A 15-year-old female patient presented with a lesion on the labium majus of three years duration. The lesion was asymptomatic, skin colored, pedunculated, and measured 20 cm in diameter [Figure 1]. Three months ago, an ulcer developed on this mass. Total excision of the lesion was performed under local anesthesia with primary closure. Histopathologic examination revealed papillomatosis, regular acanthosis, loose collagen fibers, and several dilated capillaries [Figure 2]. There was no malignancy on the ulcer biopsy. The tumor cells were negative for the immunostains S100 protein, smooth muscle actin, desmin and CD34.
Figure 1.

A solitary, bag-like, ulcerated, pedunculated mass on the left labium majus measuring 20 cm in diameter
Figure 2.
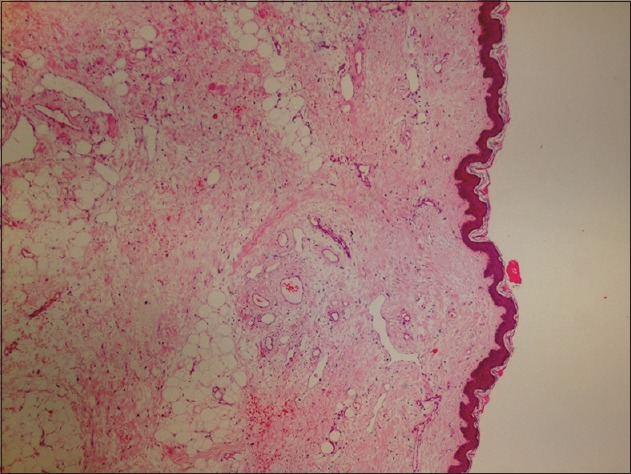
Fibrous collagen with telangiectatic vessels, covered by a hyperkeratotic and acanthotic epidermis, and adipocytes in the center of giant acrochordon (H and E, ×40)
Acrochordons, also called skin tags or fibroepithelial stromal polyps,[1] are common benign tumors seen in middle aged men and women They occur as pedunculated papules or tumors of variable size and are most commonly located on the eyelids, neck, axilla, and groin. The sex distribution of acrochordons is equal. Clinically, acrochordons resemble intradermal nevi, warts, pedunculated seborrheic keratosis, angiomyxoma and neurofibromatosis. They commonly are seen in peri-or postmenopausal women.[2,3] Acrochordons rarely occur on the vulva, cervix and extra-genital sites.[4] Despite acrochordons involving about 46% of the general population; there are a few case reports of the giant form in the literature.[5] Although a malignant transformation rate for all acrochordons was reported as 0.37%, giant acrochordons have a higher potential for malignancy, especially, chronically irritated and inflamed acrochordons. Malignancy should be ruled out in every diagnosis of giant acrochordons.[6] The relationship between acrochordons and impaired glucose tolerance, obesity, and polyps of the colon has been reported in some studies.[3]
Histopathologically, acrochordons are polypoid with variably loose to intense collagenous stroma with fine walled enlarged blood vessel in the center. Pigmentation of basal keratinocytes is increased in the epidermis. Fat cells are sometimes seen within the center of larger acrochordons.[7,8] A few smooth muscle bundles and hyalinized vascular changes may be noted at the base of acrochordon. Electrocautery and cryotherapy are generally curative. Simple excision is required in case of a giant lesion.[3]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ilango N, Jacob J, Gupta AK, Choudhrie L. Acrochordon - A rare giant variant. Dermatol Surg. 2009;35:1804–5. doi: 10.1111/j.1524-4725.2009.01294.x. [DOI] [PubMed] [Google Scholar]
- 2.Kura MM, Jindal SR, Khemani UN. Aggressive angiomyxoma of the vulva: An uncommon entity. Indian Dermatol Online J. 2012;3:128–30. doi: 10.4103/2229-5178.96712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghosh SK, Bandyopadhyay D, Chatterjee G, Bar C. Giant skin tags on unusual locations. J Eur Acad Dermatol Venereol. 2009;23:233. doi: 10.1111/j.1468-3083.2008.02816.x. [DOI] [PubMed] [Google Scholar]
- 4.Madueke-Laveaux OS, Gogoi R, Stoner G. Giant fibroepithelial stromal polyp of the vulva: Largest case reported. Ann Surg Innov Res. 2013;7:8. doi: 10.1186/1750-1164-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abbasi F, Pourghasem G, Rezaei M. Giant skin tag. J Surg Pak (Int) 2011;16:183–4. [Google Scholar]
- 6.Aksoy B, Aksoy HM, Civas E, Üstün H. Giant skin tags located in the lower half of the body: Report of two cases. Turkiye Klinikleri J Med Sci. 2009;29:1770–2. [Google Scholar]
- 7.Naik R, Baliga PB, Pai MR, Nayak S, Narayanan S. Multiple fibrolipomas of the skin. Indian J Dermatol Venerol Leprol. 2003;69:31–2. [Google Scholar]
- 8.Chan MM, Yong TT, Sittampalam K. Giant labial fibroepithelial stromal polyp. Malays J Pathol. 2013;35:91–4. [PubMed] [Google Scholar]


