Sir,
Erythroderma is the condition where more than 90% body surface area develops erythema and scaling. Common causes are eczemas (40%), psoriasis (15%), drugs and malignancy, while crusted scabies, lichen planus, dermatomyositis, etc. account for only 0.5% cases.[1,2]
Scabies is an infestation by ectoparasite of female gravid mite of Sarcoptes scabiei var. hominis. Burrow is the pathognomonic feature of scabies infestation. The average number of adult female mites on an individual suffering from the common form of scabies is about 12. Approximately 40-50 eggs are laid by each female during its lifespan of 4-6 weeks, during which time she doesn’t leave the burrow. Scabies affects all races and social classes worldwide, but accurate figures of its prevalence are difficult to obtain.[1]
The appellation “Norwegian” derives from the description in Norway by Danielssen and Boeck of a type of scabies in which a huge number of mites were present in lepers may be the number of mites was in millions. It is seen in patients with sensory anesthesia, mental impairment, physical incapacity, and immunosuppression.[1]
A 62-year-old patient presented with large, warty crusts with irregular thickening and fissuring of the scalp, neck, trunk, arms, forearms, thighs, genitalia, gluteal region, dorsum of hands and webs of fingers [Figures 1-3]. Scaling was generalized and there was sparing of palms, soles, and nails. There was no itching at the time of presentation. He developed mild itching on some occasions during the course of illness and over one a period of year, he had been treated in multiple hospitals for eczema and psoriasis and applied topical corticosteroid for his hyperkeratotic lesions [Figure 4]. On general examination, he had pallor and generalized lymphadenopathy. On dermatological examination, large thickened crusts were evident from the scalp to mid-thigh, sparing some areas of the chest, palms, soles and nails. More than 90% of skin surface was involved with erythema and scaling. Crusts could be separated with a forceps without bleeding. On mental state examination, patient had dementia and denied sensation of itching. Microscopic examination of crusts dissolved in 10% KOH revealed fields teeming with mites and eggs [Figures 5 and 6]. He was treated with ivermectin 12 mg weekly for four weeks and application of topical permethrin 5% cream every day for two weeks and then once weekly for the next two weeks. After one month of treatment the patient's erythroderma and skin lesions regressed completely.
Figure 1.

Generalized scaling all over the body
Figure 3.

Affection of web of fingers and dorsum of hand and forearms
Figure 4.

Scaling over the neck
Figure 5.
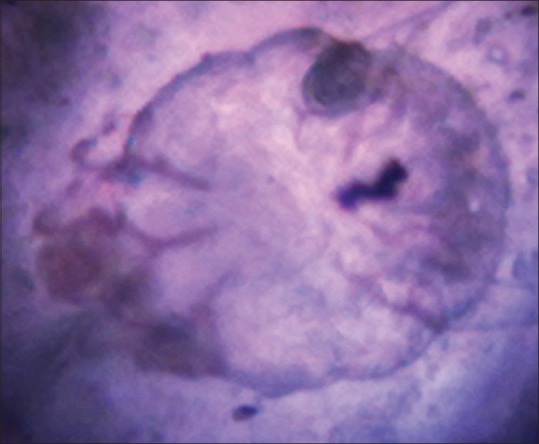
Scabies mite in KOH mount of scales (×10)
Figure 6.

Eggs of scabies mite in 10% KOH mount
Figure 2.

Scaling over back and buttocks
In common scabies, there are few mites, probably because scratching destroys the burrows. A good standard of hygiene may also help to control the mite population. In crusted scabies, the host's response to the mites is modified, allowing them to multiply.[1,3] Patients who are mentally retarded or suffer from dementia may develop crusted scabies.[2] The reason for this association with mental abnormality is not completely understood, but lack of appreciation of pruritus may be important. Crusted scabies has also resulted from inappropriate use of potent topical steroids.[3,4,5,6] Suppression of sensitivity to the mites reduces itching, so there is less scratching and destruction of burrows. Moreover, diagnosis of the cause of erythroderma is sometimes difficult and repeated biopsy is needed.
Our clinical differential diagnoses were hyperkeratotic eczema, psoriasis, contact dermatitis, but after application of topical corticosteroid the lesions didn’t resolve but rather they were exacerbated. There were crusts; and no micaceous scales or the Auspitz's sign of were absent. Thus the patient's dementia likely contributed to scabies evolving into the crusted variant while the use of topical potent corticosteroid exacerbated the erythroderma.
REFERENCES
- 1.Burns DA. Diseases caused by arthropods and other noxious animals. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Wiley-Blackwell; 2010. pp. 38.40–l4. [Google Scholar]
- 2.Berth-Jones J. Eczema, lichenification, prurigo and erythroderma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Wiley-Blackwell; 2010. pp. 23.46–9. [Google Scholar]
- 3.Herridge CF. Norwegian scabies (crusted scabies) Br Med J. 1963;1:239–40. doi: 10.1136/bmj.1.5325.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clayton R, Farrow S. Norwegian scabies following topical steroid therapy. Postgrad Med J. 1975;51:657–9. doi: 10.1136/pgmj.51.599.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macmillan AL. Unusual features of scabies associated with topical fluorinated steroids. Br J Dermatol. 1972;87:496–7. doi: 10.1111/j.1365-2133.1972.tb01597.x. [DOI] [PubMed] [Google Scholar]
- 6.Millard LG. Norwegian scabies developing during treatment with fluorinated steroid therapy. Acta Derm Venereol. 1977;57:86–8. [PubMed] [Google Scholar]


