Abstract
Background:
Rapid and proper diagnosis of sepsis is one of the daily challenges of emergency department (ED) and intensive care units. The general aim of the present study was to determine the efficacy of measuring procalcitonin levels in the early diagnosis of bacterial resistance to antibiotics administered empirically in patients with sepsis.
Materials and Methods:
The present cross-sectional study consisted of patients with clinical evidence of sepsis or systemic inflammatory response syndrome (SIRS), referring to the ED of a third-level hospital in Tehran, Iran in 2012. After collection of basic and clinical data of patients, venous blood samples were taken for routine laboratory tests and determination of procalcitonin serum levels at baseline and 6 and 24 hours after administration of the first dose of an empirical antibiotic. The subjects were divided into two groups of discharged and expired and then comparisons were made using t-test, Chi-squared test and Fisher's test. Specificity and sensitivity of procalcitonin were evaluated along with ROC curve.
Results:
In the present study, 170 patients with sepsis were included. Evaluation of serum levels of procalcitonin 24 hours after administration of antibiotics exhibited the best sensitivity and specificity for each patient's response to antibiotics. Use of the cutoff point of 6.5 mg/mL for procalcitonin can predict the disease outcome with sensitivity and specificity of 67% and 80%, respectively.
Conclusion:
It is suggested that procalcitonin be used for the diagnosis of sepsis or SIRS resulting from an infectious disease, for follow-up of treatment and for evaluation of response to treatment.
Keywords: Procalcitonin, sensitivity, sepsis, specificity
INTRODUCTION
Sepsis is a common and dangerous condition, which results it a large number of mortalities and patient complications despite recent advances.1,2,3,4 At present, the incidence of sepsis and septic shock is on the rise due to the widespread use of invasive tools and immunosuppressive drugs and an increase in the resistance of microorganisms resistant to antibiotics.5 Although antibiogram is the most reliable technique to evaluate patient response to antibiotics, it is not a very effective technique in patients with sepsis. If the patient's response to antibiotics is determined rapidly and the patient receives proper treatment, the patient will not undergo a septic shock, resulting in a 40-60% decrease in mortality and morbidity in patients with sepsis.6,7 During the past few years a relationship has been reported between serum levels of procalcitonin and the severity of injury, sepsis and deficiency of various organs.8 These studies have shown that procalcitonin might be a suitable marker to monitor the inflammatory status of patients who have been injured and are at risk.9 The results of these studies have shown that response to treatment and even initiation of response to treatment with the first dose of antibiotic result in a decrease in serum levels of procalcitonin. This decrease in procalcitonin levels, which is seen in the peak phase of antibiotic effect, is due to a decrease in bacteraemia severity, resulting in a decrease in procalcitonin level. Based on these results a decrease in procalcitonin serum levels, from the initial levels to levels below 0.5 ng/mL after administration of empirical antibiotics, is considered response to treatment.10 Therefore, the serum level of procalcitonin might be a proper factor to evaluate response to treatment. Despite the data available, there is still no answer to the question what cutoff points of serum levels of procalcitonin and what time interval cutoff points are appropriate to determine response to antibiotics. Therefore, the present study was undertaken to evaluate the efficacy of determining procalcitonin serum levels to determine prognosis and early diagnosis of bacterial resistance in sepsis in emergency units so that the sensitivity and specificity of this diagnostic method at different time intervals would be assessed so that the best time cutoff point would be determined.
MATERIALS AND METHODS
This was a cross-sectional study was carried out on all the patients with sepsis, referring to the emergency department (ED) of a third-level hospital in Tehran, Iran from July 2011 to July 2012. The study protocol was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences and the researchers observed all the guidelines of Helsinki Declaration throughout the study.
The inclusion criteria consisted of all the patients with evidence of sepsis or patients with SIR, referring to the ED. The exclusion criteria consisted of the use of corticosteroids, immunodeficiency, thyroid cancer and presence of a central vein catheter. The minimum number of subjects was determined to be 100 patients at α = 0.05 and CI: 95% with accuracy estimate of d = 0.1 and P = 0.5.
The subjects were included in the study sequentially. Patients with sepsis and SIRS with an infectious origin were included and finally patients with SIRS with or non-infectious origin based on the results of culture were excluded from the study. In addition, patients who had not received antibiotics at specific time intervals based on the protocol and had not undergone blood tests at the appropriate time were finally excluded from the study.
Demographic data, a history of previous disease, and clinical condition and its course were accurately recorded in data sheets. Serum levels of procalcitonin were determined and recorded at three intervals: before administration of antibiotics and 6 and 24 hours after administration of antibiotics. Immunoluminometric technique, with ELISA kit (USCN Life Science Inc., Wuhan), was used to determine serum levels of procalcitonin. In order to avoid paraclinical errors, the results of paraclinical recovery of patients were compared with those of clinical recovery in response to antibiotic treatment. Treatment of patients was based on clinical conditions and the guidelines of Infectious Diseases Society of America. The selected empirical antibiotic, based on the infection focus and the background information and in case of absence of a definite infection focus based on the guidelines of Infectious Diseases Society of America, was administered during the first hour of the patient's presentation at the Emergency Unit. All the patients were questioned about the antibiotics taken during the previous 3 months, use of corticosteroids, presence of a catheter which could not be removed and living in a nursing home. Therefore, the patients with evidence of infection at presentation received empirical antibiotics based on the guidelines of Infectious Diseases Society of America. Six and 24 hours after administration of antibiotics the serum levels of procalcitonin, as a marker for bacteraemia, were controlled and finally compared with patient outcomes. In order to control procalcitonin serum levels, 5 mL of venous blood were taken from the cubital vein of the left hand in supine position. The blood serum was isolated by centrifugation and stored at −20°C. In addition, 5-10 mL of venous blood was taken at three 5-10-minute intervals in order to prepare an antibiogram. Finally, the results of the clinical response of patients, including recovery from high body temperature, and the initial clinical symptoms and signs, including coughing, dysuria, etc., were evaluated.
The final outcome, including recovery or death, was evaluated along with procalcitonin serum levels. Therefore, the subjects were divided into two groups: discharged and expired. Finally, changes in procalcitonin serum levels, compared to the baseline, were evaluated at 6- and 24-hour intervals after administration of empirical antibiotics between the two groups.
Data analysis
T-test was used to evaluate differences in age and ESR between the two groups. Chi-squared test and Fisher's test were used to evaluate differences in gender distribution, paraclinical findings, a history of previous disease, source of infection, blood homeostasis status and patient clinical recovery; Mann-Whitney test was used to evaluate CRP and procalcitonin serum levels. The patients were divided into four groups to evaluate changes in procalcitonin serum levels:
A progressive decrease in procalcitonin serum levels;
An initial decrease and then an increase in procalcitonin serum levels;
An initial increase and then a decrease in procalcitonin serum levels; and
A progressive increase in procalcitonin serum levels.
Sensitivity and specificity of serial evaluation of procalcitonin serum levels for the early diagnosis of bacterial resistance to antibiotics based on the results of antibiogram were also assessed. Finally, ROC curve was drawn in order to evaluate this diagnostic technique. Statistical significance was defined at P < 0.05 for all the analyses.
RESULTS
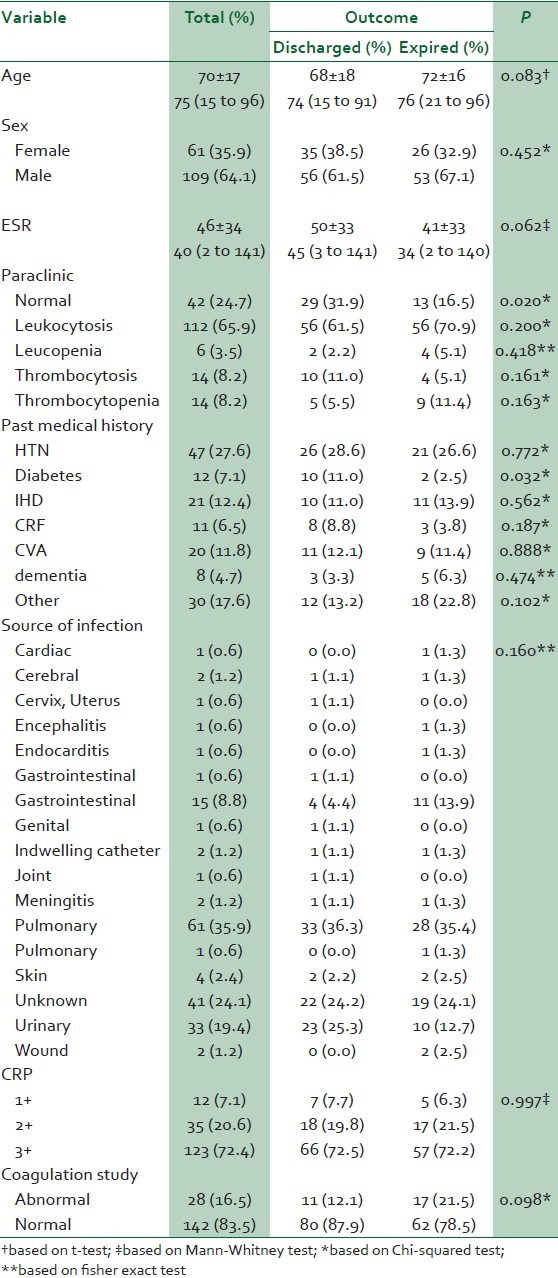
In the present study, 170 patients were evaluated: 91 patients (53.5%) recovered and were discharged and 79 (46.5%) passed away. Means and standard deviations of patient ages in the discharged and expired groups were 68 ± 18 and 72 ± 16 years, respectively (P = 0.083). In the discharged and expired groups, 35 (38.5%) and 26 (32.9%) patients were female, respectively (P = 0.45). Paraclinical findings in 29 (31.9%) and 13 (16.5%) patients were normal in the discharged and expired groups, respectively (P = 0.02). Of all the background conditions, diabetes was the only condition which differed between the two groups (P = 0.3). However, the source of infection did not exhibit any difference between the two groups (P = 0.16) [Table 1]. None of the background conditions exhibited a significant relationship with the disease outcome (P > 0.05).
Table 1.
Baseline characteristic of patients
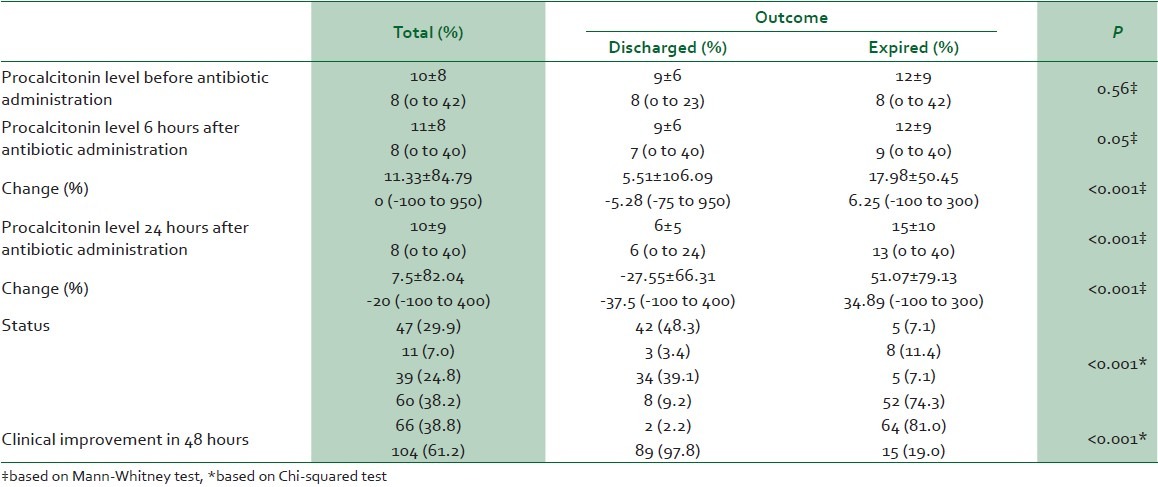
Evaluation of the serum levels of procalcitonin did not exhibit any differences in the baseline levels of this marker (before administration of antibiotics) between the discharged and expired patients (P = 0.56). The mean and standard deviation of procalcitonin serum levels before antibiotic administration was 10 ± 8 ng/mL. The means and standard deviations of this marker in the discharged and expired groups were 9 ± 6 ng/mL and 12 ± 9 ng/mL, respectively.
Six hours after administration of antibiotics the serum levels of procalcitonin reached 9 ± 6 ng/mL and 12 ± 9 ng/mL in the discharged and expired groups, respectively. Here the difference in procalcitonin serum levels between the two groups was just at the significance level (P = 0.05). After 24 hours, the procalcitonin serum levels significantly decreased, in the discharged group, to 6 ± 5 ng/mL; however, the levels in the expired group significantly increased and reached 15 ± 10 ng/mL (P < 0.001). The serum levels of procalcitonin progressively decreased in 42 (48.3%) patients in the discharged group and in 5 (7.1%) in the expired group. Procalcitonin serum levels in 3 (3.4%) patients in the discharged group and in 8 (11.4%) patients in the expired group decreased at first and then increased. Chi-squared test showed that the majority of discharged patients had a decreasing trend in procalcitonin serum levels, with statistically significant differences from the expired group (P < 0.001) [Table 2].
Table 2.
Comparison of procalcitonin serum levels in terms of disease outcome
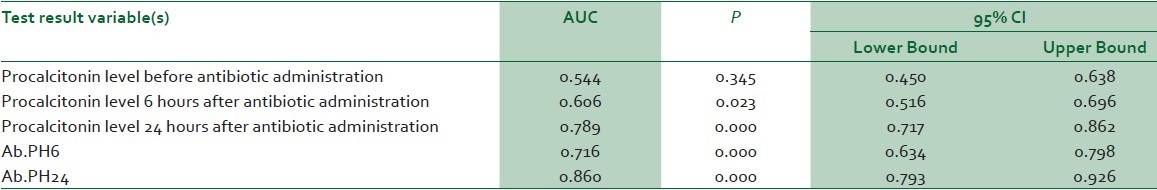
Evaluation of sensitivity of measuring procalcitonin serum levels in determining patient outcome showed the highest sensitivity 24 hours after antibiotic administration. The area under curve for this diagnostic technique 24 hours after initiation of treatment was 0.789: It was in the range of 0.717−0.862 at a confidence interval of 95% [Table 3].
Table 3.
Area under curve of procalcitonin level in several time points
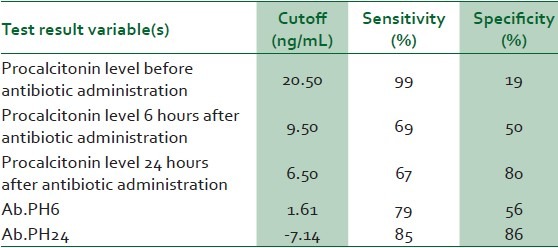
In addition, use of 6.5 ng/mL cutoff point was able to determine whether the patient had given a response to antibiotic or not, with sensitivity of 67% and specificity of 80%, i.e., when the serum level of procalcitonin is higher than this it can be postulated that there exists bacterial resistance and when it is lower than this it can be postulated with reasonable accuracy that the antibiotic administered is suitable for the treatment of infection [Table 4].
Table 4.
Sensitivity and specificity of procalcitonin in prediction of sepsis outcome
The ROC curve, too, showed that the highest procalcitonin sensitivity to determine disease outcome occurred 24 hours after antibiotic administration [Figure 1].
Figure 1.
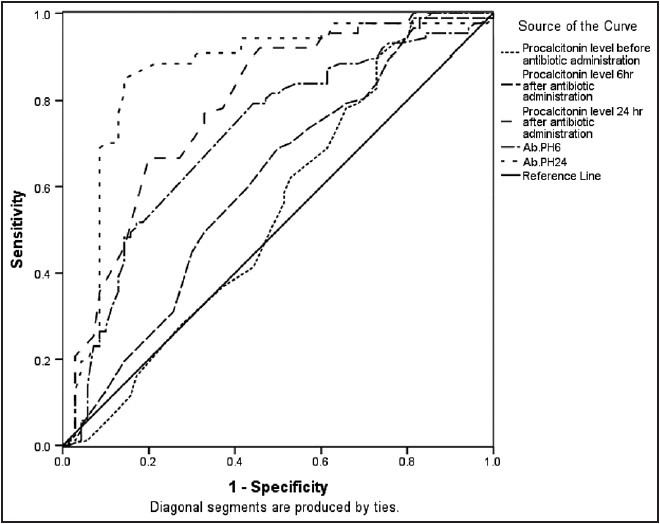
ROC curve for the evaluation of various time cutoff points in predicting the outcome of sepsis or septic shock
DISCUSSION
The present study is the first study to present concentration and time cutoff points for procalcitonin serum levels and the time to run the test. These cutoff points are a serum level of 6.5 ng/mL and 24 hours after antibiotic administration, which will contribute to more accurate follow-ups of treatment protocols of patients with sepsis. Of course, further studies are necessary so that these cutoff points can be used in new treatment protocols. However, the researchers in the present study hope that establishing such studies will open new horizons to more accurately monitor patients with sepsis and to decrease mortality rate due to such a condition, its lasting effects and the financial toll on the patient and the health systems.
The high mortality rate in the present study shows the importance of the subject of the study. In the present study, unfortunately 46.4% of the subjects (79 patients) finally succumbed to death, the majority of whom suffered from septic shock. As explained in the “Introduction”, one of the most common problems in emergency and ICU centres in hospitals is the incidence of sepsis and its role in patient mortality. Sepsis is one of the main and most important reasons for admissions into ICU centres, which prolongs the stay at ICU and increases morality rate in such centres.11
Several studies have evaluated the mortality rate due to sepsis. Hasibi et al. showed in a 3-year study that the most common reason for mortality is sepsis.12 They reported that more attention should be paid to sepsis and it is necessary for all the hospitals to employ experienced personnel and make available diagnostic and treatment techniques round-the-clock.13 During the past 10 years a large number of studies have been carried out on procalcitonin, especially in ICUs, all of which have attached great importance to procalcitonin, in comparison to CRP, IL8, IL6 and neutrophil counts, in determining the course and prognosis of sepsis and SIRS, by emphasising the fact that it is a rapid and reliable technique to initiate and terminate antibiotic treatment.14,15,16,17 In comparison to the results of the present study, a study by Castell et al. showed a higher serum level of procalcitonin in patients with infection.18 Luzzani et al. reported that a 24-hour follow-up of procalcitonin level, compared to CRP, is better correlated with the severity of infection and organ deficiency.19 A study by Arkader et al. showed that it is possible to differentiate sepsis from SIRS by evaluation of serum levels of procalcitonin, which is not possible by CRP serum levels.20 In addition, Turgul et al. showed that in patient with sepsis, septic shock and SIRS procalcitonin is a more reliable marker compared to CRP for the diagnosis of infection as a reason for systemic inflammatory response.21
Based on what was discussed, in the majority of studies procalcitonin has been compared with CRP and the majority have concluded that procalcitonin is a more appropriate marker to make a distinction between bacterial and non-bacterial reasons for inflammation.18,19,20,21,22 However, some studies have shown that in critically ill patients, such a measurement is not always useful and the values obtained have been less than the levels expected.23,24
Recent research indicates that the protocol of antibiotic therapy based on serial checking of procalcitonin levels can decrease the duration of antibiotic therapy in patients with severe sepsis or septic shock. Based on the results of these studies procalcitonin levels of 0.5−1.1 ng/mL indicate SIRS and values higher than 1.1 ng/mL indicate sepsis.10 In addition, a clinical trial showed that use of procalcitonin marker for administration of antibiotics resulted in a decrease in encounter with antibiotics and duration of antibiotic administration compared to a control group receiving antibiotics based on protocols available.25 In addition, Long et al. showed that use of procalcitonin levels in order to administer antibiotics, decreased use of antibiotics up to 14% at admission, encounter with antibiotics during the whole period up to 45% and duration of treatment up to 2 days.26 Schuetz et al. reported similar findings.27,28,29,30
Five millilitres of blood are necessary in two episodes for a blood culture procedure, which is a great volume in infants. In addition, a delay of 48 hours in the diagnosis and the need for a specific culture media for the majority of microorganisms are other disadvantages of this diagnostic method. In addition, microbial culture technique does not reflect the host inflammatory response and organ disorders.31,32
CONCLUSIONS
It is suggested that to differential diagnosis between sepsis and SIRS due to an infectious disease, procalcitonin levels be used, which is a better marker, for follow-up of treatment and evaluation of response to treatment and decrease in the use of antibiotics without any effects on clinical outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Finfer S, Bellomo R, Lipman J, French C, Dobb G, Myburgh J. Adult-population incidence of severe sepsis in Australian and New Zealand intensive care units. Intensive Care Med. 2004;30:589–96. doi: 10.1007/s00134-004-2157-0. [DOI] [PubMed] [Google Scholar]
- 3.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 4.Padkin A, Goldfrad C, Brady AR, Young D, Black N, Rowan K. Epidemiology of severe sepsis occurring in the first 24 hrs in intensive care units in England, Wales, and Northern Ireland. Crit Care Med. 2003;31:2332–8. doi: 10.1097/01.CCM.0000085141.75513.2B. [DOI] [PubMed] [Google Scholar]
- 5.Jawad I, Luksic I, Rafnsson SB. Assessing available information on the burden of sepsis: Global estimates of incidence, prevalence and mortality. J Glob Health. 2012;2:010404. doi: 10.7189/jogh.02.010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soussy CJ, Carret G, Cavallo JD, Chardon H, Chidiac C, Choutet P, et al. Antibiogram Committee of the French Microbiology Society. Report 2000-2001. Pathol Biol (Paris) 2000;48:832–71. [PubMed] [Google Scholar]
- 7.Brun-Buisson C. The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26(Suppl 1):S64–74. doi: 10.1007/s001340051121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yukioka H, Yoshida G, Kurita S, Kato N. Plasma procalcitonin in sepsis and organ failure. Ann Acad Med Singapore. 2001;30:528–31. [PubMed] [Google Scholar]
- 9.Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W. Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med. 2000;28:950–7. doi: 10.1097/00003246-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Giamarellos-Bourboulis EJ, Giannopoulou P, Grecka P, Voros D, Mandragos K, Giamarellou H. Should procalcitonin be introduced in the diagnostic criteria for the systemic inflammatory response syndrome and sepsis? J Crit Care. 2004;19:152–7. doi: 10.1016/j.jcrc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Hatamabadi HR, Darbandsar Mazandarani P, Abdalvand A, Arhami Dolatabadi A, Amini A, Kariman H, et al. Evaluation of the Acute Physiology and Chronic Health Evaluation III in predicting the prognosis of patients admitted to Emergency Department, in need of intensive care unit. Am J Emerg Med. 2012;30:1141–5. doi: 10.1016/j.ajem.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Enguix A, Rey C, Concha A, Medina A, Coto D, Diéguez MA. Comparison of procalcitonin with C-reactive protein and serum amyloid for the early diagnosis of bacterial sepsis in critically ill neonates and children. Intensive Care Med. 2001;27:211–5. doi: 10.1007/s001340000709. [DOI] [PubMed] [Google Scholar]
- 13.Hasibi M, Soudbakhsh A, Abadi Z. Mortality rate of infectious disease in relation to holidays: Three year study in Imam Khomeini Hospital. Tehran Univ Med J. 2008;65 [Google Scholar]
- 14.Vandenabeele P, Declercq W, Vanhaesebroeck B, Grooten J, Fiers W. Both TNF receptors are required for TNF-mediated induction of apoptosis in PC60 cells. J Immunol. 1995;154:2904–13. [PubMed] [Google Scholar]
- 15.Han YY, Doughty LA, Kofos D, Sasser H, Carcillo JA. Procalcitonin is persistently increased among children with poor outcome from bacterial sepsis. Pediatr Crit Care Med. 2003;4:21–5. doi: 10.1097/00130478-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Casado-Flores J, Blanco-Quirós A, Asensio J, Arranz E, Garrote JA, Nieto M. Serum procalcitonin in children with suspected sepsis: A comparison with C-reactive protein and neutrophil count. Pediatr Crit Care Med. 2003;4:190–5. doi: 10.1097/01.PCC.0000059420.15811.2D. [DOI] [PubMed] [Google Scholar]
- 17.Stryjewski GR, Nylen ES, Bell MJ, Snider RH, Becker KL, Wu A, et al. Interleukin-6, interleukin-8, and a rapid and sensitive assay for calcitonin precursors for the determination of bacterial sepsis in febrile neutropenic children. Pediatr Crit Care Med. 2005;6:129–35. doi: 10.1097/01.PCC.0000149317.15274.48. [DOI] [PubMed] [Google Scholar]
- 18.Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D, Sgarbi L. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care. 2004;8:R234–42. doi: 10.1186/cc2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luzzani A, Polati E, Dorizzi R, Rungatscher A, Pavan R, Merlini A. Comparison of procalcitonin and C-reactive protein as markers of sepsis. Crit Care Med. 2003;31:1737–41. doi: 10.1097/01.CCM.0000063440.19188.ED. [DOI] [PubMed] [Google Scholar]
- 20.Arkader R, Troster EJ, Lopes MR, Júnior RR, Carcillo JA, Leone C, et al. Procalcitonin does discriminate between sepsis and systemic inflammatory response syndrome. Arch Dis Child. 2006;91:117–20. doi: 10.1136/adc.2005.077446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tugrul S, Esent F, Celebi S, Ozcan PE, Akinci O, Cakar N, et al. Reliability of procalcitonin as a severity marker in critically ill patients with inflammatory response. Anaesth Intensive Care. 2002;30:747–54. doi: 10.1177/0310057X0203000605. [DOI] [PubMed] [Google Scholar]
- 22.Suprin E, Camus C, Gacouin A, Le Tulzo Y, Lavoue S, Feuillu A, et al. Procalcitonin: A valuable indicator of infection in a medical ICU? Intensive Care Med. 2000;26:1232–8. doi: 10.1007/s001340000580. [DOI] [PubMed] [Google Scholar]
- 23.Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: Systematic review and meta-analysis. Lancet Infect Dis. 2007;7:210–7. doi: 10.1016/S1473-3099(07)70052-X. [DOI] [PubMed] [Google Scholar]
- 24.Giamarellos-Bourboulis EJ, Mega A, Grecka P, Scarpa N, Koratzanis G, Thomopoulos G, et al. Procalcitonin: A marker to clearly differentiate systemic inflammatory response syndrome and sepsis in the critically ill patient? Intensive Care Med. 2002;28:1351–6. doi: 10.1007/s00134-002-1398-z. [DOI] [PubMed] [Google Scholar]
- 25.Christ-Crain M, Stolz D, Bingisser R, Müller C, Miedinger D, Huber PR, et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: A randomized trial. Am J Respir Crit Care Med. 2006;174:84–93. doi: 10.1164/rccm.200512-1922OC. [DOI] [PubMed] [Google Scholar]
- 26.Long W, Deng X, Zhang Y, Lu G, Xie J, Tang J. Procalcitonin guidance for reduction of antibiotic use in low-risk outpatients with community-acquired pneumonia. Respirology. 2011;16:819–24. doi: 10.1111/j.1440-1843.2011.01978.x. [DOI] [PubMed] [Google Scholar]
- 27.Schuetz P, Albrich W, Christ-Crain M, Chastre J, Mueller B. Procalcitonin for guidance of antibiotic therapy. Expert Rev Anti Infect Ther. 2010;8:575–87. doi: 10.1586/eri.10.25. [DOI] [PubMed] [Google Scholar]
- 28.Schuetz P, Batschwaroff M, Dusemund F, Albrich W, Bürgi U, Maurer M, et al. Effectiveness of a procalcitonin algorithm to guide antibiotic therapy in respiratory tract infections outside of study conditions: A post-study survey. Eur J Clin Microbiol Infect Dis. 2010;29:269–77. doi: 10.1007/s10096-009-0851-0. [DOI] [PubMed] [Google Scholar]
- 29.Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I, et al. ProHOSP Study Group. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: The ProHOSP randomized controlled trial. JAMA. 2009;302:1059–66. doi: 10.1001/jama.2009.1297. [DOI] [PubMed] [Google Scholar]
- 30.Schuetz P, Christ-Crain M, Wolbers M, Schild U, Thomann R, Falconnier C, et al. ProHOSP study group. Procalcitonin guided antibiotic therapy and hospitalization in patients with lower respiratory tract infections: A prospective, multicenter, randomized controlled trial. BMC Health Serv Res. 2007;7:102. doi: 10.1186/1472-6963-7-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alaei V, Salehzadeh F. The clinical manifestations and antibiogram results in children with UTI. J Army Univ Med Sci. 2008;8:274–80. [Google Scholar]
- 32.Worthington T, Lambert PA, Elliott TS. Is hospital-acquired intravascular catheter-related sepsis associated with outbreak strains of coagulase-negative staphylococci? J Hosp Infect. 2000;46:130–4. doi: 10.1053/jhin.2000.0810. [DOI] [PubMed] [Google Scholar]


