Abstract
Objective: To identify differences among faculty members in various health professional training programs in perceived benefits and challenges of implementing interprofessional education (IPE).
Methods: A 19-item survey using a 5-point Likert scale was administered to faculty members across different health disciplines at a west coast, multicollege university with osteopathic medicine, pharmacy, and physician assistant programs.
Results: Sixty-two of 103 surveys (60.2%) were included in the study. Faculty members generally agreed that there were benefits of IPE on patient outcomes and that implementing IPE was feasible. However, group differences existed in belief that IPE improves care efficiency (p=0.001) and promotes team-based learning (p=0.001). Program divergence was also seen in frequency of stressing importance of IPE (p=0.009), preference for more IPE opportunities (p=0.041), and support (p=0.002) within respective college for IPE.
Conclusions: Despite consensus among faculty members from 3 disciplines that IPE is invaluable to their curricula and training of health care students, important program level differences existed that would likely need to be addressed in advance IPE initiatives.
Keywords: Interprofessional education (IPE), interdisciplinary education, interprofessional relations, pharmacy education, faculty member attitudes and opinions
INTRODUCTION
In 2003, the Institute of Medicine published a report titled Health Professions Education: A Bridge to Quality,1 which stressed the importance of integrating interprofessional experiences into health education and developing core competencies for interprofessional education (IPE). The recommendations involving IPE were based on observations that interdisciplinary collaboration may have a positive impact on patient care outcomes.1-2 Since then, IPE strategies have been explored by many professional health programs in the United States. Prevalent examples of IPE include: working on interdisciplinary team-based patient cases or activities, rounding experiences, objective structured clinical exams (OSCEs), competitions, and outreach events.3-7,8-11 While these IPE experiences are non-standardized and site-dependent, the majority of them have shown positive effects on student attitudes toward interdisciplinary teamwork.3-6,8-12
Similar to other health fields of study, US pharmacy programs have been charged with incorporating IPE into their curriculum. The Accreditation Council for Pharmacy Education (ACPE) recently set forth revised Standards to include IPE initiatives as part of the criteria for accreditation.13 Some of the potential barriers to IPE include lack of other professional health programs on campus or nearby, lack of perceived benefits of IPE, a need for increased training in delivering IPE, lack of institutional support of IPE, lack of cross-discipline curriculum structure and shared learning spaces, and scheduling conflicts among the different health professional programs.2,14-17 While institutions have generally expressed interest in providing IPE experiences for students, many programs have struggled with the initial implementation process.14-18 One struggle may be associated with the attitudes and perceptions of faculty members from other health disciplines, which can offer significant challenges for development and implementation. By definition, any IPE initiative requires involvement and participation of multiple disciplines, so faculty members from these programs must be “on board.” A search of literature revealed limited data on faculty member thoughts and sentiments towards IPE implementation,19-21 even though student opinions are well documented,6,8,11,12 often with medical students expressing lower levels of enthusiasm for IPE relative to students in other professions.
This study evaluated faculty member perceptions of IPE and the perceived IPE implementation barriers across different health professional programs at Touro University in California (TUCA). The university has multiple health programs on campus, including a College of Osteopathic Medicine (COM), College of Pharmacy (COP), and a master’s program in Physician Assistant Studies (PA). The goals of this study were to identify challenges perceived by faculty members in implementing IPE and to explore possible differences in perception among the faculty members at the different colleges.
METHODS
A survey was created in SurveyMonkey (SurveyMonkey Inc., Palo Alto, CA) to evaluate perceived barriers among faculty members across multiple health professional disciplines at TUCA regarding IPE implementation. The survey questions were developed from previously identified barriers reported in the literature including lack of established benefits of IPE, decreased enthusiasm towards IPE from medical faculty members and students, need for increased training in delivering IPE, lack of institutional support of IPE, and disagreement over the venues most conducive to IPE. A total of 19 questions on IPE barriers, along with 8 commonly requested demographic questions, were included in the final survey instrument. IPE opinion questions were 5-point Likert-based questions with a final question asking respondents to identify up to 5 of their top choices of IPE venues. The survey was pilot-tested on university employees considered nonfaculty members (ie, employees with administrative support duties). The study received approval from the Institutional Review Board at TUCA.
Survey instruments were e-mailed to faculty members at COM, COP, and PA program at TUCA. Faculty member e-mails were obtained through campus human resources and were considered accurate and complete at the time of survey administration. The survey was initially launched in April 2012 and 3 reminder e-mails followed at 2-week intervals if the faculty member had not already completed the survey. Differences in demographics between the 3 faculty member groups were assessed via chi-square or Fisher exact tests (the latter if expected cell frequency was less than 5). Responses to Likert scale questions were analyzed using the Kruskal-Wallis test to examine differences in responses by college as well as by demographic variables. Multivariate linear regression models were then created for the Likert opinion questions to examine differences between programs while controlling for faculty member level variables. A set of indicator variables were derived from the categorical demographic data collected for all the variables used in the multivariate models with the exception of age, which was treated as a continuous variable. Differences in preferred IPE learning methods (favorite IPE venues) were analyzed via chi-square and Fisher exact tests. An alpha level of 0.05 was considered significant. All results were analyzed using SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
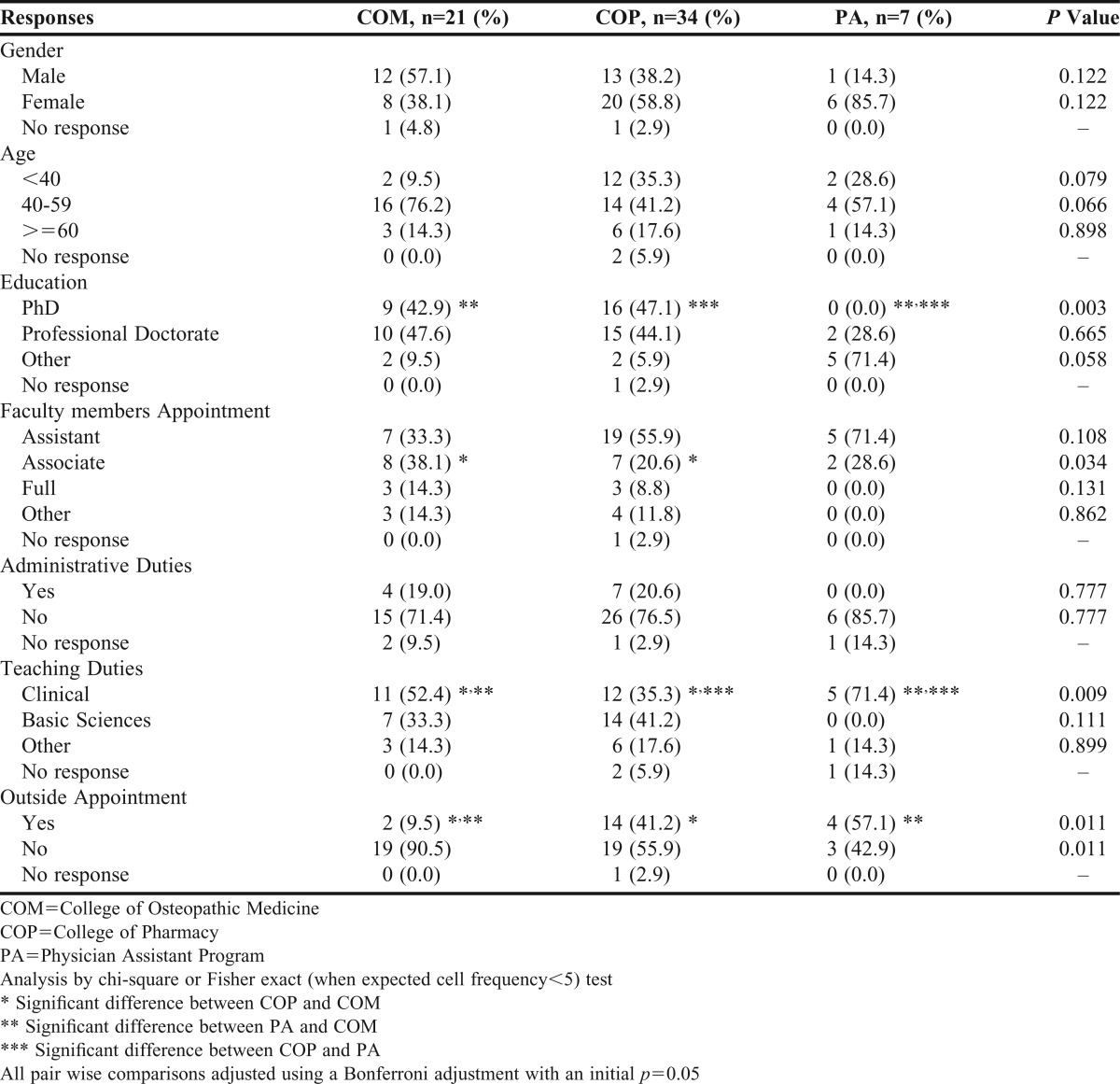
Sixty-two out of 103 faculty members surveys were included in the final analysis for an overall response rate of 60.2%. More specifically, the analyzed dataset was comprised of 21 surveys from COM (n=50, 42.0%), 34 from COP (n=45, 75.6%), and 7 from PA (n=8, 87.5%). Two returned surveys were considered incomplete, 1 because the respondent did not indicate his or her program (ie, COM, COP, or PA), and 1 because not all IPE opinion questions were answered. Only completed surveys were included in the final analysis. Demographic information is shown in Table 1. Programs were generally similar with respect to faculty member demographics, including gender, age, and percentage with an administrative duty obligation. Significant differences were noted, however, in percentage of faculty members with a PhD, academic rank, clinical teaching duties, and presence of an outside appointment.
Table 1.
Demographics of Osteopathic Medicine, Pharmacy, and Physician Assistant Faculty Responders
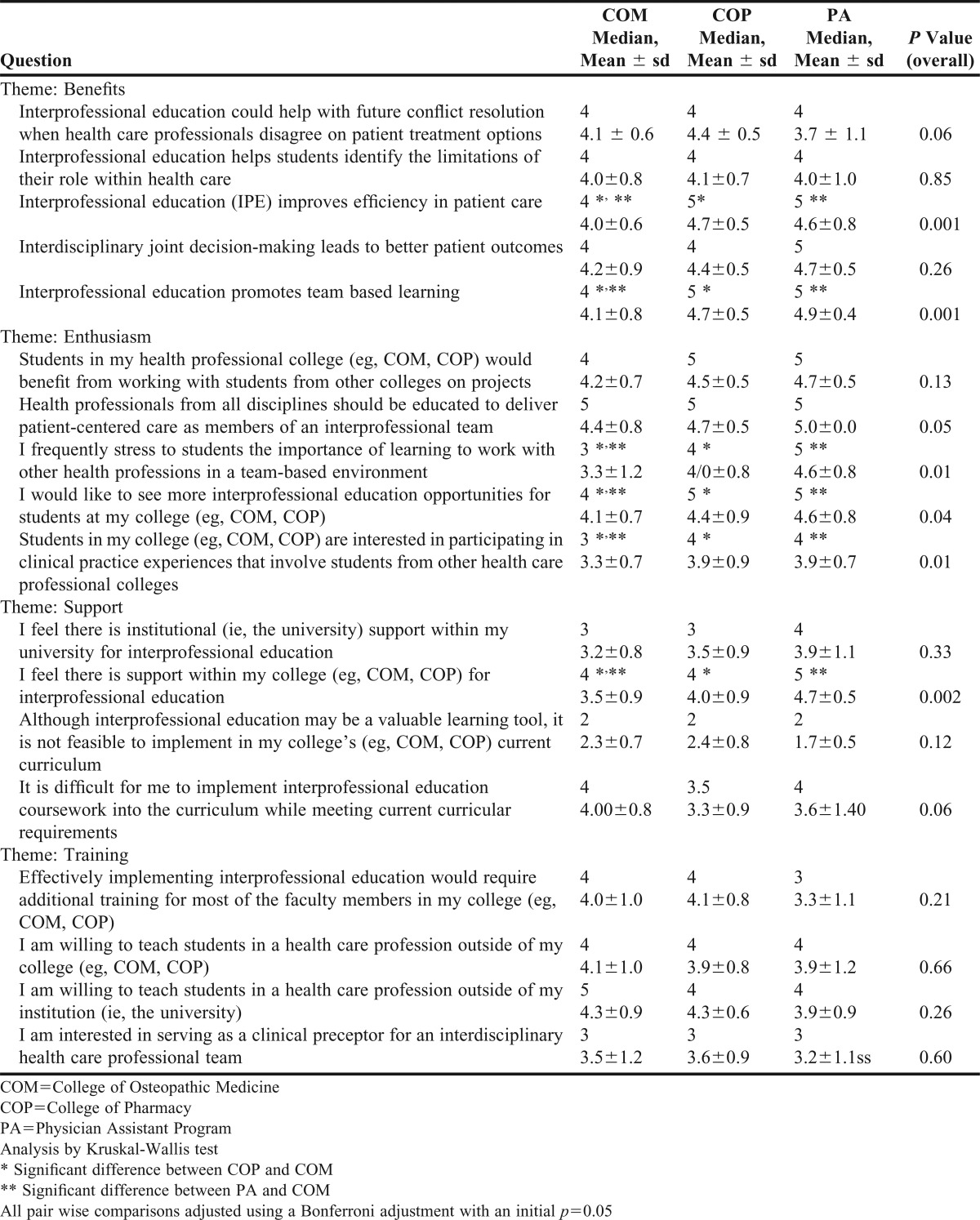
The results from the Likert scale questions are shown in Table 2. The 3 faculty member groups responded similarly (and in general, positively) regarding potential benefits of IPE. Differences were, however, observed between faculty member groups in believing IPE improves efficiency of patient care and agreeing that IPE promotes team-based learning, with higher results reported from both COP and PA respondents than from COM respondents. Significant differences in questions targeting enthusiasm for IPE were observed in how frequently faculty members stress the importance of IPE to their students and in whether faculty members wanted more IPE opportunities for students in their college, with lower levels in COM than in COP and PA. Faculty members from COP and PA were more likely than COM faculty members to believe their students were interested in participating in IPE clinical practice experiences. No differences were reported faculty members about the level of support for IPE at the university (institutional) level; however, COP and PA respondents reported significantly greater college level support relative to COM respondents. All faculty members seemed to disagree with the statement that it was not feasible to implement IPE in their current curriculum, but did indicate that it was challenging given their curriculum requirements. In addition, all faculty member groups expressed the need for additional training to effectively implement IPE. Lastly, while faculty members appeared willing to teach students outside of their respective college and institution, they were less enthusiastic about serving as an IPE clinical preceptor.
Table 2.
Survey Responses to Likert Scale Questions
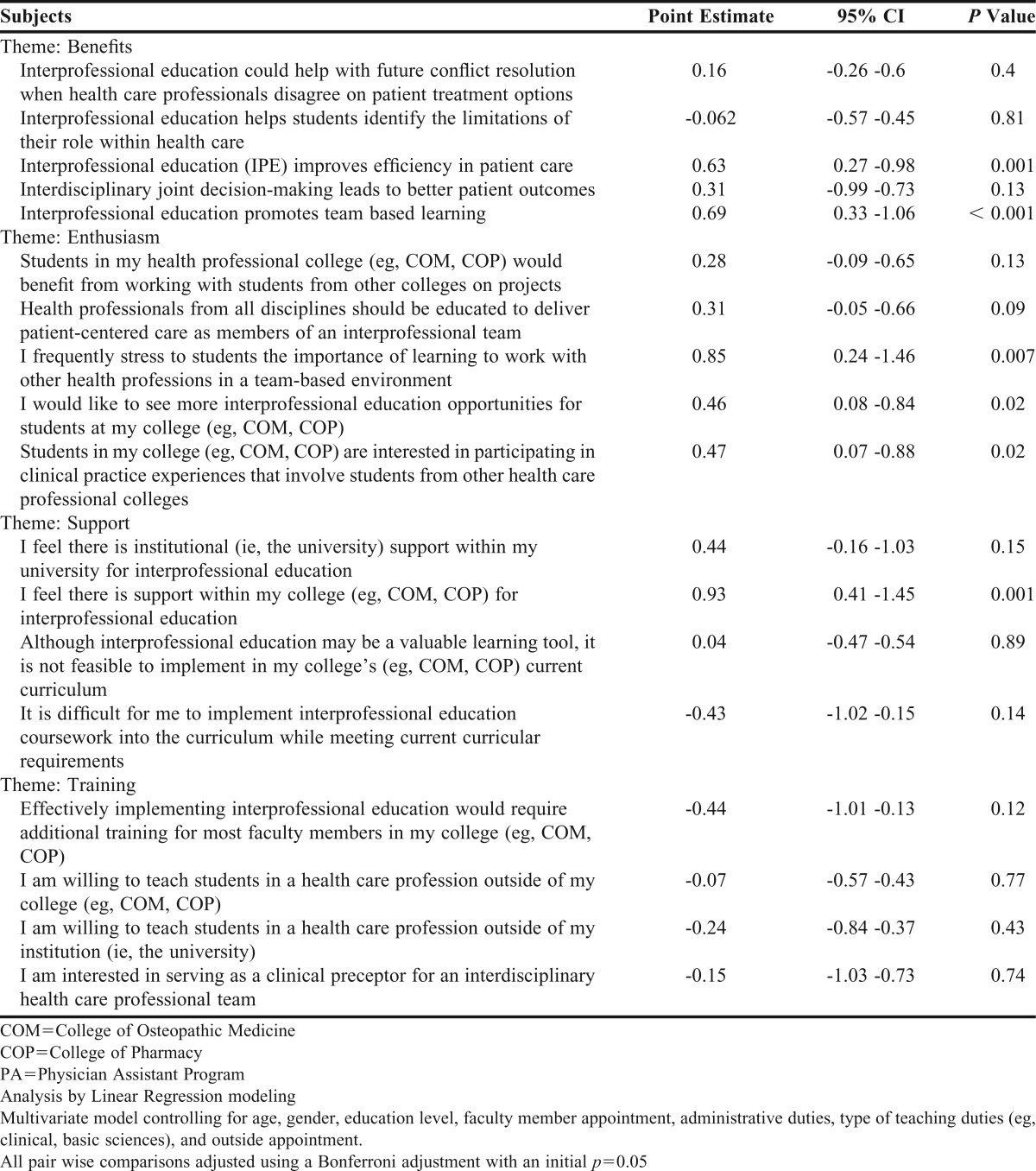
To better examine the effect of program on opinions regarding IPE, a series of multivariate models were created. Covariants used in the adjusted models included: age, gender, outside appointment, faculty member rank, and an indicator variable for clinical teaching. Because of the relative few number of faculty members and responses from the PA program, and because PA and COP results were found to be similar overall, PA and COP faculty members were grouped together for the purpose of the multivariate analyses. The coefficient for COP/PA (along with 95% confidence intervals) relative to COM is shown in Table 3. While controlling for the previously mentioned variables, faculty members from COP and PA reported more perceived benefits in patient care and team-based learning when compared to their colleagues from COM on the 5-point Likert Scale. In addition, more faculty members from COP and PA stressed the importance of learning in a team-based environment relative to COM faculty members. COP and PA faculty members also responded more favorably to the idea of increasing IPE opportunities and reported being more inclined to believe their students wanted to participate in IPE clinical practice experiences relative to COM respondents. Lastly, COP and PA faculty members expressed significantly more support for IPE within their college when compared to faculty members from COM. No other significant differences were found in the multivariate comparisons, including observed differences in opinions regarding IPE training. A subsequent subanalysis removing PA faculty members responses and comparing only COP to COM responses in a similar series of multivariate models found results were identical in terms of significant variables and the direction (sign) of their point estimate (results not shown).
Table 3.
Point Estimate for COP/PA Relative to COM
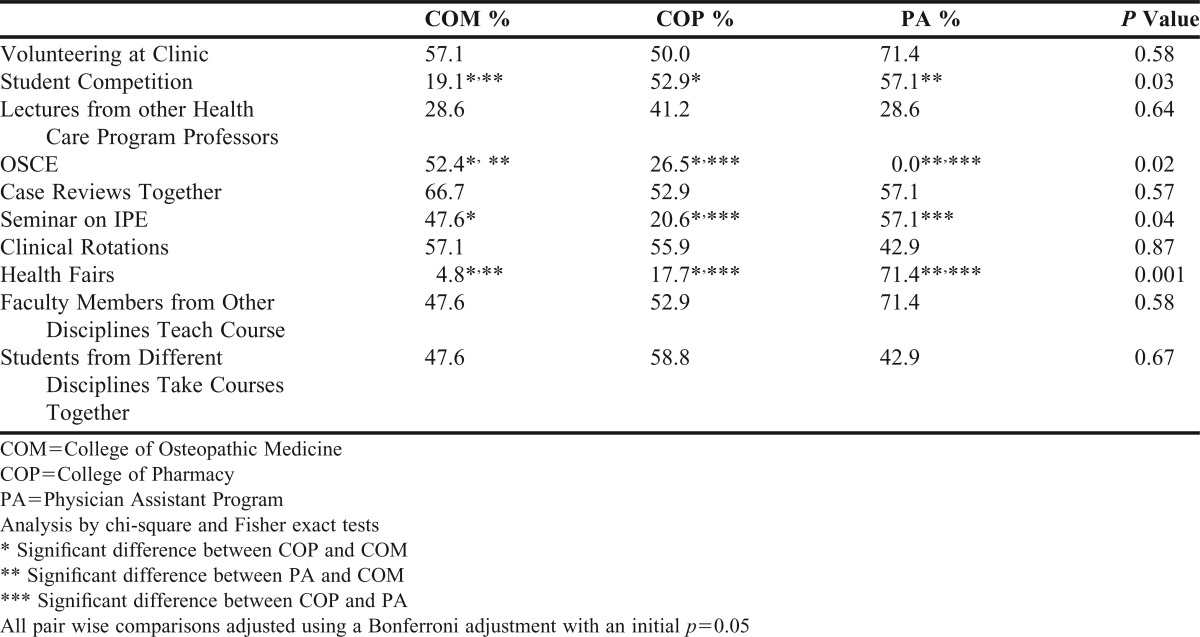
The final question asking respondents to identify their top 5 choices for IPE learning venues resulted in ranges by program from 0.0% to 71.4%, with several significant differences (Table 4). Specifically, COM faculty members preferred objective structured clinical exams (OSCEs) relative to COP and PA faculty members, with the difference between COP and PA respondents also significant. Additionally, COM and PA respondents preferred seminars on IPEs compared to COP respondents, while both COP and PA faculty members indicated a preference for student competitions relative to COM faculty members. Lastly, PA faculty members preferred health fairs to a significantly greater extent than COM and COP faculty members, and the difference between COM and COP respondents was also significant regarding health fairs. No other differences among the top 5 preferred methods of IPE delivery were found.
Table 4.
Percentage of Faculty Members Listing a Specified IPE Student Activity (Venue) in Their Top 5 Preferred Methods for Student IPE Learning
DISCUSSION
IPE requires cooperation and participation from faculty members and students from all participating disciplines. While previous studies found lower levels of enthusiasm for IPE training among students in medicine relative to students in other health care programs, including pharmacy, limited data is available to describe actual faculty member opinions and sentiments for IPE among the various health care professions.6,8,19-21 This study was conducted to explicitly examine potential differences in faculty member attitudes toward and interest in IPE along with perceived barriers among faculty members from osteopathic medicine, pharmacy , and physician assistant programs.
The demographic makeup of the 3 faculty member cohorts studied was generally similar. While the benefits of IPE previously identified in the literature were echoed in this study, results consistently showed COP and PA faculty members were more enthusiastic than their COM colleagues about IPE in their classroom and perceived greater benefits from IPE. This may reflect the principle of least interest as described by Van Winkle et al, in which the health professional power hierarchy can influence the eagerness to collaborate.22 In multivariate-adjusted models, combined COP and PA faculty members reported higher opinion scores (on a 5-point Likert scale) relative to COM faculty members in perceived support within their college for IPE, stressing the importance of IPE to students, the notion that IPE promotes team-based learning and improves patient care efficiency, and the interest to see more IPE opportunities. These results suggested important program level differences in IPE opinions that remained even after controlling for potential differences among faculty members. Whether the lack of support at the program level directly translated to the differences in enthusiasm mentioned previously was not clear. Also of interest was the lack of difference in opinion regarding support at the institutional level, suggesting at least some evidence of internal validity for the survey. Finally, obvious differences in preferred delivery methods for IPE training were of note.
The current study is in line with previous surveys of students that reported more positive attitudes about interprofessional collaboration in many health professional programs compared to students in medical programs.6,8,22-24 Previous studies indicated that medical students often express skepticism regarding the utility of IPE.25-26 Effective engagement of students in IPE requires all stakeholders, especially those in medicine, to be involved.27 A likely valuable finding from this study was that differences in opinions about IPE also exist between faculty members at the program level. Furthermore, because attitude toward IPE is the single best predictor of a faculty member’s intent to engage in IPE,28 our findings underscore the importance of showing college of medicine faculty members that IPE can improve both the practice and quality of health care. While it is unknown if reprioritizing IPE training methods (eg, less emphasis on volunteering at clinics and health fairs and more emphasis on OSCEs) of pharmacy faculty members would increase “buy-in” among medical faculty members, the differences in preferred delivery methods for IPE are areas highlighting potential differences that need to be addressed by policy and stakeholders interested in advancing IPE initiatives.
Survey responses regarding faculty member support for IPE (with the exception of perceived program level support) were relatively similar, including a lack of willingness to serve as a clinical IPE preceptor and difficulty in implementing IPE given curricular constraints. Responses also indicated that faculty members from all 3 disciplines perceived the need for additional training in order to implement IPE. Institutionalizing more faculty member development programs around IPE may help address faculty member confidence and facilitate their willingness to participate in teaching and serving as a preceptor for clinical IPEs. Meanwhile, educational institutions with multiple health professional programs could consider holding events to increase faculty member awareness of the value of IPE and implementing initiatives that improve faculty member support and encourage their involvement in IPE.10,29-31 Successful IPE programs showcase best practices that include reliable administrative support and robust interprofessional programmatic infrastructure.9,30,32 Thus, more support from college administrators and time dedicated to IPE curriculum are likely necessary to develop new or sustain existing efforts.
Several limitations should be considered when evaluating the results of this study. First, although the overall response rate was relatively high (over 60%) for a university faculty member survey, a higher participation rate was desirable. It is also unknown whether the notable differences in response rates across the 3 programs introduced any potential bias in the results. Secondly, the study population consisted of 3 programs from a single university. Results may not be directly applicable to other institutions or to other geographical regions of the country. In addition, faculty member opinions from other important health programs (eg, dental, nursing, and nutrition which TUCA does not have) were not included. Confounders at the faculty member level not measured or adequately controlled for in the multivariate model may also exist. Lastly, the study was mostly descriptive in nature and, as such, its findings were not designed to fully elucidate reasons for observed differences or to compare different strategies to attenuate these differences.
CONCLUSION
Interprofessional education is a concept centered on multi-disciplinary teamwork and is an essential component of contemporary health professional education. The general consensus of health care faculty members surveyed, regardless of discipline (ie, medicine, pharmacy, or physician assistant), is that IPE holds an important place in health professional training. Faculty member opinions diverged on the perceived barriers and benefits of IPE—with medicine faculty members less optimistic than pharmacy and physician assistant faculty members. This study provided direction on faculty members member-related areas to focus on to advance the progress of IPE in health professional training. Future research could expand this study to more multi-college health professional institutions with additional number and types of training programs and include assessment of specific attempts to overcome any perceived program level barriers to IPE.
ACKNOWLEDGMENTS
The authors would like to thank the sponsors of the 2011-2012 California Pharmacy Student Leadership (CAPSLEAD) program: Rite Aid Corporation, Pfizer, Inc, California Society of Health-System Pharmacists, and California Pharmacists Association; Benjamin Malcolm, Sukhpal Cheema, Martin Tran, and Jaspreet Kaur for their contributions to the Touro University – CA CAPSLEAD team; and especially Drs. Katherine Knapp and Layla Yousify for their support and assistance with developing our research topic.
REFERENCES
- 1.National Research Council. Health Professions Education: A Bridge to Quality. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev. 2013;3. [DOI] [PMC free article] [PubMed]
- 3.MacDonnell CP, Rege SV, Misto K, Dollase R, George P. An introductory interprofessional exercise for healthcare students. Am J Pharm Educ. 2012;76(8):Article 154. doi: 10.5688/ajpe768154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Remington TL, Foulk MA, Williams BC. Evaluation of evidence for interprofessional Education. Am J Pharm Educ. 2006;70(3):Article 66. doi: 10.5688/aj700366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saini B, Shah S, Kearey P, Bosnic-Anticevich S, Grootjans J, Armour C. An interprofessional learning module on asthma health promotion. Am J Pharm Educ. 2011;75(2):Article 30. doi: 10.5688/ajpe75230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Winkle LJ, Bjork BC, Chandar N, et al. Interprofessional workshop to improve mutual understanding between pharmacy and medical students. Am J Pharm Educ. 2012;76(8):Article 150. doi: 10.5688/ajpe768150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westberg SM, Adams J, Thiede K, Stratton TP, Bumgardner MA. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2):Article 34. doi: 10.5688/aj700234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shrader S, McRae L, King WM, 4th, Kern D. A simulated interprofessional rounding experience in a clinical assessment course. Am J Pharm Educ. 2011;75(4):Article 61. doi: 10.5688/ajpe75461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odegard PS, Robins L, Murphy N, et al. Interprofessional initiatives at the University of Washington. Am J Pharm Educ. 2009;73(4):Article 63. doi: 10.5688/aj730463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mészáros K, Lopes IC, Goldsmith PC, Knapp KK. Interprofessional education: cooperation among osteopathic medicine, pharmacy, and physician assistant students to recognize medical errors. J Am Osteopath Assoc. 2011;111(4):213–218. [PubMed] [Google Scholar]
- 11.VanderWielen LM, Vanderbilt AA, Dumke EK, et al. Improving public health through student-led interprofessional extracurricular education and collaboration: a conceptual framework. J Multidiscip Healthc. 2014;7:105–110. doi: 10.2147/JMDH.S52019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brock D, Abu-Rish E, Chiu CR, et al. Interprofessional education in team communication: working together to improve patient safety. BMJ Qual Saf. 2013;22(5):414–23. doi: 10.1136/bmjqs-2012-000952. [DOI] [PubMed] [Google Scholar]
- 13.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Chicago, Illinois. Version 2.0. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed December 27, 2013.
- 14.Buring SM, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(4):Article 59. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammick M, Freeth D, Koppel I, Reeves S, Barr H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med Teach. 2007;29(8):735–751. doi: 10.1080/01421590701682576. [DOI] [PubMed] [Google Scholar]
- 16.Sheldon M, Cavanaugh JT, Croninger, et al. Preparing rehabilitation healthcare providers in the 21st century: implementation of interprofessional education through an academic-clinical site partnership. Work. 2012;41(3):269–275. doi: 10.3233/WOR-2012-1299. [DOI] [PubMed] [Google Scholar]
- 17.Breitbach AP, Sargeant DM, Gettemeier PR, et al. From buy-in to integration: melding an interprofessional initiative into academic programs in the health professions. J Allied Health. 2013;42(3):e67–73. [PubMed] [Google Scholar]
- 18.Jones KM, Blumenthal DK, Burke JM, et al. Interprofessional education in IPPE at US Colleges and Schools of Pharmacy. Am J Pharm Educ. 2012;76(5):Article 80. doi: 10.5688/ajpe76580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Curran VR, Sharpe D, Forristall J. Attitudes of health sciences faculty members towards interprofessional teamwork and education. Med Educ. 2007;41(9):892–896. doi: 10.1111/j.1365-2923.2007.02823.x. [DOI] [PubMed] [Google Scholar]
- 20.Smith KM, Scott DR, Barner JC, DeHart RM, Scott JK, Martin SJ. Interprofessional education in six US colleges of pharmacy. Am J Pharm Educ. 2009;73(4):Article 61. doi: 10.5688/aj730461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner SF, Chamberlin GD, Heestand DE, Stowe CD. Interdisciplinary didactic instruction at academic health centers in the United States: attitudes and barriers. Adv Health Sci Educ Theory Pract. 2002;7(3):179–190. doi: 10.1023/a:1021144215376. [DOI] [PubMed] [Google Scholar]
- 22.Van Winkle LJ, Cornell S, Fjortoft N, et al. Critical thinking and reflection exercises in a biochemistry course to improve prospective health professions students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2013;77(8):Article 169. doi: 10.5688/ajpe778169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Winkle LJ, Fjortoft N, Hojat M. Validation of an instrument to measure pharmacy and medical students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2011;75(9):Article 178. doi: 10.5688/ajpe759178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lie D, Walsh A, Segal-Gidan F, Banzali Y, Lohenry K. Physician assistant students’ views regarding interprofessional education: a focus group study. J Physician Assist Educ. 2013;24(1):35–41. doi: 10.1097/01367895-201324010-00005. [DOI] [PubMed] [Google Scholar]
- 25.Wilhelmsson M, Ponzer S, Dahlgren LO, Timpka T, Faresjö T. Are female students in general and nursing students more ready for teamwork and interprofessional collaboration in healthcare? BMS Med Educ. 2011;11:Article 15. doi: 10.1186/1472-6920-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ponzer S, Hylin U, Kusoffsky A, et al. Interprofessional training in the context of clinical practice: goals and students’ perceptions on clinical education wards. Med Educ. 2004;38(7):727–736. doi: 10.1111/j.1365-2929.2004.01848.x. [DOI] [PubMed] [Google Scholar]
- 27.Whitehead C. The doctor dilemma in interprofessional education and care: how and why will physicians collaborate? Med Educ. 2007;41(10):1010–1016. doi: 10.1111/j.1365-2923.2007.02893.x. [DOI] [PubMed] [Google Scholar]
- 28.Olenick M, Allen LR. Faculty members intent to engage in interprofessional education. J Multidiscip Healthc. 2013;6:149–161. doi: 10.2147/JMDH.S38499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poirier TI, Wilhelm M. Interprofessional education: fad or imperative. Am J Pharm Educ. 2013;77(4):Article 68. doi: 10.5688/ajpe77468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buring SM, Bhushan A, Brazeau G, Conway S, Hansen L, Westberg S. Keys to successful implementation of interprofessional education: learning, location, faculty members development and curricular themes. Am J Pharm Educ. 2009;73(4):Article 60. doi: 10.5688/aj730460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kemp SP, Cressey CO, Robertson L. Final report of the health sciences interprofessional education and facilities committee. August 2012. http://sph.washington.edu/strategicplan/implementation/IPE_report.pdf. Accessed August 12, 2013.
- 32.Bridges DR, Davidson RA, Odegard PS, Maki IV, Tomkowiak J. Interprofessional collaboration: three best practice models of interprofessional education. Med Educ Online. 2011;16:Article 6035. doi: 10.3402/meo.v16i0.6035. [DOI] [PMC free article] [PubMed] [Google Scholar]


