Abstract
The Emergency Medical Dispatcher (EMD) receiving a call via 911 is the first point of contact within the acute care system and plays an important role in early stroke recognition. Published studies show that EMDs' diagnostic accuracy of stroke need to be improved. Therefore, the National Association of Emergency Medical Dispatchers (NAEMD) implemented a stroke diagnostic tool modelled after the Cincinnati Stroke Scale across 3000 cities world-wide. This is the first time a diagnostic tool that requires callers to test physical findings and report those back to the EMD has been implemented. However, the ability of EMDs and 911 callers to use this in real time has not been reported. Our goal in this pilot study was to determine the feasibility of an EMD applying the Cincinnati Stroke Scale tool during a 911 call, and to report the time required to administer the tool.
Introduction
Stroke is a neurological emergency and treatment is time dependent. One pathway posited to increase t-PA treatment rates is for emergency medical service providers to recognize stroke early [1] and triage patients to primary stroke centres. However, we and others have reported that the first link in the communications chain -- early recognition of stroke by emergency medical dispatchers (EMDs) using Card 28, the Medical Priority Dispatch System protocol could be as low as 40%.[2,3,4] Accordingly, the National Academy of Emergency Medical Dispatchers (NAEMD) recently designed and implemented a stroke diagnostic tool modelled on the Cincinnati Stroke Scale for use during interrogation of a 911 call by EMDs. While the Cincinnati Stroke Scale was developed to improve stroke recognition by paramedics in the field, the ability of EMDs to use this tool during call interrogation to better recognize stroke has not been studied.[5]
The objective of this pilot study was to determine the feasibility of Cincinnati Stroke Scale application by EMDs and the ability of EMDs to collect responses from the caller/subject to make a determination of stroke.
Methods
This prospective pilot cohort study was approved by the Committee of Human Research, University of California, San Francisco and was conducted in the County Communication Center Santa Clara, California, USA during a 3-week period in April – May 2010. We studied EMDs in the County Communication Center who completed a training program on use of Cincinnati Stroke Scale for stroke-related calls.
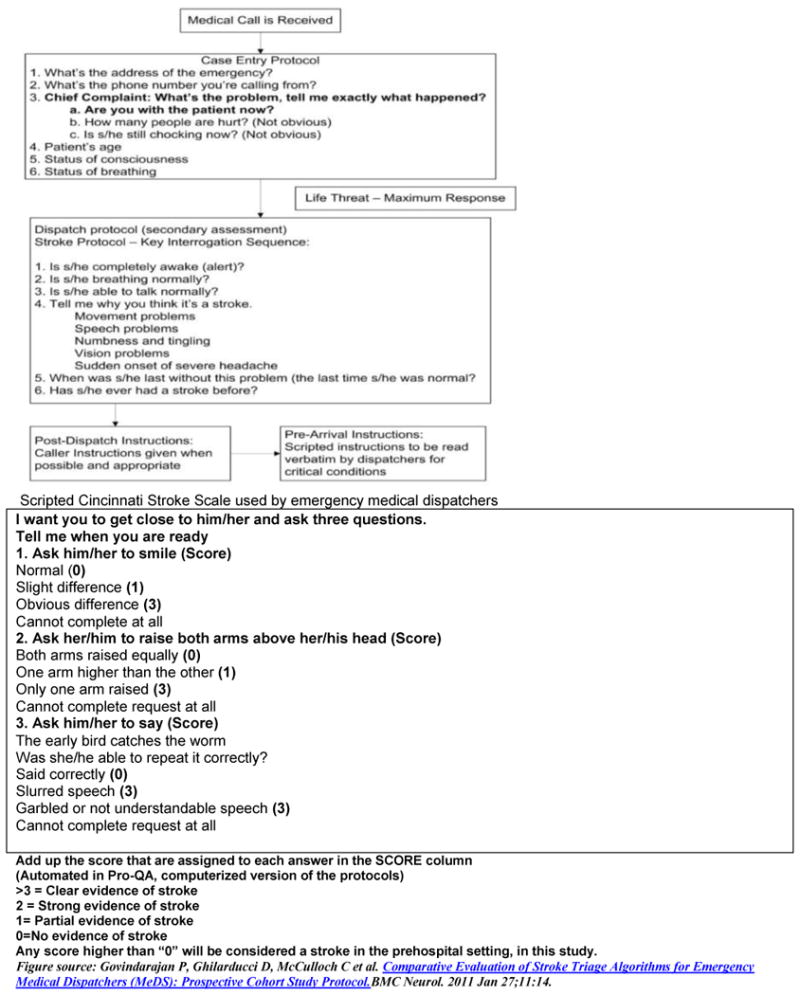
The details of the study protocol have been published elsewhere.[6]. Briefly, all medical aid calls to the county communication center were interrogated by EMDs using Medical Priority Dispatch System protocols. If the caller chief compliant was suggestive of stroke, Card 28 was used to complete the interrogation. Card 28 has two sets of questions which include the case entry questions and key interrogation questions [Figure 1]. The case entry questions preceded use of key questions in the computerized version of Card 28 and were used to determine the need for ambulance dispatch prior to launch of stroke specific questions. Key interrogation sequence was used to recognize stroke symptoms. If the caller' answers to the key questions were suggestive of stroke, EMDs assigned a dispatch determinant of stroke. This was followed by ambulance response and use of the scripted Cincinnati Stroke Scale. If any of the responses to the Cincinnati Stroke Scale were positive, EMDs recorded and confirmed an assessment of stroke.
Figure 1. Card 28 protocol in the Medical Priority Dispatch Systems Protocol used by emergency medical dispatchers.
During the study period, all medical aid calls received by EMDs were eligible. Of the eligible calls, we included calls made by subjects > 18 years of age. We excluded calls that could not be completely interrogated with Card 28 and Cincinnati Stroke Scale due to need for an immediate ambulance response, as determined by EMDs. Third party calls from subjects not in close proximity to the patient were also excluded. All responses to Card 28 questions and the Cincinnati Stroke Scale were recorded in the computer assisted dispatch (CAD) system. We defined the study outcome measures as follows:1) Elapsed time from time of first phone ring at county communication center to completion of Card 28, 2) Elapsed time from first phone ring at the county communication center to completion of Cincinnati Stroke Scale 3), and Completion of all 3 Cincinnati Stroke Scale protocol questions.
Data analysis was performed and descriptive statistics were reported.
Results
During the study period, the County Communication Center received 1143 medical aid calls. Of these calls, 37 (3%) were identified by EMDs as having symptoms suggestive of stroke, and were interrogated using Card 28. Of those calls, 28 (76%) met inclusion criteria i.e., callers were aged >18 years, were in close proximity to the patient, and could administer the Cincinnati Stroke Scale tool. None of the calls required an ambulance response prior to completion of Card 28 key questions. Twenty of 28 (71%) calls were interrogated by EMDs who had completed training of the Cincinnati Stroke Scale study procedures. Of these 20 calls, all 3 Cincinnati Stroke Scale questions were completed in 12 calls (60%). The reasons stated by EMDs for not completing the Cincinnati Stroke Scale questions included patient's impaired level of alertness that affected comprehension of Cincinnati Stroke Scale, and caller inability to administer the tool. The mean elapsed time from first ring to case completion using Card 28 was 4.43 minutes (range 3.36 -7.06 minutes) and the mean time from first ring to completion of the entire interrogation including Cincinnati Stroke Scale was 5.08 minutes (range 4.43 – 6.38 minutes).
Discussion
Overall, our study results show that EMDs with varying levels of experience are able to both interrogate a call and apply the Cincinnati Stroke Scale. In addition, layperson-callers were also able to comply with the instructions provided by EMDs during a critical situation and accurately relay the findings back to the EMDs in a majority of the calls (12/20=60%). In addition to ease of use, our second finding is that the mean time required to administer the Cincinnati Stroke Scale is only about 30 seconds more than the Card 28 protocol. This is consistent with findings reported in a simulation study by Brice et al,[7,8] in which the investigators reported an interrogation time of about 90 seconds, confirming that the new protocol will likely not cause major dispatch delays for other emergent calls. While the performance characteristics of the Cincinnati Stroke Scale and the clinical outcomes following implementation of the new tool remains to be determined, the feasibility of use in an emergency setting and lack of time delays from use of Cincinnati Stroke Scale has been demonstrated in this study. To our knowledge, this is the first study reporting feasibility and safety of Cincinnati Stroke Scale in real time after implementation of the tool world-wide.
Limitations of our study include that this was not a multi-site study and therefore may have limited generalizability to other dispatch centres. Also, the study site has remained a centre of excellence for the past 8 years and therefore the rates of adherence to the protocol and the scripted version of Cincinnati Stroke Scale may be higher compared with non-accredited dispatch centres. Third, this is only a pilot feasibility study evaluating the ability of EMDs to use the Cincinnati Stroke Scale. Due to the size of the study sample, these results should not be relied upon to modify local dispatch criteria for stroke. The second phase of this study, now in progress, aims to evaluate the diagnostic accuracy of Cincinnati Stroke Scale as a stroke tool for EMDs and report clinical outcomes after implementation of the Cincinnati Stroke Scale. Results will be shared with the prehospital community after completion of the study.
Conclusions
In this single site pilot study conducted in a center of excellence, , EMDs and layperson-callers were able to apply the Cincinnati Stroke Scale to subjects with symptoms of stroke. Layperson-callers capably interpreted the findings and relayed them back to EMDs. While these pilot findings favour recent implementation of Cincinnati Stroke Scale globally, the investigators acknowledge the limitations of the study and also recognize a strong need for a large scale study to assess the relative diagnostic accuracies of Card 28 and Card 28 combined with Cincinnati Stroke Scale for stroke recognition.
Acknowledgments
The authors thank the National Academy of Emergency Medical Dispatchers for releasing the MPDS version 12 to the authors for the pilot trial, the emergency medical dispatchers of the Santa Clara County Communication Center for participating in the study, and Amy J. Markowitz JD, for editorial assistance.
Funding: This publication was supported by NIH/NCRR UCSF-CTSI Grant Number UL1 RR024131. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Dr. Govindarajan is also supported by K08 HS 017965-02 – Agency of Healthcare Research and Quality and the CTSI – K Program, University of California San Francisco.
Footnotes
Competing Interests: None
Contributor Information
Prasanthi Govindarajan, 505 Parnassus Avenue L 126 Mail Code 0208, University of California, San Francisco Medical Center, San Francisco, CA 94143-0208.
Natalie T. DeSouza, Department of Emergency Medicine, University of California San Francisco, San Francisco, CA, USA.
Jessica Pierog, Division of Emergency Medicine, Stanford University Medical Center, Stanford, CA, USA.
David Ghilarducci, American Medical Response, Santa Cruz, CA, USA.
S. Claiborne Johnston, Department of Neurology, Epidemiology and Biostatistics, University of California San Francisco, San Francisco, CA, USA.
References
- 1.California Acute Stroke Pilot Registry (CASPR) Investigators. Prioritizing interventions to improve rates of thrombolysis for ischemic stroke. Neurology. 2005 Feb 22;64(4):654–9. doi: 10.1212/01.WNL.0000151850.39648.51. [DOI] [PubMed] [Google Scholar]
- 2.Ramanujam P, Guluma KZ, Castillo EMet, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics--San Diego experience. Prehosp Emerg Care. 2008 Jul-Sep;12(3):307–13. doi: 10.1080/10903120802099526. [DOI] [PubMed] [Google Scholar]
- 3.Buck BH, Starkman S, Eckstein M, et al. Dispatcher recognition of stroke using the National Academy Medical Priority Dispatch System. Stroke. 2009 Jun;40(6):2027–30. doi: 10.1161/STROKEAHA.108.545574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Porteous GH, Corry MD, Smith WS. Emergency medical services dispatcher identification of stroke and transient ischemic attack. Prehosp Emerg Care. 1999 Jul-Sep;3(3):211–6. doi: 10.1080/10903129908958939. [DOI] [PubMed] [Google Scholar]
- 5.Kothari RU, Pancioli A, Liu T, et al. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med. 1999 Apr;33(4):373–8. doi: 10.1016/s0196-0644(99)70299-4. [DOI] [PubMed] [Google Scholar]
- 6.Govindarajan P, Ghilarducci D, McCulloch C, et al. Comparative Evaluation of Stroke Triage Algorithms for Emergency Medical Dispatchers (MeDS): Prospective Cohort Study Protocol. BMC Neurol. 2011 Jan 27;11:14. doi: 10.1186/1471-2377-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurwitz AS, Brice JH, Overby BA, et al. Directed use of the Cincinnati Prehospital Stroke Scale by laypersons. Prehosp Emerg Care. 2005 Jul-Sep;9(3):292–6. doi: 10.1080/10903120590962283. [DOI] [PubMed] [Google Scholar]
- 8.Liferidge AT, Brice JH, Overby BA, et al. Ability of laypersons to use the Cincinnati Prehospital Stroke Scale. Prehosp Emerg Care. 2004 Oct-Dec;8(4):384–7. doi: 10.1016/j.prehos.2004.05.004. [DOI] [PubMed] [Google Scholar]


