Abstract
Objective. To assess the effect of using simulation in pharmacy student training on correct device technique.
Methods. A single-blinded, repeated measures, parallel group design study was conducted in 2011, involving all final-year pharmacy students in year 5 (final year) enrolled in the Clinical Pharmacy and Therapeutics course. Students were assessed on device technique at baseline based on previously published checklists for Diskus (DIS), Turbuhaler (TH), and pressurized Metered Dose Inhaler (pMDI). Students were randomly assigned to 2 groups: Intervention A, which included supervised hands-on education in groups and peer assessment/education; and Intervention B, which included supervised hands-on education in groups, peer assessment/education, and a simulated scenario counseling real asthma patients. The simulation involved groups of 6 students counseling 3 asthma patients on inhaler device technique. The counseling involved verbal information and physical demonstration until the patient performed all steps correctly. Student assessments on device technique were repeated 1 week postintervention.
Results. At baseline, none of the students in Intervention A (n=54) or Intervention B (n=55) performed correct technique for any of the 3 devices. One week following the intervention, a significantly higher proportion of students in Intervention B demonstrated correct technique for the Diskus, Turbuhaler, and pMDI (60.0%, 70.9%, and 69.1%, respectively) than did students in Intervention A (27.8%, 40.7%, and 42.6%, respectively, p<0.005).
Conclusion. Engaging pharmacy students with real asthma patients in a simulated scenario involving correct device technique education resulted in better device technique demonstration skills among students.
Keywords: Simulation, pharmacy education, device technique, asthma, Jordan
INTRODUCTION
Currently, treatment of 30 million cases of asthma worldwide, with 22 million from the United States alone, involves mainly inhalation therapy, with numerous inhalers on the market.1,2 To achieve optimal effectiveness of this therapy, correct device technique is vital.3,4 Inhalation therapy involves commonly used inhalers: pressurized metered dose inhalers (pMDIs) and dry powder inhalers (DPIs). The Diskus (GlaxoSmithKline, Philadelphia, Pennsylvania) and Turbuhaler (AstraZeneca Pharmaceuticals, Wilmington, Delaware), similar to the Flexhaler, are the most commonly used DPIs.5,6
Incorrect device technique with both pMDIs and DPIs is a common issue among asthmatic patients.3,4,7 In Jordan, a majority of patients and pharmacists failed to demonstrate the correct use of these devices.8,9 This is similar to other trial results in more developed countries, such as Australia and the United States.9,10 Incorrect use can lead to the delivery of sub-therapeutic doses of the medication and suboptimal benefits from the therapy, resulting in poor asthma control, increased emergency room visits, life threatening asthma exacerbations, and higher costs.11,12
As the potentially last health care providers to see a patient before inhaler use, pharmacists are in a position to provide not only patient education, but also follow up, as patients visit pharmacists much more frequently than physicians (eg, at monthly refills).13 Studies have shown that engaging pharmacists in training patients on correct device technique leads to more frequent counseling and improved asthma control and quality of life.4,14 Patients come back to the pharmacy for their inhaler refill without a physician’s prescription, giving the pharmacist the sole opportunity to review device use on continuous basis.
Better methods for educating pharmacy students on inhaler technique is needed.15 For the majority of pharmacists, their first inhaler device educational experience is in pharmacy schools, where preliminary knowledge is obtained.16 Many educational strategies aimed at optimizing inhaler device demonstration skills by students, from physical demonstration training and hands-on educational workshops to computer-based learning tutorials, have been researched.15,17 These strategies led to better device technique demonstration skills, but not enough to result in pharmacists competent in patient training.15
Using real patients in a simulated educational environment in the health sciences has yielded positive results.18,19 Simulation-based learning in pharmacy schools is one of the active-learning strategies recently recommended by the Accreditation Council for Pharmacy Education’s Standards.20 In terms of supervised, in-school education on device technique, no previous study has examined the effectiveness of using real patients in this area. Utilizing this educational method may add an important new perspective to education, considering pharmacists’ expanding role in optimizing patient medication use and health outcomes.21
At Applied Science University (ASU) in Amman, Jordan, Clinical Pharmacy and Therapeutics is a unit of study in the fifth year of the bachelor of pharmacy curriculum (a 5-year degree). The key focus of the course unit is to enable students to acquire knowledge regarding the therapeutic management of common disease states. Part of the objectives of the unit involves students practicing the manipulation of self-care medical devices for different therapeutic areas (eg, inhalers for asthma). The aim of this study was to compare the effect of 2 different educational interventions on correct device technique demonstration skills among students in this course.
DESIGN
This repeated measures, parallel group design study, approved by the ASU Ethics Committee, was conducted during the Clinical Pharmacy and Therapeutics tutorial classes in 2011. The study included all students enrolled in these classes in the fifth year (final year) of the ASU bachelor of pharmacy curriculum. Students were divided into 6 groups. Each student attended one Therapeutic and Clinical Pharmacy tutorial per week for 10 weeks, over which tutorials were provided in respiratory health, cardiovascular disease (hypertension, ischemic heart disease, and cardiac failure), endocrinology (diabetes and thyroid disorders), infectious diseases, and in areas of communication such as barriers to communication, counseling, and patient perspectives on illness. Each 3-hour tutorial was facilitated by 1 tutor (a community pharmacist) and 1 lecturer (a PhD in clinical pharmacy and expert in inhaler device technique education), were spread throughout the week, and included problem-based learning approaches for pseudo cases, as well as appropriate hands-on and small group activities. Information regarding medical devices, such as insulin pens and inhalation devices, were given in written format and explained orally during the relevant topic tutorial. Student evaluation was based on an end-of-semester oral assessment, multiple-choice and written examinations, and tutorial participation.
In the sixth week of the semester, following lectures on respiratory diseases, students were told about the study and asked to complete informed consents. Students received product information leaflets for 3 devices (DIS, TH and pMDI) and were given 15 minutes to read the leaflets and prepare to demonstrate their baseline technique for each of the devices to the tutor. At this stage, participants were not instructed on how to use the placebo devices or how to use the written information provided. Participants utilized their own learning techniques.
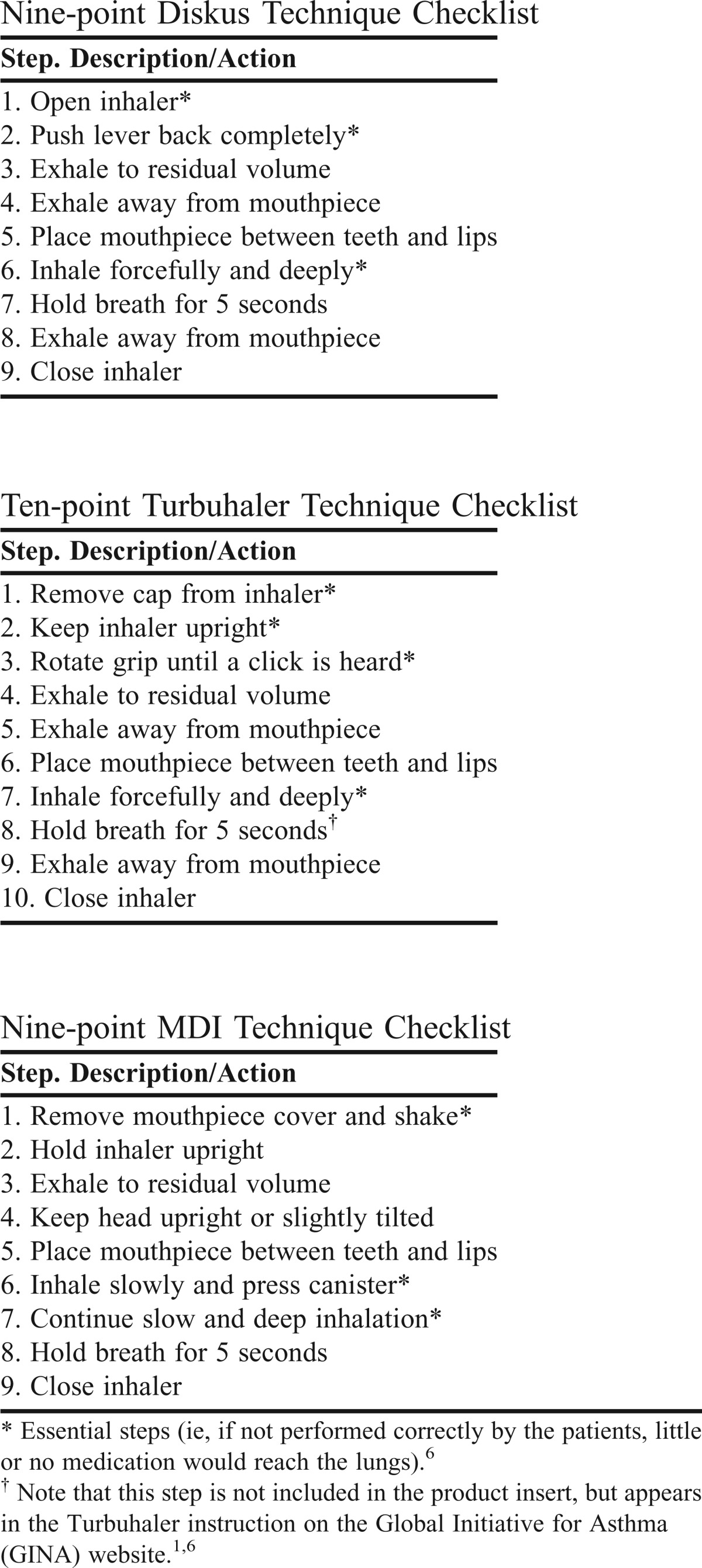
All students underwent baseline device technique assessment for the 3 inhaler devices based on a previously published step checklist for each device (see Appendix 1). The assessment was completed for all participants in a random order, with the assessor grading students at the time of demonstration. Participants were awarded 1 point for each step they performed correctly. Students were considered to have “correct technique” if they completed all steps outlined in the checklists correctly. Following baseline, all students were randomized into Intervention A or B. Based on 6 predetermined tutorial groups, 3 groups were randomly allocated to Intervention A (n=54) and 3 to Intervention B (n=55), with 18 students in each class. Intervention A consisted of supervised hands-on education in groups, plus peer assessment/education. Intervention B consisted of supervised hands-on education in groups, plus peer assessment/education, plus simulated scenario counseling a real asthma patient on correct inhaler technique. Participants in each class were randomly assigned to groups of 5-6 students by a computer-generated list to avoid student self-grouping.
A questionnaire was designed to collect data regarding students’ baseline demographic characteristics and other data including age, gender, years spent in undergraduate study, hours in practice, and place of pharmacy training (community pharmacy area in Amman or hospital ward), previous personal use of any of the devices, previous inhaler technique experience, and confidence level (a choice among “very confident,” “confident,” and “not confident”) in counseling patients on each of the devices.
The questionnaire was evaluated by 3 clinical pharmacists and then by pharmacy students (n=15) to test the clarity of the questions. Student views and comments were considered by the researchers and incorporated where appropriate into the final version. To assess test-retest reliability, the questionnaire was administered on 2 occasions to 15 randomly selected pharmacy students. The second testing took place 2 weeks after the first one. This set of data was not included in the final analysis. Test-retest reliability was calculated using Spearman’s rho, and a rho-value of 0.93 implied acceptable test-retest reliability. As English is the official language of education for all health care professionals in Jordan, the questionnaire was administered in English.
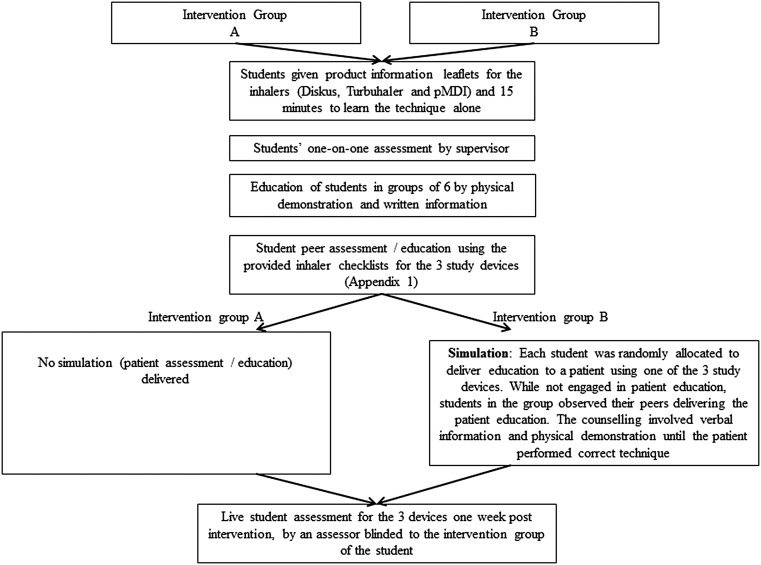
All students in Intervention A and B were required to complete the questionnaire regarding demographics and inhaler device use. Students then worked in their allocated groups and were given 20 minutes to perform hands-on education on device technique in group format, followed by peer assessment and education (Figure 1). For hands-on education, each student practiced using each of the devices and demonstrated the technique for one to the rest of the group under the supervision of an instructor. The instructor decided which of the 3 devices each student had to demonstrate, based on a predetermined random selection and explained to each group the importance of each step and its clinical effect using visual aids. Every 2 students took turns assessing and correcting each other on device technique for the 3 inhalers using the checklists provided (Appendix 1).
Figure 1.
Intervention Group A and Intervention Group B educational sequencing.
Only Intervention B performed the simulation. Three asthma patients, each using one of the inhaler devices, were recruited into the study. The patients provided informed consent forms. Patients were required to be older than 18 years, with physician-diagnosed asthma and self-administered inhaler preventative therapy by DIS, TH or pMDI. Students were introduced to the 3 asthma patients and, in their original groups of 6, educated the patients on device technique. Each student was randomly allocated to educate one of the patients using 1 of the 3 devices. Those students in the group not engaged in the patient education observed the patient counseling, which involved verbal information and physical demonstration until the patient performed all steps in each checklist correctly. Students were allowed approximately 5 minutes with each patient, an amount based on previous publications.2 This part of the class took about 40 minutes.
To avoid the effect of familiarity with the device technique because of previous exposure in the same class, each patient was asked to “‘act out” mistakes in device technique according to a scenario preplanned by the researcher. Besides demonstrating the inhaler technique steps incorrectly during their first assessment, patients were also asked to perform some incorrect techniques during the second and third assessments as well.
Students educated the patients using the specialized “Show and Tell Device Technique Education Protocol” based on our previously published methods,3,4 going through each step on the checklist to describe and demonstrate correct use. This cycle of assessment and counseling was repeated up to 3 times if necessary, until the patient had correct technique on all steps (Figure 1). Following the simulated scenario, the researcher debriefed students in each group on the mistakes each of the patients made.
One week following delivery of the intervention, the assessor who completed the baseline assessment performed random-order, one-on-one student assessment. The assessor was blinded to the intervention grouping of the students. Finally, students were asked to complete again the part of the questionnaire regarding their confidence level on counseling patients on each of the study inhaler devices.
Four weeks following baseline, an open invitation was extended to 15 students in Intervention B, randomly selected by the researcher, to attend a focus group session to elicit comments about the effectiveness of the simulation in which they participated. A series of open-ended questions were prepared as a basis for the semi-structured interview format, and the session was facilitated by the researcher. The questions were: (1) How did you feel about the inhaler technique education process being conducted in class with the engagement of real patients with asthma? (2) What did counseling real asthma patients during the tutorial class add to your experience? (3) Would you endorse the engagement of real patients in other therapeutic tutorials that consist of hands-on education involving other pharmaceutical devices?
Data were analyzed using the SPSS version 17 (SPSS, Chicago, Illinois). The mean ± standard deviation values and the 95% confidence interval (CI) were used to describe the normally distributed continuous data (normality of distribution was determined using the Kolmogorov-Smirnov test). Proportional data were analyzed using Pearson’s chi-square test (or Fisher’s exact test). For all statistical analysis, p values of 0.05 or less were considered significant. Number of students in each intervention group (A and B) performing correct technique (all steps in the device technique checklist done correctly) was compared for each device. Mean device scores were also calculated (score out of 9 for DIS and pMDI, and out of 10 for the TH), and differences between intervention groups were compared using the Mann-Whitney u test. In order to determine the effect of the simulation, in association with other factors, on correct inhaler device technique, a logistic regression analysis was performed. The dependent variable was correct technique following intervention. Independent variables included type of intervention (Intervention A or B), technique at baseline, gender, age, previous pharmacy experience (hours), years spent to date in undergraduate pharmacy studies, previous device use, and confidence in demonstrating the use of the device before intervention. Data from recordings of focus group conversations were analyzed thematically.
RESULTS
No significant difference was shown between participants in Intervention A (n=54) and Intervention B (n =55) regarding demographic characteristics, except for gender (Table 1), as there were more females in Intervention A than in Intervention B.
Table 1.
Characteristics and Demographic Information of Participants in Interventions A and B at Baseline
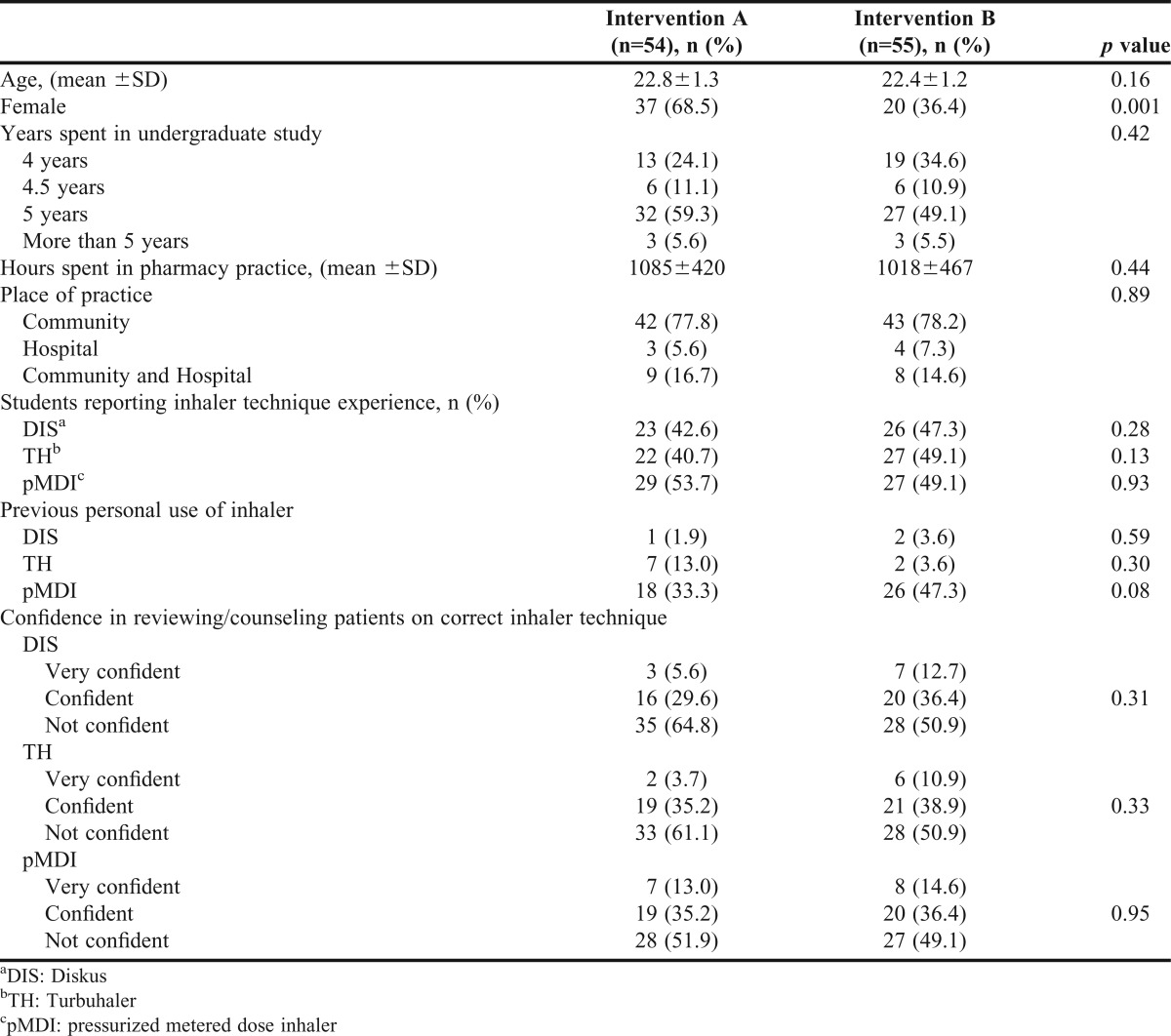
Regarding years spent in undergraduate studies (4 years for accelerated students, 5 years, the expected period, or more, for students who had failed previously), 54.2% of the students were in their fifth year—the final year of the pharmacy curricula. Nearly 30% (29.4%) were in their fourth year, which could indicate a higher level of achievement due to faster completion of preliminary subjects. Only 5.6% students exceeded the 5-year plan for their degree and were either repeating the topic or delayed for other reasons.
The majority of students reported having practiced more than 1000 hours in community and/or hospital pharmacies prior to study entry (Intervention A: 72.2%; Intervention B: 63.6%). Students’ practice hours ranged from 147 to 1775 for Intervention A and from 120 to 1490 hours for Intervention B.
More than half of the students (52.92%) reported no previous inhaler technique experience with the 3 devices. Students who did report previous experience learned it through therapeutics lectures or the virtual pharmacy in their facility (which hold inhaler placebos for students to practice with), and not through their community/hospital pharmacy training. Different confidence levels were reported by the participants in reviewing correct device technique and educating asthma patients on it for the different inhaler devices included in the study, with the majority reporting ‘not confident’ (Table 1).
At baseline, there was no significant difference in correct device technique between students assigned to Intervention A compared to those in Intervention B for the DIS, TH, and pMDI. None of the students performed correct TH technique at baseline, and few performed correct DIS and pMDI technique (Table 2).
Table 2.
Performance of Students During Inhaler Technique Demonstration
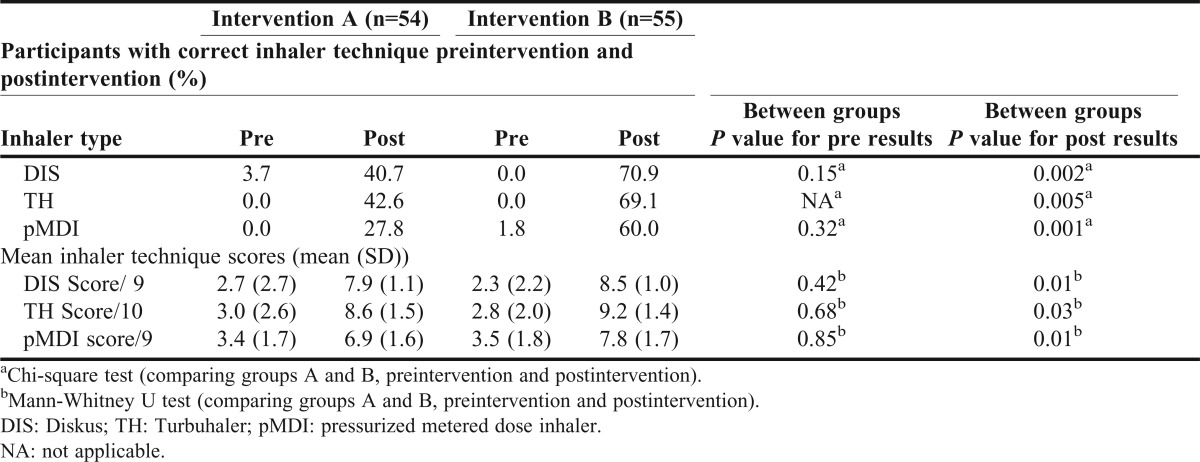
Significant differences were found based on the change in proportion of students with correct device technique for Intervention A vs Intervention B across the study (DIS: 37% vs 70.9%, p=0.003; TH: 42.6% vs 69.1%, p=0.005; pMDI 27.8% vs 58.2%, p=0.001).
No significant differences in mean scores were found between the 2 interventions at baseline for correct technique (Table 2). Change in mean score before and after the intervention showed no significant differences between Intervention A and B with regard to DIS (5.22±2.7 vs 6.18±2.6, p=0.15), TH (5.63±2.7 vs 6.40±2.47, p=0.13) and pMDI (3.52±2.14 vs 4.29±2.20, p=0.07).
Table 3 illustrates the steps students showed difficulty in performing correctly posteducation in both interventions for DIS, TH and pMDI. Significant differences between the groups were found for steps 3, 4 and 8 for the DIS (exhale to residual volume and exhale away from mouthpiece, before and after inhalation), steps 4 and 5 for the TH ( exhale to residual volume and exhale away from mouthpiece), and step 4 (keep head upright or slightly tilted) for the pMDI.
Table 3.
Proportion of Students from Interventions A (n=54) and B (n=55) who Correctly Performed the Individual Steps with Diskus (DIS), Turbuhaler (TH), and Pressurized Metered Dose Inhaler (pMDI) Postintervention
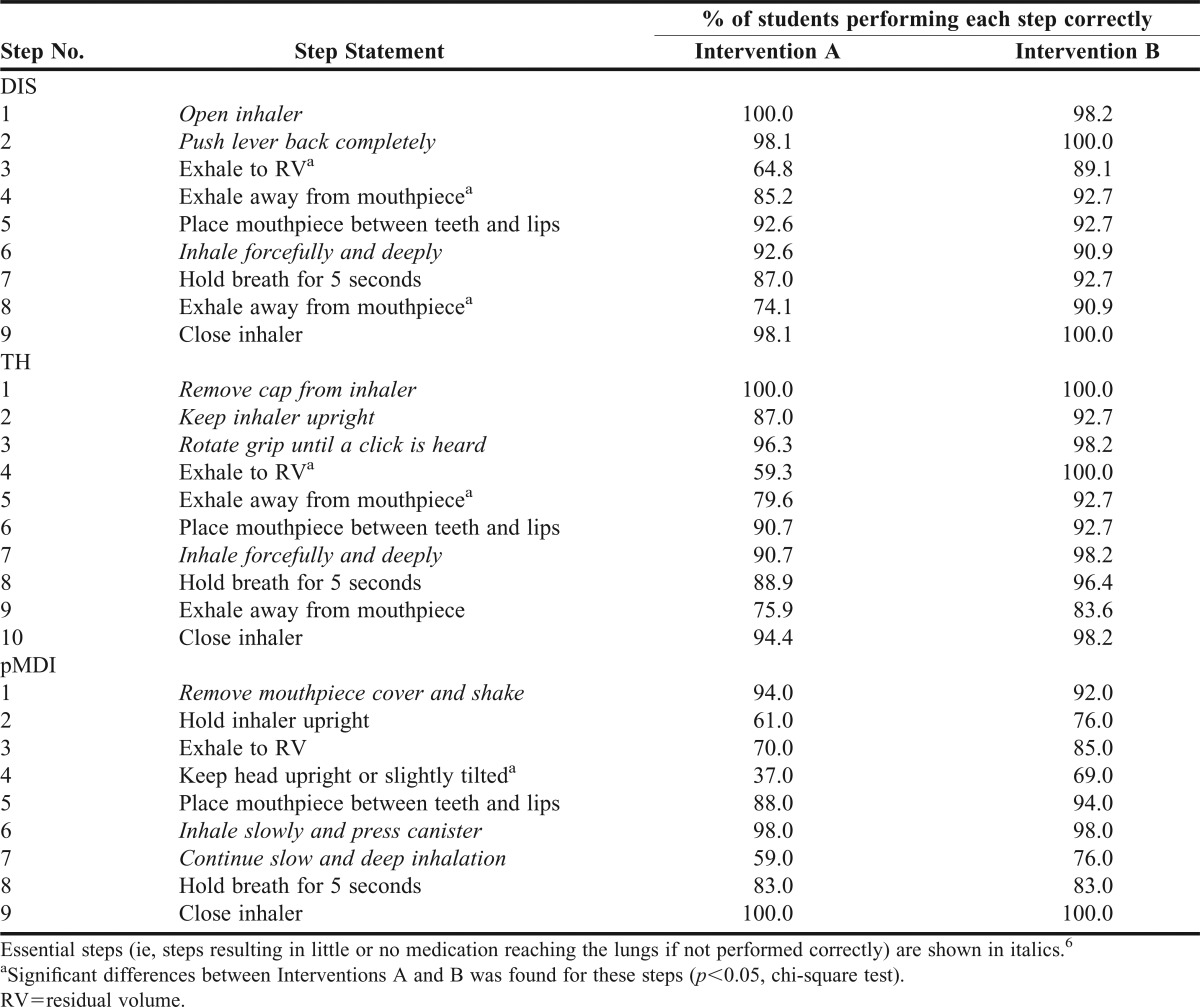
Final assessments for students in Intervention B (n=55) showed that 100% of TH, 88.9% of MDI, and 94.4% of DIS users demonstrated correctly the technique for the device they were assigned to assess/educate the patient on during the simulation process.
Logistic regression modeling the dependent variable of correct device technique posteducation (R2=0.120, p=0.001), indicated that intervention type was the only variable showing significant association with correct device technique following student education (B (standardized regression coefficient)=-0.346, t=-.321, p=0.001).
At the end of the study, no students reported “not confident” in demonstrating the technique for any of the 3 devices. A significantly lower proportion of students in Intervention A reported “very confident” for the DIS (75.9% vs 90.9%, p=0.031), TH (33.3% vs 61.8%, p=0.003), and pMDI (57.4% vs 74.5%, p=0.05) compared to students in Intervention B. The rest of the students reported “confident” in demonstrating the technique for the devices.
Fifteen students attended the focus group meeting, and they reported that the involvement of real patients in in-class device technique education added excitement and reality to the educational process, increased motivation towards learning, increased confidence, and harnessed long term memory. Students reported that lack of interaction with asthma patients and the unavailability of placebo inhalers in the community or hospital pharmacies increased the importance of this educational strategy to prepare them for their future professional responsibilities. Students endorsed the engagement of real patients in all of their hands-on practical therapeutic tutorials in the future.
DISCUSSION
Educating health care professionals on correct device technique has been researched extensively in the last 2 decades to find the ideal way to optimize skills in this area.13,22,23 Despite the known positive impact pharmacists have shown in asthma management,4,24 they are far from being routinely competent in educating patients on correct device technique.9,25 This study evaluated the effect of an in-class simulation scenario on the assessment/education of asthma patients using inhaler devices. This educational method gave rise to significantly better device technique demonstration skills than did group education (involving physical demonstration and written information) plus peer assessment.
Since pharmaceutical care is not fully developed in Jordan,26 this educational method paves the way for establishing and maturing this practice in the country. Baseline and focus group results highlighted students’ lack of interaction with asthma patients in the community and lack of performing inhaler technique education. Students reported unavailability of placebo inhalers in the community pharmacies at which they completed their pharmacy training, an indicator that this type of patient education is not effectively occurring. Placebo inhaler devices allow students to deliver thorough inhaler technique education when the technique is performed incorrectly by the patient without using a device with real medication in it.9 Other advantages of this educational approach were that it provided the opportunity for students to practice patient care away from the busy pharmacy environment and allowed them to observe frequent mistakes in patient technique, such as hand position in TH loading and head tilting during inhalation with the pMDI. Student learning in a supervised educational setting in which the student is debriefed on the mistakes and ways to correct them proved beneficial to students.
The DIS, TH and pMDI inhalers are commonly prescribed as preventative therapy both in Jordan and around the world,1,9 so incorporating them into this study allowed for important comparisons not present in previous studies.15 Providing a rationale behind each step in the device technique checklists was an important issue brought up by the students. Understanding why each step was required helped students in appreciating and memorizing the different techniques for the devices. In each device technique checklist, some steps were more problematic for the students than others even following intervention; educators might consider concentrating their efforts on these steps during undergraduate device technique education.
One of the most important parts of this educational experience was the debriefing, a process that is often difficult to perform in the typical busy pharmacy practice settings. Savoldelli et al reported that simulation without debriefing showed no improvement in skills compared to simulation followed by oral feedback.27
Previous interventional educational modules led to 100% of experienced pharmacists demonstrating correct device technique, which was sustained over time.13 When it came to pharmacy students, using different educational modules was associated with moderate achievements (40% of the students demonstrating incorrect device technique).15 This study showed similar results, namely that the percent of students in the simulation group who did not demonstrate correct technique following education was just as high for some of the devices (DIS =40%, TH =29%, and pMDI =31%). It should be noted however that nearly all students (94.5%) in this group demonstrated correct technique for the device they were assigned to assess/educate the patient on during the simulation intervention. Hence, providing the students with the opportunity to educate all 3 patients on each of the inhaler devices could have led to optimal results. In addition, lack of student motivation for learning inhaler device technique was suggested as an important factor for this drawback.15 Results from the focus group assessments indicated that integrating real patients in the process increased students’ motivation towards learning, which could have affected the results positively.
Written information is not effective in correcting patient, student, or pharmacist inhaler device technique.28 Prior to baseline assessment, students were given written information and a placebo inhaler device for the 3 devices, mimicking the real-life scenario in which pharmacists study independently information about device technique through the product information leaflets before patient counseling. Physical demonstration is needed in this area of education as well.28 Physical demonstration was incorporated into group training and peer education in this process. Peer education, moreover, promotes the interchange of ideas, provides opportunities for students to reflect critically on their practice, increases their motivation by allowing them to take responsibility for their own learning, and helps them gain a clearer understanding about the process.29,30 Based on the approach introduced by Pike, a process of ‘‘overview, teach, and review’’ was built into the simulated scenario to help students retain the information longer.31
One limitation of this study was that engaging real patients in educating pharmacy students cost time and resources, limiting the scope of this educational methodology. Remunerating patients for their time and traveling costs was expensive and recruiting the patients was not simple either. Patients felt embarrassed to admit they had asthma in front of a large group of students. Having to repeat the same scenario many different times resulted in patient discomfort. From the students’ perspectives, assessing and educating the same asthma patient as their peers could have reduced the realism of the process. To resolve these limitations, we recommend a large enough number of recruited patients so that the process is not repeated more than once for any one patient. For better generalization of results, we recommend a larger number of students from different pharmacy schools. Although the change in students’ confidence was apparent from survey responses, the use of 3 choices (very confident, confident, and not confident) with 2 positive and 1 negative choice may have forced the students to provide answers that were not entirely in line with their true level of confidence, which could be more accurately assessed with, for example, surveys based on 5-7 choices (eg, confident, somewhat confident, neutral response, somewhat unconfident, unconfident). The improvements in Intervention B students’ device technique demonstration skills could be a result of observing the device technique demonstration more times (1 to 3 times) than the Intervention A students were able to. However, Thomas et al showed that mere observation of device technique demonstration is not enough to produce better skills.15 Although it would have been more efficacious for each student to practice the simulation with each patient using each inhaler device, this was not feasible. The results from the focus group shed light on the value of this educational process through the eyes of the students. Certain positive outcomes reported by the students, such as the simulation intervention “harnessing their long term memory” is an important outcome that needs to be evaluated in future studies by retesting of student’s skills. Follow-up inhaler technique assessment was done 1 week following the intervention, and longer assessment time may be needed for future studies to assess long-term retention of skills.
CONCLUSION
The use of simulation in pharmacy student training significantly improved correct device technique. Using simulation and real patients in Clinical Pharmacy and Therapeutic practical classes opened new perspectives and could be a potentially effective way to bridge specific gaps between the classroom and the community. However, more work still needs to be done to ensure that all students are able to demonstrate proper technique prior to graduation. Future studies could continue to focus on the exploration and evaluation of simulation in different therapeutic areas, given the current significance and wide use of the medical devices among a broad range of chronically ill patients.
ACKNOWLEDGMENT
This study was funded by the Deanship of Academic Research at the Applied Science University in Amman, Jordan. The authors wish to thank the patients and students who participated.
Appendix 1. Inhaler Technique Checklists
REFERENCES
- 1. Global Initiative for Asthma (GINA) - Global Strategy for Asthma Management and Prevention - Revised Workshop Report 2012. Available online at: http://www.ginasthma.org. Accessed May 2014.
- 2.National Heart Lung and Blood institute. Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma (2007). Available online at: http://www.nhlbi.nih.gov/guidelines/asthma/02_sec1_intro.pdf. Accessed May 2014.
- 3.Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ Couns. 2008;72(1):26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol. 2007;119(6):1537–1538. doi: 10.1016/j.jaci.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 5.Roche N, Huchon GJ. Rationale for the choice of an aerosol delivery system. J Aerosol Med. 2000;13(4):393–404. doi: 10.1089/jam.2000.13.393. [DOI] [PubMed] [Google Scholar]
- 6.Basheti IA, Bosnic-Anticevich SZ, Armour CL, Reddel HK. Checklists for Powder Inhaler Technique: A Review and Recommendations. Respir Care. 2014;59(7):1140–1154. doi: 10.4187/respcare.02342. [DOI] [PubMed] [Google Scholar]
- 7.Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47(3):251–256. doi: 10.3109/02770900903580843. [DOI] [PubMed] [Google Scholar]
- 8.Khassawneh BY, Al-Ali MK, Alzoubi KH, Batarseh MZ, Al-Safi SA, Sharara AM, et al. Handling of inhaler devices in actual pulmonary practice: metered-dose inhaler versus dry powder inhalers. Respir Care. 2008;53(3):324–328. [PubMed] [Google Scholar]
- 9.Basheti IA, Qunaibi E, Bosnic-Anticevich SZ, Armour CL, Khater S, Omar M, et al. User error with Diskus and Turbuhaler by asthma patients and pharmacists in Jordan and Australia. Respir Care. 2011;56(12):1916–1923. doi: 10.4187/respcare.01205. [DOI] [PubMed] [Google Scholar]
- 10.Fink JB. Inhalers in asthma management: is demonstration the key to compliance? Respir Care. 2005;50(5):598–600. [PubMed] [Google Scholar]
- 11.Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J. 2002;19(2):246–251. doi: 10.1183/09031936.02.00218402. [DOI] [PubMed] [Google Scholar]
- 12.Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respir Care. 2005;50(10):1360–1374. [PubMed] [Google Scholar]
- 13.Basheti IA, Armour CL, Reddel HK, Bosnic-Anticevich SZ. Long-term maintenance of pharmacists’ inhaler technique demonstration skills. Am J Pharm Educ. 2009;73(2):32. doi: 10.5688/aj730232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawksworth GM, James L, Chrystyn H. Characterization of the inspiratory manoeuvre when asthmatics inhale through a Turbohaler pre- and post-counselling in a community pharmacy. Respir Med. 2000;94(5):501–504. doi: 10.1053/rmed.1999.0768. [DOI] [PubMed] [Google Scholar]
- 15.Toumas M, Basheti IA, Bosnic-Anticevich SZ.Comparison of small-group training with self-directed internet-based training in inhaler techniques Am J Pharm Educ 200973(5Article 85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thurmon TB, Schwartz LL, Jervis KP. Asthma education in the student laboratory. J Pharm Pract. 2013;26(1):29–31. doi: 10.1177/0897190012466045. [DOI] [PubMed] [Google Scholar]
- 17.Erickson SR, Chang A, Johnson CE, Gruppen LD. Lecture versus Web tutorial for pharmacy students’ learning of MDI technique. Ann Pharmacother. 2003;37(4):500–505. doi: 10.1345/aph.1C374. [DOI] [PubMed] [Google Scholar]
- 18.Clever SL, Dudas RA, Solomon BS, Yeh HC, Levine D, Bertram A, et al. Medical student and faculty perceptions of volunteer outpatients versus simulated patients in communication skills training. Acad Med. 2011;86(11):1437–1442. doi: 10.1097/ACM.0b013e3182305bc0. [DOI] [PubMed] [Google Scholar]
- 19.Okuda Y, Bryson EO, DeMaria S, Jr., Jacobson L, Quinones J, Shen B, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76(4):330–343. doi: 10.1002/msj.20127. [DOI] [PubMed] [Google Scholar]
- 20.Accreditation council for pharmacy education accreditation guidlines. Available online at: https://www.acpe-accredit.org/standards/. Accessed May 2014.
- 21.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543. [PubMed] [Google Scholar]
- 22.O’Connell MB, Hewitt JM, Lackner TE, Pastor JD, 3rd, Wong MT, Bishop AL. Short- and long-term retention of a nursing home education program on metered-dose inhaler technique. Ann Pharmacother. 1992;26(7-8):980–984. doi: 10.1177/106002809202600723. [DOI] [PubMed] [Google Scholar]
- 23.Cain WT, Cable G, Oppenheimer JJ. The ability of the community pharmacist to learn the proper actuation techniques of inhaler devices. J Allergy Clin Immunol. 2001;108(6):918–920. doi: 10.1067/mai.2001.119153. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Cardenas V, Sabater-Hernandez D, Kenny P, Martinez-Martinez F, Faus MJ, Benrimoj SI. Effect of a pharmacist intervention on asthma control. A cluster randomised trial. Respir Med. 2013;107(9):1346–1355. doi: 10.1016/j.rmed.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 25.Gemicioglu B, Borekci S, Can G. Investigation of knowledge of asthma and inhaler devices in pharmacy workers. J Asthma. 2014:1–7. doi: 10.3109/02770903.2014.928310. [DOI] [PubMed] [Google Scholar]
- 26.Yousef AM, Al-Bakri AG, Bustanji Y, Wazaify M. Self-medication patterns in Amman, Jordan. Pharm World Sci. 2008;30(1):24–30. doi: 10.1007/s11096-007-9135-x. [DOI] [PubMed] [Google Scholar]
- 27.Savoldelli GL, Naik VN, Park J, Joo HS, Chow R, Hamstra SJ. Value of debriefing during simulated crisis management: oral versus video-assisted oral feedback. Anesthesiology. 2006;105(2):279–285. doi: 10.1097/00000542-200608000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respir Care. 2005;50(5):617–623. [PubMed] [Google Scholar]
- 29.Topping KJ, Smith EF, Swanson I, Elliot A. Formative peer assessment of academic writing between postgraduate students. Asses Eval Higher Educ. 2000;25(2):149–166. [Google Scholar]
- 30.Basheti IA, Ryan G, Woulfe J, Bartimote-Aufflick K. Anonymous peer assessment of medication management reviews. Am J Pharm Educ. 2009;74(5):77. doi: 10.5688/aj740577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pike RW. Creative training techniques handbook. Tips, tactics, and how to’s for delivering effective training. 2nd ed. Minneapolis, MN: Lakewood Publications; 1994:1-41.