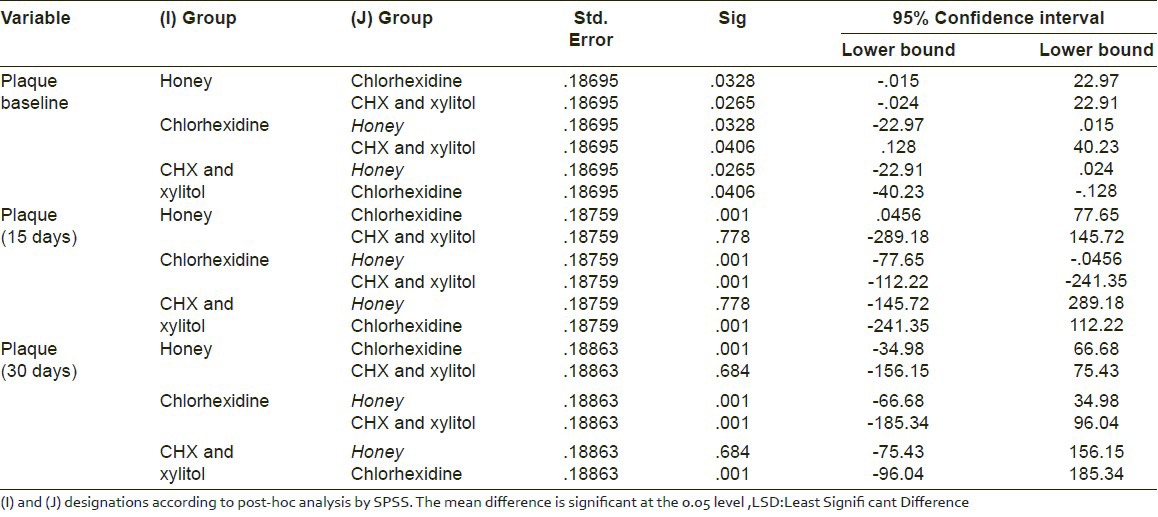
Figure 1.
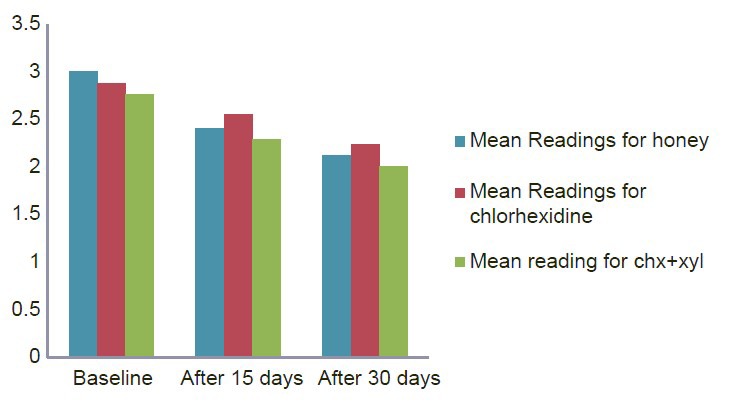
Mean plaque score change of three groups from baseline to 30 days
DISCUSSION
Dental plaque is a complex, specific but highly variable structural entity resulting from colonization of microorganisms embedded in a gelatinous extracellular matrix on tooth surfaces, restorations and other parts of oral cavity.[16,17,18,19,20,21,22,23,24,25]
Chlorhexidine is the leading antiplaque agent till date, because of its many ideal properties, and its efficacy has been proven by many studies. Chlorhexidine acts by damaging the cell membrane of prokaryotes and by disrupting the cytoplasmatic constituents.[9]
Some of cariogenic microorganisms are naturally resistant to chlorhexidine. Cariogenic microorganisms do not metabolize xylitol and hence, salivary mutans streptococcus counts drop with consistent use of xylitol-sweetened gum, probably because xylitol “starves” the cariogenic microorganisms.[6] Thus, it was thought the synergistic effect of xylitol chewing gum and 0.2% chlorhexidine mouthwash is better than 0.2% chlorhexidine mouthwash alone.
The antibacterial property of honey was first recognized in 1892 by van Ketel. Honey inhibits a wide range of bacterial species in vitro. The antimicrobial activity of honey is due to high osmotic pressure, physical properties, enzymatic glucose oxidation reaction. Honey has high osmotic properties so it can extract water from bacterial cells and cause them to die. Among the possible mechanisms are the presence of inhibitory factors such as flavonoids, hydrogen peroxide, low pH, and high osmolarity due to its sugar concentration. All types of saturated sugar syrups have a tendency to reduce microbial growth due to its high osmolarity and honey is also saturated. Hydrogen peroxide is the main antibacterial substance produced by enzymatic reaction from honey.[10,12,13] According to Ahmadi et al.,[11] honey shows greatest antibacterial activity at 100% concentration.
In the present study there was a significant difference between honey and chlorhexidine mouthwash when compared against plaque. Nayak PA et al., (2010)[1] analyzed the effect of Manuka honey and chlorhexidine mouthwash. They found no significant difference between both the groups. In the present study there is no significant difference between honey and chlorhexidine + xylitol group. The results of these two groups on plaque could not be compared with other studies as no studies have been reported in the literature which has tried to assess the same effect. We found a statistically significant difference between chlorhexidine and chlorhexidine + xylitol group. Decker et al.,[8] investigated the effect of combining xylitol and chlorhexidine on the viability of Streptococcus sanguis or S. mutans. The xylitol and chlorhexidine combination showed a significant antibacterial effect on streptococci when compared to pure xylitol or chlorhexidine used alone. When xylitol chewing gum is chewed thrice a day directly after meals then only the maximum effect occurs.[6,7]
The results of present study suggest that honey has a plaque inhibitory effect which is statistically equal to chlorhexidine mouthwash and is less potent than the combination of chlorhexidine gluconate and xylitol. Within the limitations of the study honey has shown a good antiplaque activity, however clinical trials of large duration with large sample size and microbial analysis are required for better validation of honey as antiplaque agent.
CONCLUSION
Honey is one of the most potent anti-bacterial agents having a wide spectrum of pharmacological and medicinal activities. It has a number of pharmacological activities due to the presence of various types of bioactive compounds. In this study, honey and chlorhexidine + xylitol group has stood the test by demonstrating more effects than chlorhexidine on plaque. This is an encouraging result which clearly favors promotion of honey among the rural communities, especially belonging to low socioeconomic strata as honey is easily accessible. As xylitol also acts as an antiplaque agent, the combination of it with chlorhexidine mouthwash is more effective in reducing plaque. Researchers need to have a fresh look in the area of herbal medicine as well as in synergistic effect of chlorhexidine with other anti- plaque agents.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nayak PA, Nayak UA, Mythili R. Effect of Manuka honey, chlorhexidine gluconate and xylitol on the clinical levels of dental plaque. Contemp Clin Dent. 2010;4:214–7. doi: 10.4103/0976-237X.76386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xime’nez-Fyvie LA, Haffajee AD, Som S, Thompson M, Torresyap G, Socransky SS. The effect of repeated professional supragingival plaque removal on the composition of the supra-and subgingival microbiota. J Clin Periodontol. 2000;27:637–47. doi: 10.1034/j.1600-051x.2000.027009637.x. [DOI] [PubMed] [Google Scholar]
- 3.Gupta D, Bhaskar DJ, Gupta RK, Karim B, Jain A, Singh R, et al. A randomized controlled clinical trial of Ocimum sanctum and chlorhexidine mouthwash on dental plaque and gingival in ammation. J Ayurveda Integr Med. 2014;5:109–16. doi: 10.4103/0975-9476.131727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kayalvizhi G, Suganya G, Balaji Subramaniyan R. A Cuppa for Caries Free Teeth? International Journal Contemporary Medical Research. 2014;1:19–27. [Google Scholar]
- 5.Zanatta FB, Antoniazzi RP, Rosing CK. The effect of 0.12% chlorhexidine gluconate rinsing on previously plaque-free and plaque-covered surfaces: A randomized, controlled clinical trial. J Periodontol. 2007;78:2127–34. doi: 10.1902/jop.2007.070090. [DOI] [PubMed] [Google Scholar]
- 6.Gupta D, Bhaskar DJ, Gupta RK, Karim B, Gupta V, Punia H, et al. Eff ect of Terminalia chebula extract and chlorhexidine on salivary pH and periodontal health: 2 weeks randomized control trial. Phytotherapy Research. 2014;287:992–8. doi: 10.1002/ptr.5075. [DOI] [PubMed] [Google Scholar]
- 7.Gupta D, Bhaskar DJ, Gupta RK. Germany: Lap Lambert Academic Publishing; 2013. Contemporary and alternative dentistry: Ayurveda in dentistry. [Google Scholar]
- 8.Decker EM, Maier G, Axmann D, Brecx M, von Ohle C. Effect of xylitol/chlorhexidine versus xylitol or chlorhexidine as single rinses on initial biofilm formation of cariogenic streptococci. Quintessence Int. 2008;39:17–22. [PubMed] [Google Scholar]
- 9.Gupta RK, Gupta D, Bhaskar D, Yadav A, Obaid K, Mishra S. Preliminary antiplaque ef cacy of aloe vera mouthwash on 4 day plaque re-growth model: Randomized control trial. Ethiop J Health Sci. 2014;24:139–44. doi: 10.4314/ejhs.v24i2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahuja A, Ahuja V. Apitherapy - A sweet approach to dental diseases-Part I: Honey. J Adv Dent Res. 2010;1:81–6. [Google Scholar]
- 11.Ahmadi-Motamayel F, Hendi SS, Alikhani MY, Khamverdi Z. Antibacterial activity of honey on cariogenic bacteria. J Dent. 2013;10:10–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Jeffrey AE, Echazarreta CM. Medical uses of honey. Rev Biomed. 1996;7:43–9. [Google Scholar]
- 13.Cooper RA, Jenkins L. A comparison between medical grade honey and table honeys in relation to antimicrobial efficacy. Wounds. 2009;21:29–36. [Google Scholar]
- 14.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970;41:41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 15.Axelsson P, Lindhe J. Efficacy of mouth rinses in inhibiting dental plaque and gingivitis in man. J Clin Periodontol. 1987;14:205–12. doi: 10.1111/j.1600-051x.1987.tb00968.x. [DOI] [PubMed] [Google Scholar]
- 16.Gupta D, Gupta RK, Bhaskar DJ, Gupta V. Comparative Evaluation of Terminalia chebula Extract Mouthwash and Chlorhexidine Mouthwash on Plaque and Gingival Inflammation - 4-week Randomized Control Trial. Oral Health Prev Dent. 2014 doi: 10.3290/j.ohpd.a32994. doi: 10.3290/j.ohpd.a32994. [DOI] [PubMed] [Google Scholar]
- 17.Gupta D, Bhaskar DJ, Gupta RK, Jain A, Yadav P, Dalai DR, et al. Is complementary and alternative medicine effective in job satisfaction among dentists with musculoskeletal disorders? A cross sectional study. Medycyna Pracy. 2014;65:317–23. [PubMed] [Google Scholar]
- 18.Karim B, Bhaskar DJ, Agali A, Gupta D, Gupta RK, Jain A, et al. Effect of Aloe vera mouthwash on periodontal health: Triple blind randomized control trial. Oral Health Dent Manag. 2014;13:14–9. [PubMed] [Google Scholar]
- 19.Vaid N, Bhargava D, Chandavarkar V, Sharma R, Mishra M. Juvenile Myofibromatosis of Mandible-A Case Report. International Journal of Contemporary Medical Research. 2014;1:72–9. [Google Scholar]
- 20.Gupta D, Bhaskar DJ, Gupta RK, Karim B, Kanwar A, Jain A, et al. Use of complementary and alternative medicine for work related musculoskeletal disorders associated with job contentment in dental professionals: Indian outlook. Ethiop J Health Sci. 2014;24:117–24. doi: 10.4314/ejhs.v24i2.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gupta D, Dalai DR, Swapnadeep, Mehta P, Indra B N, Rastogi S, et al. Acupuncture (針灸ZhēnJiǔ) - An Emerging Adjunct in Routine Oral Care. Journal of Traditional Complementary Medicine. 2014;4:218–23. doi: 10.4103/2225-4110.139113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jain A, Bhaskar DJ, Gupta D, Agali C, Gupta V, Mark R. Dental Hand for Rural population: Teledentistry. J Contemp Dent. 2014;4:27–9. [Google Scholar]
- 23.Gupta D, Batra R, Mahajan S, Bhaskar DJ, Jain A, Shiju M, et al. Comparative Evaluation of the Complementary and Alternative Medicine Therapy and Conventional Therapy Use for Musculoskeletal Disorders Management and Its Association with Job Satisfaction among Dentists of West India. J Tradit Complement Med. 2014;4:263–7. doi: 10.4103/2225-4110.126632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain A, Bhaskar DJ, Gupta D. Germany: Lap Lambert Academic Publishing; 2013. Adverse oral habits; pp. 8–10. [Google Scholar]
- 25.Gupta D, Nagar P, Karim B, Khan IM, Naveen B, Chaturvedi M, et al. Oral Health Dent Manag. Vol. 13. Uttarakhand: a cross sectional study; 2014. Tobacco abuse amongst the school going students of 15 to 18 years of Almora district; pp. 680–6. [PubMed] [Google Scholar]


