Abstract
Background:
Cervical cancer is the second most common cancer among Iranian women and among the few cancers that could be easily diagnosed in the pre-malignant stage. We aimed to assess the status of cervical cancer screening in women referred to health care centres in Tabriz, northwest Iran.
Materials and Methods:
This descriptive-analytical study was done on 441 women referred to health care centres of Tabriz, northwest Iran. The centres were selected using the multi-stage cluster sampling method. The participants were selected from the active records of those centres. A questionnaire regarding the socio-demographic characteristics and cervical cancer screening and reasons for referring or not referring for screening was completed by the participants A P < 0.05 was considered as significant.
Results:
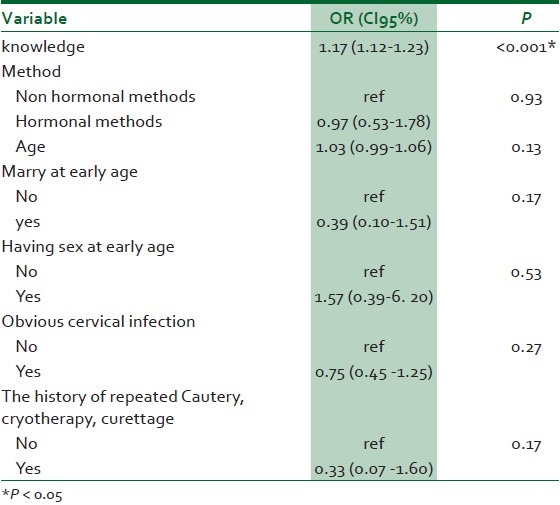
Out of the participants 49.4% of women had done the Pap smear test while 50.6% had never done this test. The main reason why women had not performed cervical cancer screening was being unaware of the importance of it (46.1%). Logistic regression analysis with adjustment showed a significant relationship between screening and awareness scores (OR = 1.17, CI = 95%:1.12-1.23), when the effect of other confounding factors [total awareness scores, risk factors (marriage or having sexual intercourse at a young age, history of obvious cervical infection, cautery, cryotherapy or repeated curettage), age and type of family planning] in screening was controlled.
Conclusion:
Suitable and continuous educational programmes especially for high risk women should be implemented through the health care services. Preparing educational brochures and pamphlets and providing adequate training on the necessity of early referral and marriage counseling could also be effective in improving woman's awareness and performance.
Keywords: Cervical cancer, Pap smear, performance
INTRODUCTION
Cancer, the third leading cause of death and the second most important group of chronic non-communicable diseases, is one of the main challenges faced by Iran's health care system.1 Cancer affects an individual's mind, body, and family leading to a change in the patients' entire lives.2 Cervical cancer is the second most common cancer among Iranian women and the third most common cancer among American women after uterine and ovarian cancers.3 The American Cancer Society (ACS) had predicted that by 2013 about 12340 new cases of invasive cervical cancer would be diagnosed leading to 4030 deaths.4 Based on the statistics provided by the cancer record of the ACS, the prevalence of cervical cancer is 6-7% per 100, 000 women, in the US. Despite international reports on the screening, diagnosis, and treatment of cervical cancer, no clear statistics are available on the incidence, mortality, and morbidity rates of this cancer in Iran because there is no cancer recording system in the country.5
Cervical cancer is a globally important issue in health care and about half a million cases of cervical cancer occur annually.4,6 The risk factors for cervical cancer are sexual intercourse at younger ages, having multiple sexual partners, smoking, history of human papiloma virus (HPV) infection, immune deficiency, multiparity, diet lacking fresh fruits and vegetables, obesity, poverty, frequent contraction of sexually transmitted diseases such as herpes simplex virus (HSV) type-2 infection, exposure to diethylstilbestrol (DES) in utero, history of intraepithelial neoplasia, not frequent use of condoms, familial history of cervical cancer, history of genital wart infection, history of genital wart infection in the partner, repeated curettages, partner with penile cancer, partner's other wife having cervical cancer, low personal hygiene, consumption of oral contraceptives, and history of trauma to the cervix.4,7,8,9
Cervical cancer is among the few cancers that could be easily diagnosed in the pre-malignant stage.10 Dysplasia usually has no clinical sign and its diagnosis is often made based on cytological findings using the Pap smear test. Since dysplasia is a transient stage in the pathology of cervical cancer, its immediate diagnosis is of utmost importance. Dysplasia should be identified in very early stages and treatment should be started.8 The Pap smear test is used for screening disease related to the ectocervix and endocervical canal. Cervical cytology is the most effective and gold standard method for screening cervical cancer.7,10 Invasive cervical cancer is considered as a preventable type of cancer because it has a long pre-invasive phase. Therefore, several years would pass before precancerous lesion resulting from HPV infection or other causes change into invasive cancerous lesion. In the pre-cancerous phase early diagnosis and treatment could prevent invasive cervical cancer.4,7,9 Cytological screening programmes are highly effective in the early diagnosis of this cancer. Based on figures from 2008-2010, the lifetime risk of developing cervical cancer among U.S. women is approximately 1 in 151. Despite organised and frequent screening programs in the United States, 30% of cervical cancers occur in women who have never done the Pap smear test compared to 60% in developing countries.4 Women who were never or infrequently screened had a higher risk of suffering from cervical cancer.9
In the absence of Pap smear test, lesions can also be identified in colposcopy evaluations. However, since all women cannot be referred to clinics for cervical biopsy and colposcopy evaluation and considering that these methods are time consuming, expensive, and need expertise, the Pap smear test has been presented and accepted as a screening method for cervical cancer for women in different societies. Performing the Pap smear test could be an indicator of the fair distribution of health care among various social levels.11 According to the Iranian Ministry of Health and Medical Education, cervical cancer screening should be done for all women after marriage. The 35-54-year-old women are at a higher risk; but, screening is also done 3 years after marriage for married women less than 18 years of age. After three normal and reliable Pap smear samples and no other risk factors, the Pap smear test could be repeated every 3 years.12
Presenting free screening methods for this type of cancer per se cannot prevent invasive cervical lesions. Adequate education regarding these methods should also be presented to women who do not believe they are at risk or are inconsiderate about referring for these tests.13,14 In such situations, suitable counseling methods could change women's attitudes.15 Therefore, awareness about cervical cancer and its screening is very important.10 In Iran, despite the fact that the Pap smear test was done free of charge in health care centres during 1999, only 24% of eligible women in areas covered by Tehran University of Medical Sciences underwent this test.16 Fear of having cervical cancer, pain, and shyness have been reported as the main reasons for not performing this test.17
Despite previous studies on assessing the attitudes, beliefs, and performance of women with cervical cancer, we found no studies on the status of cervical cancer screening according to the step by step protocol of the Ministry of Health and Medical Education. Therefore, we aimed to assess the status of cervical cancer screening and its related factors in women referring to health care centres in Tabriz, northwest Iran in order to take a step forward in improving the quality of services provided for women.
MATERIALS AND METHODS
This was a descriptive-analytical study in which the status of performing Cervical Cancer Screening and its related factors was done on women referred to health care centres in Tabriz, Iran. Inclusion criteria were: women referred to health centres for health care with records, having literacy more than elementary school, interest to attend in research, not being single, and age range of 18-49; and exclusion criteria were: individuals' refusing from participating in study. The study population included all the women referred to health care centres of Tabriz. The sample size estimated 440 people according to the previous study.15
n = z2pq/d2 = 1.96 × 1.96 × 0.6× 0.4/0.0025 = 368.64 = 370 and with considering 20% drop out it is considered 440.
The standardized confidence value was 95%. The amount of acceptable error, d = 0.05, Z = 1.96, P = 0.6
Sampling was done using a multistage cluster sampling method. In the first stage, 25 health care centres or health sub-centres were selected from 65 health centres and stations of Tabriz. In the next stage, based on sample size and the number of active records of every centre, 15-20 records were randomly selected and investigated and after phone call to women with mentioned records and explaining the study objectives, they were invited. Women in reproductive age who were literate, willing, and consented to participate in this study were chosen. The subjects were excluded if they decline to continue with the study. Data collecting tool was a researcher-regulated questionnaire which in order to achieve the study objective, it was designed according to information in guidelines. The questionnaire generally consisted of: questions about cervical cancer screening, reasons for not to perform cervical cancer screening and the factors that had affect on screening of cervical cancer which included socio-demographic characteristics and the history of reproduction, the questions about awareness, knowledge and risk factor questions related to cervical cancer. The awareness had 24 questions. According to the answers, a respondent scores 1 for right answers and scores 0 for wrong or unknown ones. So the total minimum score was 0 and the maximum was 24. Finally, each question and the mean of awareness score compared with chi-square and t-test in two groups.
A total of 10 faculty members evaluated the questionnaire and corrections were made to the questionnaires according to the feedbacks. Test and re-test were implemented on 30 subjects to determine the reliability (intraclass correlation coefficient, ICC) and internal consistency (Cronbach'sαcoefficient). ICC (CI: 95%) and Cronbach's α were 0.82 (0.74-0.88) and 0.8 respectively.
Required permission was taken from the ethical committee of Tabriz University of Medical Sciences.
The questionnaire was completed by subjects after the researcher introduced the study objectives in an appropriate place. Before data collection, ethical satisfaction form was given to the participants and written consent also was received and voluntariness and confidentiality of the information were emphasized. Descriptive statistics were used to examine the frequency distribution and mean of data and inferential statistics including chi-square and Fisher's exact test and t-test were used to achieve the research queries. The obtained data were analyzed through SPSS 13.
This study was approved by the Research Committee of Tabriz University of Medical Sciences (code: 5.4.9290).
RESULTS
Of the 441 participants, 218 (49.4%) women had done the Pap smear test while 223 (50.6%) had never done this test.
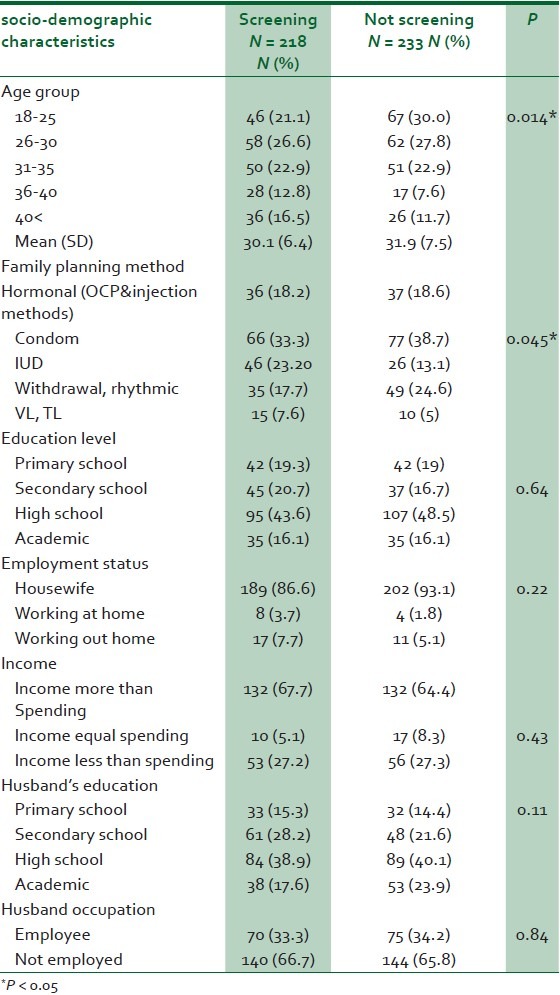
The socio-demographic characteristics of the participants are presented in Table 1. The mean (SD) age of people who had done the test was significantly lower than women who had not done the test. Regarding the family planning method, most women who had taken the test used condoms, and then IUD while women who had not taken the test used condoms and then withdrawal. We found no significant difference between the two groups with respect to educational status, occupation, income, and partner's education status and occupation [Table 1].
Table 1.
The association of socio-demographic characteristics with performing screening methods:
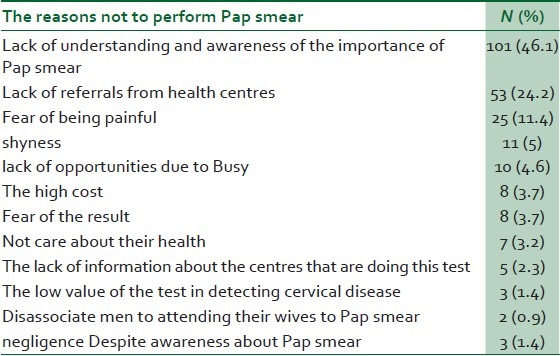
The mean (SD) age for the first Pap smear was 25.21 (5.5) years. Only 38.3% of the women frequently referred for testing. The referral interval for testing was more than 3 years and on the 5-10 menstruation days for most participants. The mean (SD) number of Pap smear test was 2.05 (1.5) times and the mean (SD) time between the start of sexual relationship to doing the test was 5.2 (5.7) years [Table 2]. The most common reason for not doing the test was that the respondents did not know the importance of testing (46.1%) [Table 3].
Table 2.
The status of the screening in women performing Pap smear
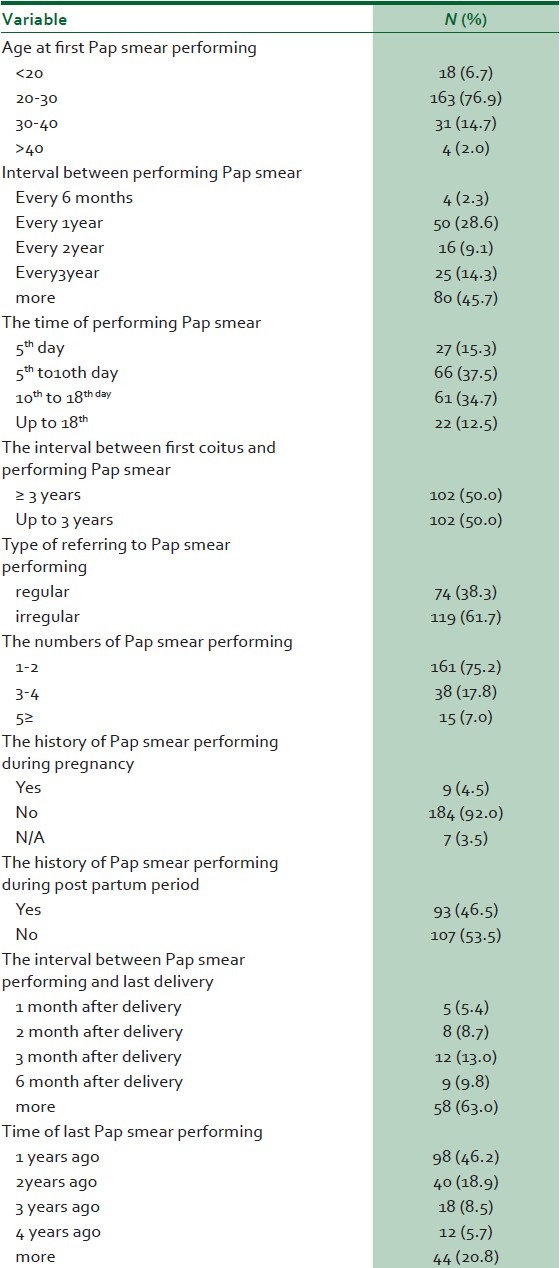
Table 3.
The reasons not to perform Pap smear
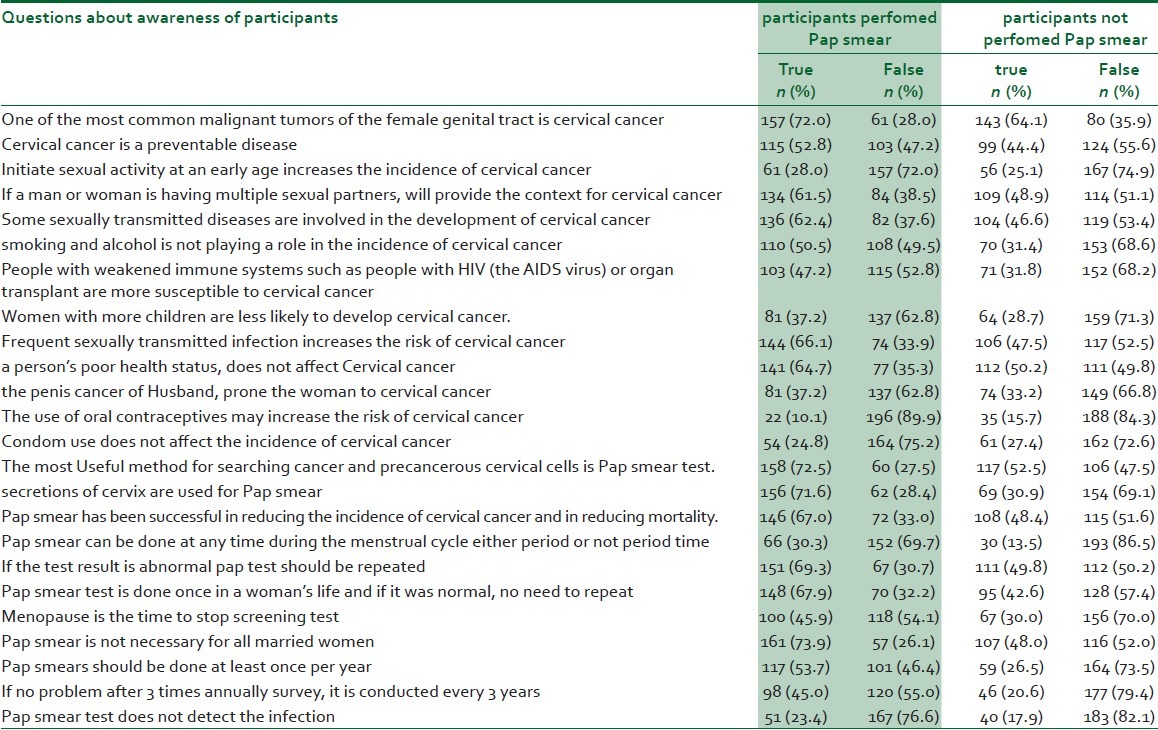
We found a statistically significant correlation between cervical cancer screening and mean awareness scores between women who had not taken the test 8.75 (4.9) and those who had 12.39 (4.8) (P < 0.001). We found a significant difference between the two groups in the 24 questions related to awareness, except for questions 1, 2, 3, 13, and 24 (P < 0.05) [Table 4].
Table 4.
Awareness of the participants regarding cervical cancer screening (Pap smear)
Among the various mentioned risk factors for cervical cancer, a significant difference was seen between the two groups with respect to marriage or having sexual intercourse at a young age, history of obvious cervical infection, cautery, cryotherapy or, repeated curettage.
Logistic regression analysis with adjustment showed a significant relationship between screening and awareness scores (OR = 1.17, CI = 95%: 1.12-1.23), when the effect of confounding factors (total awareness scores, the four mentioned risk factors, age, and type of family planning) in screening was controlled [Table 5]. Hence, as the women became more aware, their performance enhanced.
Table 5.
The prediction value of different factors for doing cervical cancer screening
We also found that in women who had done the test, the most important source of information (48%) were the health care personnel. Others were mass media (21.6%), office of physicians (15.2%), friends (5.6%), seminars and conferences (5.6%), and books (3%) were other sources of information, respectively.
DISCUSSION
In this study, 218 (49.4%) women had done the Pap smear test while 223 (50.6%) had never done this test. In another study in Iran, 41.6% of women had done the test once in their lives.15 This is while other studies in other countries have reported a rate of 85%18 and 93%.19 Therefore, it seems that the awareness and performance of Iranian women is weaker.
The referral interval for taking the test was 3 years in most women (45.7%) with a mean (SD) of 3.7 (1.3) years. Fitzhugh and colleagues found a mean of 1.8 year in their study.20 Barroso and co-workers reported that 39% of women referred for testing every 6 months and 34.5% of women referred for testing annually.21 The results of these studies are not consistent with ours. According to the guidelines of managed care (no.33) issued by the Ministry of Health and Medical Education, after 3 normal and reliable Pap smear samples and no other risk factors, the Pap smear test could be repeated every 3 years.12 Therefore, it can be concluded that the intervals for doing Pap smear tests in the studied population is not desirable. This inconsistency could be attributed to the individual's lack of awareness, incorrect culture, and the indifference of the health care personnel in educating and guiding women to take Pap smear tests. Therefore, it should be taken into account that the awareness of the health care personnel regarding the necessity of screening should be increased in order to be able to guide and recommend taking the test to women. The time of screening for most women (37.5%) was day 5-10 of menstruation. According to the guidelines of managed care (no.33), the best time for taking Pap smear samples is about 2 weeks after the first menstruation day (days 10-18 of the menstruation cycle).12
The mean interval for taking the Pap smear test from the start of sexual relationship was more than 5 years among our participants. According to the guidelines for managed care, screening begins in all women after marriage. Of course, in married women who are 18-years-old or younger, screening should be done 3 years after marriage.
The most prevalence reason for referring for Pap smear testing was recommendation by physicians and the healthcare team (49.5%). In another study in Iran the most important reasons for referral were signs of disease (31.8%) and recommendations made by healthcare personnel (29.5%).22 Therefore, it seems that the encouragement of the health care team was better in our study.
We found that most of the participants (46.1%) were not aware of the importance of being screened. However, other studies have shown that the most important reasons for not being screened were having no sign of disease (50.5%) and lack of awareness (37.7%).22 Another study also confirmed that lack of knowledge about the importance of screening was the most frequent reason for not being screened.23 On the other hand, lack of recommendation by nurses and physicians24 and shame25 were the most important reasons for not being screened in other related studies. All the mentioned studies directly or indirectly confirm that the level of awareness regarding the importance of screening should be raised among women.
In this study women who had been screened had a significantly higher awareness score. This finding was consistent with another similar study on an Iranian population.23 Moreover, another study showed that women who had higher awareness scores had been screened at least once in their lives.26 As awareness on the importance of screening rose, the woman's performance increased almost uniformly.15 Therefore, considering the consistent findings in this regard, preparing suitable educational programmes on cervical cancer screening seems necessary for improving awareness in this regard.
Consistent with Chang's study,26 we found that health care personnel were the most important source of information regarding cervical cancer screening. Baghiani-Moghadam concluded that physicians are the most effective sources of information on Pap smear testing.22 The cause of this inconsistency could be because health care personnel in Tabriz received better training that those in Yazd. Moreover, it should be noted that our study was done on women referring to health care centres and therefore, it is logical that they would get information from the health care personnel.
We found a significant relationship between cervical cancer screening and age and type of family planning; so that most of the women who referred for screening were 26-30 years old. Also, people who used IUD took Pap smear tests more frequently.
In one study age, education, and place of residence had a significant effect on the women's performance.15 Another study showed that education and marital status were significant factors for taking Pap smear tests.9 However, in a study done in Iran, no significant relationship was found between performance, marital status, type of contraception, and age of marriage.23 It seems that higher education level increases woman's performance in taking Pap smear tests by increasing their awareness; although we did not find a significant relationship between education level and screening. Among the family planning methods, people who used IUD and surgical techniques referred for screening more than women who used other techniques. There are several reasons for higher screening rates in women who have IUDs. Women are advised to take a Pap smear test before placing the IUD and during periodic examinations by midwives. Also, in forms related to the family planning method that health care personnel should complete before placing IUDs, there is an item where women should state the time of their last screening date. If a long time has passed they are advised to be screened. Among the various risk factors for cervical cancer, a significant difference was seen between the two groups with respect to marriage or having sexual intercourse at a young age, history of obvious cervical cancer, cautery, cryotherapy or repeated curettage. Consistently, another study showed that pregnancy before the age of 20, beginning sexual intercourse before the age of 16, using oral contraceptives for 5 years, and smoking were the main risk factors for cervical cancer.23 In another study, about 53% of the studied women were passive smokers. Since the participants in our study were selected from married individuals, we could not evaluate the relationship between marital status and taking the Pap smear test. Another restriction of this study was including literate women to complete the questionnaire.
CONCLUSION
The frequency of performing cervical cancer screening was not desirable in our study. Therefore, suitable and continuous educational programmes should be implemented through the mass media. Preparing educational brochures and pamphlets and providing adequate training on the necessity of early referral and marriage counseling could also be effective in improving woman's awareness and performance. The role of health care personnel as important and reliable sources of information for women should also be taken into account. Reducing the cost of screening by policy makers can also help in the proper screening of all women regardless of their socio-demographic status. Other multi-centre studies should be performed to confidently generalize the findings of this study. We also suggest performing further studies on the status of cervical cancer screening in single women and those with dysplasia, as well as to assess the role of training on the rate of referral for cervical cancer screening.
ACKNOWLEDGEMENTS
We would like to thank the Student Research Committee of Tabriz University of Medical Sciences for their financial support. Also, we would like to thank the participants and all the personnel of the healthcare centres of Tabriz who helped us during this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Nasrabadi AN, Bahabadi AH, Hashemi F, Valiee S, Seif H. Views of Iranian patients on life with cancer: A phenomenological study. Nurs Health Sci. 2011;13:216–20. doi: 10.1111/j.1442-2018.2011.00604.x. [DOI] [PubMed] [Google Scholar]
- 2.Spiegel D. Mind matters in cancer survival. Psychooncology. 2012;21:588–93. doi: 10.1002/pon.3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Health and Medical Education, Non-communicable disease, cervical cancer. 2012. [Last accessed on 2014 Jun 11]. available from: http://iec.behdasht.gov.ir/index.aspx?fkeyid=&siteid=143&pageid=29375&siteid=143 .
- 4.The American Cancer Society. What are the key statistics about cervical cancer? [Last accessed on 2013 Nov 4]. Available from: http://www.cancer.org/Cancer/CervicalCancer/DetailedGuide/cervicalcancerkey-statistics/2013 .
- 5.Behtash N, Karimizarchi M. Cervical cancer: The preventive role of HPV vaccine. Tehran Univ Med J. 2007;64:1–8. [Google Scholar]
- 6.Shepherd JH, Milliken DA. Conservative surgery for carcinoma of the cervix. Clin Oncol (R Coll Radiol) 2008;20:395–400. doi: 10.1016/j.clon.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Guideline for Screening for Cervical Cancer. Approved By The Guideline Group On Cervical Cancer Screening. 2009 [Google Scholar]
- 8.Centers for Disease Control and Prevention. Gynecologic Cancers: Cervical cancer risk factors. [Last accessed on 2013 Sept 3]. Available from: http://www.cdc.gov/cancer/cervical/basic_info/risk_factors.htm .
- 9.Nelson W, Moser R, Gaffeg A, Waldron W. Adherence to cervical cancer screening, guideline for U.S. women aged 25-64: data from the 2005 Health Information National Trends Survey (HINTS) J Women's Health (Larchmt) 2009;11:1759–65. doi: 10.1089/jwh.2009.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright TC, Jr, Cox JT, Massad LS, Twiggs LB, Wilkinson EJ. ASCCP-Sponsored Consensus Conference. 2001 Consensus Guidelines for management of women with cervical cytological abnormality. JAMA. 2004;287:2120–9. doi: 10.1001/jama.287.16.2120. [DOI] [PubMed] [Google Scholar]
- 11.Giard RW, Blok P. Cervical smears unsuitable for exclusion of cervical carcinoma. Ned Tijdschr Geneeskd. 2000;144:86–7. [PubMed] [Google Scholar]
- 12.Instruction of managed care's, number (33) Guidance for Pap Smear. Tehran: Ministry of Health and Medical Education; 2004. [Last accessed on 2014 Jun 11]. Ministry of Health and Medical Education. Available from: http://darman.kaums.ac.ir/Default.aspx?PageID=86 . [Google Scholar]
- 13.Hilton LW, Jennings-Dozier K, Bradley PK, Lockwood-Rayermann S, DeJesus Y, Stephens DL, et al. The role of nursing in cervical cancer prevention and treatment. Cancer. 2003;98(9 Sippl):2070–4. doi: 10.1002/cncr.11677. [DOI] [PubMed] [Google Scholar]
- 14.Sancho-Garnier H, Khazraji YC, Cherif MH, Mahnane A, Hsairi M, El Shalakamy A, et al. Overview of cervical cancer screening practices in the extended Middle East and North Africa countries. Vaccine. 2013;31(Suppl 6):G51–7. doi: 10.1016/j.vaccine.2012.06.046. [DOI] [PubMed] [Google Scholar]
- 15.Ramezani-Tehrani F, Mohammad K, Rahgozar M, Naghavi M. Knowledge and practice of Iranian women toward cervical cancer. J Reprod Infertility. 2000;2:50–6. [Google Scholar]
- 16.Eslamshahr region reported reproductive health, Department of medical and health sciences. Tehran: 2000. [Google Scholar]
- 17.Percac-Lima S, Aldrich LS, Gamba GB, Bearse AM, Atlas SJ. Barriers to follow-up of an abnormal Pap smear in Latina women referred for colposcopy. J Gen Intern Med. 2010;25:1198–204. doi: 10.1007/s11606-010-1450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Randolph WM, Freeman DH, Jr, Freeman JL. Pap smear use in a population of older Mexican-American women. Women Health. 2002;36:21–31. doi: 10.1300/J013v36n01_02. [DOI] [PubMed] [Google Scholar]
- 19.Solomon D, Breen N, McNeel T. Cervical cancer screening rates in the United States and the potential impact of implementation of screening guidelines. CA Cancer J Clin. 2007;57:105–11. doi: 10.3322/canjclin.57.2.105. [DOI] [PubMed] [Google Scholar]
- 20.Fizhugh VA, Heller DS. Improved awareness of Pap smear may not affect its use in Nigeria. J Low Genit Tract Dis. 2009:852–4. [Google Scholar]
- 21.Barroso MF, Gomes KR, Andrade JX. Frequency of Pap smear testing in young women with an obstetric history in Teresina, Piauí, Brazil. Rev Panam Salud Publica. 2011;29:162–8. [PubMed] [Google Scholar]
- 22.Baghyanimoghaddam M. Survey on knowledge, attitude and practice of 15-49 years age group married women related to Pap smear test in Yazd city in 2001. J Mazandaran Univ Med Sci. 2003;13:79–87. [Google Scholar]
- 23.Bahmanjanbeh F. Survey on knowledge, attitude and practice of women occupied in Islamic Azad University of Tabriz related to screening test of cervical cancer, [MSc Thesis] Tabriz: School of Nursing and Midwifery, Tabriz University of Medical Sciences; 1997. [Google Scholar]
- 24.Lartey M, Goubert G, Cronje HS. Knowledge, attitudes and practices of rural women in south Africa regarding the Pap smear. Int J Gynaecol Obstet. 2003;83:315–6. doi: 10.1016/s0020-7292(03)00295-9. [DOI] [PubMed] [Google Scholar]
- 25.Yakhforushha A, Solhi M, EbadiFardAzar F. Effects of education via health belief model on knowledge and attitude of voluntary health workers regarding Pap smear in urban centers of Qazvin. J Nurs Midwifery Shahid BeheshtiUniv Med Sci. 2008;18:25–30. [Google Scholar]
- 26.Chang CC, Tseng CJ, Liu WW, Jain S, Horng SG, Soong YK, et al. Clinical evaluation of a new model of self-obtained method for the assessment of genital human papilloma virus infection in an underserved population. Chang Gung Med J. 2002;25:664–71. [PubMed] [Google Scholar]


