Abstract
Background:
Primary care physicians (PCPs) encounter a large number of patients with dermatological diseases. However, delivering appropriate management is a challenge considering the inadequate dermatology training offered during the undergraduate medical curriculum. Teledermatology is the clinical evaluation of skin lesions by dermatologists and allows patients to be diagnosed and treated from a distant site. It is seen as a potential solution to the shortage of specialists and providing equitable service in remote areas.
Aim:
The study was aimed at estimating the diagnostic agreement of common dermatological conditions between a PCP and a teledermatologist.
Materials and Methods:
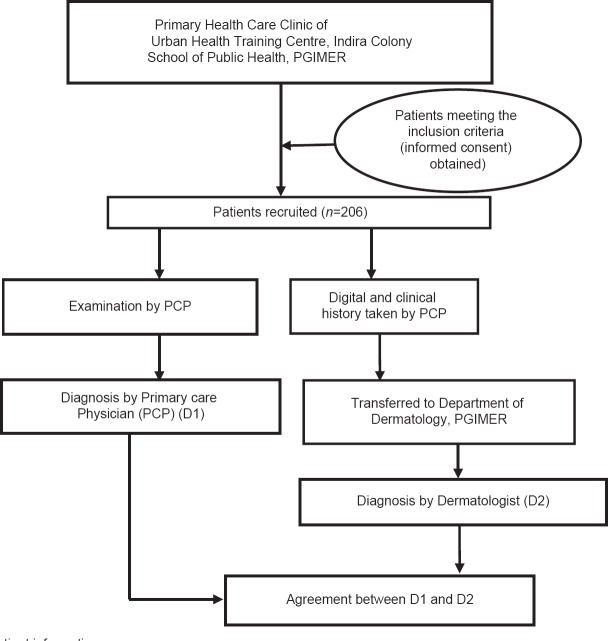
Consecutive patients with dermatological ailments who attended a primary health care clinic were recruited into the study, examined by the PCP and offered a diagnosis. The clinical images and patients’ history were collected and transferred to a dermatologist at a tertiary center who also made a diagnosis. Agreement between diagnosis made by the PCPs and the teledermatologist was measured using kappa (κ) statistics.
Results:
Overall agreement between the diagnoses made by a PCP and the dermatologist was found to be 56%. Poor κ agreement (<0.4) was seen in the diagnosis of psoriasis and eczema.
Conclusion:
Teledermatology can supplement specialist dermatology service in remote areas. There was poor agreement in the diagnosis of psoriasis, classifying various types of eczematous conditions and fungal infections. Scarce manpower in dermatology at the primary health care level compounded by the burden of skin ailments necessitates training of PCPs in common dermatological conditions.
Keywords: Dermatologist, diagnostic agreement, primary care physician
INTRODUCTION
The prevalence of skin diseases in the general population varies from 6.3% to 11.16% as reported in various studies.[1,2,3,4,5,6,7] Majority (60%) of these patients are treated by non-dermatologists, mostly primary care physicians (PCPs) who encounter and treat a significant proportion of skin disease.[8]
The rural remote population, which is around 70% of the total population, has limited access to specialist skin care.[9] The network of primary care providers can be utilized to tackle the scarcity of specialist dermatologists and augment the dermatological services in rural areas.
The high numbers of patients with skin morbidities reporting to PCPs having limited training in dermatology poses serious implications for appropriate cost-effective treatment and care.[10,11,12]
Teledermatology allows patients with dermatological complaints to be diagnosed and possibly, treated from a distance. There are two types of teledermatology: real-time (synchronous) and store- and-forward (asynchronous). In store- and-forward teledermatology, the dermatologist analyzes stored images obtained at an earlier point in time and then provides a diagnosis and management plan.[13] Teledermatology holds great potential for revolutionizing the delivery of dermatology services, providing equitable service to remote areas and allowing PCPs to refer patients to dermatology centers of excellence at a distance. The feasibility of teledermatology in augmenting specialist dermatology services in remote areas needs further exploration.
The present study was thus planned to document the level of agreement between the diagnosis of common dermatological conditions made by PCPs and teledermatologist.
MATERIALS AND METHODS
The present exploratory study was carried out at the Primary Health Care Clinic of School of Public Health, Post Graduate Institute of Medical Education and Research (PGIMER), situated at Indira Colony, an urban resettlement colony in Chandigarh. A total of 206 patients who attended the clinic during the period of data collection from July to December 2011 with dermatological conditions were recruited into the study consecutively after obtaining written informed consent. Pregnant women and patients with concurrent systemic diseases were excluded. Patients who came for follow up (i.e. those registered earlier) were also excluded.
Each patient thus recruited was examined by the PCP. A clinical diagnosis (D1) was made and the patient was advised appropriate management. At the same time, a digital image (with the help of a 10.1 megapixel digital camera, 4× optical zoom, 2.5” LCD, of make Panasonic DMC-F2) of the lesion and a short structured history was collected by the physician for each patient. Clinical photographs were taken against a blue background to maintain uniformity. The clinical images and the patients’ history sheet thus collected were coded and stored in an electronic form in a computer. Once in a month, an electronic copy of all the clinical images (stored in a flash drive) and patients’ history sheets were sent to the Department of Dermatology, PGIMER. The images were then reviewed by a dermatologist, and a final diagnosis (D2) was made on a monthly basis [Figure 1].
Figure 1.
Flow of patient information
The PCP was a medical graduate with 3 years of training in primary care and public health. The PCP was provided a structured history-taking template. However, no formal training was provided to him regarding dermatological history-taking and diagnosis. The specialist teledermatologist was a faculty at the Department of Dermatology of a premier tertiary care government hospital.
The pattern and type of disease prevalent in the community was explored by descriptive statistics. Agreement between the diagnosis made by a PCP (D1) and the specialist dermatologist (D2) was calculated using kappa (κ) statistics. The operational issues regarding collection, storage and transfer of images were documented on a daily basis in a diary. Ethical aspects of the study were approved by the intramural research committee, PGIMER, Chandigarh.
RESULTS
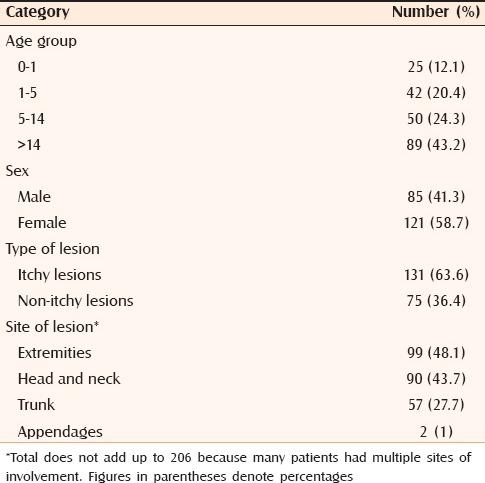
A total of 206 patients with dermatological diseases were recruited into the study. Of these, 85 (41.3%) were males while 121 (58.7%) were females. Most of the patients (89 cases, 43.2%) were in the adult age group > 14 years, followed by 50 (24.3%) from the age group of 5-14 years. Itchy lesions (131, 63.6%) outnumbered non-itchy lesions (75, 36.4%). Lesions were distributed mostly over the extremities (48.1%) followed by the head and neck region (43.7%), and trunk (27.7%). Only 1% of lesions occurred in the appendages (nails) [Table 1].
Table 1.
Distribution of dermatoses (diagnosed by the teledermatologist) according to age, sex, type and site of lesion
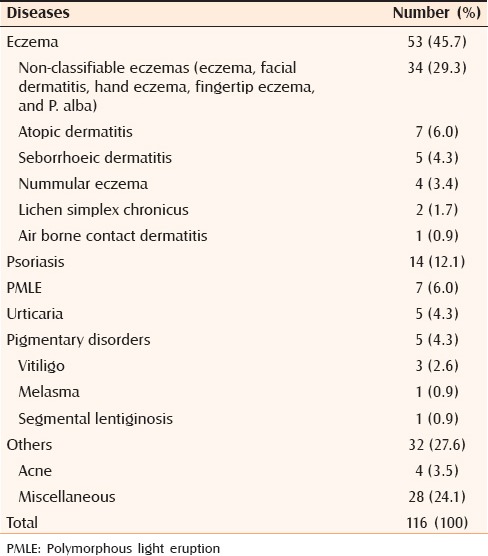
Among the infective disorders diagnosed by the dermatologist, bacterial infection (40.4%) was the most common followed by fungal infection (28.7%) and scabies (19.2%) [Table 2]. Among the non-infective dermatoses, eczemas (45.7%) were in majority followed by psoriasis (12.1%), urticaria (4.3%), polymorphous light eruption (PMLE) (6.0%) and pigmentary disorders (4.3%). Contact dermatitis, atopic eczema, seborrhoeic dermatitis, nummular eczema, lichen simplex chronicus, hand eczema and fingertip eczema were some of the other disorders noted under eczemas [Table 3].
Table 2.
Distribution of infective dermatoses (diagnosed by the dermatologist)
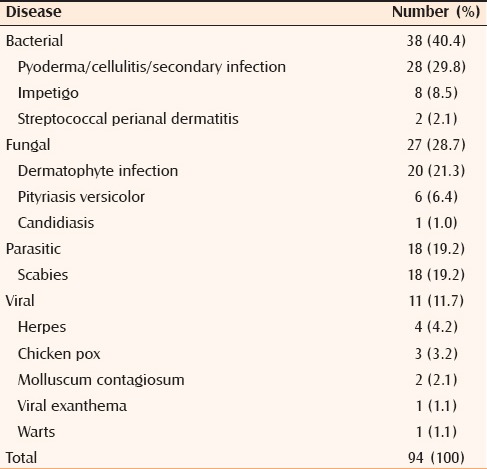
Table 3.
Distribution of non-infective dermatoses (diagnosed by the teledermatologist)
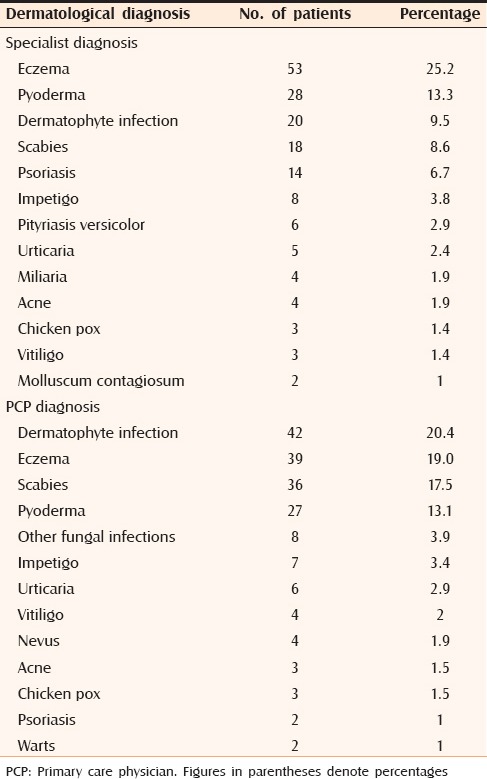
The ten most common diagnoses made by a PCP accounted for nearly 84% of the diagnoses whereas those accounted for 74.5% as diagnosed by specialist dermatologists. The most common diagnoses made by a PCP were dermatophyte infection (20.4%), scabies (17.5%), eczema (19.0%), pyoderma (13.1%). Most common diagnoses made by the dermatologist were eczema (25.2%) followed by pyoderma (13.3%), dermatophyte infection (9.5%), scabies (8.6%) and psoriasis (6.7%) [Table 4].
Table 4.
Most common diagnosis made by dermatologist and PCP
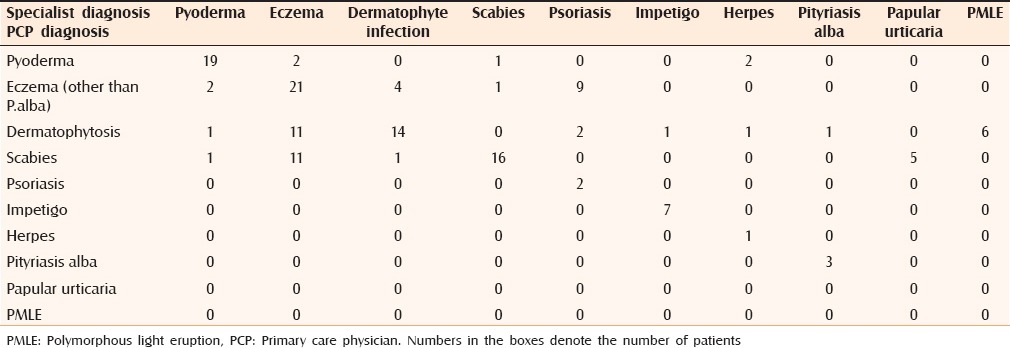
The overall degree of agreement between the diagnoses made by a PCP and the final diagnoses by the dermatologist was 56%. Good agreement (κ > 0.7) was seen in the diagnosis of pyoderma (0.76), moderate agreement (<0.4< κ <0.7) was found in scabies (0.56) and dermatophyte infection (0.49). However, κ agreement was poor (κ < 0.4) in case of eczema (0.37) and psoriasis (0.27).
PCPs correctly diagnosed only 2 of the 14 cases of psoriasis but 7 out of 8 cases of impetigo and 16 out 18 cases of scabies were diagnosed correctly. However, 11 cases of eczema had been misclassified as scabies. All five cases of papular urticaria had been misidentified as scabies whereas PMLE had been misdiagnosed as dermatophyte infection in 6 out of 7 instances. The PCP could correctly diagnose pityriasis versicolor in 6 out of 7 cases [Table 5].
Table 5.
Comparison of common diagnoses made by the PCP and the dermatologist
DISCUSSION
Dermatology is still regarded as a subject of marginal importance during graduate medical education. Diagnostic skills for common dermatologic diseases among medical graduates therefore remain elusive. The scarcity of specialized human resources in dermatology coupled with poor access to dermatology services in remote areas leaves no other option but to explore the role of teledermatology as a support tool in primary care dermatology. Since dermatology is a specialty with utmost importance of visual inspection, a significant proportion of common conditions can be diagnosed and treated by teledermatology. Based on the criteria proposed by Kanthraj, this study can be classified as Grade-3 teledermatology practice, i.e. a large (>100 subjects) prospective study without a gold standard comparison.[14] The present study showed that 10 common diagnoses account for more than three-fourths of the skin disorders encountered in primary healthcare clinic. The PCPs thus need to be trained on these 10 common skin conditions so that they can appropriately manage a large proportion of patients with common dermatologic complaints.
Certain diagnoses like airborne contact dermatitis, PMLE, lichen simplex chronicus, nummular eczema, papular urticaria, hand eczema, fingertip eczema, pitted keratolysis and molluscum contagiosum were made exclusively by the dermatologist. PCPs tended to overdiagnose dermatophyte infection, eczema, scabies and pyoderma. Non-dermatologists occasionally used non-specific terms such as rash, dark circles, dry skin, fungal infection to diagnose some conditions.
There are many studies documenting overall agreement between the diagnosis made by the PCP and the face-to-face consultation with the dermatologist. The level of agreement reported from such studies ranged from 40% to 60%. All of these studies highlighted poor knowledge of dermatology in primary care providers.[15,16,17,18,19] Further, studies by Graells et al. and Porta et al. have reported higher diagnostic agreement of 72% and 65.5%, respectively.[20,21]
The present study reported an overall agreement of 56% between the primary care provider and the dermatologist. The diagnostic agreement between primary care providers and remote dermatologists ranged from 34.4% to 61% across different studies.[22,23,24,25] Store-and-forward teledermatology also provided a high level of patient satisfaction, and was effective in remote supervision and education of general practitioners. Face-to-face consultations with the specialist were avoided in 69% of consultations.[24] Teledermatology has educational value for primary care providers as well.[22]
Since the diagnosis by the specialist dermatologist was based on digital images of patients seen by the PCP, taking proper images for better visualization becomes extremely important. Therefore, a simple manual on camera specification, background of images, site (s) to be photographed and quality of the images should be prepared. Although American Telemedicine Association has set guidelines for standard teledermatology practice, we need to look at them critically and adapt them suitably.[26]
Limitation
The major limitation in this study stems from the fact that the diagnosis made by the dermatologist is based on digital images and patient's history and not actually examining the patient which could have been the ideal situation.
CONCLUSION
Teledermatology can reduce the need for conventional clinical consultations while still maintaining clinical safety. Teledermatology can supplement specialist dermatology service in remote areas. The role of teledermatology as a useful training tool, supervision of primary care providers, and for clinical governance and quality assurance in clinics in remote rural areas needs to be explored further.
There was poor agreement in the diagnosis of psoriasis, fungal infections and recognizing various types of eczematous conditions. This study thus highlights the importance of training PCP in the field of dermatology to recognize common skin conditions encountered in routine practice.
ACKNOWLEDGMENT
We acknowledge the financial assistance received from the PGIMER intramural research grant and Ford Foundation IAPSM Grant.
Footnotes
Source of Support: The study was supported by IAPSM Ford Foundation Research Grant and PGIMER intramural research grant
Conflict of Interest: None declared.
REFERENCES
- 1.Gangadharan C, Joseph A, Sarojini A. Pattern of skin diseases in Kerala. Indian J Dermatol Venereol Leprol. 1976;42:49–51. [PubMed] [Google Scholar]
- 2.Dayal SG, Gupta GP. A cross section of skin diseases in Bundelkhand region, UP. Indian J Dermatol Venereol Leprol. 1977;43:258–61. [PubMed] [Google Scholar]
- 3.Kuruvilla M, Sridhar KS, Kumar P, Rao GS. Pattern of skin diseases in Bantwal Taluq, Dakshina Kannada. Indian J Dermatol Venereol Leprol. 2000;66:247–8. [PubMed] [Google Scholar]
- 4.Rao GS, Kumar SS, Sandhya Pattern of skin diseases in an Indian village. Indian J Med Sci. 2003;57:108–10. [PubMed] [Google Scholar]
- 5.Das KK. Pattern of dermatological diseases in Gauhati Medical College and Hospital Guwahati. Indian J Dermatol Venereol Leprol. 2003;69:16–8. [PubMed] [Google Scholar]
- 6.Devi T, Zamzachin G. Pattern of skin diseases in Imphal. Indian J Dermatol. 2006;51:149–50. [Google Scholar]
- 7.Nair PS, Nair TG. Pattern of dermatological diseases in Trivandrum. Indian J Dermatol Venereol Leprol. 1999;65:261–3. [PubMed] [Google Scholar]
- 8.Stern RS, Nelson C. The diminishing role of the dermatologist in the office-based care of cutaneous diseases. J Am Acad Dermatol. 1993;29:773–7. doi: 10.1016/0190-9622(93)70243-m. [DOI] [PubMed] [Google Scholar]
- 9.Thappa DM. History of Dermatology, Venereology and Leprology in India. J Postgrad Med. 2002;48:160–5. [PubMed] [Google Scholar]
- 10.Ramsay DL, Mayer F. National survey of undergraduate dermatologic medical education. Arch Dermatol. 1985;121:1529–30. [PubMed] [Google Scholar]
- 11.Pariser RJ, Pariser DM. Primary care physicians’ errors in handling cutaneous disorders. A prospective survey. J Am Acad Dermatol. 1987;17:239–45. doi: 10.1016/s0190-9622(87)70198-4. [DOI] [PubMed] [Google Scholar]
- 12.Ramsay DL, Weary PE. Primary care in dermatology: Whose role should it be? J Am Acad Dermatol. 1996;35:1005–8. doi: 10.1016/s0190-9622(96)90137-1. [DOI] [PubMed] [Google Scholar]
- 13.Vañó-Galván S, Hidalgo A, Aguayo-Leiva I, Gil-Mosquera M, Ríos-Buceta L, Plana MN, et al. Store-and-forward teledermatology: assessment of validity in a series of 2000 observations. Actas Dermosifiliogr. 2011;102:277–83. doi: 10.1016/j.ad.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Kanthraj GR. A longitudinal study of consistency in diagnostic accuracy of teledermatology tools. Indian J Dermatol Venereol Leprol. 2013;79:668–78. doi: 10.4103/0378-6323.116735. [DOI] [PubMed] [Google Scholar]
- 15.Fleischer AB, Jr, Feldman SR, Bradham DD. Office-based physician services provided by dermatologists in the United States in 1990. J Invest Dermatol. 1994;102:93–7. doi: 10.1111/1523-1747.ep12371739. [DOI] [PubMed] [Google Scholar]
- 16.Kirsner RS, Federman DG. Managed care: The dermatologist as a primary care provider. J Am Acad Dermatol. 1995;33:535–7. doi: 10.1016/0190-9622(95)91410-2. [DOI] [PubMed] [Google Scholar]
- 17.Federman D, Hogan D, Taylor JR, Caralis P, Kirsner RS. A comparison of diagnosis, evaluation, and treatment of patients with dermatologic disorders. J Am Acad Dermatol. 1995;32:726–9. doi: 10.1016/0190-9622(95)91449-8. [DOI] [PubMed] [Google Scholar]
- 18.Solomon BA, Collins R, Silverberg NB, Glass AT. Quality of care: Issue or oversight in health care reform? J Am Acad Dermatol. 1996;34:601–7. doi: 10.1016/s0190-9622(96)80058-2. [DOI] [PubMed] [Google Scholar]
- 19.Gerbert B, Maurer T, Berger T, Pantilat S, McPhee SJ, Wolff M, et al. Primary care physicians as gatekeepers in managed care. Primary care physicians’ and dermatologists’ skills at secondary prevention of skin cancer. Arch Dermatol. 1996;132:1030–8. [PubMed] [Google Scholar]
- 20.Graells J, Espinola A, Barrio C, Muñoz MD, Román A, Parellada N. Minor cutaneous ambulatory surgery and cryotherapy. Comparative study between a dermatologist and family physicians. Actas Dermosifiliogr. 2007;98:171–7. [PubMed] [Google Scholar]
- 21.Porta N, San Juan J, Grasa MP, Simal E, Ara M, Querol MA. Diagnostic agreement between primary care physicians and dermatologists in the health area of a referral hospital. Actas Dermosifiliogr. 2008;99:207–12. [PubMed] [Google Scholar]
- 22.Caumes E, Le Bris V, Couzigou C, Menard A, Janier M, Flahault A. Dermatoses associated with travel to Burkina Faso and diagnosed by means of teledermatology. Br J Dermatol. 2004;150:312–6. doi: 10.1111/j.1365-2133.2004.05745.x. [DOI] [PubMed] [Google Scholar]
- 23.See A, Lim AC, Le K, See JA, Shumack SP. Operational teledermatology in Broken Hill, rural Australia. Australas J Dermatol. 2005;46:144–9. doi: 10.1111/j.1440-0960.2005.00166.x. [DOI] [PubMed] [Google Scholar]
- 24.Thind CK, Brooker I, Ormerod AD. Teledermatology: A tool for remote supervision of a general practitioner with special interest in dermatology. Clin Exp Dermatol. 2011;36:489–94. doi: 10.1111/j.1365-2230.2011.04073.x. [DOI] [PubMed] [Google Scholar]
- 25.Henning JS, Wohltmann W, Hivnor C. Teledermatology from a combat zone. Arch Dermatol. 2010;146:676–7. doi: 10.1001/archdermatol.2010.110. [DOI] [PubMed] [Google Scholar]
- 26.Krupinski E, Burdick A, Pak H, Bocachica J, Earles L, Edison K, et al. American Telemedicine Association's practice guidelines for teledermatology. Telemed J E Health. 2008;14:289–302. doi: 10.1089/tmj.2007.0129. [DOI] [PubMed] [Google Scholar]