Abstract
Objective. To describe an interprofessional communication course in an academic health sciences center and to evaluate and compare interpersonal and interprofessional communication self-efficacy beliefs of medical, nursing, and pharmacy students before and after course participation, using Bandura’s self-efficacy theory as a guiding framework.
Design. First-year nursing (n=36), first-year medical (n=73), and second-year pharmacy students (n=83) enrolled in an interprofessional communication skills development course voluntarily completed a 33-item survey instrument based on Interprofessional Education Collaborative (IPEC) core competencies prior to and upon completion of the course during the fall semester of 2012.
Assessment. Nursing students entered the course with higher interpersonal and interprofessional communication self-efficacy beliefs compared to medical and pharmacy students. Pharmacy students, in particular, noted significant improvements in communication self-efficacy beliefs across multiple domains postcourse.
Conclusion. Completion of an interprofessional communications course was associated with a positive impact on health professions students’ interpersonal and interprofessional communication self-efficacy beliefs.
Keywords: Interprofessional communication, interpersonal communication, self-efficacy beliefs
INTRODUCTION
Communication is inherent in the provision of patient-centered care.1-4 Pharmacists, for example, use communication skills to counsel patients, assess the appropriateness of self-care, and recommend appropriate medication(s) to prescribers. While ubiquitous in nature, communication skills and abilities have only in the past couple decades received focused attention in the training of health care professionals.5 Health care communication, or lack thereof, has been posited to influence patient outcomes related to patient safety, clinical decision-making, redundancies in care, and patient and societal costs.6-8 The Accreditation Council for Pharmacy Education Standards indicate graduates of professional programs should be able to employ communication skills in multiple settings and with multiple constituents.9 Additionally, recently revised 2013 Center for the Advancement of Pharmacy Education Outcomes call for students to possess the ability to participate as part of a health care team by exhibiting respect, understanding, and values necessary to meet patient needs and communicate verbally and nonverbally when interacting with individuals, groups, or organizations.10 Furthermore, the Affordable Care Act deems communication vital to the success of accountable care organizations and patient-centered medical homes.11
Health care-related communication can be conceptualized broadly into 2 domains: interprofessional and interpersonal communication. The Interprofessional Education Collaborative (IPEC) defines interprofessional collaboration as “multiple health workers from different professional backgrounds working together with patients, families, carers [sic], and communities to deliver the highest quality of care.”12 The collaborative identifies (1) values and ethics, (2) roles and responsibilities, (3) interprofessional communication, and (4) teams and teamwork as the 4 Core Competencies for Interprofessional Collaborative Practice.12 IPEC further describes competent students as being able to effectively use communication techniques to enhance team function, organize and share information with patients, families, and health care providers in a way that is appropriate for each, share knowledge with confidence and respectfulness, actively listen and encourage others’ ideas, use appropriate language, especially in difficult situations, and appreciate one’s own expertise within the health care team.12
Interpersonal communication involves communication between 2 or more individuals and considers both audience and contextual factors.13 Ideally, pharmacy graduates should exhibit satisfactory interpersonal communication skills across multiple audiences and contexts. Interprofessional communication considers both health care-specific audiences (eg, disciplines or professions) and contexts (eg, practice settings). The extent to which pharmacists engage in interpersonal and interprofessional communication is often practice-setting dependent.4 For example, community pharmacists may spend relatively more time interacting with patients in a dyadic, interpersonal manner and less time communicating with other health professional audiences, whereas pharmacists who go on rounds with a health care team in the institutional setting may devote relatively more time to interprofessional communication.
Engagement in interpersonal and interprofessional communication is also influenced in part by self-efficacy beliefs. Bandura’s self-efficacy theory posits that a positive relationship exists between task-specific communication self-efficacy and the extent to which individuals engage in interpersonal and interprofessional communication.14-16 Conversely, individuals with low task-specific self-efficacy beliefs are relatively more likely to refrain from engaging in communicative behaviors.17 Students who complete a health professions program without possessing the knowledge of and skills to engage in effective communication may be less likely to communicate with patients or fellow health professionals.18
Pharmacy educators are tasked with developing and/or refining students’ communication skills; however, the manner in which this occurs in schools/colleges varies.9,10,18-20 East Tennessee State University’s (ETSU’s) Academic Health Sciences Center (AHSC) requires medical, nursing, and pharmacy students to complete a course designed to strengthen both interpersonal and interprofessional communication skills. The objectives of this manuscript are to describe the design and implementation of a blended-learning, required, interprofessional communication skills course at ETSU’s AHSC and to assess health profession students’ interprofessional and interpersonal communication skills self-efficacy beliefs precourse and postcourse. We hypothesized that health profession students’ self-efficacy beliefs would improve by completing this course and thus increase the likelihood of engagement in interprofessional and interpersonal communication.
DESIGN
ETSU’s AHSC includes colleges of medicine, nursing, pharmacy, public health, and clinical and rehabilitative health sciences. ETSU received a large educational grant from the Kellogg Foundation in 1992 to advance interprofessional health care training with a rural focus, a portion of which was used to develop an interprofessional communication elective course. The success of the course led administrators to require it for all medical and nursing students in 2000, and for pharmacy students beginning in 2007 with the founding of the Bill Gatton College of Pharmacy. In the fall 2012 semester, the 2-credit hour “Communication Skills for Health Professionals” course enrolled 192 first-year medical, nursing, clinical psychology, and second-year pharmacy students.
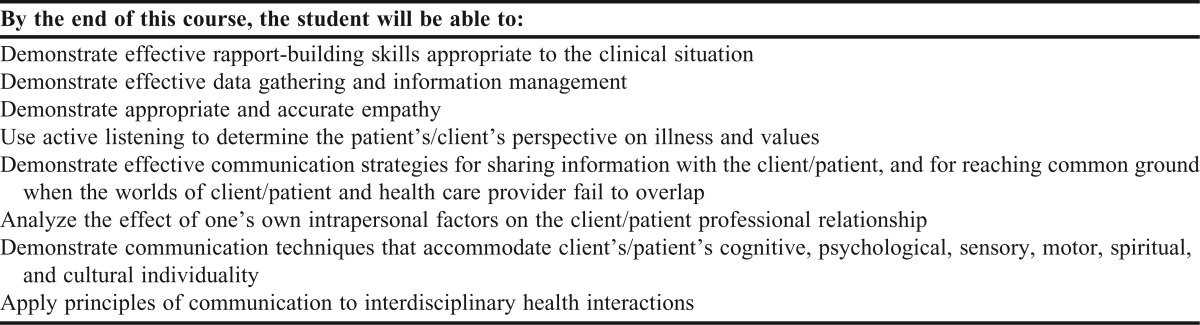
Learning objectives were developed by faculty members based on curricular outcomes across colleges and the IPEC Competencies (Table 1). Upon course completion, students were expected to be proficient in pre-identified core communication skills such as rapport building, information management, and active listening. Further, students were expected to acknowledge and apply appropriate communication principles and values to various settings and situations.
Table 1.
“Communication Skills for Health Professionals” Course Objectives
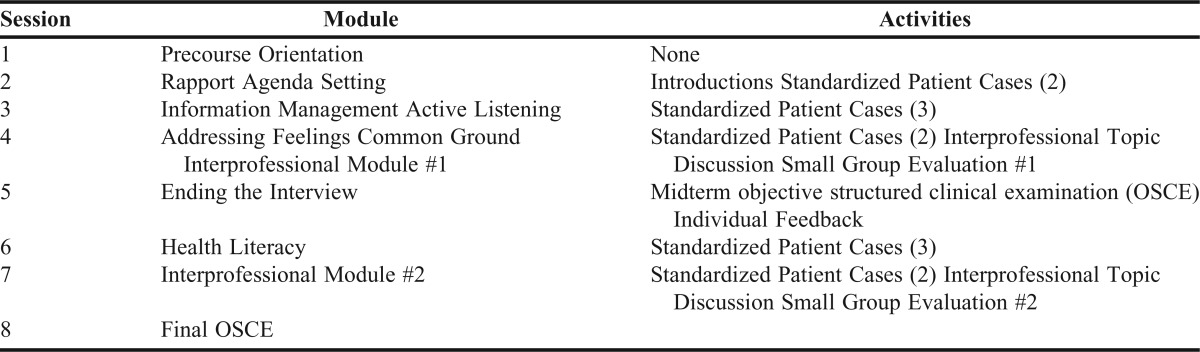
The course utilized a biweekly, blended learning format that incorporated computer-mediated, self-directed learning modules designed to introduce and teach students core communication skills (Table 2). Students were required to complete 1-3 preclass online modules per class period. Each module contained interactive presentations, video examples, and preclass assessments consisting of 2 or 3 open-ended questions. Each module contained approximately 40 slides to introduce students to the skills they would practice in their subsequent small group setting. Module content consisted of an introduction to a selected communication skill, individual elements that comprise the skill, step-by-step processes to implement the skill in an interview, and video examples of the skill being employed. Video vignettes portrayed both properly performed and poorly performed core communication skills. The total estimated time to complete each module and preclass assessment was roughly 1 hour.
Table 2.
Communication Skills for Health Professionals Schedule and Activities
Students were divided into small groups of 6-7 with stratified representation from each discipline (ie, medicine, nursing, pharmacy, psychology). The small groups met for 3 hours every other week. During every small group session, each student participated in standardized patient (SP) interviews and received constructive formative feedback from faculty members using the validated Common Ground Rating Scale.21 The scale was also employed as an assessment tool during objective structured clinical examinations (OSCE). Standardized patient scenarios were developed to focus on the core skills highlighted in the preclass module and incorporated skills discussed in previous modules. Purposefully organizing the modules enabled students to continually improve and build upon previous material and practiced skills. For example, students’ agenda setting skills, introduced in one online module, were thereafter developed through communication with an SP who had several health concerns. Students had to discover each concern, prioritize and address said concerns, and close the interview ensuring that each problem was adequately addressed. Cases were constructed with minimal focus on profession-specific competencies (eg, diagnoses, pharmacotherapy). Two to 3 different SP cases were incorporated into each small group session.
A faculty member from one of the participating colleges served as a facilitator for each student group. A 3-hour precourse training workshop was used to train new faculty facilitators in small group mediation and formative and summative assessment. Videos of student interviews and role-play techniques helped train faculty members to evaluate interview performances and to lead small group discussions. Faculty members were encouraged to have every student interview at least one SP during each small group session to promote skill development. The SPs were trained to lead students into a line of communication that allowed use of the introduced skills. The SPs were recruited and trained through the College of Medicine’s Standardized Patient Program.
Formal evaluations via an OSCE consisted of 8-minute recorded interviews at the midpoint (1 interview) and end (2 interviews) of the semester to assess achievement of course objectives. These interviews focused on utilizing interpersonal communication skills practiced in preOSCE small group meetings. For the midterm OSCE, students met one on one with their small group facilitator for 30 minutes to observe their recorded interview and assess their performance. Student-facilitator meetings and feedback did not occur following final OSCEs because of course scheduling logistics. The final OSCE examination, in addition to the 2 interviews, also consisted of an online component with which students viewed an interprofessional communication video of a physician, nurse, and pharmacist discussing the care of an end-of-life patient and answered reflective questions based on communication skills witnessed.
To emphasize interprofessional communication in the course, students participated in two 45-minute interprofessional communication discussions during 2 regularly scheduled small group meetings. The first interprofessional communication discussion centered on a scene from the film Wit that involved a disagreement between a physician and nurse and a short film produced by ETSU titled “Intensity in the ICU,” in which a seasoned nurse and medical resident disagree on patient care processes. Prior to class, students viewed the videos and answered open-ended questions to discuss in class. The discussion questions required students to identify and evaluate verbal and nonverbal communication, perceived power struggles in the interactions, causes of conflict, and alternative, more constructive means with which each situation could have been handled. The second interprofessional communication discussion focused on a paper-based case scenario in which a newly established patient sought a refill for a narcotic prescription from a prescriber. The scenario incorporated the refill history provided by the pharmacist and office visit summary from a weekend encounter with a nurse practitioner at a walk-in clinic. Students explored patient interests and expectations regarding pain control and medication prescribing, discovered the importance of interprofessional collaboration, and recommended solutions to the case.
In addition to facilitator-provided feedback, student peers also actively participated in the formative feedback portion of small group sessions. This period of reflection was essential as group members learned to provide constructive feedback to their interprofessional peers and noted communication skill use. Students received a small group grade based on their contribution to the group, interprofessional engagement in group discussion, and provision of feedback to peers.
To evaluate the impact of the course on student self-efficacy beliefs, the authors developed a 33-item survey instrument specific to course learning objectives and IPEC Core Competencies.12 Survey items were pilot-tested and revised for relevance and clarity by faculty members from each college, a survey methodologist, and 2 communication skills scholars. Students voluntarily completed the survey instrument before and after the required course. Given that only 4 clinical psychology students were enrolled in the course, analyses presented in this manuscript are limited to medical, nursing, and pharmacy students. Communication skill perceptions were gathered using a 5-point Likert scale. Students provided a coded identifier that was used to match precourse and postcourse surveys. Kruskal-Wallis, Mann-Whitney, and Wilcoxon signed rank tests were employed to examine matched preassessments and postassessments within colleges and to explore differences in self-efficacy beliefs across colleges. An a priori alpha level was set at 0.05. Data were analyzed using SPSS version 20 (IBM, Armonk, NY). The study was approved by the East Tennessee State University Institutional Review Board.
EVALUATION AND ASSESSMENT
One hundred percent of course enrollees completed the precourse assessment and 87% (n=167/192), the postcourse assessment. Twenty-seven of 33 survey item responses were significantly different across cohorts precourse, with nursing students reporting higher interpersonal and interprofessional communication self-efficacy scores across a majority of items compared to medical and pharmacy students. Among these differences, pharmacy students, in particular, noted significantly lower self-efficacy beliefs compared to other disciplines regarding their ability to communicate effectively with health care team members (p=0.014), use patient-engaging strategies to reach common ground when communicating (p=0.001), actively involve patients in health care plans (p=0.032), and effectively contribute as a member of a health care team (p=0.001) (Table 3).
Table 3.
Precourse Significant Response Frequencies Across Colleges
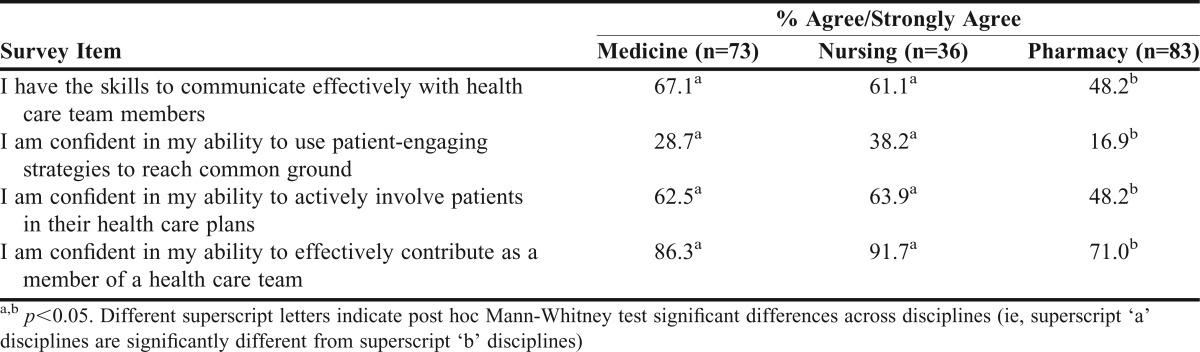
Table 4 presents student postcourse response frequencies and percent changes pre/post course for each survey item. Students from all 3 professions noted an increase in self-efficacy beliefs after completing the communications course. Only 3 items were significantly different across college cohorts postcourse (Table 5). Pharmacy students perceived relatively less confidence than their colleagues in medicine and nursing in their ability to develop positive interdependent relationships with other health care team members (p=0.020), and in their ability to use patient-engaging strategies to reach common ground (p=0.039). Medical and pharmacy students noted a lower understanding compared to nursing students of the roles of other health care team members (p=0.017).
Table 4.
Student Interprofessional and Interpersonal Communication Self-Efficacy Beliefs: Postcourse Response Frequencies and Percent Change Pre/Postcourse within Each Collegea

Table 5.
Postcourse Significant Response Frequencies and Percent Changes Across Colleges
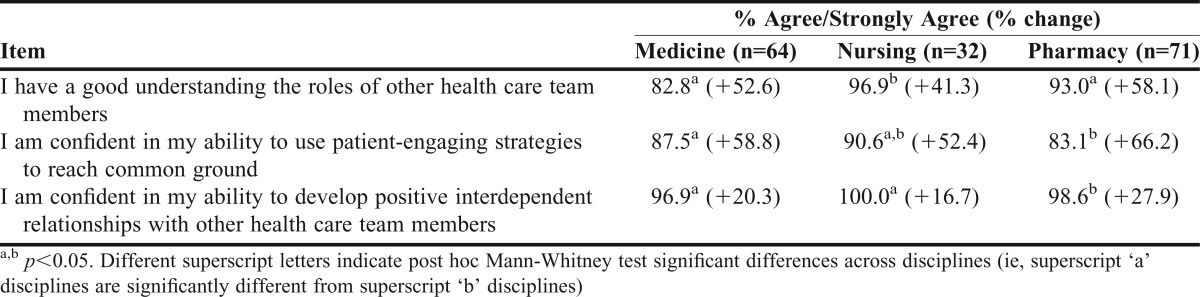
Pre-/postmatched analyses of pharmacy and medical student responses were all significant for improvement in self-efficacy (p<0.001). Despite nursing students’ high precourse self-efficacy belief rankings, matched analyses showed a significant improvement in self-efficacy beliefs for all but 1 survey item compared to precourse self-reports. Across health professions, pharmacy students demonstrated the greatest increase between pre/post course self-efficacy beliefs.
DISCUSSION
The Communication Skills for Health Professionals course improved students’ self-confidence in their communication skills across all 3 colleges. Even though causality cannot be implied, this is the first course in the medicine, nursing, and pharmacy curricula that addressed interpersonal and interprofessional communication. Overall, there was a 32.7% increase in agree/strongly agree responses from precourse to postcourse, and only 0.6% of students disagreed/strongly disagreed with the statements on the postcourse survey instrument. The most notable end-of-course achievement was that each discipline showed improved self-efficacy beliefs in interpersonal and interprofessional communication skills. Students noted increased confidence in their ability to utilize core communication skills in a simulated patient setting. Students were also more confident in their ability to respectfully collaborate with colleagues from other health care professions—a skill that they can carry with them as they enter the workforce.
Prior to taking the course, pharmacy students expressed lower self-efficacy beliefs than their nursing and medicine counterparts in 2 interpersonal domains (patient-engaging strategies and actively involving patients in their own care) and 2 interprofessional domains (developing relationships and recognizing roles). One of the demographic differences across cohorts was curricular progression; pharmacy students enrolled in the course were in their second professional year whereas medicine and nursing students were just beginning their first semester. Medical and nursing students beginning their respective programs may not have had enough time to accurately gauge their communication abilities, thus overestimating their confidence, whereas pharmacy students had had 2 semesters during which they had been able to calibrate communication abilities in both community and clinical settings prior to assessing communication skill self-confidence. Additionally, previous work experience may have allowed pharmacy students a greater opportunity for interpersonal and interprofessional encounters prior to enrolling in the course. While it is reasonable to expect previous student work and experiential education to result in stronger precourse self-efficacy beliefs, these experiences could provide a more realistic, lower estimation of confidence in communication abilities, especially interprofessional communication skills considering the isolation from physicians and nurses in many community pharmacy settings. Differences in precourse self-efficacy beliefs may also have been a function of differences in personality traits across professional cohorts. Despite differences precourse, results postcourse indicated course participation resulted in similar, positive self-efficacy beliefs across all professions, thus supporting engagement in interpersonal and interprofessional communicative behaviors.
The course underwent several revisions over the years that strengthened the interprofessional focus, including the addition of purposeful interprofessional communication skill development activities and integration of pharmacy-specific scenarios into curricular content. A weakness of the course design was the number of facilitators—each with his/her own teaching and communication styles—necessary to conduct small group sessions. However, results of our study were consistently positive despite fidelity limitations. Moreover, facilitator training was conducted to minimize this variation.
Barriers to conducting the course over the years included reserving adequate small group space, recruiting sufficient faculty facilitators to lead 30 small groups, and recruiting and training SPs. To overcome such barriers, a biweekly schedule was employed to make efficient use of limited resources. Creating a course of this magnitude required cooperation from deans, administrators, and faculty members. We overcame the need for space by using 3 buildings in close proximity to each other, each with rooms to accommodate small groups. The substantial faculty member commitment from each college was eased by allowing facilitators to conduct small groups on a biweekly basis.
Student feedback obtained via summative course evaluations was used to make improvements to the course and to provide constructive feedback to facilitators. Course coordinators from each discipline also annually reviewed module content based on student feedback and revised based on literature, if applicable. For example, per student feedback, and in combination with curricular revisions, the course was moved to the first year of the pharmacy curriculum to expose pharmacy students to these skills earlier in their didactic careers. As of this publication, precourse and postcourse survey responses were collected from 1 semester of the course. In an effort to examine relationships between self-efficacy belief perceptions and actual communication skills of students, further evaluation is underway to score videotaped student precourse and postcourse OSCEs, and thereafter compare OSCE outcomes to student self-efficacy beliefs. Longitudinal analysis is also warranted to track self-efficacy beliefs across the curriculum. Such an analysis could reveal gaps in the curriculum where certain communication skills warrant additional practice or instruction.
SUMMARY
Our findings suggest that a biweekly, blended learning interpersonal and interprofessional communication skills course positively impacted self-efficacy beliefs of medical, nursing, and pharmacy students at an academic health sciences center. Prior to taking the course, pharmacy students indicated less confidence than their medicine and nursing colleagues in some interpersonal and interprofessional communication skills. Implementation of such a course could increase the likelihood of future pharmacists engaging in communicative behaviors that promote and improve patient care.
ACKNOWLEDGMENTS
The authors would like to thank all expert panel members who invested time in the survey development. The authors also express appreciation to the students who participated in the study.
REFERENCES
- 1.Cipolle RJ, Strand L, Morley P. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management, Third Edition. McGraw Hill Professional. 2012 [Google Scholar]
- 2.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update) Cochrane Database Syst Rev. 2013;3:CD002213. doi: 10.1002/14651858.CD002213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 4.Duggan A. Understanding interpersonal communication processes across health contexts: advances in the last decade and challenges for the next decade. J Health Commun. 2006;11(1):93–108. doi: 10.1080/10810730500461125. [DOI] [PubMed] [Google Scholar]
- 5.Makoul G. Communication skills education in medical school and beyond. JAMA. 2003;289(1):93. doi: 10.1001/jama.289.1.93. [DOI] [PubMed] [Google Scholar]
- 6.Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–203. doi: 10.1056/NEJMp1211775. [DOI] [PubMed] [Google Scholar]
- 7.The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient- and Family-centered Care: A Roadmap for Hospitals. Oakbrook Terrace, IL: The Joint Commission, 2010.
- 8.Wright KB, Sparks L, O’Hair HD. Health Communication in the 21stCentury (2nded). Blackwell; 2013. [Google Scholar]
- 9.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the Doctor of Pharmacy degree. Chicago: Accreditation Council for Pharmacy Education; 2011. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. [Google Scholar]
- 10.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education (CAPE) 2013 Educational Outcomes. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leasure EL, Jones RR, Meade LB, et al. There is no “i” in teamwork in the patient-centered medical home: defining teamwork competencies for academic practice. Acad Med. 2013;88(5):585–592. doi: 10.1097/ACM.0b013e31828b0289. [DOI] [PubMed] [Google Scholar]
- 12.Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC; 2011.
- 13.Beebe SA, Beebe SJ, Redmond MV. Interpersonal Communication: Relating to Others. 6th ed. Allyn & Bacon; 2010.
- 14.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice Hall; 1986.
- 16.Bandura A. Self-Efficacy: The Exercise of Control. Macmillan; 1997.
- 17.McCroskey JC, McCroskey LL. Self-report as an approach to measuring communication competence. Communication Research Reports. 1988;5(2):108–113. [Google Scholar]
- 18.Rogers ER, King SR. The influence of a patient-counseling course on the communication apprehension, outcome expectations, and self-efficacy of first-year pharmacy students. Am J Pharm Educ. 2012;76(8):Article 152. doi: 10.5688/ajpe768152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beardsley RS. Communication skills development in colleges of pharmacy. Am J Pharm Educ. 2001;65:307–314. [Google Scholar]
- 20.Kimberlin CL. Communicating with patients: skills assessment in US colleges of pharmacy. Am J Pharm Educ. 2006;70(3):Article 67. doi: 10.5688/aj700367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lang F, Mccord R, Harvill L, Anderson DS. Communication assessment using the common ground instrument: psychometric properties. Fam Med. 2004;36(3):189–198. [PubMed] [Google Scholar]


