Abstract
Objective. To evaluate the effectiveness of asthma education delivered by student pharmacists and to assess the impact of child and caregiver baseline asthma knowledge on asthma control in children.
Design. Student pharmacists developed and implemented asthma self-management education interventions for children and their caregivers and performed asthma screenings for children at a series of asthma camps.
Assessment. Eighty-seven children, ages 5-17 years, and their caregivers were enrolled in this study. A previously validated asthma questionnaire was modified to assess asthma knowledge among children and adults. Asthma knowledge increased significantly in children following participation in the education intervention (p<0.001). The education intervention, however, did not increase caregiver knowledge of asthma. A significant association was observed between caregiver baseline asthma knowledge and better asthma control in their children (p=0.019).
Conclusion. The results of this study demonstrate that student pharmacist-delivered asthma education can positively impact asthma knowledge in children, and that caregivers’ knowledge of asthma is strongly correlated with better asthma control in their children.
Keywords: asthma, education, experiential, camp, interdisciplinary
INTRODUCTION
Asthma is the most common chronic disease among children in the United States.1 The National Heart, Lung and Blood Institute (NHLBI) guidelines for the diagnosis and management of asthma emphasize the importance of asthma self-management education, even including it as 1 of the 4 key components of effective asthma management.2 Previous studies showed that asthma self-management education programs for children and adolescents improve lung function and feelings of self control, and reduce missed school days, days with restricted activity, and emergency room visits.3 Only 12 percent of people with asthma received formal patient education in 2008, according to the National Health Interview Survey (NHIS).4 Thus, increasing dissemination of formal education to people with asthma is one of the objectives of Healthy People 2020.5 Many primary care pediatricians are not able to routinely provide asthma education in accordance with NHLBI asthma guidelines because time is constrained and demands compete during typical visits.6 Lack of routine primary care visits can further limit children’s receipt of asthma education. Therefore, alternative methods of providing asthma education are recommended.2
The asthma guidelines recommend asthma education interventions be repetitious, which requires reinforcement by all members of the health care team at various points of care. They also recommend use of interventions provided by pharmacists be considered; “such programs are feasible, and they merit further studies of effectiveness.”2 Previous studies showed that community pharmacy-based asthma education could have a positive impact on asthma-related outcomes when delivered as part of a structured program.7-8 However, the frequency of asthma education delivered by pharmacists in the community setting can be limited by both patient-related and practice-related obstacles (ie, space constraints, patient attitudes towards pharmacists as asthma educators, and limited pharmacist knowledge regarding optimal asthma management).9-10 Methods to overcome these obstacles need to be explored so that interventions provided by pharmacists become recommended instead of only considered.
The Center for the Advancement of Pharmacy Education (CAPE) 2013 Educational Outcomes recommend that pharmacists be “capable of functioning collaboratively as members of an interprofessional team, advocating for patients and demonstrating leadership, providing care for diverse patient populations, contributing to the health and wellness of individuals and communities, and educating a broad range of constituents.”11 In an effort to address the above needs and obstacles, the For Your Good Health, LLC. (FYGH) asthma camp series was developed to teach children and caregivers asthma self-management skills in a camp environment. This interdisciplinary camp model was directed by a group of physicians and pharmacists and staffed by student pharmacists and university athletes.
The primary objective of this study was to evaluate the impact of student pharmacist delivered asthma education on child and caregiver knowledge of asthma. The secondary objective was to assess child and caregiver baseline asthma knowledge and its effect on asthma control in children attending the asthma camps.
DESIGN
This cross-sectional study received Institutional Review Board approval from Duquesne University prior to implementation. The FYGH asthma camps were hosted at Duquesne University’s A.J. Palumbo Center, a sports complex in downtown Pittsburgh. Previous studies showed that caregiver knowledge of asthma and asthma treatment could improve asthma control and severity in children.12 Therefore, caregivers were strongly encouraged (though not required) to attend the camps and participate in the educational activities with their children so they could reinforce key concepts at home and increase their own asthma knowledge. The camp setting provided adequate space for large groups of children and caregivers to receive formal education. The asthma guidelines support the delivery of asthma education in community settings, stating that they can “positively affect large numbers of persons who have asthma, especially in poor, inner-city communities.”2 Six day camps were offered over a period of 2 years—3 per summer. Camps were held on Saturdays from 9:00am to 2:00pm. Asthma screenings and education were conducted during the morning session, a healthy lunch was provided, and the afternoon ended with sports skills instruction. Duquesne University student pharmacists developed and implemented the asthma education interventions and performed the asthma screening assessments, with training and oversight provided by pharmacist and physician faculty members. Sports skills were taught by Duquesne University student athletes and coaches. Caregivers were encouraged to watch the sports skills session so that they could continue to help their children with these skills at home.
The camps were offered to all children in the Pittsburgh area free of cost. Children with and without a prior diagnosis of asthma were encouraged to attend so this model’s effectiveness at identifying children with undiagnosed and uncontrolled asthma could be evaluated and recommendations for follow-up care could be provided.13 Participating children were required to attend 1 of the 6 FYGH asthma camps. Study consent was not required for camp enrollment. Six health screenings were held at various locations throughout Pittsburgh each spring prior to the summer asthma camp in an effort to increase identification of children with potential undiagnosed or uncontrolled asthma and related complications (obesity, hypertension, and tobacco smoke exposure) and to invite them to attend the asthma camp series. The majority of screenings were held at afterschool programs and at public housing projects. Asthma, blood pressure (BP), body mass index (BMI), and tobacco smoke exposure screenings were the only services provided at the community-based events. Fliers for the camps were distributed at each screening and children and caregivers were encouraged to attend. Other methods for camp recruitment included mass e-mails to local hospitals and universities, posters and fliers distributed at pediatric practices, sports leagues, schools and churches, media releases, and advertisements in local newspapers and health bulletins. Research assistants obtained written consent and assent for participation in the study during camp registration. If children attended multiple camps, written consent and assent was required prior to each camp. Children were not restricted from participation in multiple camps and if they did so, they were counted as separate subjects for each session.
Strategies utilized for sample retention included having well-known athletes provide sports instruction (eg, university athletes and coaches), providing free wellness screenings and counseling for caregivers (eg, blood pressure, cholesterol, BMI), providing t-shirts, basketballs, backpacks, and water bottles with the FYGH logo on them (which also increased awareness of the camps), raffling off giveaways for children and caregivers that included prizes such as iPods and gift cards, and providing free lunch.
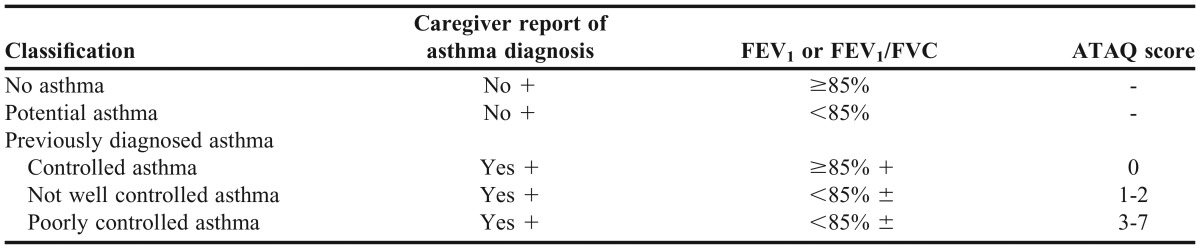
Demographic information such as age, gender, race, and ethnicity was collected during camp registration via a permission slip that parents were required to complete for participation in the camp, regardless of participation in the study. Parental report of asthma diagnosis was used along with Spirometry (KoKo Legend portable spirometer, Inspire Health, Longmont, CO) and the Asthma Therapy Assessment Questionnaire (ATAQ)14 to classify lung function in all children attending the camps, regardless of prior asthma diagnosis. The asthma screening classification system was used in this study is described in Table 1.
Table 1.
Asthma Screening Classification
Under the guidance of 2 pharmacist faculty members and as part of an advanced experiential education requirement, various groups of sixth-year student pharmacists developed hands-on, interactive educational activities that were implemented at each camp. The student pharmacists were required to review the NHLBI guidelines during their first week of practice experience. They were then given 2 weeks to develop the educational activities, which gave faculty members time to ensure the interventions adequately addressed the 4 key components of effective asthma management (avoidance of asthma triggers, compliance with asthma medication, proper inhaler technique, and the importance of an asthma action plan), and that the interventions were appropriate for the intended audience. The students were instructed to make the lessons less academic and more hands-on. This project required higher order thinking skills as students were asked to synthesize new information in order to develop novel educational activities. Numerous activities were created, such as interactive skits to teach proper inhaler technique, game shows highlighting the differences between controller and reliever medication, and a memory game of asthma triggers. One group created a large cardboard house that contained common asthma triggers. They worked with small groups of children to make the house more “asthma friendly,” discussing ways to either eliminate or decrease exposure to each of the triggers. Each activity lasted up to 15 minutes, and small groups of children and caregivers rotated through each of the 4 stations. Having multiple student pharmacists present allowed for various educational activities that reinforced important aspects of optimal asthma management. All children and caregivers, regardless of prior asthma diagnosis, were encouraged to participate in the education sessions.
A simplified version of Fitzclarence and Henry’s 31-question Asthma Knowledge Questionnaire to assess caregiver knowledge of asthma was administered to children and their caregivers during the camps. 15 Fewer than half the questions from the original questionnaire were included in an effort to decrease administration time. Each specific question was chosen based upon adequate coverage of the topic during the camp and level of perceived difficulty. Pictorial representation was used when possible, and “circle the above” and “yes/no” questions were used most frequently. The questionnaire was administered to children and caregivers separately at the beginning and end of each camp to assess the effectiveness of the intervention. Each questionnaire was administered and graded by study personnel, took roughly 10 minutes to complete, and was worth 15 possible points.
Statistical analyses, including simple descriptive statistics and simple tests of hypotheses, were performed using JMP version 10 (SAS Institute Inc., Cary, NC). Statistical analysis of initial and final asthma knowledge scores required a paired comparison of calculated differences, the null hypothesis for which was that the average of the paired differences was zero. This method improved the sensitivity of the test, compared to a standard 2-group comparison of averages, by letting each subject serve as their own control. Logistic regression was used for testing hypotheses between a categorical dependent variable (such as asthma control) and a continuous independent response (such as preintervention asthma knowledge test scores). A 1-way ANOVA was used to test the reverse case involving a categorical independent variable and a continuous dependent variable. In all cases, the alpha level for significance was established as 0.05.
EVALUTATION AND ASSESSMENT
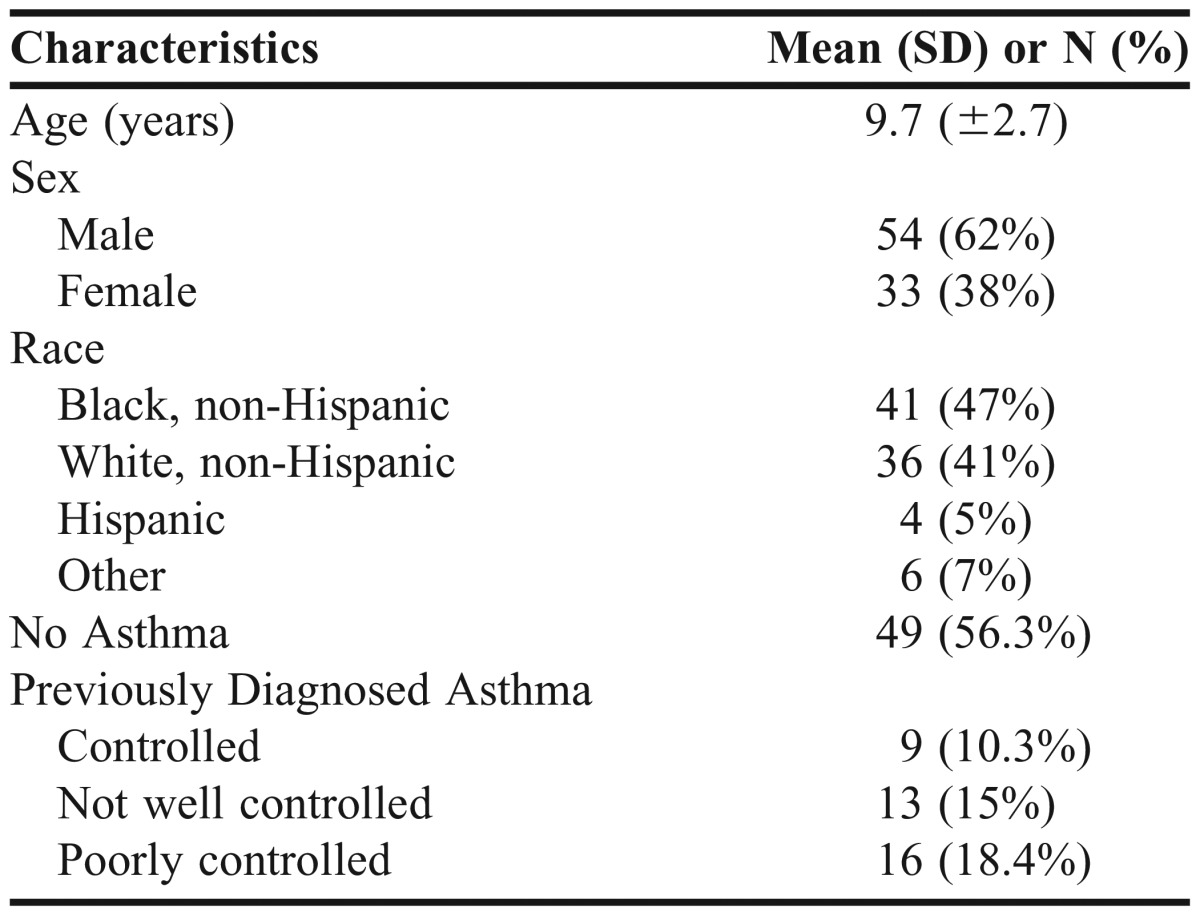
Eighty-seven children and their caregivers were enrolled in the asthma camp study over the 2 years. Four children attended more than 1 camp, but each was counted as a unique subject for each session. Demographic characteristics and results from the asthma screening are presented in Table 2.13
Table 2.
Demographic Characteristics and Asthma Screening Results
All 87 children participated in the educational intervention and completed the preintervention knowledge test, but 11 (13%) elected not to complete the postintervention knowledge test. Only 45 caregivers (52%) participated in the educational intervention, and 42 (48%) completed the preintervention and postintervention knowledge tests. Complete preintervention and postintervention tests were collected for 76 children (87%) and 42 caregivers (48%). The mean difference among children between the preintervention test (10.4 ± 2.7) and postintervention test (12.9 ± 2.2) was 2.5 ± 2.5 (p<0.001). The mean difference among caregivers between the preintervention test (8.8 ± 4.3) and postintervention test (8.4 ± 4.3) was -0.33 ± 5.3 (p=0.68).
No correlation was observed between preintervention test scores and asthma control for children with previously diagnosed asthma. The association was tested using a 1-way analysis of variance, which suggested that the 3 groups were essentially equivalent at the alpha equal to 0.05 level. We did discover a significant association between caregiver preintervention test scores and asthma control in their children (p=0.019). Higher average preintervention test scores in caregivers were associated with “controlled” and “not well controlled” asthma in their children (mean test scores, 12.8 and 11.5, respectively), whereas lower scores (mean test score, 8.54) corresponded to “poorly controlled” asthma.
DISCUSSION
This study demonstrated that student pharmacist-delivered asthma education was effective in increasing asthma knowledge in children. Previous studies evaluated student pharmacist-delivered screenings and education in adults with various disease states,16, 17 but this is the first study to assess the effectiveness of student pharmacists as asthma educators in the pediatric population. Knowledge of asthma pathophysiology, symptoms, triggers, and medication use increased significantly in the child cohort following participation in the education intervention.
Student pharmacist-delivered asthma education, however, did not increase asthma knowledge in the caregiver cohort. Some parents did not attend the camp with their child, and some who did attend chose not to participate in the educational intervention. This was evident in the lower number of completed preintervention and postintervention tests for caregivers compared to children (48% and 87%, respectively). It was observed that many of the caregivers who did not participate in the educational activities spent their time socializing with other caregivers. Therefore, we plan to develop a separate educational track for caregivers in the future. This may enhance participation for those who wanted to give their children autonomy in camp participation, or for those who just preferred adult socialization. Lack of participation could also have been a result of the fact that the majority of children (56%) attending the camps did not have a previous asthma diagnosis and their parents did not, therefore, have a personal incentive to participate. Interestingly, child preintervention test scores were higher than caregiver preintervention test scores, suggesting greater baseline knowledge of asthma in children. This could be the result of few existing asthma education models targeting caregivers or of selection bias, with caregivers having less asthma knowledge electing to participate in the education intervention.
Previous studies noted that asthma counseling is infrequent in community pharmacies, with major limiting factors being time constraints and limited facilities to conduct patient education.9 Sixth-year student pharmacists completing experiential learning have more time to devote to the development and delivery of novel asthma education interventions, as well as the necessary training and support to do so effectively. In turn, this process is a great learning experience for student pharmacists.
The secondary objective of this study was to assess the effect of child and caregiver baseline knowledge of asthma on asthma control in children with previously diagnosed asthma. A correlation between baseline asthma knowledge and asthma control was not observed in children attending the sports camps. A significant association was, however, discovered between caregiver preintervention test scores and asthma control in their children, with higher test scores observed for caregivers whose children had controlled or not well controlled asthma compared to those with poorly controlled asthma. These findings are comparable to previous studies, which showed caregiver-child education had a more favorable effect than child education alone on asthma morbidity.18 Children need the support of caregivers to help them avoid asthma triggers and to ensure compliance with asthma medication regimens. The correlation between asthma control and caregiver knowledge, coupled with decreased baseline asthma knowledge and engagement, highlights the demand for programs that specifically target the educational needs of caregivers.
Caregivers and children provided positive feedback on the camp model. One family drove more than 300 miles to attend because they couldn’t find a similar camp in their area. One caregiver said she thought she knew a lot about controlling asthma, but the camp presented new information to her. One child described the camp as life-changing because her breathing difficulties had prevented her from participating in sports and resulted in underdeveloped motor skills. Her caregiver explained that no one had worked with her on her missing skills but that changed dramatically at the camp when she learned how critical physical activity is to her well-being. Since attending the camp, the child’s physical activity level changed significantly, from walking only to the bus stop to routinely walking, and even running.
The development and implementation of the camps was time and resource intensive. Our core interdisciplinary group consisted of 2 pharmacist faculty members and 2 physicians. We staffed the camps with student pharmacist and athlete volunteers, which entailed additional training. Our pharmacy practice residents assisted with student pharmacist training and organization, and the assistant director of intercollegiate athletics recruited and trained student athletes.
There were several limitations to our study. First, the asthma classification system we used relied on caregiver recall to document asthma diagnosis and to further classify children with previously diagnosed asthma according to asthma control level using the ATAQ. Caregiver-provided medical histories can be unreliable, and recall bias and symptom perception are both limitations in using such questionnaires. Second, despite being modified from a previously validated asthma knowledge questionnaire, our version of the questionnaire was not validated. Future goals include assessing the reliability and internal consistency of this questionnaire when administered to pediatric subjects. There were also different student pharmacists who provided the educational interventions at each camp, and this was not accounted for in the study analysis. Lastly, this study consisted of a convenience sample of subjects who voluntarily attended one of the asthma camps, and, therefore, may not be representative of the entire population.
SUMMARY
Our study demonstrated that student pharmacist-delivered asthma education can positively impact asthma knowledge in children. The results also demonstrated the need for new programs to target the educational needs of caregivers. Caregiver asthma knowledge was strongly associated with better asthma control in children with a previous diagnosis of asthma. Additionally, the caregivers in this study had lower baseline asthma knowledge compared to the children, and were not effectively impacted or engaged in the education interventions. Further research is needed to develop comprehensive asthma education programs that meet the needs of both children and caregivers.
ACKNOWLEDGMENTS
This project was funded, in part, under grants from the Pennsylvania Department of Health and For Your Good Health, LLC. The authors would like to acknowledge Sherene Lemonias, assistant athletic director at Duquesne University, for organizing and overseeing the sports skills at each camp.
REFERENCES
- 1.Zahran HS, Bailey C, Garbe P. Vital Signs: asthma prevalence, disease characteristics, and self-management education-United States, 2001-2009. MMWR. 2011;60(17):547–552. [PubMed] [Google Scholar]
- 2.EPR. Expert panel report 3: Guidelines for the diagnosis and management of asthma (EPR 2007). NIH Publication Number 08-5846. Bethesda, MD: U.S. Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program, 2007.
- 3.Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: systematic review and meta-analysis. BMJ. 2003;326(7402):1308–1309. doi: 10.1136/bmj.326.7402.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control. National Health Interview Survey (NHIS) data: 2008 lifetime and current asthma. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. http://www.cdc.gov/asthma/nhis/08/data.htm. Accessed July 8, 2013.
- 5.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=36. Accessed July 8, 2013. [PubMed] [Google Scholar]
- 6.Cabana MD, Chaffin DC, Jarlsberg LG, et al. Selective provision of asthma self-management tools to families. Pediatrics. 2007;121:e900. doi: 10.1542/peds.2007-1559. [DOI] [PubMed] [Google Scholar]
- 7.McLean W, Gillis J, Waller R. The BC Community Pharmacy Asthma Study: a study of clinical, economic and holistic outcomes influenced by an asthma care protocol provided by specially trained community pharmacists in British Columbia. Can Respir J. 2003;10(4):195–202. doi: 10.1155/2003/736042. [DOI] [PubMed] [Google Scholar]
- 8.Saini B, Krass I, Armour C. Development, implementation, and evaluation of a community pharmacy-based asthma care model. Ann Pharmacother. 2004;38(11):1954–1960. doi: 10.1345/aph.1E045. [DOI] [PubMed] [Google Scholar]
- 9.Osman LM, Bond CM, MacKenzie J, Williams S. Asthma advice giving by community pharmacists. Int J Pharm Pract. 1999;7:12–17. [Google Scholar]
- 10.Stergachis A, Gardner JS, Anderson MT, Sullivan SD. Improving pediatric asthma outcomes in the community setting: does pharmaceutical care make a difference? J Am Pharm Assoc. 2002;42(5):743–752. doi: 10.1331/108658002764653522. [DOI] [PubMed] [Google Scholar]
- 11.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education (CAPE) Educational Outcomes 2013. Am J Pharm Educ. 2013;77(8):Article S8. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Largo TW, Borgialli M, Wisinski CL, et al. Healthy Homes University: a home-based environmental intervention and education program for families with pediatric asthma in Michigan. Public Health Rep. 2011;126(1):14–26. doi: 10.1177/00333549111260S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elliott JP, Marcotullio N, Skoner DP, Lunney P, Gentile DA. An asthma sports camp series to identify children with possible asthma and cardiovascular risk factors. J Asthma. 2013 Dec 19 [Epub ahead of print] [DOI] [PubMed]
- 14.Skinner EA, Diette GB, Algatt-Bergstrom PJ, et al. The asthma therapy assessment questionnaire (ATAQ) for children and adolescents. Dis Manag. 2004;7(4):305–313. doi: 10.1089/dis.2004.7.305. [DOI] [PubMed] [Google Scholar]
- 15.Fitzclarence CA, Henry RL. Validation of an asthma knowledge questionnaire. J Paediatr Child Health. 1990;26:200–204. doi: 10.1111/j.1440-1754.1990.tb02429.x. [DOI] [PubMed] [Google Scholar]
- 16.Letassy N, Dennis V, Lyons T, et al. Know your diabetes risk project: student pharmacists educating adults about diabetes risk in a community pharmacy setting. J Am Pharm Assoc. 2010;50:188–194. doi: 10.1331/JAPhA.2010.09206. [DOI] [PubMed] [Google Scholar]
- 17.Harris C, Doucette W, Reist J, Nelson K. Organization and results of student pharmacist bone mineral density screenings in women. J Am Pharm Assoc. 2011;51:100–104. doi: 10.1331/JAPhA.2011.09062. [DOI] [PubMed] [Google Scholar]
- 18.Findley S, Thomas G, Madera-Reese R, et al. A community-based strategy for improving asthma management outcomes for preschoolers. J Urban Health. 2011;88(1):85–99. doi: 10.1007/s11524-010-9479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


