Abstract
Context:
Development of the cultural formulation interview (CFI) in DSM-5 required validation for cross-cultural and global use.
Aims:
To assess the overall value (OV) of CFI in the domains of feasibility, acceptability, and utility from the vantage points of clinician-interviewers, patients and accompanying relatives.
Settings and Design:
We conducted cross-sectional semi-structured debriefing interviews in a psychiatric outpatient clinic of a general hospital.
Materials and Methods:
We debriefed 36 patients, 12 relatives and eight interviewing clinicians following the audio-recorded CFI. We transformed their Likert scale responses into ordinal values – positive for agreement and negative for disagreement (range +2 to −2).
Statistical Analysis:
We compared mean ratings of patients, relatives and clinician-interviewers using nonparametric tests. Clinician-wise grouping of patients enabled assessment of clinician effects, inasmuch as patients were randomly interviewed by eight clinicians. We assessed the influence of the presence of relatives, clinical diagnosis and interview characteristics by comparing means. Patient and clinician background characteristics were also compared.
Results:
Patients, relatives and clinicians rated the CFI positively with few differences among them. Patients with serious mental disorders gave lower ratings. Rating of OV was lower for patients and clinicians when relatives were present. Clinician effects were minimal. Clinicians experienced with culturally diverse patients rated the CFI more positively. Narratives clarified the rationale for ratings.
Conclusions:
Though developed for the American DSM-5, the CFI was valued by clinicians, patients and relatives in out-patient psychiatric assessment in urban Pune, India. Though relatives may add information and other value, their presence in the interview may impose additional demands on clinicians. Our findings contribute to cross-cultural evaluation of the CFI.
Keywords: Acceptability, clinician-effects, cultural formulation interview, debriefing, feasibility, influence of relatives, utility
INTRODUCTION
Urbanization and globalization have contributed to the importance and appreciation of the interests of cultural psychiatry. Culture is relevant for a wide range of conditions, not just mainstream psychiatric disorders, but also medically unexplained symptoms[1] and various chronic diseases.[2] After developing the outline for cultural formulation in DSM-IV, the current DSM-5 now includes an operational approach to assessment that addresses cultural issues as a feature of clinical evaluation.[3] The role of culture in making a diagnosis, value of the approach of the cultural formulation, its possible applications and potential barriers in the use of DSM-5 have been widely discussed.[4,5,6,7] Although research tools had previously been available for cultural assessment (e.g. explanatory model interview catalogue (EMIC) interviews for cultural epidemiology[8,9] and the short explanatory model interview [SEMI])[10] an interview guide for cultural assessment in clinical practice had been lacking. The cultural formulation interview (CFI) for DSM-5 aimed to fill this gap. It was a product of the cultural issues subgroup of the culture and gender group for DSM-5.
Having developed the tool, it required validation, and the cultural interest group was sensitive to the need for validating such a tool. The importance of that has been articulated in the section of DSM-5 explaining the use of the manual. Considering further needs and anticipated future development of diagnostic assessments, the CFI was included among several instruments for which further study and scientific assessment are needed. A series of field studies were, therefore, undertaken to examine the feasibility, acceptability and clinical utility of the CFI. Cognizant of DSM aspirations for global validity, an aspect of the field, which is particularly relevant to the interests of cultural psychiatry, field trials were also included in settings beyond the U.S. Other countries where the field studies were conducted include India, Peru, the Netherlands, Canada and Kenya. Two of the field sites for validating the CFI were located in India.[11] Diverse and rapidly changing cultural features of Indian urban patients and clinicians pose a challenge as well as an opportunity to test the CFI. Cultural epidemiological studies[12] using EMIC interviews had influenced the development of the CFI.
To fulfill expectations, the CFI had to be short enough to be feasible in busy clinical practice settings. Although categorical and/or numeric coding is required for many research instruments, an open-ended assessment interview was more relevant for clinical assessment to enhance therapeutic relationships. Patients are more likely to value an interview that enables them to tell their story with reference to issues that matter for them, even though such issues may extend beyond the scope of criteria for an Axis-I diagnosis. Inasmuch as many Indian patients come to treatment with a family member, and effective treatment requires ongoing support of family, the relevance and acceptability for the CFI for accompanying family was also a relevant issue.
This study aimed to assess the overall value (OV) of the CFI and with reference to domains of feasibility, acceptability and clinical utility from the vantage points of clinicians, patients and their families. It aimed to compare the perceived value among these three groups of stakeholders in the interview, and the relative value of each domain of the CFI for each group. Clinician-specific effects and the influence of the presence of an accompanying relative on the perceived value of the CFI were also assessed. Our study also aimed to identify determinants of the perceived value with reference to salient sociodemographic features of patients and clinicians, and features of clinical diagnosis.
MATERIALS AND METHODS
Setting
Pune is the 8th largest metropolis in India[13] with a population of 5,049,968.[14] It is a centre for education, industry and technology undergoing rapid urbanization and environmental pollution. Health services include a mix of government facilities, nongovernmental health services, private practice and a mix of private and nongovernmental organization (NGO) partnerships. The study was completed in the Psychiatry Department of the King Edward Memorial Hospital (KEM), a general hospital with 650 beds. It is a private charitable trust, enabling it to serve both paying and nonpaying patients. It has a mix of primary and tertiary services in various disciplines of medicine. Psychiatry outpatients are generally from middle and low-income groups with diverse clinical problems.
Instruments
The CFI is a semi-structured interview assessing four domains of interest. These include a cultural definition of the problem; cultural perceptions of cause, context and supports; self-coping, past help-seeking and current preferences; and patients’ concerns about the relationship with their clinician. The CFI was translated into Marathi - the local vernacular – by the investigators, who are fluent in both languages. It was back-translated by two academic experts in literature and translation. Consensus meetings to ensure the validity and clarity of the translation contributed to the final Marathi version. Questions in both languages were retained on the interview forms used to administer the CFI. A Hindi version was adapted from prior Hindi translations provided by the PGIMER – Dr. Ram Manohar Lohia hospital site, Delhi, and from the KEM Hospital, Mumbai. This adapted version was back-translated and reviewed in consensus meetings according to the same process as the Marathi translation. The version used in the field trials had 14 questions, and an updated version for patients published in the DSM-5 has 16 items; another version for clinical informants has 17 items.
After each CFI, we administered debriefing interviews – debriefing interview for clinicians (DIC), debriefing interview for patients (DIP) and relatives if present (DIP-R). Each included the same substantive content with Likert-formatted response options, but with wording adapted for particular stakeholder interests of each group. Questions assessed the level of stakeholders’ agreement or disagreement with assertions of the feasibility (F), acceptability (A) and perceived clinical utility (U) of the CFI. For example, The feasibility domain included the assertion that the questions “were easy to understand;” the acceptability domain included the assertion that the CFI “helped me feel more at ease in the interview;” and the utility domain included the assertions that it “helped me communicate important aspects of my background, such as religious faith and/or culture” and “helped me understand how my background and current situation affect my problem.”
The effect of the CFI on the quality of the relationship with the clinician was assessed with regard to agreement with the following assertions in the DIP: The CFI “helped me explain my main concerns,” “encouraged me to share important information that I might not have mentioned otherwise,” and “helped me feel more at ease in the interview.” Analogous assertions were also assessed in the DIC. Assertions about the clinical utility for the clinician included, “gave me confidence in the diagnosis,” “facilitated treatment planning,” and “helped me assess the severity of the patient's problem.” The full DIC, DIP and DIP-R are available as supplementary files.
The perceived value of the CFI was analyzed for F, A and U items, and for the OV as a composite of all three. After the 1st and 3rd interviews the clinicians were asked seven questions about F and A for which responses were coded, and four open-ended questions encouraging reflection on the CFI, including questions they regarded as most and least useful. They were also asked about how best to incorporate the CFI in routine clinical practice despite the perceived challenges.
The capacity to consent quiz verified patients’ capacity to consent to the study. The Mini-Cog test was administered to patients over 65 years to document cognitive capacity.
All the patient- and relative-related debriefing forms were translated using standard methods into Marathi and Hindi as described above for the CFI. All the instruments in English were mostly the same across all the field sites. Translations focused on meaning rather than words, retaining closeness to the original. Considering high diversity and the multitude of dialects among Indian settings, having the original English questions and instructions on the interview forms helped clinician ensure that patients followed the questions thus ensuring the validity.
Design
Clinician interviewers were required to have some level of postgraduate, doctoral or master's level training in fields of medicine, nursing, clinical psychology or social work. They were fluent in the local languages of the clinical population. Adult patients, 18-80 years of age were recruited from the psychiatric outpatient clinic. New patients were recruited preferentially, and if a new patient was unavailable, the patient was assigned to a CFI clinician interviewer who had no prior experience with that patient. The clinician interviewer obtained consent after verifying the patient could answer 8 out of the 10 questions of the capacity to consent questionnaire correctly. Patients who failed the capacity to consent or Mini-Cog tests were excluded. Patients with acute suicidality, acute intoxication or withdrawal, dementia, mental retardation or florid psychosis were also excluded. A patient demographic form was completed by the patient with assistance from the research team if necessary.
The CFI was administered and audio-recorded, and the same clinician then conducted a standard clinical diagnostic interview to make a DSM-IV-TR diagnosis. Each clinician was required to complete at least three CFI interviews. Another clinician subsequently conducted debriefing interviews for the patient, CFI clinician interviewer and accompanying relative if present. Eight clinicians conducted CFI interviews, three of whom debriefed other clinicians or patients, and two additional clinicians conducted only debriefing interviews.
Analysis
Four categories of response to questions of the debriefing instruments were coded in a Likert format (strongly agree, agree, disagree and strongly disagree). For analysis response variables were coded with positive values for agreement (+1 agree and +2 for strongly agree) and negative values for disagreement (−1 disagree and −2 for strongly disagree). Most items of the debriefing were formulated such that agreement indicated positive valuation of the CFI (e.g. “helped me explain my main concerns”), and disagreement indicated disvaluation. Those items for which agreement indicated negative valuation were reverse coded for analysis (e.g. “took more time to share my perspective than i wanted”).
Although a neutral response option (value “0”) was not available for rating by a respondent, “0” was theoretically possible as a mean summary value from the analysis of a group of items or a group of respondents, that is, a “functional zero” (so named because “observation” cannot have value as zero but their function “mean” can). All items of each debriefing instrument were analyzed as an indicator of the OV of the CFI, and three subgroups of items were analyzed for F, A and U. The internal consistency of the index and sub-indices was assessed with Cronbach's alpha statistic. One item each from the F and A domains of DIP and DIP-R was omitted from data processing due to low internal consistency.
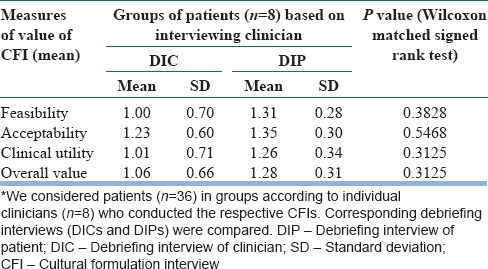
Means adjusted for the number of items were computed for patient, clinician and relative debriefing indices and sub-indices. Each patient was interviewed only once, but eight clinicians conducted 36 CFIs, thus exposing patients to random clinician effects. To adjust for clinician effects, we averaged patient and clinician debriefing scores by clinician and then applied paired t-test, and Wilcoxon matched signed rank test between corresponding means (i.e. mean for DIPs and DICs for each clinician). An example of analyses adjusted for clinician effects is presented in Table 1.
Table 1.
Pair wise analyses of DIC and DIP adjusted for clinician effects*
We used the Friedman test, a nonparametric equivalent of repeated measures ANOVA, to compare the domains of F, A and U within each of the three groups (clinicians, patients and relatives). For the 12 patients who were accompanied by relatives, our analysis grouped these interviews by the clinician interviewers for comparison of clinicians, patients and relatives in blocked triplets using the Friedman test. We also report the ungrouped analysis using the Kruskal–Wallis (K-W) test.
To determine whether the presence of a relative in the interview influenced the perceived value of the CFI by patients or clinicians, the debriefing interviews with relatives were compared with debriefing interviews without relatives for the index and sub-indices. We used the same approach for comparing the perceived value of the CFI for patients with a diagnosis of a common mental disorder (CMD) and a serious mental disorder (SMD).
Analyses adjusted for clinician effects had a smaller sample size, thus reducing the observed level of significance. Consequently, effect size, analogous to the “interaction tests” logic, rather than P values were compared.[15]
To determine whether clinician interview experience affected the perceived value of the CFI, we compared the debriefing data from first interviews of clinicians with the last interview of each clinician. Inasmuch as the first and third debriefing interviews of clinicians had additional questions, we also compared these debriefing interviews. For both, we used the Wilcoxon matched signed rank test.
We compared the perceived value of the CFI administered by each of the eight clinicians. Means of both DICs and DIPs, index and sub-indices, were compared for the interviews of these clinicians, using the K-W test.
To assess the influence of numeric sociodemographic variables for patients on the perceived value, we used the Spearman rank correlation coefficient to test for the strength of associations for age and years of schooling with the index and sub-indices. To consider the influence of gender, we compared the debriefing interviews between male and female patients and for male and female clinician interviewers, using the Mann–Whitney rank sum test.
To assess the impact of clinician experience on perceived value, the Spearman correlation coefficient was used to test the strength of association for years of experience, hours of cross-cultural training and frequency of treating patients from other cultural groups.
Ethical review
The ethics committee of the KEM hospital research center approved the project protocol.
RESULTS
A total of 10 clinicians participated – three men and seven women. Seven of the eight clinician interviewers were psychiatrists, and one was a psychiatric trainee. Two clinical psychologists who did not administer CFI interviews and three CFI clinician interviewers conducted debriefing interviews. 36 patients were recruited during the months of May-June 2012 yielding 36 DIPs, 12 DIP-R's, 36 DICs and 16 DIC_1-3 (extended first and third DIC interviews).
Cultural formulation interview patient and clinician sample
Twenty-two male and 14 female patients (mean age 38.28 years, standard deviation (SD) 12.46) were interviewed. Their mean education was 12.97 years (SD 4.03) and mean annual income was Rs. 218,399 (SD 148,940) (median Rs. 120,000) based on reports of 15 patients; others were unwilling or unable to provide income data. Only 10 of them had independent source of income, while 18 depended on others, and 8 had mixed sources of income. 21 patients were married; 12 had never married, and 3 were separated or divorced. Eighteen were employed, 8 unemployed, 4 each were homemakers and students, one was retired and another was a sanyasi (renounced household). Thirty-two spoke Marathi as mother-tongue, two Hindi, and one each spoke Guajarati and English.
Mean age of interviewing clinicians was 39.1 years, while that of debriefing clinicians was 32.4 years. All interviewing clinicians regarded themselves to be from mainstream society. They were Hindu and fluent in Marathi – the local vernacular, though one had English as the first language. Six interviewing clinicians identified the medical or psychiatric community as their primary or secondary social group/community, and two regarded this question as not applicable. Among the six clinicians, only one had named ‘family-friends group’ as background social group/community of affiliation. Despite relatively similar backgrounds, their reporting on cross-cultural training and frequency of seeing culturally different patients was widely variable. Clinicians had between 3 and 22 years of clinical experience (mean 13.25 [SD 7.36], median 13 years).
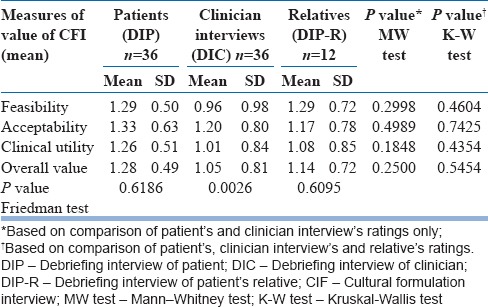
Comparing ratings of patients, clinicians and relatives
The mean values of F, A, U and OV were >0 for patients, clinicians and relatives. When the means obtained from DIPs and DICs (N = 36) were compared, patients and clinicians both rated the CFI feasible, acceptable and useful [Table 2]. The scores on the index of OV and sub-indices (F, A and U) were comparable among patients (N = 36), relatives (N = 12) and clinician-interviews (N = 36). Among patients and relatives, the index (OV) and sub-indices were comparable with each other. Among clinicians, however, the F subscale was lower than the other two (P = 0.0026, Friedman test).
Table 2.
Feasibility, acceptability and utility showing the value of CFI rated by patients, clinician-interviews and relatives
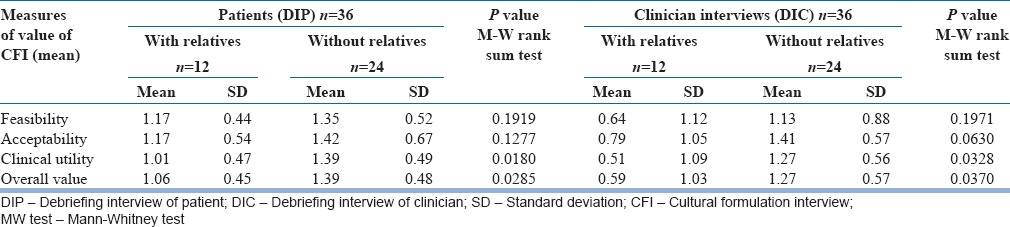
Presence of relatives
For the 12 interviews of patients with accompanying relative, differences in the OV and subscales did not differ significantly among clinician interviewers, patients and relatives, although clinicians reported the lowest values [Table 3]. Patients’ and clinicians’ ratings were also lower in interviews with an accompanying relative. Both patients and clinicians rated U and OV to be significantly higher in interviews without relatives [Table 4]. F and A were also greater, but not statistically significant.
Table 3.
Value of the CFI based on debriefing interviews with patients, clinicians and patient's relatives when present during CFI*
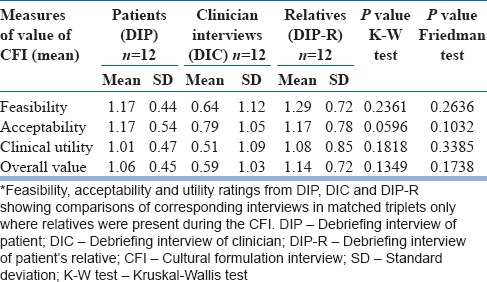
Table 4.
Value of the CFI based on debriefing interviews of clinicians and patients: Comparison with reference to presence of relatives
Clinical characteristics of patients
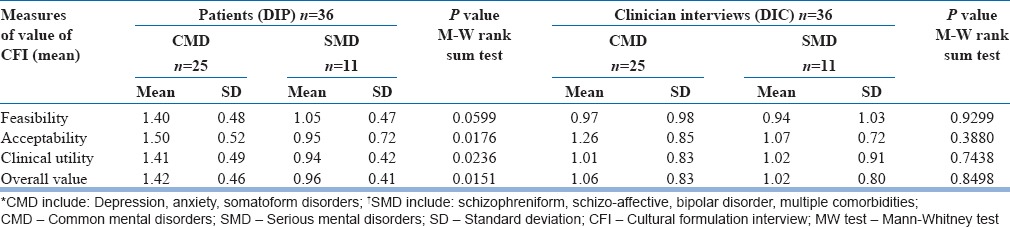
Twenty-five patients were diagnosed with a CMD, and 11 with a SMD. Patients with SMD rated A, U and OV significantly lower than those with CMD [Table 5]. F was marginally lower among patients with SMD. No differences were significant for clinicians.
Table 5.
Value of the CFI based on debriefing interviews of clinicians and patients: comparison of CMD* and SMD†
Of the 36 study patients, 22 were new cases (first or second clinic visit), and 14 were follow-up cases. Differences between debriefing ratings for new and follow-up patients were not significant, but the ratings for follow-up patients were consistently higher (not shown in the tables).
Clinician effects
We adjusted for clinician effects by grouping interviews according to clinician interviewers [Table 6]. Mean individual clinician ratings for OV ranged from −0.39 to 1.97, and for patients they ranged from 0.78 to 1.50. Ratings for F, A, U and OV differed significantly among clinicians, but not patients.
Table 6.
Value of the CFI based on debriefing interviews: Comparison among eight clinicians
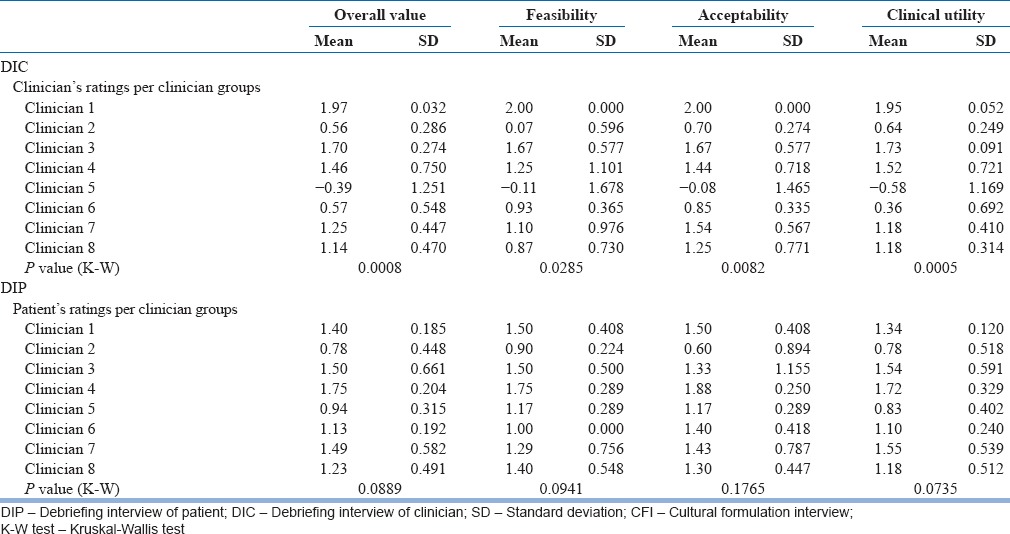
Comparisons of DIP and DIC ratings for OV, F, A and U adjusted for clinician effects [Table 1], did not change results from the unadjusted comparison [Table 2], and neither was significant. Clinician effects were also compared for the ratings with and without relatives, and for CMD and SMD. On considering, the confidence intervals for effect size, the direction and significance of the results was retained for both comparisons (not shown in Tables).
Responses to open-ended questions by patients
Most patients appreciated the CFI indicating that it helped them explain relevant background and vital concerns. They did not object to additional required time, and they did not feel the questions were intrusive. No patient or relative reported discomfort with any question. In fact, some patients said clinicians should ask more personal questions directly, including questions about sexual matters.
A 27-year-old lady with double depression indicated characteristic appreciation of the opportunity to elaborate concerns in the CFI.
“Usually I answer briefly; here I was able to talk at length.…I could talk about things that I wasn’t able to tell others. And because generally the questions were quite open and clarified when needed, I think I will get the right treatment.” She continued, “the question about my background-what happens at home etc., was the most helpful about the CFI. …Starting to disclose these things from the start were helpful…”
Other patients appreciated CFI questions prodding them to think in a useful way about their problems. They also felt the interview strengthened their relationship with the clinician.
Several patients acknowledged difficulty in naming their illness. A few patients had difficulty with questions about the role of cultural identity. “The one question about cultural background … I didn’t like it. I don’t think I had an answer to it. I don’t think others would understand it either.” However, most patients found these questions useful, especially after reconsidering with the debriefing clinician.
Several patients acknowledged the importance of speaking in their mother-tongue. “If [the questions] were in English it would have been difficult for me to express myself. It was in my mother-tongue, and hence it was easy. Although I understand these languages, expression would have been difficult.”
Clinicians typically appreciated the value of the CFI for clarifying the diagnosis, e.g. differentiating an anxiety disorder from a possibly paranoid disorder. They recognized complementary qualities of the CFI and standard diagnostic interview. For those emphasizing the priority of a categorical diagnosis, contextual details were less important than a diagnostic niche. “Initial diagnosis suggested by the CFI was perhaps adjustment disorder, but after the diagnostic interview I realized that the patient had a Schizophreniform Disorder.”
DISCUSSION
While it is important to acknowledge the relevance of race, ethnicity and culture in scientific reporting,[16] the CFI provides a significant advance for cultural psychiatry. It provides a means for operationalizing the outline for cultural formulation proposed in DSM-5, enabling its use for mainstream psychiatry. This study demonstrates the value of the CFI for clinicians, patients and patients’ relatives not just in North America, but also in a typical Indian urban outpatient psychiatry clinic serving lower middle-class patients. Although developed for the DSM-5 in North America, our findings show that the value of the CFI is not limited to North America.
Clinical value of the cultural formulation interview
Although the acknowledged value of the CFI did not differ significantly for clinicians, patients and accompanying relatives, clinicians’ ratings were uniformly lower than patients’ for feasibility, acceptability and utility [Table 2]. The sample may have been too small to identify statistically significant differences, if any. Further experience with the CFI will determine whether this consistent difference is significant. Analysis of the cross-site data, which provides a larger sample for analysis may show either a significant finding across sites or identify cross-site differences, depending on effect size.
It may be more remarkable, however, that this difference was not significant than if it had been, inasmuch as several clinician interviewers were skeptical at the outset about the value of the CFI. They were concerned about the additional time it would require and hesitant about conducting such an interview on their first meeting with a patient before establishing a rapport. Some clinicians do not recognize the relevance of culture in their clinical practice and are unwilling to consider their own. On completing the clinician demographic form, two psychiatrists responded to a question about their cultural identity with “not applicable.” Experience with the CFI, however, appeared to enhance the regard of most clinicians for the value of the CFI. Nevertheless, it was not so for all, and it was notable that the valuation of the CFI differed significantly and substantially among the eight clinician raters [Table 6]. One of them had a consistent negative rating. Although this had an effect on the overall valuation by patients (Spearman correlation 0.81, P = 0.015), patients did not vary as much as clinicians, and no patients gave a negative valuation on the debriefing. This shows that clinicians are more likely to differ substantially, and it is important to consider clinician effects on the value of the CFI. But patients are more consistent in their positive regard.
Role of relatives
Both patients and clinicians rated the OV and particularly the clinical utility of the CFI higher in the absence of relatives [Table 4]. Although relatives may add useful information, it appears that their presence nevertheless imposes limitations on the diagnostic ease for clinicians and the empathic quality of the CFI for patients. Perhaps patients become defensive with relatives participating in the session, and their presence may limit patients’ capacity to discuss the family contributions to the perceived nature and causes of presenting problems. Narratives of relatives, however, indicated their satisfaction with the CFI. They appeared to value the opportunity to participate in the evaluation, which may help them fulfil responsibilities as caretakers. Although the differences are small, relatives’ ratings have been higher not only than the patients whom they accompanied, but also than the clinicians themselves [Table 3]. This explains how relatives glean more benefit from the CFI than the clinicians or patients, who should not be denied that benefit considering their role as co-therapists.
Relatives also indicated puzzling aspects of patients’ problems for which they wanted clarification, e.g. some suggested additional questions about why patients wanted to die, or why they behaved abnormally despite supportive caretaking. The presence of relatives provides both an opportunity to discuss the role of relatives and a challenge for the clinician to manage complex interactions in which stigma, the problematic role of relatives and limited privacy constraining frank discussion are relevant in varying degrees for different assessments. Findings suggest the need to consider and to plan for the presence of a relative in a diagnostic interview. Clinicians need to protect the privacy of their patients, even in the relatively more sociocentric Indian society, but with care not to inappropriately burden or blame families whose capacity for caretaking is an essential resource.
Role of the nature of illness
Although clinicians made little or no distinction in the value of the CFI for patients with diagnoses of serious and common mental disorders, patients with CMDs valued nearly all aspects of the CFI more highly than patients with SMDs [Table 5]. Even though, ratings for the latter group remained positive, limited capacity for insight and abstraction, which are more typically features of SMDs, appear to limit appreciation of the value of the CFI.
Sociodemographics and clinical characteristics of patients
It is notable that years of education made no difference to ratings of the value of the CFI for patients. Findings also indicated the absence of gender differences. Further attention to educational and gender differences to assess cultural affects is warranted, however, from pooled and cross-site analyses of CFI data, and from consideration of same-sex and cross-sex interviews for clinicians and patients.
Ordinal sequence of cultural formulation interview and the clinician factors
A paired t-test analysis showed that first and third CFI clinician interviews, and their first and last interviews were rated similarly. These findings indicated that the level of training for use of the CFI was adequate and appropriate.
Limitations
The small sample size limited our ability to assess patient and clinician characteristics that affect their ratings of the value of the CFI. Questions about the clinical and cultural experience of clinicians require further consideration, and further attention to clinician effects is also warranted. Our preliminary analyses of clinician effects, based on grouping and comparing responses of the eight clinicians indicate similar trends, but more difficulty in demonstrating the significance of our findings reported here. Further analysis of the pooled sample from collaborating sites will provide an opportunity to assess clinician and site-specific effects.
CONCLUSIONS
Development of the CFI has been responsive to fundamental questions about the cultural context of the clinical validity of psychiatric practice. The impact of inexorable processes of urbanization and globalization, and the global aspirations of the DSM have indicated a need for attention and validation of a patient-centered approach to clinical assessment–not only in North America but other culturally diverse settings. This study in Pune, India, like other international studies of the group, demonstrated the value of the CFI. It showed that to communicate mental health problems; patients’ preferences for explaining their own priorities is an important matter not only for them but also for clinicians whom they consult for help.
This study showed that patients, clinicians and accompanying relatives agreed in their positive assessment of the value of the CFI overall and with respect to its feasibility, acceptability and clinical utility. The inter-rater reliability of the CFI among these stakeholders and qualitative accounts explaining why it was valued argue for its use in psychiatric training and practice. The clinical value of the CFI may also extend well beyond psychiatry in other areas of clinical practice for which the quality of a therapeutic alliance and frameworks attentive to patients’ experience, meaning and behavior are no less important. The capacity of the CFI to transcend the clinical, geographical and cultural boundaries of patient-clinician relationships for enhanced clinical effectiveness recommends its further consideration and use as a contribution of cultural psychiatry to mainstream practice.
ACKNOWLEDGMENTS
The CFI was developed by the cultural issues subgroup of the Culture and Gender Group for DSM-5. Dr. Roberto Lewis-Fernandez, Dr. Neil Aggarwal, Dr. Ladson Hinton and Dr. Christian Schindler provided valued comments on an earlier version of the manuscript. The King Edward Memorial Hospital and Research Centre, Pune, sanctioned the study, provided logistical support and funds for patient compensation and data management. Draft Hindi translations were provided by Dr. Smita Deshpande (Ram Manohar Lohia Hospital, Delhi) and Dr. Shubhangi Parkar (KEM Hospital, Mumbai). Dr. Vaishali Naik and Ms. Priya Dabak assisted with translations of the Marathi and Hindi instruments. We thank consultants of the department of psychiatry for graciously foregoing their share of compensation for data management and staff of the department for help and coordination. We are grateful to patient participants for sharing their stories, for their enthusiasm and generosity in support of the aims and interests of the study. We acknowledge the editorial contributions of Ms. Neha Chitgopekar, Ms. Ankita Deshmukh and Ms. Shraddha Deo on early drafts of the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Röhricht F, Gudi A, Lewis-Fernández R. Medically unexplained physical symptoms masking (cenesthopathic) schizophrenia: A case series. J Psychiatr Pract. 2010;16:258–64. doi: 10.1097/01.pra.0000386913.85182.b6. [DOI] [PubMed] [Google Scholar]
- 2.Cabassa LJ, Blanco C, Lopez-Castroman J, Lin KH, Lui SM, Lewis-Fernández R. Racial and ethnic differences in diabetes mellitus among people with and without psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Gen Hosp Psychiatry. 2011;33:107–15. doi: 10.1016/j.genhosppsych.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis-Fernández R, Aggarwal NK, Bäärnhielm S, Rohlof H, Kirmayer LJ, Weiss MG, et al. Culture and psychiatric evaluation: Operationalizing cultural formulation for DSM-5. Psychiatry. 2014;77:130–54. doi: 10.1521/psyc.2014.77.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis-Fernández R, Aggarwal NK. Culture and psychiatric diagnosis. Adv Psychosom Med. 2013;33:15–30. doi: 10.1159/000348725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aggarwal NK. Reassessing cultural evaluations in geriatrics: Insights from cultural psychiatry. J Am Geriatr Soc. 2010;58:2191–6. doi: 10.1111/j.1532-5415.2010.03139.x. [DOI] [PubMed] [Google Scholar]
- 6.Ware NC, Kleinman A. Culture and somatic experience: The social course of illness in neurasthenia and chronic fatigue syndrome. Psychosom Med. 1992;54:546–60. doi: 10.1097/00006842-199209000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Abbey SE, Garfinkel PE. Neurasthenia and chronic fatigue syndrome: The role of culture in the making of a diagnosis. Am J Psychiatry. 1991;148:1638–46. doi: 10.1176/ajp.148.12.1638. [DOI] [PubMed] [Google Scholar]
- 8.Weiss M. Explanatory Model Interview Catalogue (EMIC): Framework for comparative study of illness. Transcult Psychiatry. 1997;34:235–63. [Google Scholar]
- 9.Weiss MG, Doongaji DR, Siddhartha S, Wypij D, Pathare S, Bhatawdekar M, et al. The Explanatory Model Interview Catalogue (EMIC). Contribution to cross-cultural research methods from a study of leprosy and mental health. Br J Psychiatry. 1992;160:819–30. doi: 10.1192/bjp.160.6.819. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd KR, Jacob KS, Patel V, St Louis L, Bhugra D, Mann AH. The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychol Med. 1998;28:1231–7. doi: 10.1017/s0033291798007065. [DOI] [PubMed] [Google Scholar]
- 11.Paralikar VP, Deshpande SN, Jadhav S, Weiss MG. Indian contribution to the cultural formulation interview and the DSM-5: Missing details from the position paper. Indian J Psychiatry. 2013;55:307–8. doi: 10.4103/0019-5545.117160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paralikar V, Agashe M, Sarmukaddam S, Deshpande S, Goyal V, Weiss MG. Cultural epidemiology of neurasthenia spectrum disorders in four general hospital outpatient clinics of urban Pune, India. Transcult Psychiatry. 2011;48:257–83. doi: 10.1177/1363461511404623. [DOI] [PubMed] [Google Scholar]
- 13.Top 10 Urban Agglomeration of India by Population 2011. The Indian Census. 2011. [Last cited on 2013 Nov 07]. Available from: http://www.census2011.co.in/facts/topurbanpopulation.html .
- 14.Pune City Census 2011 data. [Last cited on 2013 Nov 07]. Available from: http://www.census2011.co.in/census/city/375-pune.html .
- 15.Matthews JN, Altman DG. Statistics notes. Interaction 2: Compare effect sizes not P values. BMJ. 1996;313:808. doi: 10.1136/bmj.313.7060.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis-Fernández R, Raggio GA, Gorritz M, Duan N, Marcus S, Cabassa LJ, et al. GAP-REACH: A checklist to assess comprehensive reporting of race, ethnicity, and culture in psychiatric publications. J Nerv Ment Dis. 2013;201:860–71. doi: 10.1097/NMD.0b013e3182a5c184. [DOI] [PMC free article] [PubMed] [Google Scholar]


