BACKGROUND AND CHARGES
According to the Bylaws of the American Association of Colleges of Pharmacy (AACP), the Professional Affairs Committee is to study issues associated with the professional practice as they relate to pharmaceutical education, and to establish and improve working relationships with all other organizations in the field of health affairs. The Committee is also encouraged to address related agenda items relevant to its Bylaws charge and to identify issues for consideration by subsequent committees, task forces, commissions, or other groups.
President Peggy Piascik established the theme for 2013-2014 as “the relentless pursuit of excellence.”1 President Piascik acknowledges that academic pharmacy is at the crossroads of many areas of change, including the continuing evolution of pharmacy as a profession, how health care is delivered in America and rapid changes in higher education. As the roles of pharmacists continue to change, pharmacy technician roles must also evolve, necessitating changes in pharmacy technician training and education. Specifically, the 2013-2014 Professional Affairs Committee is charged to: (1) Describe the elements that should be present in a quality technician education/training program; (2) Identify potential role(s) of pharmacy academic institutions and pharmacy faculty in the education, training, and certification of pharmacy technicians; and (3) Recommend strategies to develop collaborations/relationships between schools/colleges of pharmacy and pharmacy technician education/training programs to advance pharmacy practice in the evolving health care system.
Members of the Professional Affairs Committee (PAC) include faculty representing multiple disciplines from various schools/colleges of pharmacy, a coordinator from an American Society of Health-Systems Pharmacists (ASHP) accredited pharmacy technician education/training program as well as professional staff from ASHP, the Pharmacy Technician Certification Board (PTCB) and the Pharmacy Technician Educators Council (PTEC).
Prior to an in-person meeting of the committee, pertinent background information and resource materials were distributed, and a conference call was held to develop a strategy for addressing committee charges. The committee members met for a day and a half in Crystal City, Virginia on October 28-29, 2013, to discuss the various facets related to this issue as well as to develop a process and strategies for addressing the charges. Following the process development and delegation of assignments related to the committee charges, the PAC communicated via electronic communications, as well as through personal exchanges via telephone and email.
The result is the following report, which discusses the elements and importance of a well educated and trained pharmacy technician workforce and also provides information on current collaborations between schools/colleges of pharmacy and pharmacy technician education/training programs. Disseminating the purpose and framework behind these collaborations may assist members of the academy to identify potential strategies and roles for schools/colleges of pharmacy in the education, training and certification of pharmacy technicians. In addition, these examples may help to guide the development of these collaborations at other member institutions. Pharmacy technicians are viable members of the health care sector and are necessary to the pharmacy profession for pharmacists to satisfy the Joint Commissioners of Pharmacy Practice (JCPP)Vision for Pharmacy Practice:2 Patients achieve optimal health and medication outcomes with pharmacists as essential and accountable providers within patient‐centered, team-based health care.
Charge 1: Describe the elements that should be present in a quality technician education/training program
A pharmacy technician is an individual who, under the supervision of a licensed pharmacist, assists in pharmacy activities that do not require the professional judgment of a pharmacist.3 The Occupational Outlook Handbook of the Bureau of Labor Statistics forecasts a positive demand for pharmacy technician positions. The average growth rate for pharmacy technicians for the 10-year timeframe between 2012 and 2022 is projected at 20% compared with 11% for all occupations.4 There were 355,300 pharmacy technician positions in 2012 and there is a projected numeric increase of 70,700 pharmacy technician positions between 2012 and 2022.4 As pharmacists assume a larger number of patient-centered roles, pharmacy technicians are increasingly responsible, under pharmacist supervision, for technical and distributive functions such as computer entry, labeling, medication preparation, record keeping, and maintenance of an appropriate supply of medications in pharmacies in all settings.3,5 Evolving roles of pharmacy technicians include participating in medication adherence services, medication safety, pharmacy benefit management, immunization assistance, supply chain management, informatics, transitions of care and medication therapy management services.5,6
The PAC decided to provide information regarding the evolution of the pharmacy technician education, training, certification and accreditation to inform the academy and to fulfill this charge. Pharmacy technician education/training, certification and program accreditation has developed substantially over the past thirty years. There is evidence of the development of quality in each of these facets for pharmacy technicians that is currently demonstrated in student pharmacist education/training at schools/colleges of pharmacy. In order to appreciate the elements that should be present to ensure a knowledgeable and trained pharmacy technician, as well as the value of the pharmacy technician to the health care workforce, it is important to understand the development of the education, training and certification of pharmacy technicians, as well as the accreditation of pharmacy technician education/training programs. Appendix A contains a glossary of terms that are useful when examining this evolution.
Pharmacy Technician Education/Training Program Accreditation
Education involves conveying knowledge, understanding and cultivating reasoning abilities while training involves teaching skills and building proficiency through actual practice.7 Pharmacy technician education/training programs are responsible for the cultivation and development of pharmacy technicians as schools/colleges of pharmacy are responsible for the cultivation and development of student pharmacists.
An examination of pharmacy technician education/training and regulations in other countries demonstrates how important this role is to health care. The Pharmacy Examining Board of Canada sets the standards for registered pharmacy technicians. The first step for a person interested in becoming a pharmacy technician is to enroll in a program that has been accredited by the Canadian Council for Accreditation of Pharmacy Programs (CCAPP).8 The next step is Structured Practical Training. An approved educational program and practical training will help prospective technicians meet the standards set by the National Association of Pharmacy Regulatory Authorities (NAPRA).8 Standards include receiving and preparing prescriptions, complying with legal regulations, collaborating with other members of a health care team, and maintaining quality control standards. Completion of these steps allows technicians to sit for exams through the Pharmacy Technician Qualifying Board, which was piloted in Alberta and Ontario in 2010.8 The Pharmacy Technician Qualifying Exam is a rigorous two-part assessment. The first, the MCQ, is a multiple choice exam consisting of 170 questions.8 The second part, the OSPE, consists of stations that technicians must complete.8 In some stations, candidates write their responses. In others, they interact with people in situations designed to simulate situations that could happen at work. An exam of jurisprudence, or law and ethics, is also required.
Becoming a pharmacy technician in Great Britain requires a formalized education/training process. Since 2011, pharmacy technicians are legally required to be registered with the General Pharmaceutical Council (GPhC) to practice in Great Britain.9 In order to register, the pharmacy technician needs to complete both knowledge and competency-based qualifications which have been approved by the GPhC.9 These qualifications may be studied separately, for example by earning a diploma in Pharmacy Service Skills or earning a national certificate in pharmacy services that meets the country’s Qualifications and Credit Framework (QCF).9 A pharmacy technician can also complete a single qualification, such as the National Pharmacy Association Level 3 qualifications, which combines both the knowledge and the competency elements. Regardless of the training/competency route, pharmacy technician training usually takes two years to complete and involves a combination of study either at a college or by open learning, in addition to practical work experience.9 The GPhC determines the amount of relevant work experience required for registration.
While most pharmacy technicians in the US have been trained on the job, either formally or informally, more individuals are enrolling in formal pharmacy technician education/training programs.3 Pharmacy technician education/training programs are generally affiliated with a vocational school, a community college, or a university, hospital, or another health care organization (i.e., pharmacy employer).3 Pharmacy technician education/training programs are found in the public and private sectors, may be for-profit or not-for-profit, and may be accredited.10 There are multiple pathways to pharmacy technician education/training including high school apprentice programs, community and technician colleges, the military, continuing education programs, career and trade schools, hospital-owned programs, online programs, partnerships between online didactic programs with local experiential training, pharmacy retailers and open source courses (i.e., Massive Open Online Courses [MOOCs]).10 The credentials of the individuals who teach in pharmacy technician education/training programs can vary, especially for those programs that are not accredited.10 Credentials for graduates of pharmacy technician education/training programs vary and may include a certificate of completion or an associate degree.3
Accreditation is an integral aspect of ensuring a quality educational experience. Accreditation provides enhanced recruitment potential for pharmacy technician trainees, improved marketing of pharmacy technician education/training programs, and the opportunity for peer review and quality improvement. There are two types of accreditation for pharmacy technician education/training programs: institutional and programmatic (also known as specialized). Institutional accreditation evaluates the educational institution as a whole, with less attention paid to the standards of individual programs offered by the institution; whereas programmatic accreditation focuses specifically on an individual program.11 Agencies that execute national institutional accreditation of pharmacy technician education/training programs are recognized by the US Department of Education, and none has a formal national affiliation with the pharmacy profession.
Program accreditation for pharmacy technician education/training programs is offered by ASHP. There are currently 258 pharmacy technician education/training programs in the ASHP accreditation process.12 ASHP is one of the four national organizations (which included AACP, the American Pharmacists Association [APhA] and the National Association of Retail Druggists [now known as the National Community Pharmacists Association [NCPA]) who led a pharmacy profession study in the 1960’s on the role of pharmacy technicians, which led to the US Department of Health, Education & Welfare to recommend the development of a pharmacist aide curriculum.13 In the 1970s, ASHP developed training guidelines and competency standards for hospital supportive personnel.13 This led to the initiation of ASHP providing accreditation of pharmacy technician education/training programs in 1982 at the request of hospital pharmacists who expressed a need for a more formal method of oversight to ensure the quality of training.13 In 1988, the ASHP Foundation held an invitational conference on pharmacy technical personnel, and almost a decade later in 1996, the first model curriculum for pharmacy technician training was developed by ASHP, APhA, AACP, PTEC and the American Association of Pharmacy Technicians (AAPT). The Model Curriculum provides a starting point for identifying core competencies for pharmacy technicians and a framework for training pharmacy technicians for all practice settings and geographic locations.5 The second model curriculum was developed in 2001 by the aforementioned associations and the National Association of Chain Drug Stores (NACDS).13
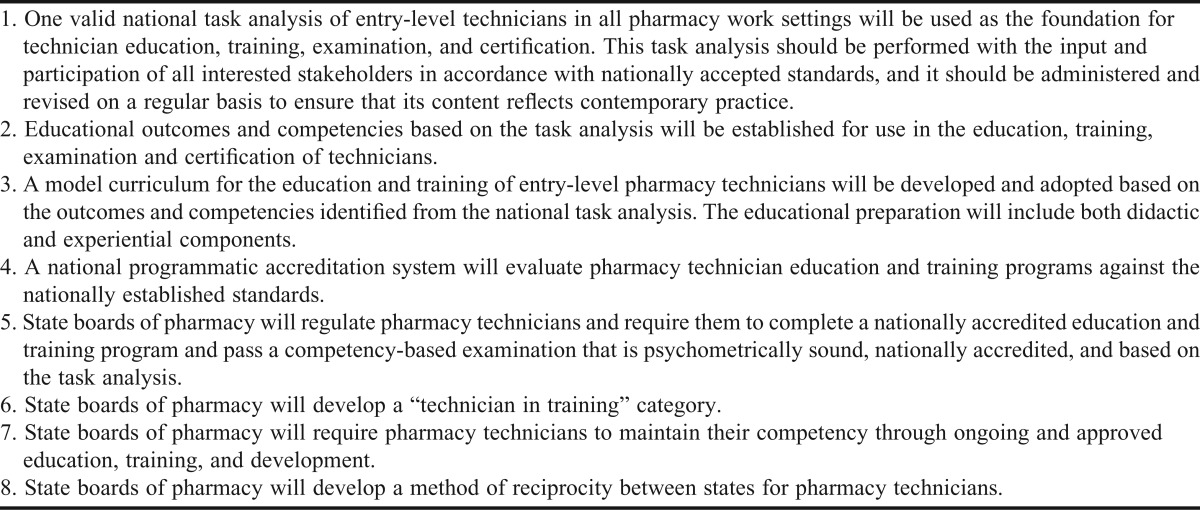
The ASHP Commission on Credentialing (COC) is responsible for the accreditation of pharmacy residency programs and pharmacy technician education/training programs. In 2004, the COC dedicated a specific seat on the commission to pharmacy technician education/training. In 2009, the Council on Credentialing in Pharmacy (CCP) developed the Pharmacy Technician Credentialing Framework,14 which provides guidance for policy development regarding the education, training, certification and regulation of pharmacy technicians in the US (Table 1). In 2013, the ASHP COC finalized a new accreditation standard15 and guidance document16 for pharmacy technician education/training programs (effective January 15, 2015), which was developed to protect the public, serve as a guide for pharmacy technician education/training program development, provide criteria for the evaluation of new and established programs and promote continuous improvement of established programs. ASHP utilizes the PTCB’s scope of practice analysis data to determine the required outcomes for programs.5
Table 1.
Council on Credentialing in Pharmacy: Pharmacy Technician Credentialing Framework Elements14
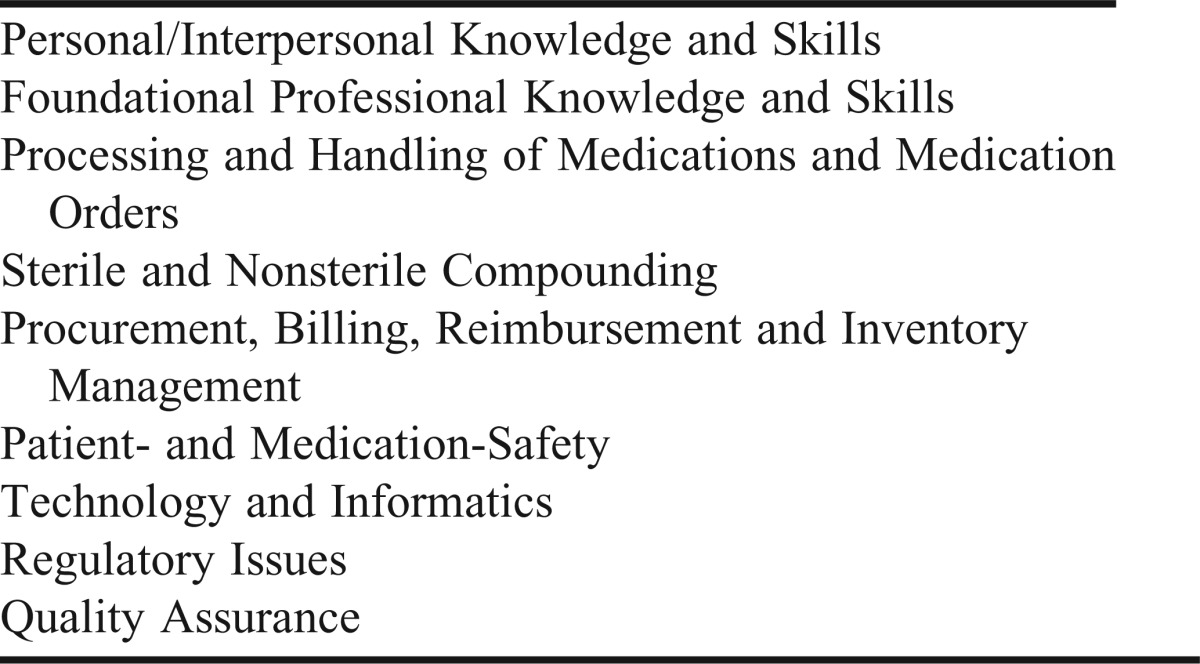
There are six components to the new standard, including Administration, Program Faculty, Education and Training, Students, Evaluation and Assessment, and Graduation and Certificate.15 The standard mandates the program composition be a minimum of 600 hours (160 hours of didactic training, 80 hours of simulation (laboratory) training, 180 hours of experiential in at least 2 different practice sites (one of which must be a dispensing pharmacy), and 200 hours up to the programs’ discretion).15 There is also an updated Model Curriculum that provides detail on how to meet the goals defined in the new accreditation standard for pharmacy technician education/training programs.17 The Model Curriculum goal categories are listed in Table 2. The Model Curriculum includes objectives and instructional objectives for each of the goal categories, as well as examples of learning activities for each portion of the program, including the didactic, simulated (laboratory), and experiential program components.17
Table 2:
American Association of Health-System Pharmacists (ASHP) Model Curriculum Goal Categories17
In August 2013, the formation of the Pharmacy Technician Accreditation Commission (PTAC) was announced.18 PTAC, a collaboration between the Accreditation Council for Pharmacy Education (ACPE) and ASHP, will be responsible for the joint approval of pharmacy technician education/training programs starting in late 2014. This collaboration combines ACPE’s expertise and credibility in accrediting professional pharmacy degree programs with ASHP’s strengths in accrediting pharmacy technician education/training and pharmacy residency programs.19 This collaboration will continue to ensure the quality and standardization of the education/training programs for pharmacy technicians.
Pharmacy Technician Certification
Certification is the voluntary process by which a nongovernmental agency or association grants recognition to an individual who has met certain predetermined qualifications specified by that agency or association.3 There are many benefits to certification including validation of achievement and knowledge, improved employment opportunities, and career growth. Certified pharmacy technician (CPhT) is the only national credential available to pharmacy technicians.
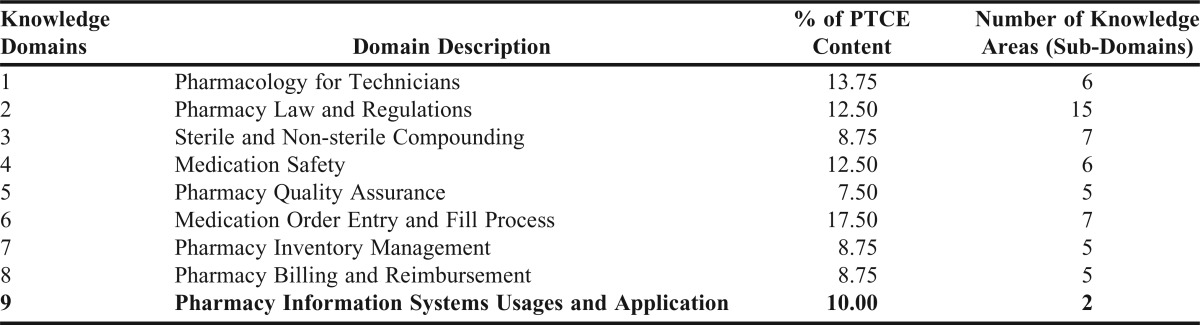
PTCB, founded in 1995, administers the Pharmacy Technician Certification Exam (PTCE). More than 500,000 technicians have been certified by PTCB since 1995.20 The PTCE is accredited by the National Commission for Certifying Agencies (NCCA). PTCB consistently works to improve the certification process for pharmacy technicians. Consistent with industry best practices and accreditation standards, PTCB conducts a regular Job Analysis Study as the foundation for its national certification program.11,21 In 2012, the PTCB conducted the most recent Job Analysis Study, whose purpose was to analyze the requirements of the pharmacy technician occupation and to use the resulting information to develop a new test blueprint (test content outline) for the PTCE.20 A total of 25,712 pharmacy technicians from every state and practice setting participated in the 2012 Job Analysis Study.22 The updated PTCE, which was implemented November 2013, more strongly emphasizes certain knowledge areas, including medication safety and pharmacy information systems.22 The updated PTCE contains more specific knowledge groupings or “domains,” each with sub-domains.22 Appendix B contains the updated PTCE domains.23
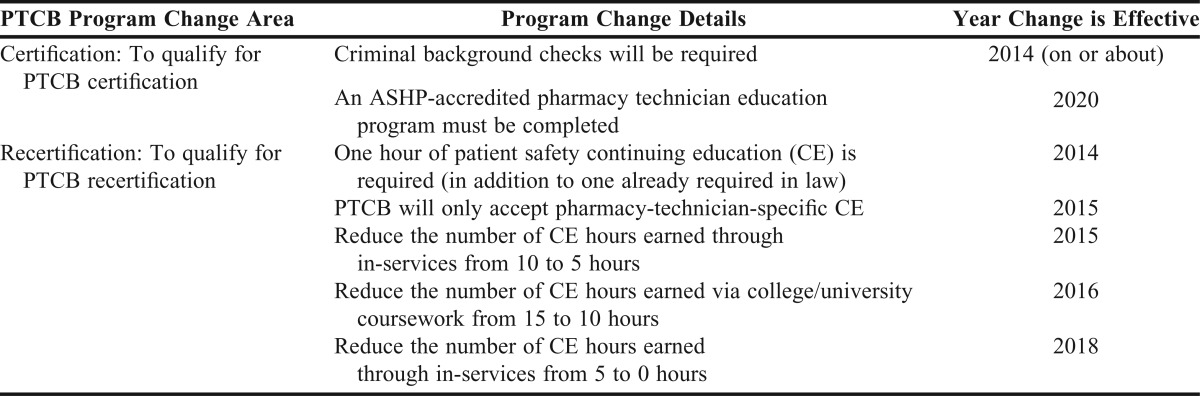
PTCB has announced future changes to its certification program to advance pharmacy technician qualifications by elevating PTCB’s standards for national certification and recertification.24 One of the future changes, starting in 2020, is that PTCB candidates will be required to complete an ASHP-accredited pharmacy technician education/training program. This change enables standardized training, pursuant to ASHP standards, to precede certification—the same process utilized for student pharmacists to become licensed pharmacists. Table 3 lists the PTCB program changes which will be phased in over the next seven years.
Table 3.
Future Changes to the Pharmacy Technician Certification Board (PTCB) Certification Program24
The Pharmacy Technician Certification Program,25 founded in 2005, is administered by the National Health career Association. The Pharmacy Technician Certification Program administers the ExCPT examination,25 and as of August 2009, 5,100 individuals were certified via the ExCPT examination.7 The ExCPT examination is a psychometrically sound exam and is based on a national job task analysis conducted on a regular basis, most recently in 2010.3 The ExCPT content outline is comprised of three domains: (1) regulation and technician duties; (2) drugs and drug products; and (3) the dispensing process.5 The Pharmacy Technician Certification Program is accredited by the National Commission for Certifying Agencies (NCCA).
The Regulation of Pharmacy Technicians
State boards of pharmacy regulate the practice and work activities of pharmacy technicians. While regulatory approaches differ substantially among the states, virtually all state boards of pharmacy have amended their pharmacy practice acts and regulations in recent years, allowing an expanded role for pharmacy technicians in the delivery of pharmacy services.3,5 According to the 2013 Survey of Pharmacy Law of the National Association of Boards of Pharmacy (NABP), over 80% of the state boards of pharmacy in the US and US territories license, register or certify pharmacy technicians, and at least two states are currently working on legislation in this area.26 Currently, over one-third of jurisdictions have continuing education requirements that pharmacy technicians must meet in order to maintain their license, certification or registration.26
Not all states have education, training and certification requirements for pharmacy technicians. Some states require board of pharmacy approval of pharmacy technician education/training programs.26 On-the-job training or a job-specific utilization plan for technicians is accepted in lieu of more formalized training in some states.7,26 There is also state-by-state variation in the types of examinations and continuing education that are required for granting and/or maintaining pharmacy technician registration. Therefore, standardized pharmacy technician education, training and certification are not uniformly required. The 2010 NABP Task Force on Pharmacy Technician Education and Training Programs recommended that state boards of pharmacy license or register pharmacy technicians, accept PTCB certification, report pharmacy technician disciplinary information to a central clearing-house and require pharmacy technician education/training that meets standardized guidelines.27 In addition, the task force recommended that by 2015, state boards of pharmacy require pharmacy technicians to have completed an accredited education/training program as a condition of certification.27 Further changes in the regulation of pharmacy technicians will continue as the practice of pharmacy continues to evolve and new patient care models emerge.
The education, training, and certification of pharmacy technicians as well as the accreditation of pharmacy technician education/training programs have progressed greatly, yet there continues to be a lack of consistency and standardization of these elements due to many issues and influencing factors. There is a need to establish national standards for the education, training and certification of pharmacy technicians to provide the optimal deployment of the pharmacy workforce to meet the health care demands and delivery of quality health care services to the public.28 The pharmacy profession has an obligation to ensure that pharmacy technicians are subject to rigorous standards—standards that are required of pharmacists and other health care professionals in order to provide the highest quality health care to improve patient outcomes and protect the public’s health.
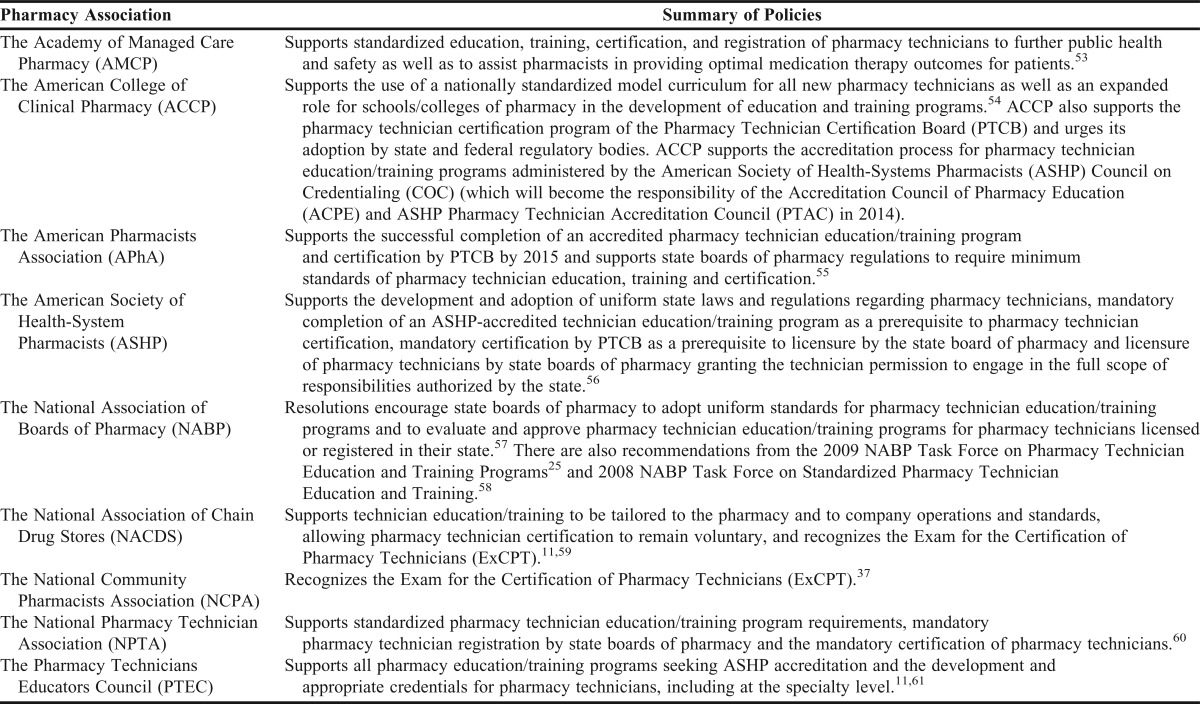
Several national pharmacy organizations have policies or guidelines regarding pharmacy technician education, training, and certification, as well as program accreditation (Table 4). AACP has the current policies pertaining to pharmacy technicians:29
• AACP supports the inclusion of outcomes related to pharmacist supervision and management of pharmacy technicians in the professional degree program, as well as process analysis skills necessary to optimally integrate pharmacy technicians into pharmacy workflow and services. These outcomes should be addressed in the didactic and experiential components of the curriculum. (Source: Bylaws and Policy Development Committee, 2011 in an amendment to the original policy statement from the Professional Affairs Committee, 1990)
• AACP supports the creation of partnerships with other national pharmacy organizations to develop a framework to ensure an educated, trained, and certified pharmacy technician workforce to enable pharmacists to provide medication therapy management and other patient care services. (Source: Professional Affairs Committee, 2011)
• AACP supports training and education for pharmacy technicians that include outcomes deemed appropriate by the profession and that are based on sound educational principles. (Source: Bylaws and Policy Development Committee, 2011 in an amendment to the original policy statement from the Professional Affairs Committee, 1990).
• AACP supports innovative relationships between colleges and schools of pharmacy and pharmacy technician education programs that enhance the quality of the respective educational programs offered by each. (Source: Bylaws and Policy Development Committee, 2011 in an amendment to the original policy statement from the Professional Affairs Committee, 1990).
The 2002 AACP Argus Commission Report expressed the need for pharmacy education to be involved with pharmacy technician education/training programs.30 In fact, this report had a recommendation to determine the extent of the collaboration that exists between schools/colleges of pharmacy and pharmacy technician education/training programs and to develop strategies to facilitate these collaborations—items that will be discussed in this report. The need for pharmacy education and pharmacy technician education/training programs to work together is still evident today. Achieving effective and enhanced models for pharmacy services in all practice settings will depend on the full utilization of pharmacists’ professional knowledge and contact with patients and other health care providers. Enabling pharmacists to “redistribute” their focus to more clinical and patient-centered activities will only be possible if pharmacy technicians are adequately educated, trained and qualified to handle medication distribution and other related tasks. Pharmacy technicians play key roles in many aspects of today’s medication-use system. Having a workforce of technicians with proper knowledge and training is integral as the pharmacy profession looks to change the pharmacy practice model and enable pharmacists to provide the best possible care to patients.
Table 4.
Summary of Technician Education, Training, Certification and Accreditation Policy Statements of National Pharmacy Associations
Charge 2: Identify potential role(s) of pharmacy academic institutions and pharmacy faculty in the education, training, and certification of pharmacy technicians
A review of the literature was conducted to assist in the identification of emerging and existing successful collaborative practices between schools/colleges of pharmacy and pharmacy institutions/organizations involved in the education, training, and certification of pharmacy technicians. Very few articles describing partnerships/collaborations between academic pharmacy and technician education/training programs were found. Further, those existing articles tend to focus on schools/colleges of pharmacy collaborations with health care institutions and community pharmacies to improve pharmacy services (e.g., medication reconciliation, asthma education, smoking cessation, prescription error reduction, tele-pharmacy, drive-through pharmacy)31, 32, 33, 34, 35, 36, 37 , importance of pharmacy technician credentialing for successful pharmacy services38, pharmacy technician roles to enhance pharmacy clinical and operational capabilities39, 40, 41, versus collaborations with pharmacy technician programs42, 43 or pharmacy technician-to-student pharmacist pathway programs.44, 45
In order to gather more information to address their second charge, the PAC chose to investigate the current relationships and successful practices between schools/colleges of pharmacy and institutions engaged in pharmacy technician education. The PAC initially created an online inquiry that was distributed to pharmacy practice chairs (PPCs) of schools/colleges of pharmacy and directors of pharmacy technician education/training programs. The inquiry requested the name of the school/college of pharmacy or pharmacy technician education/training program and the accreditation status of the pharmacy technician education/training program. If a collaboration existed the respondent was asked to describe the collaboration, why the entities felt that the collaboration was considered important and valuable, what (if any) financial arrangements/incentives were in place to support the collaboration, key factor(s) associated with the success of the collaboration, and barriers encountered in the development/maintenance of the collaboration. Those respondents who were not part of a collaboration were asked about issues prohibiting the creation of a collaboration. All respondents were asked about collaborations that would be considered a “best practice” between a school/college of pharmacy and a pharmacy technician education/training program. Several examples of potential collaborative activities were included to assist the respondent in completing the survey. The inquiry was distributed in early October 2013 and was available for two weeks. A reminder was sent to the groups one week after the initiation of the online inquiry.
There were 54 responses from the colleges/schools of pharmacy inquiry and 95 responses from the pharmacy technician education/training program directors/coordinators’ inquiry representing all eight of the AACP/NABP districts.46 The most frequently cited program collaborations included pharmacy technician student education, student pharmacists and technician student co-curricular activities, student pharmacist pipeline programs, advisory board/council membership, and student pharmacists serving as laboratory assistants. Of particular note, 28 (52%) of the PPCs expressed a lack of interest in these types of relationships stating that they were neither a priority, important, of interest to, mission-consistent, or financially advantageous for their programs. Only four (4%) of respondents from pharmacy technician education/training programs expressed this viewpoint.
Summary of Initial Inquiry to Pharmacy Practice Chairs and Pharmacy Technician Education/Training Program Directors/Coordinators
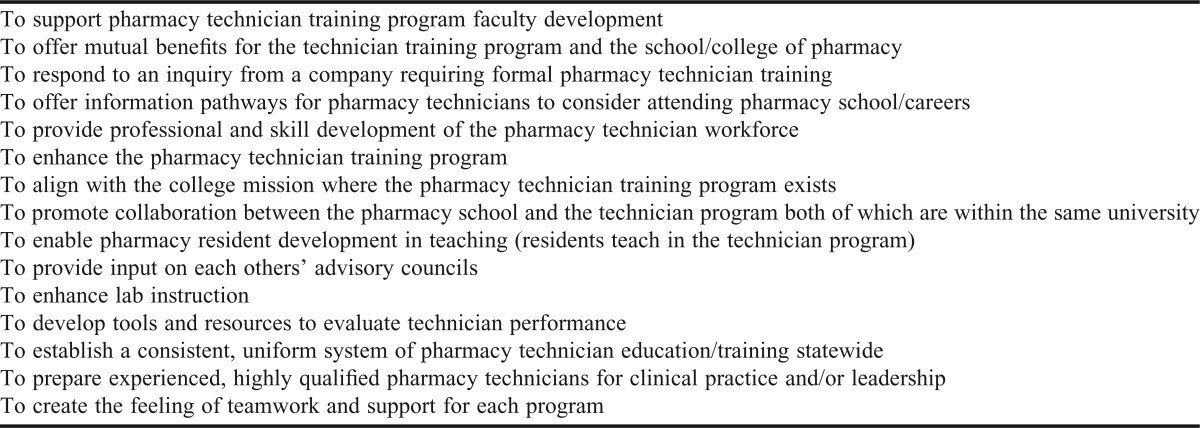
The initial question asked respondents to state why their school/college of pharmacy or pharmacy technician education/training program developed a relationship/collaboration considered to be important and valuable. Pharmacy Practice Chairs (PPCs) responses focused on the mutually beneficial nature of the collaboration while pharmacy technician education/training program directors/coordinators described pharmacy technician pathways to pharmacy school/careers in pharmacy as the primary reason. They also included statements pertaining to the enhancement of the training program and technician skill development as reasons in addition to providing teaching opportunities for residents. Reasons submitted for schools/colleges of pharmacy and pharmacy technician programs to develop a collaborative relationship are included in Table 5.
Table 5.
Reasons for schools/colleges of pharmacy and pharmacy technician training programs to develop a collaborative relationship (provided by the PAC initial inquiry to schools/colleges of pharmacy and pharmacy technician education/training programs)
When respondents were asked to state the key factor(s) for their successful relationship/collaboration, both sets of respondents cited open communication as important. Additional responses included the importance of physical location proximity, involvement of faculty and administration, student pharmacist involvement, and faculty having a previous relationship with the technician program either as an instructor or alumnus.
A question focused on the barriers encountered in developing/maintaining the relationship/collaboration resulted in similar answers indicating the issues of the lack of available time, finances/cost, administrative turnover, communication difficulties, and persuading administration on the value of the collaboration. Of note, one pharmacy practice chair and three pharmacy technician program respondents stated that they experienced no barriers.
When asked about the issues that have prohibited their school/college of pharmacy and pharmacy technician education/training program from developing a relationship/collaboration, both sets of respondents provided a variety albeit very similar reasons. Several respondents cited that collaborations of this type have not been a priority, nor of interest or perceived value. Additional reasons included lack of physical proximity to either program, lack of time and resources, curricular scheduling inconsistencies, competition for experiential sites, no mandate for continued ACPE accreditation, potential for technician training program competition, and lack of incentive to do so.
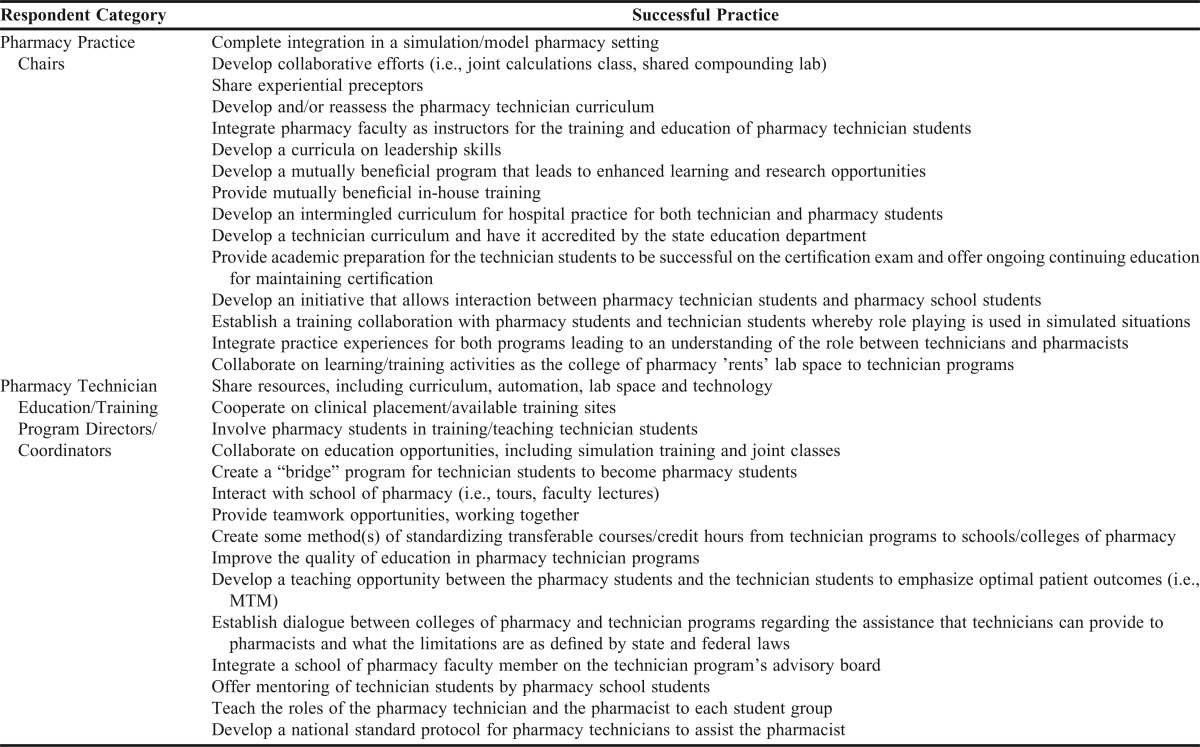
A question was posed which asked the respondents for examples of collaborative best practices that they were aware of between a school/college of pharmacy and pharmacy technician education/training program. PPCs submitted examples including pharmacy technician education/training delivered by student pharmacists and overseen by pharmacy faculty for technicians not able to attend formal education programs. In addition, collaboration to enhance the strengthening of high school science education for pipeline development was mentioned. Pharmacy technician education/training program directors/coordinators submitted many more examples to include supporting pharmacy technician student matriculation into schools/colleges of pharmacy, classes including both pharmacy school and pharmacy technician students, developing curriculum to teach both types of students their roles in new health care delivery models, sterile and chemotherapy compounding training enhancement, faculty from both types of programs serving on advisory boards/councils, student pharmacists mentoring pharmacy technician students, and teaching opportunities for student pharmacists.
In contrast to an awareness of a best practice, an additional question inquired as to what the respondent considered a “best practice” could be between a school/college of pharmacy. Many responses to this question were received from PPCs and pharmacy technician training program directors/coordinators alike. A compilation of these responses is included in Appendix C.
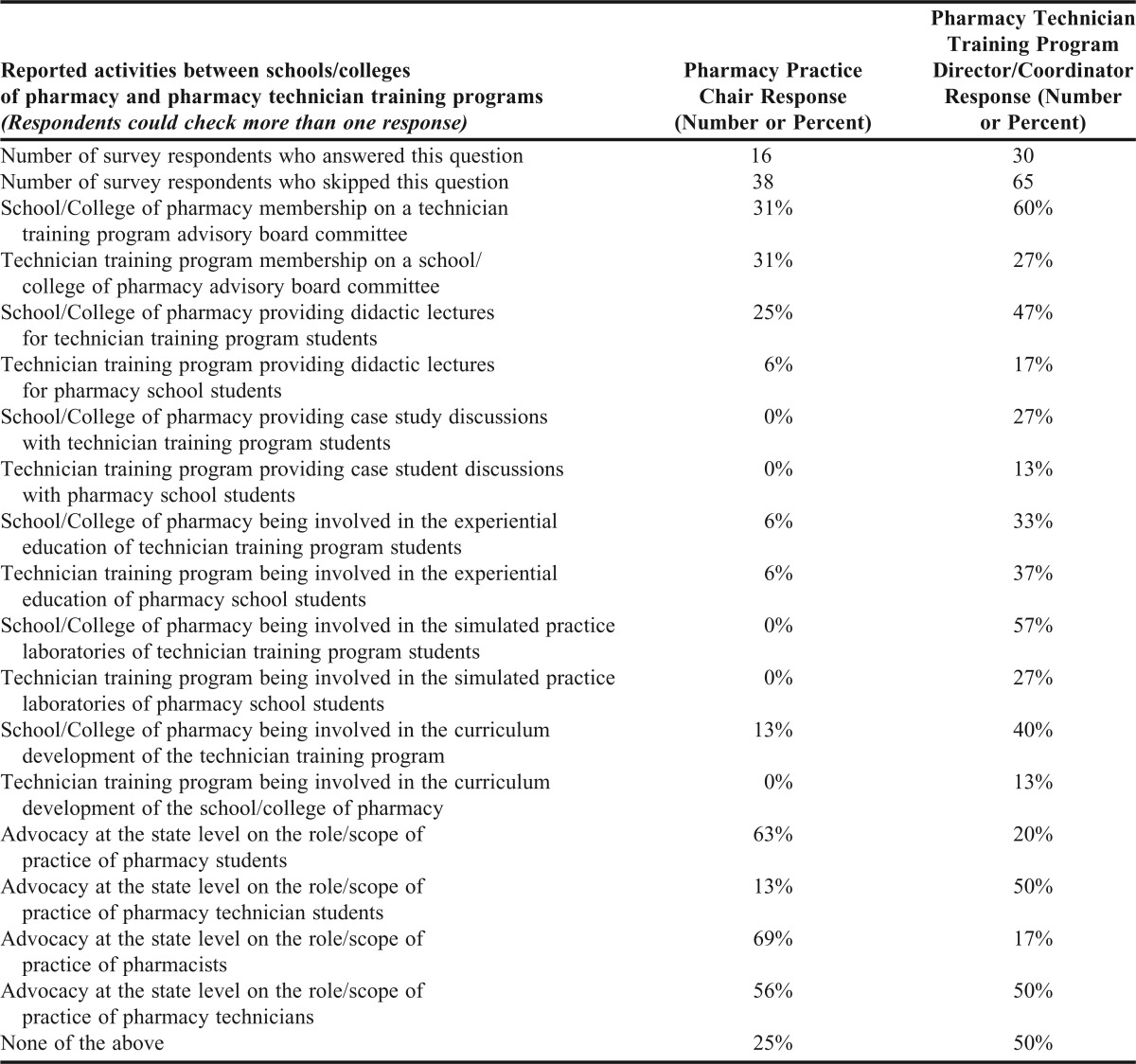
The last section of the inquiry provided an opportunity for the respondents to report any activities they were aware of between their school/college of pharmacy and a pharmacy technician education/training program (and vice-versa). One of the most surprising results from this final question was that 38 of the 54 (70%) PPCs and 65 of the 95 (68%) of the Pharmacy Technician Education/Training Program Directors/Coordinators did not answer this question. Reported activities from this inquiry are included in Table 6.
Table 6.
Reported Activities from the Initial Inquiry to Pharmacy Practice Chairs and Pharmacy Technician Education/Training Program Directors/Coordinators regarding Collaborations between schools/colleges of pharmacy and pharmacy technician education/training programs
Results from the initial inquiry were discussed during the in-person meeting of the PAC in October 2013, which served as the basis for the development of a more detailed inquiry to identify specific successful collaborative practices across the academy. A secondary online inquiry was developed requesting the name of the school/college of pharmacy and pharmacy technician education/training program, a brief description about the collaborative relationship between the two entities, whether the collaboration was emerging or existing (on-going), and why the collaboration would be classified as successful between the entities. Nineteen respondents submitted collaboration descriptions, of which 14 were described as existing and 5 as emerging activities. An invitation was made to those respondents to provide more detailed information about the collaboration including outcomes, critical need(s) being addressed, successful aspect(s), challenges to formation/implementation, stakeholder(s) acceptance/considerations and advice or lessons learned. These detailed descriptions can be found on the AACP website.47
Ten institutional partnerships submitted responses from the invitation to provide more detailed information regarding their collaboration. The submitted collaborative activities were categorized into seven broader focus areas, which included involvement in: advisory councils; advocacy initiatives (including legislative); education/curriculum; experiential education; school/college matriculation agreements; patient care/workforce enhancement; and research (Table 7).
Table 7.
Description of collaborations between schools/colleges of pharmacy and pharmacy technician/education training programs (Information from the PAC Call for Successful Practices to schools/colleges of pharmacy and pharmacy technician/education training programs)
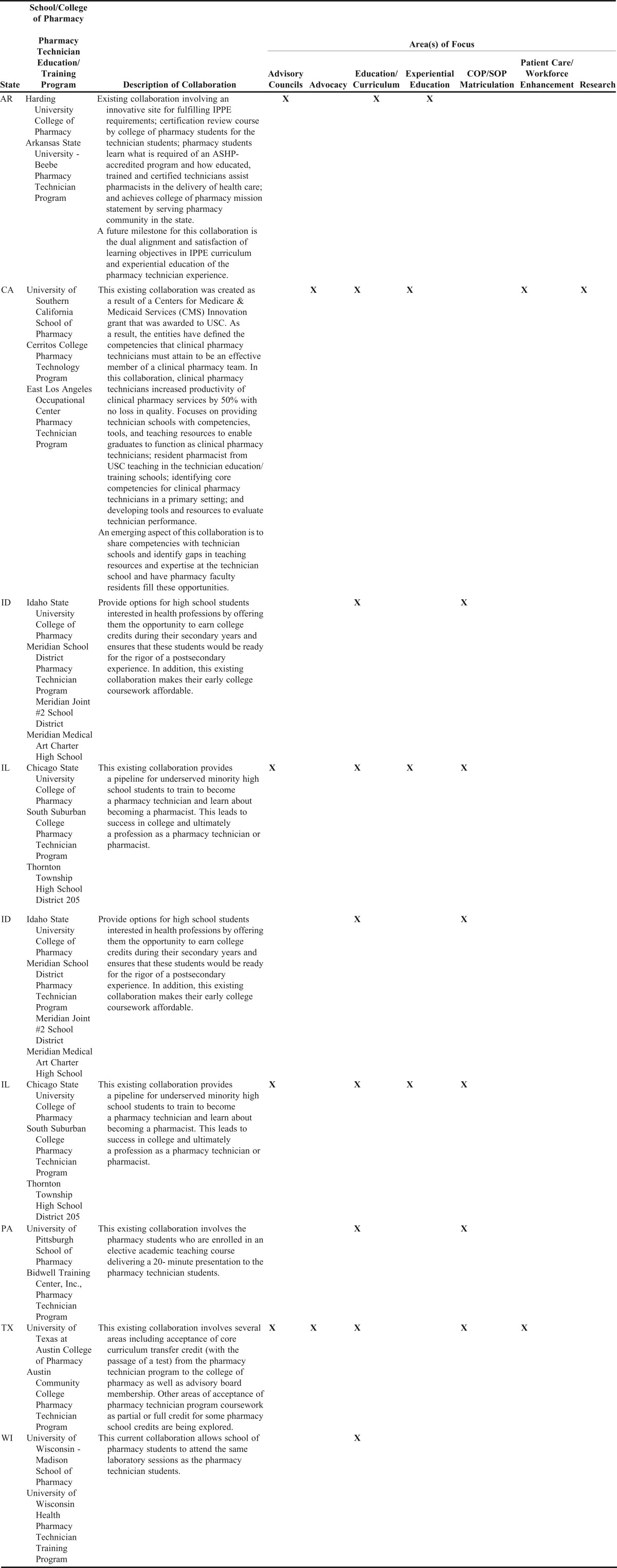
Advisory Council Participation Collaborations
Faculty of schools/colleges of pharmacy serve as members of advisory councils for pharmacy technician education/training programs as do technician educators for advisory boards/councils at school/colleges of pharmacy. Some of these relationships are outgrowths of academic pharmacy faculty having previously served as pharmacy technician program directors and/or faculty. Faculty members assist with program accreditation, professional presentations, and related endeavors. In addition, academic pharmacy faculty help program directors to ensure that their curriculums include/incorporate current pharmacy practice models and services.
Advocacy Initiatives Collaborations
Academic pharmacy faculty engage in advocacy initiatives involving state boards of higher education and legislatures on behalf of improving pharmacy technician education and regulation of technician activities. In addition to supporting the strengthening of pharmacy technician licensure and certification requirements, faculty members are also engaged in health care-related demonstration projects involving pharmacy technicians to influence scope of practice and payment model initiatives.
SOP/COP Matriculation Collaborations
School/Colleges of pharmacy have developed articulation agreements leading to pharmacy technician students matriculation into pharmacy programs. These initiatives include science/math proficiency strengthening, “bridge program” development, recognition of technician program coursework/laboratory completion to satisfy pharmacy school course/laboratory requirements upon admission, guaranteed interview/admission programs, and other initiatives to strengthen future student pharmacist application pools and application pathways.
Education and Curricular Development/Delivery Collaborations
Pharmacy faculty and student pharmacists serve as instructors for technician education/training programs and certification preparation in addition to leading efforts to strengthen technician education/training program accreditation efforts. Student pharmacists and pharmacy technician students are enrolled in “team building” combined courses to simulate pharmacy practice environments. Pharmacy technician programs utilize sterile compounding laboratories at schools/colleges of pharmacy during downtimes, and the reverse also occurs. Student pharmacists teach in technician education/training laboratories and in certification preparation courses. Faculty members also serve as compounding laboratory instructors for both the school/college of pharmacy and pharmacy technician program. Student pharmacists also have employment opportunities as program instructors in technician education/training programs.
Experiential Education (IPPE/APPE) Collaborations
Student pharmacists complete elective experiential rotation courses at pharmacy technician program institutions (didactic and laboratory focus). Student pharmacists are engaged in didactic and laboratory teaching, assessments, and related activities to expose them to educational pedagogy as well as leadership development opportunities.
Patient Care/Workforce Development/Enhancement Collaborations
Academic pharmacy has worked with health care institutions to improve the quality and comprehensiveness of pharmacy technician education/training to achieve institutional and patient care quality measures. These partnerships have been created to prepare experienced, highly-qualified pharmacy technicians for advanced clinical practice and/or leadership roles within health care organizations. Both pharmacy faculty and residents have engaged in these programs and activities.
Research-Related Collaborations
Academic pharmacy has also been engaged in education and patient care-focused research partnerships designed to demonstrate the impact of patient-centered care initiatives provided by pharmacists. These research endeavors have potential impact not only on workforce development enhancement but help to expand scope of practice and pharmacy services reimbursement/payment model.
Charge 3: Recommend strategies to develop collaborations/relationships between schools/colleges of pharmacy and pharmacy technician education/training programs to advance pharmacy practice in the evolving health care system.
As well-described in the Charges 1 and 2, momentum is building to promote quality pharmacy technician education/training programs, and there are many potential roles by which schools/colleges of pharmacy and faculty can invest in such programs. While the reported existing and emerging notable practices serve to provide ideas for collaborations, the PAC suggests several key strategies for future efforts.
1. Work through consortia. In many states and regions, there are existing consortia which provide venues to work through common initiatives and issues in pharmacy.48 Some are focused on experiential education, and others are broader and include schools, pharmacy stakeholders, boards of pharmacy, and others who are working to advance pharmacy practice. AACP-NABP district meetings, which are held annually, could serve as another venue. An ongoing agenda item for pharmacy technician education/training in these meetings should enable productive discussions and action items which are enacted locally.
2. Plan strategically. Just as missions guide the commitments of schools/colleges of pharmacy, missions for pharmacy technician education/training programs may align with existing educational or practice advancement foci. Even when a state institution seeks to work with a private or for-profit pharmacy technician program, specific goals and objectives may support a new collaboration or enhance an existing one.
3. Assure true partnership. Some of the existing collaborations are sustained by a champion in the school/college of pharmacy and another in the pharmacy technician program. When personnel transitions occur, the collaboration is put at risk. These joint ventures will be more sustainable when guided by multiple parties at the partner institutions. Not only can the workload be shared, but broader input may generate quality improvements or strategic initiatives, which provide benefit to both or all partners.
4. Make it official. Some of the collaborations state that they do not have formalized memoranda of understanding or affiliation agreements. Such legal documents should protect the partners from potential misunderstandings and will establish commitments. For example, a school/college of pharmacy may provide access to the pharmacy practice laboratory for pharmacy technician training. Such in-kind support should be specifically detailed. The collaborative partners should review memoranda or affiliation agreements at least annually, especially during the formative stage of development.
5. Learn nationally; focus locally. Many national initiatives serve to guide formation of partnerships around the standards of quality and safety. Examples include Pharmacy Practice Model Initiative (PPMI)49 , Center for Pharmacy Practice Accreditation (CPPA)50, and the Institute for Safe Medication Practices (ISMP).51 Shared goals between schools/colleges of pharmacy and pharmacy technician education/training programs need to be examined in the local context of state scopes of practice and regulatory oversight of pharmacy practice.
POLICY STATEMENTS, RECOMMENDATIONS AND SUGGESTIONS
Policy Statements
AACP supports the completion of an American Society of Health-System Pharmacists (ASHP) accredited pharmacy technician education/training program, certification by the Pharmacy Technician Certification Board (PTCB), and registration by state boards of pharmacy for pharmacy technicians.
(Potential replacement of the current AACP policy: AACP supports training and education for pharmacy technicians that include outcomes deemed appropriate by the profession and that are based on sound educational principles.)
The following amended policy statement was adopted by the AACP House of Delegates on July 30, 2014: AACP supports the completion by pharmacy technicians of an accredited pharmacy technician education/training program, certification by an accredited certification agency, and registration by state boards of pharmacy.
The following policy statement was adopted by the AACP House of Delegates on July 30, 2014: AACP encourages schools/colleges of pharmacy to collaborate with pharmacy technician education/training programs in an area(s) of potential interest and enhancement for both entities.
Recommendations
AACP should strengthen and develop new avenues of collaboration with national organizations responsible for the education, training and accreditation of pharmacy technicians.
AACP should develop an Institute on the topic of collaborations between schools/colleges of pharmacy and pharmacy technician education/training programs to enable partners to create or further develop such partnerships.
Suggestion
Schools and colleges of pharmacy should consider areas of collaborations with pharmacy technician education/training programs.
A CALL TO ACTION
As described under Charge 1, the ability for pharmacists to successfully fulfill patient care provider roles depends on how well pharmacy technicians are prepared to function in their roles as pharmacy supportive personnel. The profession cannot successfully advance without it. The recent upward trend in the number of pharmacists and the expansion of the certified pharmacy technician workforce provide assurance about the capacity of this medication-oriented workforce to take on new roles.28 The pharmacy academy may need to have a better recognition of the value that pharmacy technicians bring to the profession. It can no longer continue to sit on the “sidelines” but should make it a priority to become involved in national, state, and local discussions and endeavors focused on formalized education, training, and certification of all pharmacy technicians. Academic pharmacy needs a greater level of involvement to help ensure that all professionals who will be engaged in these efforts are qualified to do so. Becoming involved in activities that will make a difference for the profession is a responsibility of all organizations whose missions focus on advancing pharmacist-provided patient care.
To achieve this level of involvement, schools/colleges of pharmacy should give increased consideration to forming effective collaborations with institutions/organizations focused on the education, training, and certification of pharmacy technicians. The above inquiries have provided evidence that some schools/colleges of pharmacy and pharmacy technician programs have developed and are developing several areas of collaboration to advance pharmacy practice in the evolving health care environment. However, many schools/colleges of pharmacy and pharmacy technician education/training programs have not given much thought to the value of these types of partnerships nor have encouraged these partnerships. Schools/colleges of pharmacy and pharmacy technician educators have many potential avenues to explore as health care and pharmacy education continues to advance.
As an example, student pharmacist involvement in teaching laboratory skills for pharmacy technician students may help to provide co-curriculum experiences consistent with Standard 14 of the ACPE Draft Accreditation Standards 2016.52 Through these partnerships, the key issues can be addressed collectively and more effectively than if addressed in silos. All pharmacy organizations should consider working together to achieve these goals and play a role in advancing the profession together.
Appendix A. Glossary of Terms3
Accreditation: The process whereby an association or agency grants public recognition to an organization, site, or program that meets certain established qualifications or standards, as determined through initial and periodic evaluations.
Certificate: A document issued upon successful completion of the pre-determined level of performance of a certificate program or of a pharmacy residency or fellowship.
Certification: The voluntary process by which a nongovernmental agency or an association grants recognition to an individual who has met certain predetermined qualifications specified by that organization. This formal recognition is granted to designate to the public that this person has attained the requisite level of knowledge, skill, and/or experience in a well-defined, often specialized, area of the total discipline. Certification usually requires initial assessment and periodic reassessments of the individual’s knowledge, skill, and/or experience.
Certified: An adjective used to describe an individual who holds certification that is incorporated into the name of the credential awarded that person. For example, a pharmacy technician who has passed as national certification examination is a CPhT.
Competence: The ability of the individual to perform his/her duties accurately, make correct judgments, and interact appropriately with patients and colleagues. Professional competence is characterized by good problem-solving and decision-making abilities, a strong knowledge base, and the ability to apply knowledge and experience to diverse patient care situations.
Continuing education (CE): for the pharmacy profession is a structured educational activity designed or intended to support the continuing development of pharmacists and/or pharmacy technicians to maintain and enhance their competence.
Credential: Documented evidence of professional qualifications. Examples of credentials include academic degrees, certification and state licensure.
Credentialing: (1) The process of granting a credential and (2) the process by which an organization or institution obtains, verifies, and assesses an individual’s qualifications to provide patient care services.
License: A credential issued by a state or federal body indicating that the holder is in compliance with the minimum mandatory governmental requirements necessary to practice in a particular profession or occupation.
Pharmacy Technician: An individual who, under the supervision of a licensed pharmacist, assists in pharmacy activities not requiring the professional judgment of the pharmacist.
Registered: Adjective used to describe a pharmacist or pharmacy technician who has met state requirements for licensure and whose name has been entered on a state registry of practitioners who are licensed to practice in that jurisdiction.
Appendix B.
Pharmacy Technician Certification Exam (PTCE) Domains21
Appendix C.
Pharmacy Practice Chairs and Pharmacy Technician Education/Training Program Director/Coordinator Best Practices (generated from the PAC Initial Inquiry to Schools/Colleges of Pharmacy and Pharmacy Technician Education/training Programs)
References
- 1.Piascik P. The Relentless Pursuit of Excellence in Pharmacy Education. American Journal of Pharmaceutical Education. Volume 77 Issue 7, Article 139. [Google Scholar]
- 2.Joint Commission of Pharmacy Practitioners (JCPP) Vision. http://www.amcp.org/Tertiary.aspx?id=8463. Accessed April 7, 2014. [DOI] [PubMed]
- 3.Credentialing in Pharmacy: A Resource Paper (2010) Council on Credentialing in Pharmacy (CCP) Resource Documents. http://www.pharmacycredentialing.org. Accessed April 7, 2014.
- 4.Bureau of Labor Statistics. U.S. Department of Labor, Occupational Outlook Handbook, 2012-13 Edition, Pharmacy Technicians. http://www.bls.gov/ooh/Healthcare/Pharmacy-technicians.htm. Accessed April 7, 2014.
- 5.Council on Credentialing in Pharmacy. Scope of Contemporary Pharmacy Practice: Roles, Responsibilities, and Functions of Pharmacists and Pharmacy Technicians. http://www.pharmacycredentialing.org. Accessed April 7, 2014.
- 6.McAllister EB. Pharmacy Technicians: Roles in Evolving Care Delivery Models—Current and Future Issues & Visions. Presentation at the November 7, 2013 Joint Commission of Pharmacy Practitioners (JCPP) meeting.
- 7.Myers CE. Opportunities and challenges related to pharmacy technicians in supporting optimal pharmacy practice models in health systems. Am J Health-Syst Pharm. 2011;68:1128–36. doi: 10.2146/ajhp110056. [DOI] [PubMed] [Google Scholar]
- 8.Pharmacy Technician Schools in Canada. http://www.healthcarepathway.com/pharmacy/pharmacy-technician-canada.html. Accessed April 7, 2014.
- 9.Entry requirements and training for pharmacy technicians. http://www.nhscareers.nhs.uk/explore-by-career/pharmacy/pharmacy-technician/entry-requirements-and-training. Accessed April 7, 2014.
- 10.Liles JM. State of Pharmacy Technician Education. Presentation at the November 7, 2013 Joint Commission of Pharmacy Practitioners (JCPP) meeting.
- 11.White paper on pharmacy technicians 2002: Needed changes can no longer wait. Am J Health-Syst Pharm. 2003;60:37–51. doi: 10.1093/ajhp/60.1.37. [DOI] [PubMed] [Google Scholar]
- 12.ASHP Technician Training Directory. http://www.ashp.org/menu/Accreditation/TechnicianTrainingDirectory.aspx. Accessed April 7, 2014.
- 13.American Society of Health-System Pharmacists (ASHP) > 30 years of Pharmacy Technician Accreditation presentation. August 20, 2013 Council on Credentialing Meeting. [Google Scholar]
- 14.Council on Credentialing in Pharmacy. Council on Credentialing in Pharmacy: Pharmacy Technician Credentialing Framework. http://www.pharmacycredentialing.org. Accessed April 7, 2014.
- 15.Pharmacy Technician Accreditation: Accreditation Standard for Pharmacy Technician Training Programs-NEW January 2014. http://www.ashp.org/menu/Accreditation/TechnicianAccreditation. Accessed April 7, 2014.
- 16.Pharmacy Technician Accreditation: Guidance Document-New Standard. http://www.ashp.org/menu/Accreditation/TechnicianAccreditation. Accessed April 7, 2014.
- 17.Pharmacy Technician Accreditation: Model Curriculum for Pharmacy Technician Education and Training Programs-New Standard. http://www.ashp.org/menu/Accreditation/TechnicianAccreditation. Accessed April 7, 2014.
- 18.Pharmacy Technician Accreditation: Pharmacy Technician Accreditation Commission (PTAC)-New Pharmacy Technician Accreditation Commission Launched. http://www.ashp.org/menu/Accreditation/TechnicianAccreditation. Accessed April 7, 2014.
- 19.Abramowitz PW. PTAC: A New Collaboration to Expand Pharmacy Technician Education Training. http://www.ashpintersections.org/2013/11/pharmacy-technician-accreditation-commission-a-new-collaboration-to-expand-pharmacy-technician-education-and-training/. Accessed April 7, 2014.
- 20.PTCB: Become a PTCB CPhT. http://www.ptcb.org/get-certified#.UrKFK4eA2M8. Accessed April 7, 2014.
- 21.PTCB: Job Analysis Study. http://www.ptcb.org/get-certified/prepare/job-analysis#.UrP9bYeA2M8. Accessed April 7, 2014.
- 22.PTCB: PTCB To Introduce Updated Certification Exam on November 1. http://www.ptcb.org/about-ptcb/news-room/news-landing/2013/08/27/updatedPTCErelease#.UrQA14eA2M9. Accessed April 7, 2014.
- 23.PTCB: Important Updates to the PTCE. http://www.ptcb.org/get-certified/prepare/important-changes#.UrQB6IeA2M9. Accessed April 7, 2014.
- 24.PTCB Certification Program Changes. http://www.ptcb.org/about-ptcb/crest-initiative#.UrKKS4eA2M8. Accessed April 7, 2014.
- 25.ExCPT Pharmacy Technician Certification: Pharmacy Technician Certification (CPhT) http://www.nhanow.com/pharmacy-technician.aspx. Accessed April 7, 2014.
- 26.National Association of Boards of Pharmacy. 2013 Survey of Pharmacy Law: Licensing Law Section-Status of Pharmacy Technicians. 2012 [Google Scholar]
- 27.NABP: 2009-2010 Report of the Task Force on Pharmacy Technician Education and Training Programs Released. http://www.nabp.net/news/2009-2010-report-of-the-task-force-on-pharmacy-technician-education-and-training-programs-released/. Accessed April 7, 2014.
- 28.Maine LL, Knapp KK, Scheckelhoff DJ. Pharmacists And Technicians Can Enhance Patient Care Even More Once National Policies, Practices, And Priorities Are Aligned. Health Affairs. doi: 10.1377/hlthaff.2013.0529. 32, no.11 (2013):1956–1962. [DOI] [PubMed] [Google Scholar]
- 29.AACP House of Delegates: Cumulative Policies, 1980-2012. http://www.aacp.org/governance/HOD/Pages/default.aspx. Accessed April 7, 2014.
- 30.Argus Commission Reports: Argus Commission Final Report 2001-02. http://www.aacp.org/governance/COMMITTEES/argUS/Pages/CommitteeReports.aspx. Accessed April 7, 2014.
- 31.Sen S, Siemianowski L, Murphy M, McAllister SC. Implementation of a pharmacy technician-centered medication reconciliation program at an urban teaching medical center. Am J Health Syst Pharm. 2014;71(1):51–6. doi: 10.2146/ajhp130073. [DOI] [PubMed] [Google Scholar]
- 32.Smith SB, Mango MD. Pharmacy-based medication reconciliation program utilizing pharmacists and technicians: a process improvement initiative. Hosp Pharm. 2013;48(2):112–9. doi: 10.1310/hpj4802-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry TM, Prosser TR, Wilson K, Castro M. Asthma friendly pharmacies: a model to improve communication and collaboration among pharmacists, patients, and healthcare providers. J Urban Health. 2011;1(88 Suppl):113–25. doi: 10.1007/s11524-010-9514-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zillich AJ, Aquilino ML, Farris KB. Knowledge and attitudes about smoking cessation among pharmacy technicians. J Am Pharm Assoc. 2004;44(5):578–82. doi: 10.1331/1544-3191.44.5.578.zillich. [DOI] [PubMed] [Google Scholar]
- 35.Odukoya OK, Stone JA, Chui MA. How do community pharmacies recover from e-prescription errors. Res Social Adm Pharm. 2013 doi: 10.1016/j.sapharm.2013.11.009. Dec 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lam AY, Rose D. Telepharmacy services in an urban community health clinic system. J Am Pharm Assoc. 2009;49(5):652–9. doi: 10.1331/JAPhA.2009.08128. [DOI] [PubMed] [Google Scholar]
- 37.Chui MA, Halton K, Peng JM. Exploring patient-pharmacist interaction differences between the drive-through and walk-in windows. J Am Pharm Assoc. 2009;49(3):427–31. doi: 10.1331/JAPhA.2009.07165. [DOI] [PubMed] [Google Scholar]
- 38.Keresztes JM. Education…A must in all levels of pharmacy practice. Ann Pharmacother. 2010;44(11):1826–8. doi: 10.1345/aph.1P393. [DOI] [PubMed] [Google Scholar]
- 39.Alkhateeb FM, Shields KM, Broedel-Zaugg K, Bryan A, Snell J. Credentialing of pharmacy technicians in the USA. Int J Pharm Pract. 2011;19(4):219–27. doi: 10.1111/j.2042-7174.2011.00095.x. [DOI] [PubMed] [Google Scholar]
- 40.Keresztes JM. Role of pharmacy technicians in the development of clinical pharmacy. Ann Pharmacother. 2006;40(11):2015–9. doi: 10.1345/aph.1G578. [DOI] [PubMed] [Google Scholar]
- 41.Doucette WR, Nevins JC, Gaither C, Kreling DH, Mott DA, Pedersen CA, Schommer JC. Organizational factors influencing pharmacy practice change. Res Social Adm Pharm. 2012;8(4):274–84. doi: 10.1016/j.sapharm.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Wick JY. Using pharmacy technicians to enhance clinical and operational capabilities. Consult Pharm. 2008;23(6):447–58. doi: 10.4140/tcp.n.2008.447. [DOI] [PubMed] [Google Scholar]
- 43.Hudgens J, Park T. Perceptions of pharmacy technicians and students regarding technicians as pharmacy instructors. Am J Pharm Educ. 2011;75(8):151. doi: 10.5688/ajpe758151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mack DR. The pharmacy technician’s role in pharmacy student education. Am J Pharm Educ. 2008;72(6):138. doi: 10.5688/aj7206138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Awé C, Bauman J. Theoretical and conceptual framework for a high school pathways to pharmacy Program. Am J Pharm Educ. 2010;74(8):Article 149. doi: 10.5688/aj7408149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.NABP District Composition. http://www.nabp.net/about/district-composition. Accessed April 7, 2014.
- 47.Successful Practices in Academic Pharmacy. http://www.aacp.org/resources/education/Pages/SuccessfulPracticesinPharmaceuticalEducation.aspx. Accessed April 7, 2014.
- 48.Report of the 2012-2013 Professional Affairs Committee: Tables of Influence—Is Pharmacy Hungry Enough? http://www.ajpe.org/doi/abs/10.5688/ajpe7710S21. Accessed April 7, 2014. [DOI] [PMC free article] [PubMed]
- 49.Pharmacy Practice Model Initiative (PPMI) http://www.ashpmedia.org/ppmi/. Accessed April 7, 2014.
- 50.Center for Pharmacy Practice Accreditation. http://pharmacypracticeaccredit.org. Accessed April 7, 2014.
- 51.Institute for Safe Medication Practices. https://www.ismp.org. Accessed April 7, 2014.
- 52.ACPE Standards Revision 2106. https://www.acpe-accredit.org/deans/StandardsRevision.asp. Accessed April 7, 2014.
- 53.Academy of Managed Care Pharmacy (AMCP) Policy Digest: Pharmacy Technicians in Support of Managed Care. http://amcp.org/WorkArea/DownloadAsset.aspx?id=15847. Accessed April 7, 2014.
- 54.American College of Clinical Pharmacy (ACCP) Position Statement. Pharmacy Technician Education, Training, and Certification. www.accp.com/docs/positions/positionStatements/Technician_Position_Statement.pdf. Accessed April 7, 2014.
- 55.American Pharmacists Association (APhA) Policy Manual: Pharmacy Technicians. http://www.pharmacist.com/policy-manual. Accessed April 7, 2014.
- 56.ASHP Policy Positions 1982-2013 (policies only): Policy 1216. http://www.ashp.org/Import/PRACTICEANDPOLICY/PolicyPositionsGuidelinesBestPractices/BrowsebyDocumentType/PolicyPositions.aspx. Accessed April 7, 2014.
- 57.NABP Technicians: NABP Task Force Reports and Resolutions. http://www.nabp.net/programs/cpe-monitor/cpe-monitor-service/technicians/#TFandRes. Accessed April 7, 2014.
- 58.NABP 2008-2009 Report of the Task Force on Standardized Pharmacy Technician Education and Training. http://www.nabp.net/news/2008-2009-report-of-the-task-force-on-standardized-pharmacy-technician-education-and-training/. Accessed April 7, 2014.
- 59.NCPA: Professional Development-Pharmacy Technician Training and Certification. https://www.ncpanet.org/index.php/ce-professional-development. Accessed April 7, 2014.
- 60.NPTA Strategic Vision. http://www.pharmacytechnician.org/en/cms/?490. Accessed April 7, 2014.
- 61.PTEC FAQ: What is PTEC? http://www.pharmacytecheducators.com/faq. Accessed April 7, 2014.


