Abstract
Background:
To utilise an autopsy-based approach to study the febrile deaths and deaths due to malaria during monsoon period of three years at a tertiary care teaching hospital in Mumbai, India.
Materials and Methods:
All autopsies done at the hospital during monsoon period from 2005 to 2007 when fever was the main presenting symptom were included in the study. Monsoon period was defined from June to September. A study on the duration of hospital stay of malaria deaths was also attempted.
Results:
There were 202 autopsies of febrile illness during the study period. Malaria resulted in 20.8% of the deaths besides other causes. A majority of deaths had intrapulmonary haemorrhages as the only pathological finding. Incidence of malaria deaths was more during monsoon period than the non-monsoon period. Plasmodium falciparum was the most common species responsible for malaria deaths while cerebral malaria was the most common mode of death. In 27% of the cases, post-mortem examination helped to arrive at the correct final diagnosis. In 88.1% of the cases, malaria deaths occurred within the first 24 hours of admission to the hospital.
Conclusion:
The study reiterates the fact that malaria remains a preventable but major cause of death in India, predominantly during the monsoon period. The study also emphasises the importance of developing treatment protocols for malaria during such crucial times besides reinforcing the existing preventive measures.
Keywords: Autopsy, cerebral malaria, death, fever, malaria, monsoon rains
INTRODUCTION
Malaria is amongst the leading causes of morbidity and socioeconomic burden in the world along with diseases such as diarrhoea, HIV/AIDS, tuberculosis, measles, hepatitis B and pneumonia.1,2 Around 36% of world's population in 90 countries in tropical and sub-tropical regions is exposed to risk of contracting malaria.3 According to World Health Organisation, 300-500 million cases of malaria occur every year, of which Africa accounts for 90% of the cases.4,5 Annual mortality from malaria is estimated to range from 700,000 to 2.7 million, with more than 75% being African children and expectant mothers.5 In South East Asia, India contributed to 73% of all the reported cases of malaria and 28% of all reported deaths in 2007.3 Ecological diversity, multi-ethnicity and financial variability in India complicates the epidemiology of malaria.3,6 The incidence of malaria increases in monsoon season, which is attributable to favourable breeding environment for mosquitoes.7,8 Monsoon (rainy season) in western India (including Mumbai where the study was performed) extends from June to September and is accompanied by heavy rainfall along with water logging and flooding, especially in low-lying parts of many cities.7,9 Flooding and water logging with stagnation leads to an increased incidence of diseases associated with them, malaria being the foremost, not only claiming many lives but also reducing productive man hours.7,9 Some recent studies have reported gradual decrease in the cases of deaths due to malaria in India, others claim that the true incidence of malaria and deaths due to malaria are grossly under reported.10,11 According to a reputed national newspaper, 237 deaths were reported from Mumbai from 2005 to 2007 due to malaria (http://www.thehindubusinessline.in/2007/06/27/stories/2007062701422100.htm). Studies pertaining to malaria are predominantly ante-mortem in nature, including verbal autopsies and studies taking into account the malaria cases reporting for treatment. However, in the present study, a prospective post-mortem autopsy-based approach was utilised to determine the causes of febrile deaths, with an emphasis on deaths in patients with malaria who succumbed to febrile illness during monsoon rains.
MATERIALS AND METHODS
This was a hospital-based prospective study of patients who were admitted to the hospital in Mumbai on account of fever during monsoon period over a period of three years from 2005 to 2007, after an ethical approval from the institutional review board and an informed consent. Monsoon period for the study was defined from June to September of every year, which corresponded with heavy rainfall.
The study involved the examination of ante-mortem haemogram, liver function test, renal function test, peripheral blood smear examination for parasites and blood culture results. Immediate post-mortem blood samples and splenic imprints were examined for the presence of parasites and malarial pigments. Tissues from brain, heart, lungs, liver, gastrointestinal tract, spleen, kidney, urinary bladder and gall bladder were preserved in formalin and subjected to histopathological examination after staining with haematoxylin and eosin stain and additional pearl's stain, Masson's trichrome and reticulin stain when indicated. Malaria was diagnosed if the ring, schizonts and/or gametocytes of the malaria parasite were identified either in the antemortem or in the post-mortem peripheral blood smears or by the presence of malaria pigment in the splenic imprint or in the tissues collected for histopathological examination. Post-mortem examination was also performed to elucidate the possible mode of death in these cases. Immunological tests to identify the malaria antigen were not performed due to their non-availability in the hospital. All findings were conglomerated to reach the final diagnosis. All autopsies were performed by two pathologists, and the histopathology slides for each case were reviewed independently by two histopathologists to reach a final cause of death. Cases where there was a discrepancy between the histopathologists, the final diagnosis was given after mutual discussion and agreement. Chi square test and calculation of percentages were the only statistical tools applied for data analysis.
RESULTS
During the study period of three years, the hospital recorded 5,676 deaths of patients who died after admission to hospital due to some disease process. Of these, 1,074 deaths had autopsy giving an autopsy rate of 18.9%. A total of 464 autopsies were performed during the monsoon period, of which 202 autopsies (43.6%) had fever as the main presenting symptom [Table 1].
Table 1.
Autopsy statistics for the study period from 2005 to 2007
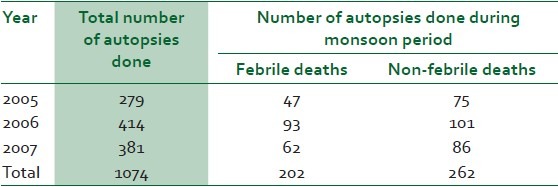
In the study population of 202 autopsies, 78.7% were male while 21.3% were female cases with a male to female ratio of 3.7:1. The age of these cases ranged from 2 months to 73 years with a median age of 31 years. Cases belonging to 21-40 years, which comprises the main economically productive population of any community, accounted for the maximum number of deaths [Figure 1].
Figure 1.
Age distribution of the autopsy cases of febrile deaths during monsoon season from 2005 to 2007
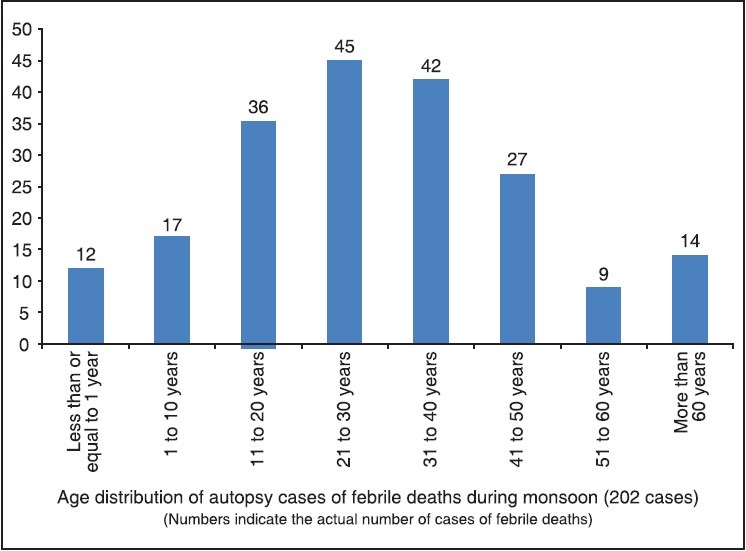
The various cause of deaths observed during the monsoon season are depicted in Figure 2. Malaria accounted for 42 deaths; in a significant proportion of deaths, the main pathological findings were only intra pulmonary haemorrhages, and thus were grouped together as a single entity. This group could not be classified further due to resource constraints.
Figure 2.
Distribution of the cause of death in the autopsy cases of febrile deaths during monsoon season from 2005 to 2007
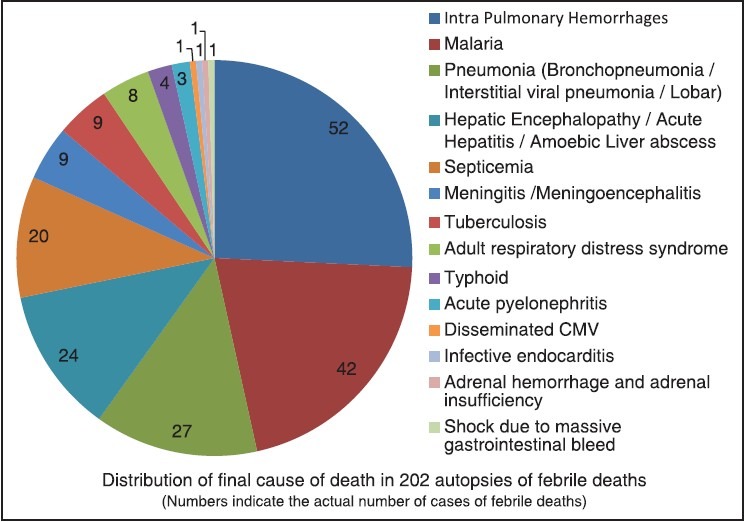
A comparison of malaria deaths during monsoon period and non-monsoon period of the study was done. Malaria was responsible for 20.8% of the deaths during the monsoon period of the study, while only 2.3% of the deaths occurred due to malaria in the non-monsoon period. The occurrence of deaths due to malaria during monsoon had a P value of <0.0001 compared to those in the non-monsoon period [Table 2]. Of the 42 deaths due to malaria, 78.6% were males and 21.4% were females with a male to female ratio of 3.7:1.
Table 2.
Comparison of malaria deaths during monsoon and non monsoon periods
Cerebral malaria was the commonest mode of death in our study accounting for 47.6% of the deaths. Other modes of death included multi-organ failure, acute renal failure, liver cell failure with or without necrosis, lobar pneumonia, hepatorenal failure, myocarditis, encephalopathy, cerebral haemorrhage and severe anaemia. One case had acute pyogenic meningitis in association with peripheral parasitaemia [Figure 3].
Figure 3.
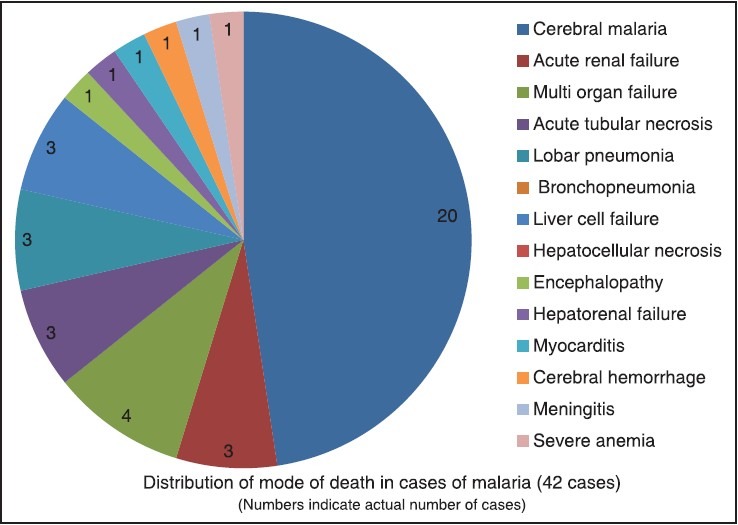
Distribution of the mode of death in malaria cases during monsoon season from 2005 to 2007
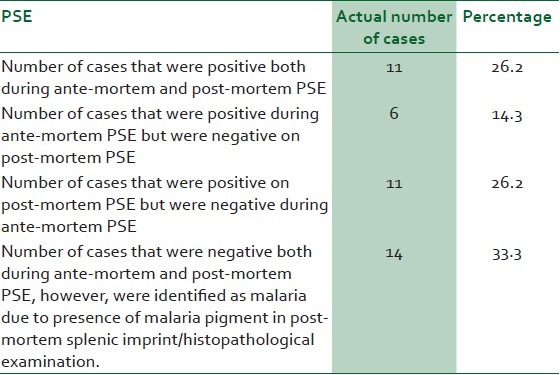
The ante-mortem and post-mortem slide positivity for malaria parasite is summarised in Table 3. In 26.2% of the cases, both ante-mortem and post-mortem peripheral smear examination were positive, while in 26.2% cases, peripheral blood smears were negative ante-mortem but were found to be positive on post-mortem smear examination. In 14.3% of the cases, ante-mortem smear was positive but it was negative on post-mortem examination. The diagnosis of malaria in these cases was confirmed by histopathological examination. All these cases were given anti malaria treatment in the ante-mortem period, which could have been the reason for smear negativity during post-mortem smear examination.
Table 3.
Peripheral smear examination (PSE) of deaths due to malaria
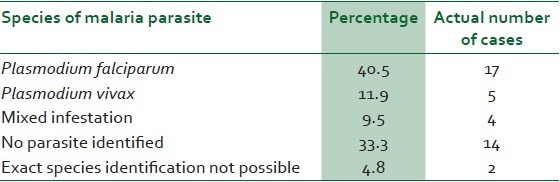
The distribution of species of malaria parasite in these 42 malaria cases is shown in Table 4. Mixed infestation by both Plasmodium falciparum and Plasmodium vivax was seen in 9.5% of these cases, while no parasite could be identified in 38% of the malaria deaths. In two cases, the exact identification of species of malaria parasite was not possible due to low index of infestation and poor morphology. In 22 cases of the total 202 cases of febrile deaths during monsoon of the study period, malaria parasite could be identified during the post-mortem peripheral smear examination. A post-mortem slide positivity rate of 10.89% was observed.
Table 4.
Distribution of infestation patterns of malaria parasite (42 cases of malaria)
A review of the total hospital stay of these malaria deaths revealed that 88.1% of deaths occurred within the first 24 hours of admission, indicating the short time in which a clinician has to salvage such cases, that too in a situation where the number of such cases is rising.
DISCUSSION
In South-East Asian region, India accounts for the largest population being exposed to the risk of malaria.3 In India of the 29 states, Orissa accounted for 25% of cases of malaria while Maharashtra contributes to 2% of the total malaria burden in 2004.3,9 A total of 1144 malaria deaths were reported from India in 2009.
Inadequate drainage systems, water logging and stagnation provide an ideal place for breeding of mosquitoes.7 This problem is exacerbated by monsoon rains. Solanki et al. in their study observed that the incidence of malaria steadily rose from zero to 1.2% from January to July, which further increased to 13.3% in August, doubled (26.1%) in September and then almost tripled (36.8%) in October. In November, it dropped to 18.1%. This was in accordance with monsoon which arrives in India by June and remains till September.12 Gupta et al. in their study of malaria in the New Delhi region of India showed that 53% of the malaria cases occurred in the monsoon period followed by post monsoon period which accounted for 29% of the total cases.13 Muddaiah et al., over a period of 3 years, found a steady increase of malaria cases from June to September in their outpatient department as well as in their inpatients. This coincides with monsoon rains in India.14 Increased incidence of malaria during monsoon seasons have been supported by other authors as well.8,15 In the present study also, the number of deaths due to malaria were more during the monsoon rains than during the non-monsoon period of the year.
Whereas ante-mortem data on malaria is in plenty, studies discussing malaria death are limited. Muddaiah et al. in a series of 314 malaria cases (studied on both outpatient and inpatient basis) had 255 (80.5%) males and 59 (19.5%) females with a male to female ratio of 4.3:1. About 55.7% of the patients were between 21 to 40 years of age; however, only 2 patients died due to malaria in their study.14 Solanki et al. in their study reported a maximum number of deaths in the age group of 21-30 years (35.9%). Male to female ratio was 1.22:1, with male preponderance.12 Desai et al. in a study of 50 cases of malaria found 47 deaths in males and 3 deaths in females.15 In India, the states of Assam,9,16,17 Arunachal Pradesh and Rajasthan are reported to have a higher incidence of malaria in children as compared to adults while the situation looks reversed in the Indo-Gangetic plains.18,19,20 However, in our study, deaths due to malaria were more frequent in males than in females, with a sex ratio of 3.7:1.
Cerebral malaria is reported to be the most common mode of death in cases of malaria.3 Cerebral malaria is histopathologically characterised by the presence of engorged cerebral capillaries and venules with parasitised and non-parasitised red blood cells. On post-mortem examination, the brain appears swollen and its cut surface appears slate gray and may show petechiae. Microscopy may show presence of Durċk's granulomas.21,22 In our study also, cerebral malaria was the most common mode of death, accounting for 47.6% of malaria deaths. Desai et al. in their study of 50 cases of malaria due to P. falciparum reported 44 deaths due to cerebral malaria while in north western Tanzania; Kaatano et al. found cerebral malaria to account for 18.9% of malaria deaths.15,23 Though Muddaiah et al. reported hepatopathy to be the most common complication of malaria in a study of 314 patients, cerebral malaria accounted for all the deaths in their study while Rane et al. reported cerebral malaria to account for 48% of malaria deaths.14,24 Shukla et al. in their study of malaria in Jabalpur city of Madhya Pradesh reported an incidence of 8.5% of cerebral malaria and 25.6% of their cases with cerebral malaria died.25 Besides cerebral malaria, multi-organ failure, acute renal failure, liver cell failure with or without necrosis, extensive pulmonary oedema, hepatorenal failure, myocarditis, cerebral haemorrhage and severe anaemia were the other modes of death encountered in our study, as has also been reported in literature.3,14,21
Data from the India's National Vector Borne Disease Control Program (NVBDCP) show that in the national capital Delhi, 668,761 blood slides were examined for malaria parasite in 2007 and only 182 slides were positive.13 Kar et al. in their epidemiological study from Haridwar, a city in India, showed an increase in the slide positivity rate (SPR) from 0.23% to 11.4% after 1998.26 In a hospital-based study of 448 cases of febrile illness in the Ratnagiri district of Maharashtra, Mishra et al. reported a SPR of 9.82.27 Slide positivity rates in India from few states have been reported to range from 4.7 to 12.6, thus indicating the under reporting of malaria cases at the national level.3 In the study presented, a post-mortem SPR of 10.89% was observed, emphasizing the importance of evaluating a post-mortem peripheral smear in febrile deaths of unknown cause. In spite of extensive literature search, no reference regarding post-mortem smear positivity was found.
State Vector Borne Disease Control Program of Madhya Pradesh, a part of NVBDCP, reported a gradual decrease in the number of malaria cases over a span of 10 years from 1996 to 2007. There was also a gradual decrease in the number of cases due to P. vivax; however, there was an upward trend for malaria cases due to P. falciparum in the non-Enhanced Malaria Control Program regions (EMCP). In EMCP regions, the number of cases due to P. vivax remained almost constant, while the percentage of cases due to P. falciparum increased from 32.7% in 1996 to 62.2% in 2007.28 A similar trend of increasing incidence of malaria due to P. falciparum and a falling trend of malaria due to P. vivax has also been reported by Kar et al.26 Kumar et al. in their study of the burden of malaria in India reported a 50% rise of P. falciparum infestation in India. They also found that the proportion of P. vivax and P. falciparum varies widely in different parts of the country with areas such as in Indo-Gangetic plains and northern hilly states prevalence of P. falciparum is less than 10% while in forested areas the proportion is reversed, with P. falciparum accounting for most of the cases of malaria.3 P. falciparum-positive cases have been reported by other authors ranging from 59.1% to 71.6%.3,12,15,27 In our study as well, P. falciparum was responsible for 40.5% of deaths due to malaria. A rising trend of malaria due to P. falciparum is evident. However, in a study at a secondary care level hospital in Northern India, Anand et al. found 85.4% cases positive for P. vivax and 14.6% positive for P. falciparum.29 In a study of 680 patients of malaria by Limaye et al., P. falciparum accounted for 30% of the cases while P. vivax was responsible for 50% cases, the remaining were mixed infestations.7
In the present study, we found that 88.1% of deaths due to malaria occurred within the first 24 hours of hospital admission, giving very less time for intervention to the treating physician. This emphasises the importance of keeping malaria as a crucial differential diagnosis and developing and instituting protocols for upfront anti-malaria therapy, depending upon the regional sensitivity patterns, especially during monsoon periods. To the best of our knowledge, duration of hospital stay before death due to malaria has never been studied.
The study emphasises the need for community-based approaches for reducing the deaths due to malaria and other diseases associated with monsoon. Most important of these include steps to improve drainage system to prevent water logging and breeding of mosquitoes. Methods such as consistent use of mosquito nets with or without impregnated with pesticides, mosquito repellent coils and creams should also be encouraged.30 Proper communication between the healthcare providers at the grass root level and the community needs to be strengthened. Provision and use of antigen-based rapid card test for detection of malaria and formulation of anti-malaria treatment protocols depending upon the sensitivity patterns of malaria parasite in the local region needs to be promoted so that such a protocol may be initiated on the slightest suspicion of malaria, especially during monsoon.31
Various aetiologies have been implicated as a cause for intrapulmonary haemorrhages including vasculitides, infections (leptospirosis, CMV, invasive aspergillosis, tuberculosis), collagen vascular diseases, diffuse alveolar damage etc.32 However, in the present study, in spite of thorough histomorphological examination and due to resource constraints the group, intrapulmonary haemorrhages could not be further categorised. Few of the deaths due to febrile illnesses could not be included in the study due to lack of the consent from the relatives of the deceased. This being a tertiary level hospital-based autopsy study, the incidence of deaths due to malaria and other causes may be slightly higher than that in the community and may also be considered as a limitation of the study.
It can be concluded from the study that malaria remains a very important disease responsible for deaths in India, especially during monsoon periods. The disease predominantly affects the economically productive population of the country, leading to socioeconomic losses. The study substantiates the reports of an increase in P. falciparum cases, while cerebral malaria being the most common mode of death. An important aspect of the study was the documentation of the short duration of hospital stay of patients who died of malaria. Availability of bedside rapid antigen-based card tests to detect the presence of malaria antigen would help in diagnosis and management of such patients, and this is highly recommended. Besides the above facts, the usefulness of autopsy and post-mortem peripheral smear examination in arriving at a correct diagnosis cannot be underestimated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Murray CJ, Lopez AD. Evidence-based health policy - lessons from the Global Burden of Disease Study. Science. 1996;274:740–3. doi: 10.1126/science.274.5288.740. [DOI] [PubMed] [Google Scholar]
- 2.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 3.Kumar A, Valecha N, Jain T, Dash AP. Burden of malaria in India: Retrospective and prospective view. Am J Trop Med Hyg. 2007;77(6 Suppl):69–78. [PubMed] [Google Scholar]
- 4.Breman JG. The ears of the hippopotamus: Manifestations, determinants, and estimates of the malaria burden. Am J Trop Med Hyg. 2001;64(1-2 Suppl):1–11. doi: 10.4269/ajtmh.2001.64.1. [DOI] [PubMed] [Google Scholar]
- 5.Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 2005;434:214–7. doi: 10.1038/nature03342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Das A, Anvikar AR, Cator LJ, Dhiman RC, Eapen A, Mishra N, et al. Malaria in India: The center for the study of complex malaria in India. Acta Trop. 2012;121:267–73. doi: 10.1016/j.actatropica.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Limaye CS, Londhey VA, Nabar ST. The study of complications of vivax malaria in comparison with falciparum malaria in Mumbai. J Assoc Physicians India. 2012;60:15–8. [PubMed] [Google Scholar]
- 8.Laneri K, Bhadra A, Ionides EL, Bouma M, Dhiman RC, Yadav RS, et al. Forcing versus feedback: Epidemic malaria and monsoon rains in northwest India. PLoS Comput Biol. 2010;6:e1000898. doi: 10.1371/journal.pcbi.1000898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das NG, Baruah I, Kamal S, Sarkar PK, Das SC, Santhanam K. An epidemiological and entomological investigation on malaria outbreak at Tamulpur PHC, Assam. Indian J Malariol. 1997;34:164–70. [PubMed] [Google Scholar]
- 10.Hay SI, Gething PW, Snow RW. India's invisible malaria burden. Lancet. 2010;376:1716–7. doi: 10.1016/S0140-6736(10)61084-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dhingra N, Jha P, Sharma VP, Cohen AA, Jotkar RM, Rodriguez PS, et al. Million Death Study Collaborators. Adult and child malaria mortality in India: A nationally representative mortality survey. Lancet. 2010;376:1768–74. doi: 10.1016/S0140-6736(10)60831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solanki RL, Kumawat BL, Anuradha Y, Joshi U, Kochar DK, Kalra VB. Pathology of malaria with special references to haematological changes in malaria. Indian J Pathol Microbiol. 1996;39:391–414. [PubMed] [Google Scholar]
- 13.Gupta S, Gunter JT, Novak RJ, Regens JL. Patterns of Plasmodium vivax and Plasmodium falciparum malaria underscore importance of data collection from private health care facilities in India. Malar J. 2009;8:227. doi: 10.1186/1475-2875-8-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muddaiah M, Prakash PS. A study of clinical profile of malaria in a tertiary referral centre in South Canara. J Vector Borne Dis. 2006;43:29–33. [PubMed] [Google Scholar]
- 15.Desai SP, Vora IM, Phatak AM, Bhalerao M. Plasmodium falciparum malaria - a diagnostic dilemma. Indian J Pathol Microbiol. 1996;39:477–9. [PubMed] [Google Scholar]
- 16.Dev V, Phookan S, Sharma VP, Anand SP. Physiographic and entomologic risk factors of malaria in Assam, India. Am J Trop Med Hyg. 2004;71:451–6. [PubMed] [Google Scholar]
- 17.Prakash A, Mohapatra PK, Bhattacharyya DR, Doloi P, Mahanta J. Changing malaria endemicity - a village based study in Sonitpur, Assam. J Commun Dis. 1997;29:175–8. [PubMed] [Google Scholar]
- 18.Shukla RP, Pandey AC, Mathur A. Investigation of malaria outbreak in Rajasthan. Indian J Malariol. 1995;32:119–28. [PubMed] [Google Scholar]
- 19.Dhiman RC, Pillai CR, Subbarao SK. Investigation of malaria outbreak in Bahraich district, Uttar Pradesh. Indian J Med Res. 2001;113:186–91. [PubMed] [Google Scholar]
- 20.Srivastava HC, Kant R, Bhatt RM, Sharma SK, Sharma VP. Epidemiological observations on malaria in villages of Buhari PHC, Surat, Gujarat. Indian J Malariol. 1995;32:140–52. [PubMed] [Google Scholar]
- 21.Newton CR, Hien TT, White N. Cerebral malaria. J Neurol Neurosurg Psychiatry. 2000;69:433–41. doi: 10.1136/jnnp.69.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohanty S, Mishra SK, Patnaik R, Dutt AK, Pradhan S, Das B, et al. Brain swelling and mannitol therapy in adult cerebral malaria: A randomized trial. Clin Infect Dis. 2011;53:349–55. doi: 10.1093/cid/cir405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaatano GM, Mashauri FM, Kinung'hi SM, Mwanga JR, Malima RC, Kishamawe C, et al. Patterns of malaria related mortality based on verbal autopsy in Muleba District, north-western Tanzania. Tanzan J Health Res. 2009;11:210–8. doi: 10.4314/thrb.v11i4.50185. [DOI] [PubMed] [Google Scholar]
- 24.Rane SR, Bapat VM, Holla W. Malaria still a threat to life - a postmortem study. Indian J Pathol Microbiol. 2003;46:17–9. [PubMed] [Google Scholar]
- 25.Shukla MM, Singh N, Singh MP, Tejwani BM, Srivastava DK, Sharma VP. Cerebral malaria in Jabalpur, India. Indian J Malariol. 1995;32:70–5. [PubMed] [Google Scholar]
- 26.Kar PK, Dua VK, Gupta NC, Gupta A, Dash AP. Plasmodium falciparum gametocytaemia with chloroquine chemotherapy in persistent malaria in an endemic area of India. Indian J Med Res. 2009;129:299–304. [PubMed] [Google Scholar]
- 27.Mishra G. Hospital based study of malaria in Ratnagiri district, Maharashtra. J Vector Borne Dis. 2003;40:109–11. [PubMed] [Google Scholar]
- 28.Singh N, Dash AP, Thimasarn K. Fighting malaria in Madhya Pradesh (Central India): Are we losing the battle? Malar J. 2009;8:93. doi: 10.1186/1475-2875-8-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anand K, Kant S, Kumar G, Kapoor SK. Clinical case definition of malaria at a secondary level hospital in northern India. Southeast Asian J Trop Med Public Health. 1999;30:243–5. [PubMed] [Google Scholar]
- 30.Sabin LL, Rizal A, Brooks MI, Singh MP, Tuchman J, Wylie BJ, et al. Attitudes, knowledge, and practices regarding malaria prevention and treatment among pregnant women in Eastern India. Am J Trop Med Hyg. 2010;82:1010–6. doi: 10.4269/ajtmh.2010.09-0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bharti PK, Silawat N, Singh PP, Singh MP, Shukla M, Chand G, et al. The usefulness of a new rapid diagnostic test, the First Response Malaria Combo (pLDH/HRP2) card test, for malaria diagnosis in the forested belt of central India. Malar J. 2008;7:126. doi: 10.1186/1475-2875-7-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage: Diagnosing it and finding the cause. Cleve Clin J Med. 2008;75:258, 260, 264–5 passim. doi: 10.3949/ccjm.75.4.258. [DOI] [PubMed] [Google Scholar]


