Abstract
Purpose
The Accreditation Council for Graduate Medical Education (ACGME) states that “residents should participate in scholarly activity.” However, there is little guidance for effectively integrating scholarly activity into residency. This study was conducted to understand how pediatric residency programs are meeting ACGME requirements and to identify characteristics of successful programs.
Methods
The authors conducted an on-line cross-sectional survey of all pediatric residency program directors in October 2012, assessing program characteristics, resident participation in scholarly activity, program infrastructure, barriers, and outcomes. Multivariate logistic regression was used to identify characteristics of programs in the top quartile for resident scholarly activity participation.
Results
The response rate was 52.8% (105/199 programs). 78.6% (n=77) of programs required scholarly activity, although definitions were variable. When including only original research, systematic reviews or meta-analyses, and case reports or series with references, resident participation averaged 56% (range 0–100%). Characteristics associated with high participation programs included: 1) a scholarly activity requirement (odds ratio (OR) =5.5, 95% confidence interval (CI) 1.03–30.0); 2) program director belief that all residents should present work regionally or nationally (OR=4.7, 95% CI 1.5–15.1); and 3) mentorship by >25% of faculty (OR=3.6, CI 1.2–11.4). Only 47.1% (n=41) of program directors were satisfied with resident participation and only 30.7% (n=27) were satisfied with the quality of research training provided.
Conclusions
The results suggest resident scholarly activity experience is highly variable and suboptimal. Identifying characteristics of successful programs can improve the resident research training experience.
Research and scholarly activity are integral parts of residency training. Research participation increases residents’ ease in critically evaluating literature, fosters critical thinking, and can improve patient care through increased use of evidence-based medicine.1,2 In addition, research exposure may influence career paths.3
The Accreditation Council for Graduate Medical Education (ACGME) states that “residents should participate in scholarly activity.”4 Residency programs must provide a curriculum that advances residents’ knowledge of basic research principles, ensures participation in scholarly activity and allocates resources to facilitate this participation.4 However, this requirement is vague and allows much flexibility in its interpretation. Although individual programs have developed curricula to meet the requirement, these curricula are diverse and result in variable resident productivity and satisfaction.5–12
In 2001, the American Academy of Pediatrics (AAP) Committee on Pediatric Research reported that only 10% of graduates pursue traditional research careers.13 They encouraged research training early and recommended that programs establish curriculum for educating residents.13 Additionally, the AAP suggested that residency programs promote research rotations and encourage trainees to participate in a research project. Notably, neither the AAP nor the ACGME clearly defines their definition of scholarly activity or research.
Providing meaningful research training during residency remains a challenge.6,8 A 2001 survey of pediatric residents found that most reported only fair or poor knowledge of grant writing, statistical analysis, IRB regulations, manuscript writing and research design.3 A large percentage also reported little interest in conducting research during residency, although those who participated in a formal research training curriculum were more likely to want to conduct research.
Despite ACGME requirements, there is little guidance on how to effectively integrate scholarly activity into residency and the current state of pediatric resident scholarly activities is not well documented. While there are isolated reports of successes,5–7,9,14 there are few broad-based studies identifying characteristics of successful training programs.15 Our study objectives were to characterize the current state of resident scholarly activities in pediatric programs nationally and to identify characteristics of successful training programs. We defined success as being in the top quartile of programs for resident participation in scholarly activity. We also looked at the percentage of residents in a program presenting work nationally/internationally and publishing as secondary markers of success. Our definition of scholarly activity included only original research studies, systematic literature reviews or meta-analyses, and case reports or case series with references, to distinguish between original research and other scholarly activities. We chose these markers to define success because we felt an ideal program would provide exposure to all residents, and because an objective marker of quality would be scholarly activity leading to presentation or publication.
METHODS
Survey Administration
We performed a national cross-sectional web-based survey of pediatric program directors in October 2012. The survey was distributed via the Association of Pediatric Program Directors (APPD) list-serve. Recruitment letters with the survey link were emailed to program directors with 2 reminders. We received Institutional Review Board approval from Weill Cornell Medical College and research approval from the APPD.
Survey content
We developed the survey instrument (see Appendix A) after literature review and revised it after piloting it in June 2012 with several pediatric residency program directors and after peer-review by the APPD Research and Scholarship Task Force. Pilot answers were not included in analysis but program directors participating in the pilot received the final survey, allowing those programs to participate. The survey consisted of 20 questions in the following domains: 1) program characteristics; 2) resident participation in scholarly activity; 3) infrastructure to support scholarly activity; 4) barriers; and 5) outcomes. Survey questions related to program characteristics and outcomes were close-ended, while other questions offered closed and open-ended options.
Potential factors associated with resident scholarship included program-level characteristics and infrastructure. Survey items included program demographics (geographic region, size [small ≤ 30 residents, medium 31–60 residents, large >60 residents], setting [university-affiliated, community-based, military, or other]), and the existence of programmatic support for scholarship. We asked whether participation in scholarly activity was a graduation requirement, whether promotion was linked to scholarly project progress, and about minimum scholarly activity requirements. We asked program directors to rate the importance of a series of goals for resident scholarly activity, with a 5-option response scale ranging from “not at all important” to “extremely important.” Programmatic support included infrastructure (research director, scholarship review committee, statistician, research track, special training pathways, research curriculum, sufficient faculty mentors, resident work-in-progress sessions, Research Day, prize for resident scholarship), as well as individual support (funding, protected time for residents), faculty support (funding, protected time for faculty), and Chairman support. We also asked program directors to review barriers to resident scholarly activity and characterize each as a major barrier, minor barrier, or not a barrier. We asked program directors to report their program percentage compliance for the ACGME survey question assessing resident satisfaction with opportunities to participate in scholarly activity or research. We asked program directors to rate the importance of a series of goals for resident scholarly activity, with a 5-option response scale ranging from “not at all important” to “extremely important.” Lastly, we asked program directors to report on the scholarly activities of faculty within their department.
Analysis
We included all surveys with two or more questions completed in the analysis. We analyzed program traits as standard summary statistics -- mean and standard deviation for continuous variables and percentage for categorical variables. If a continuous variable had a skewed distribution, we calculated median and interquartile range (IQR). We compared respondent characteristics to characteristics of all programs nationally using FREIDA (the American Medical Association’s on-line website), although FREIDA divided programs into different program setting categories: university-based; community-based; community-based/ university affiliated, and military. Open-ended responses to any questions were reviewed and categorized into pre-existing categories (most expanded upon already existing answer choices) or separate categorizes if necessary.
We used Chi-square or Fisher’s Exact test to evaluate the association between two categorical variables. For our primary and secondary outcomes -- percent of residents who participated in scholarly activity and who presented at national/international meetings or published articles -- we divided programs into top quartile versus lower quartiles. We used logistic regression to evaluate the effect of potential factors on outcomes.
We developed the final regression model in stages, using separate models for the primary and secondary outcomes. First, univariate analyses were performed. We considered factors with p-values < 0.2 in the multivariable logistic regression. If factors were highly correlated within each domain only one factor was considered. We derived a model with statistically significant factors only (p< 0.05) using backward elimination technique. We calculated odds ratios (OR), 95% confidence intervals (CI), and p values. To address multiplicity adjustment, we used a modified alpha level of (0.05/number of comparisons) based on Bonferroni correction. Lastly, we calculated the Pearson correlation coefficient to test for correlation between our primary outcome and program response to the question “In your last ACGME resident survey, how satisfied were the residents with the opportunities your program provides for them to participate in research or scholarly activities?” We performed analyses in SAS Version 9.2 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Program Characteristics
We received responses from 105/199 programs (52.8 %). Half (n =51) of responding programs were medium-sized and 74% (n=77) were university-based (Table 1). Median faculty size per department was 70. We were unable to assess characteristics of non-respondents. The proportion of respondents was similar to all programs nationally in terms of size and geographic location, but we had over-representation of university-affiliated programs.
Table 1.
Characteristics of Responding U.S. Pediatric Residency Programs Compared to All Pediatric Residency Programs Nationally
| Variable | Total Respondents (N=105) |
All Accredited Programs Nationally (N = 199) |
p-value |
|---|---|---|---|
| Program Size based on Number of Categorical Residents, N (%) | p = 0.29 | ||
| Small (<30) | 30 (29.1) | 72 | |
| Medium (31–60) | 51 (49.5) | 80 | |
| Large (>60) | 22 (21.4) | 47 | |
|
Number of Faculty Members in the Department of Pediatrics, median (Interquartile Range 25%–75%) |
70 (40–120) |
Not available | |
| Residency Program Setting,* N (%) | p< .0001 | ||
| University-affiliated | 77 (74.0) | 100 | |
| Community** | 22 | 93 | |
| Military | 1 (1.0) | 6 | |
| Other | 4 (3.8) | ||
| Location, N (%) | p = 0.49 | ||
| Northeast | 31 (29.8) | 58 | |
| Midwest | 31 (29.8) | 45 | |
| South | 31 (29.8) | 69 | |
| West | 11 (10.6) | 27 | |
|
Number of Pediatric Fellowship Programs Median (Interquartile Range 25%–75%) |
2 (0–7) |
Not available | |
| Participation in scholarly activity is a requirement for graduation, N (%) | 77 (78.6) | —— | |
| Program links annual resident promotions to progress on their scholarly project, N (%) | 11 (14.3) | —— |
Note: All categories might not add up to 105 if respondents failed to answer a particular demographic question
Programs can indicate more than 1 answer choice
Community includes those programs who identified themselves either as a community-university affiliated program or a community-only program
Participation in Scholarly Activity
Participation in scholarly activity was a graduation requirement for most responding programs (78.6%, n=77), although promotion was generally not linked to project progress (14.3%, n=11). Program definitions of scholarly activity were highly variable. While 95.9% (n=94) of responding program directors included original research studies, 93.0% (n=91) included case reports or case series with references, and 88.8% (n=87) included quality improvement projects, only 73.4% (n=72) included systematic reviews or meta-analyses, 72.2% (n=70) included advocacy projects, 68.4% (n=67) included curriculum development, and 61.2% (n=60) included a book chapter. A small majority included giving a local teaching conference (60.2%, n=59) or grand rounds (57.1%, n=56).
Resident Scholarly Achievements
When scholarly activity was limited to original research studies, systematic reviews or meta-analyses, and case reports or series with references, the mean proportion of categorical pediatric residents participating over the past 3 years was 56%, with significant variability (range 0–100%). The same variability was true for residents presenting at a regional conference (mean 27%, range 0%–100%), presenting at a national or international conference (mean 13%, range 0%–80%), and publishing (mean 8%, range 0%–60%).
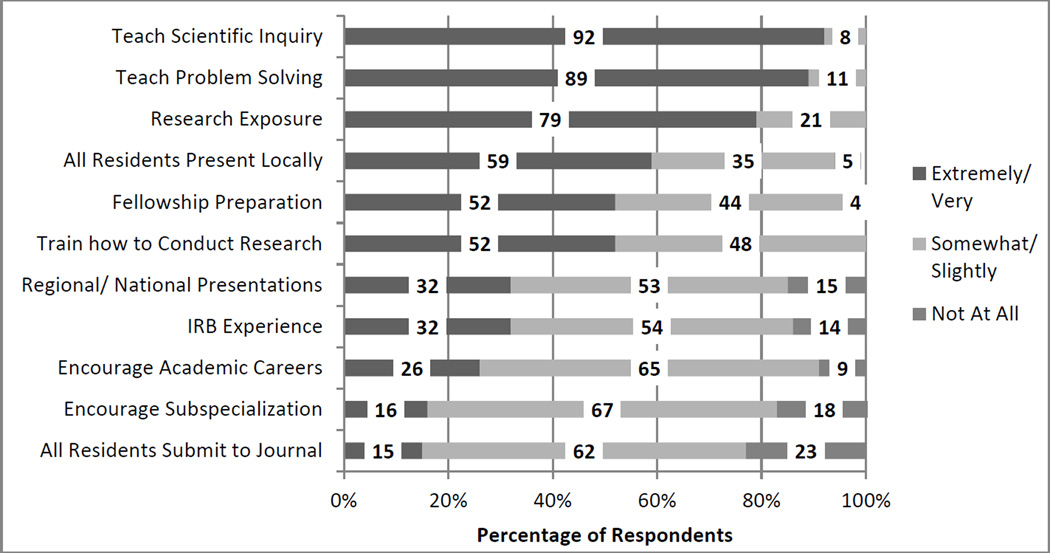
Program Director Goals
We asked program directors to rate the importance of eleven goals for resident scholarly activity (Figure 1). Top goals were: 1) teaching scientific inquiry (91.8%, n=89); 2) teaching problem-solving skills (88.7%, n=86); 3) providing research exposure (79.4%, n=77); 4) having all residents present their work locally (59.4, n=57%); 5) training residents how to conduct research (52.1%, n=50); and 6) preparing residents for fellowship (52.1%, n=50).
Figure 1.
Program Director Goals for Scholarly Activity for Pediatric Residency
Infrastructure to Support Scholarly Activity
Resources available to programs to support resident scholarly activity were variable (Table 2). The most common resource was funding (91.7%, n=88). While few programs had full or partial funding for residents to complete scholarly activity (15.8%, n=15 and 24.2%, n=23), many had full or partial funding to support conference presentations (40.6%, n=39 and 39.6%, n=38). Most program directors endorsed having a research day (79.4%, n=77), Chairman support (70.1%, n=68), sufficient faculty mentors (65.0%, n=63) and a statistician (65.0%, n=63). Large programs (95.2%, n=20) were more likely to report having sufficient faculty mentors compared with small (51.9%, n=14) or medium size programs (59.6%, n=28) (p=0.001 and p=0.003, respectively). Only one-third of programs (35.1%, n=34) had a research curriculum. The least available resource was protected faculty time (7.2%, n=7).
Table 2.
Resources Available to Responding U.S. Pediatric Residency Programs Stratified by Program Size
| Resources, N (%) | Alla (N = 105) |
Small (N = 30) |
Medium (N = 51) |
Large (N = 22) |
Overall p-value |
|---|---|---|---|---|---|
| Research funding | 88 (91.7) | 24 (88.9) | 41 (89.1) | 21 (100) | 0.31 |
| Research day or other venue for residents to present their work | 77 (79.4) | 21 (77.8) | 37 (78.7) | 18 (85.7) | 0.76 |
| Chairman support | 68 (70.1) | 18 (66.7) | 33 (70.2) | 15 (71.4) | 0.93 |
| Sufficient number of faculty mentors | 63 (65.0) | 14 (51.9) | 28 (59.6) | 20 (95.2) | 0.004 † ‡ |
| A statistician | 63 (65.0) | 20 (74.1) | 29 (61.7) | 12 (57.1) | 0.42 |
| Opportunity for residents to present work-in-progress | 55 (56.7) | 16 (59.3) | 21 (44.7) | 16 (76.2) | 0.049 ‡ |
| Award for resident scholarly accomplishments | 53 (54.6) | 12 (44.4) | 26 (55.3) | 14 (66.7) | 0.31 |
| A research director | 48 (49.5) | 17 (63.0) | 22 (46.8) | 7 (33.3) | 0.12 |
| A research curriculum | 34 (35.1) | 13 (48.1) | 16 (34.0) | 5 (23.8) | 0.21 |
| A scholarship review committee | 28 (28.9) | 13 (48.2) | 10 (21.3) | 4 (19.1) | 0.027 * † |
| Faculty funding to support resident scholarly activity | 11 (11.3) | 5 (18.5) | 3 (6.4) | 3 (14.3) | 0.25 |
| Required protected research time (months) | |||||
| 0 | 66 (70.2) | 21 (77.8) | 31 (70.5) | 13 (61.9) | 0.70 |
| 1 | 20 (21.3) | 5 (18.5) | 10 (22.7) | 5 (23.8) | |
| >1 | 8 (8.5) | 1 (3.7) | 3 (6.8) | 3 (14.3) | |
| A special training pathway | 13 (13.4) | 0 (0) | 3 (6.4) | 9 (42.9) | <.0001 † ‡ |
| Maximum number of additional elective time (months), | |||||
| 0 | 11 (11.5) | 5 (18.5) | 5 (10.6) | 1 (4.8) | 0.23 |
| 1 | 35 (36.5) | 11 (40.7) | 19 (40.4) | 5 (23.8) | |
| 2 | 27 (28.1) | 8 (29.6) | 12 (25.5) | 6 (28.6) | |
| 3 | 14 (14.6) | 3 (11.1) | 7 (14.9) | 4 (19.1) | |
| >=4 | 9 (9.4) | 0 (0) | 4 (8.5) | 5 (23.8) | |
| A research track within the program | 9 (9.3) | 0 (0) | 4 (8.5) | 5 (23.8) | 0.015 † |
| Protected time for faculty | 7 (7.2) | 1 (3.7) | 1 (2.1) | 4 (19.1) | 0.036 ‡ |
2 subjects had missing data for program size; therefore, the sum of each row may not add up to total column. Not all respondents answered each question.
= p<0.05 for small vs. medium;
= p<0.05 for small vs. large;
= p<0.05 for medium vs. large
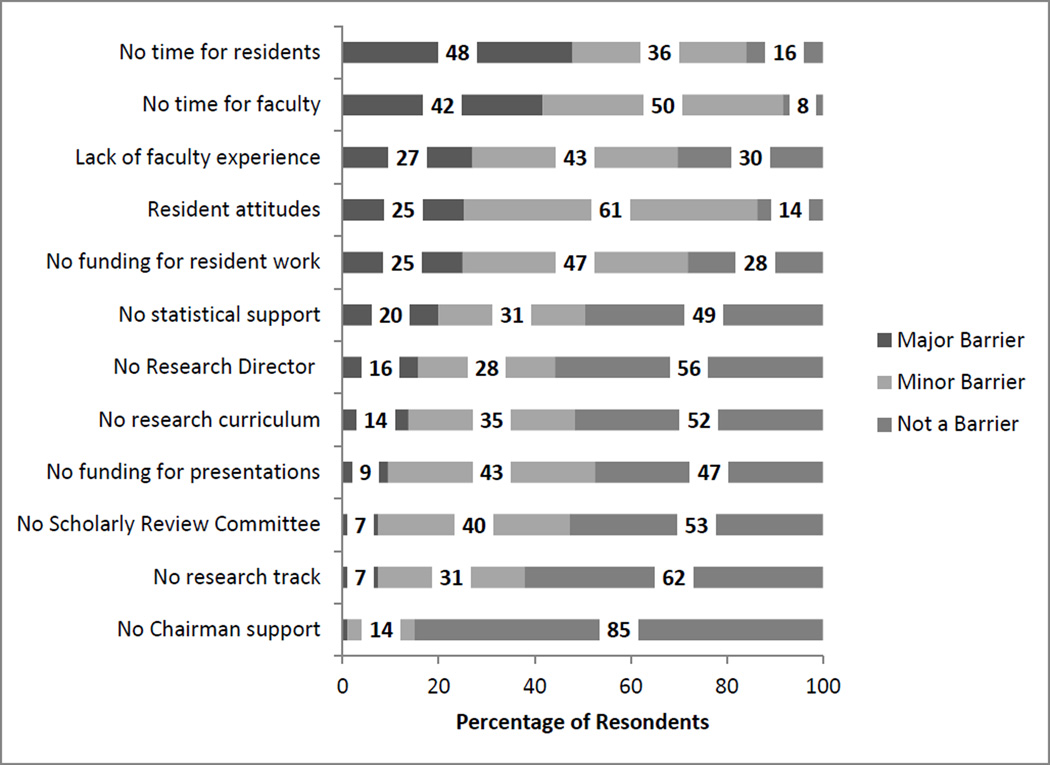
Barriers to Resident Scholarly Activity
Program directors identified numerous barriers to supporting resident scholarly activity (Figure 2). The top five major barriers were: 1) lack of resident time to conduct scholarly activity (47.9%, n=45); 2) lack of faculty time to mentor residents (41.7%, n=40); 3) lack of faculty experienced in conducting scholarly activity (27.1%, n=26); 4) resident attitudes (25.3%, n=24); and 5) lack of funding to support residents conducting scholarly activity (25.0%, n=24).
Figure 2.
Pediatric Residency Director Reported Barriers to Resident Scholarly Activity
Factors Associated with Successful Resident Scholarly Activity Programs
We identified three factors associated with being in the top quartile of programs for resident scholarly activity participation (≥85% participation): 1) requirement for resident participation in scholarly activity ((OR)=5.5, 95% CI 1.03–30.0); 2) program director belief in having all residents present their work regionally or nationally (OR=4.7, CI 1.5–15.1); and 3) having >25% of faculty mentor residents in the last 3 years (OR=3.6, CI 1.2–11.4). When we ran the same model utilizing program director belief in having all residents present their scholarly work locally (due to co-linearity with program director belief in presenting scholarly work regionally or nationally), this factor approached but did not achieve statistical significance (OR=3.10, 95% CI 1.0–9.7, p=0.05).
Because there was only 56% overlap between programs in the top quartile for participation and our productivity outcomes, we developed new multivariate models for our secondary outcomes. We could not identify any significant factors (data not shown). However, there was a trend toward significance for awarding of a prize for resident scholarly accomplishments (OR=2.2 (0.9–5.2), p=0.075).
We found a positive correlation between a program being in the top quartile for resident participation in scholarly activity and responses to the ACGME survey question on resident satisfaction with opportunities to participate in scholarly activity (correlation coefficient=0.32, p=0.01).
Program Director Satisfaction
Only 47.1% (n=41) of program directors reported being extremely or very satisfied with the percentage of residents engaged in scholarly activity. Less than half (48.9%, n=43) were extremely or very satisfied with the quality of scholarly activity and only 30.7% (n=27) were extremely or very satisfied with the quality of their program in training residents to produce scholarly activity.
DISCUSSION
Our results suggest that the scholarly activity experience for pediatric residents is highly variable and suboptimal. There appear to be many barriers for programs, including lack of resident and faculty time and lack of experienced faculty. We identified 3 factors associated with high participation programs: a requirement for scholarly activity, program director belief in the importance of all residents presenting their work regionally or nationally, and broad-based faculty mentorship. This is the first national pediatric survey, to our knowledge, to identify such factors. We were unable to identify factors associated with high rates of scholarly productivity. Nonetheless, these results provide important insight to inform national discussions on research training in pediatric graduate medical education.
The variability we found with regard to scholarly activity requirements has been described in other disciplines.15, 16 It is likely that the experience of residents will remain highly variable unless a common definition of scholarly activity is adopted. Despite this variability, it is clear that the requirements of pediatric residency programs have changed over time. While a 1996 national survey of pediatric residency programs found only 27% required scholarly activity participation,1 79% of programs we surveyed had a scholarly activity requirement. Notably, only 35% of programs reported having a formal resident research curriculum which is comparatively much lower than rates reported in internal and family medicine (47% and 76.6% respectively).15,17
Nearly all program directors identified the same top goals for a resident scholarly activity program -- teaching scientific inquiry and problem-solving skills. These are well aligned with the goals of the AAP Committee on Research.13 Many program directors also endorsed goals related to influencing trainee careers. Studies support that engaging residents in research may lead to increased participation in research post-residency.18 In addition, given fellowship research requirements,19 participating in research as a resident may help prepare trainees as they move to the next phase of training.
The variability in research training experienced by residents may account for research training deficiencies reported in post-graduate resident surveys as well as the low number of pediatricians pursuing academic careers.13,20 In annual national surveys of recent pediatric graduates from 2003–2009, quality of research training was rated lowest of all training areas.20 Providing a formal research curriculum and mentored research experience appears important for addressing this gap. Studies of residents who have completed mentored research projects have found that the experience increases knowledge, skills and the desire to conduct research.16,21–23
For programs looking to build or enhance a resident research program, we identified 3 factors associated with high participation programs. Two of those factors – a requirement for scholarly activity participation and program director belief that all residents should present their work regionally or nationally – emphasize the importance of leadership that values resident scholarly activity. Program director support has been identified as a critical factor in other studies.24 While there are many ways of defining a “successful” research program, ensuring that all residents are participating in a more rigorously defined scholarship experience (our definition of success) would help to reduce the variability experienced by residents and meet many goals endorsed by program directors, the ACGME and the AAP.
The third factor, broad-based faculty mentorship, is a challenge for many programs. Providing faculty development in mentoring and research conduct, as well as incentivizing faculty to mentor residents, will be important for establishing high participation research training programs. Certain incentives, such as mentoring awards, may be particularly important for programs with fewer monetary resources given that lack of funding is reported as a major barrier by 25% of programs in this study.
With recent curriculum changes mandated by the ACGME, including providing residents with 6 months of individualized curriculum, many programs may increase opportunities for resident scholarly activity participation to satisfy these requirements.4 Schedule changes that accommodate individualized curriculum may be necessary to help programs overcome the top barrier to resident scholarly activity– lack of resident time. However, amid national uncertainty regarding financing graduate medical education, and the many ACGME training requirements, programs may come under increasing pressure to balance patient care needs, financing, and the desire to encourage trainees in their research pursuits.25
Limitations
There were several limitations to this study. First, our response rate was 52.8%, which may make our results subject to non-response bias. This response rate is not dissimilar, however, to response rates for similar national surveys in other disciplines.17 Our distribution of respondents was similar to all pediatric programs nationally with regard to size and geographic location. It is difficult to determine if we had a greater proportion of university-affiliated programs because FREIDA categorizes programs differently, or if more university programs actually responded, possibly reflecting the stronger focus on research in university settings. If the latter is true, our results might overestimate the training occurring within pediatric residency programs nationally and rates of resident participation in scholarly projects. This should be further investigated. Additionally, this survey was only distributed to pediatric program directors and does not reflect resident perspectives. Future studies assessing detailed resident perspectives should be performed.
We were also unable to identify factors associated with high productivity among residency programs, as program director self-report may not be the ideal methodology, because far fewer residents present their work nationally/ internationally or publish in a journal, or because there are other factors not assessed by this survey associated with high productivity. Finally, inherent limitations of a survey format do not allow exploration of details about unique individualized programs or institution specific resources that may contribute to the success of scholarly activity programs, including recruiting residents interested in research to such programs.
Conclusions
The current state of resident scholarly activity in pediatric training programs appears suboptimal and there is much work to be done to institute a formal research curriculum broadly. This study identified some of the barriers and limitations as perceived by program directors, including protected time for residents and faculty, lack of faculty skilled in research, resident attitudes, and funding. Of programs with the highest levels of participation, items most associated with participation were making research activity a requirement, program director belief in the importance of all residents presenting regionally or nationally, and having >25% of faculty available for mentorship. It is our hope that identification of these barriers and strengths will help programs focus their efforts at the most necessary and pertinent arenas to improve their research programs, fulfill ACGME requirements, and advance pediatric research careers. We also hope it will inspire national discussions in light of the many changes occurring within graduate medical education.
Table 3.
Logistic Regression Identifying the Effects of Features on High Participation Scholarly Activity Programs*
| Program Features | Univariate Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| OR (95% C.I.) |
p-value | OR (95% C.I.) |
p-value | |
|
Participation in scholarly activity is required: Yes |
5.8 (1.2–27.3) | 0.027 | 5.5 (1.03–30.0) | 0.047 |
| No | 1.0 (Ref) | |||
|
Program director believes having all residents present their scholarly project is extremely or very important: Yes |
4.7 (1.6–13.4) | 0.004 | 4.7 (1.5–15.1) | 0.01 |
| No | 1.0 (Ref) | |||
|
>25% of faculty have mentored residents in the last 3 years: Yes |
4.8 (1.7–13.7) | 0.004 | 3.6 (1.2–11.4) | 0.027 |
| No | 1.0 (Ref) | |||
|
Regional Location: Northeast |
1.0 (Ref) |
|||
| Midwest | 1.8 (0.5–6.6) | 0.37 | ||
| South | 3.2 (0.9–11.3) | 0.07 | ||
| West | 0.5 (0.05–4.7) | 0.51 | ||
|
Protected time for faculty to support resident scholarly activity is available: Yes |
8.5 (0.9–80.2) | 0.062 | ||
| No | 1.0 (Ref) | |||
|
>75%residents satisfied with scholarly activity opportunities provided in more recent ACGME resident survey: Yes No |
2.9 (0.9–9.7) 1.0 (Ref) |
0.082 | ||
“High Participation” represents the top quartile of programs, or >85% participation by residents in conducting original research studies, systematic reviews or meta-analyses, or case reviews or series with references
Acknowledgments
We thank the pediatric program directors who participated in this study.
Funding/Support: This project was supported in part by funds from the Clinical Translational Science Center (CTSC), National Center for Advancing Translational Sciences (NCATS) grant #UL1-TR000457-06.
Footnotes
The authors have no potential conflicts of interest.
Other disclosures: None
Ethical approval: We received institutional review board approval from Weill Cornell Medical College to conduct this study.
Previous presentations: We presented our findings as a poster presentation at the Association of Pediatric Program Directors and Council on Medical Student Education in Pediatrics national conference on April 12, 2013 in Nashville, Tennessee. We presented our findings as a platform presentation at the Pediatric Academic Societies’ national conference on May 4, 2013 in Washington D.C.
Contributor Information
Erika L. Abramson, Departments of Pediatrics and Public Health, Weill Cornell Medical College, New York, NY.
Monique M. Naifeh, Department of Pediatrics, University of Oklahoma, Oklahoma City, OK..
Michelle D. Stevenson, Department of Pediatrics, University of Louisville, Louisville, KY.
Christopher Todd, Department of Pediatrics, Texas Tech University, Amarillo, TX..
Emilie D. Henry, Department of Pediatrics, the University of Oklahoma, Oklahoma City, OK.
Ya-Lin Chu, Department of Public Health, Weill Cornell Medical College, New York, NY.
Linda M. Gerber, Department of Public Health, Weill Cornell Medical College, New York, NY.
Su-Ting T. Li, Department of Pediatrics, University of California Davis, Sacramento, CA.
REFERENCES
- 1.Brouhard BH, Doyle W, Aceves J, McHugh MJ. Research in pediatric residency programs. Pediatrics. 1996 Jan;97(1):71–73. [PubMed] [Google Scholar]
- 2.Rothberg MB. Overcoming the obstacles to research during residency: what does it take? Jama. 2012 Dec 5;308(21):2191–2192. doi: 10.1001/jama.2012.14587. [DOI] [PubMed] [Google Scholar]
- 3.Cull WL, Yudkowsky BK, Schonfeld DJ, Berkowitz CD, Pan RJ. Research exposure during pediatric residency: influence on career expectations. The Journal of pediatrics. 2003 Nov;143(5):564–569. doi: 10.1067/S0022-3476(03)00324-X. [DOI] [PubMed] [Google Scholar]
- 4.Accreditation Council on Graduate Medical Education Common Program Requirements. [Accessed April 3, 2013];2011 Jul 1; https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQPIF/320_pediatrics_07012013.pdf. [Google Scholar]
- 5.Mills LS, Steiner AZ, Rodman AM, Donnell CL, Steiner MJ. Trainee participation in an annual research day is associated with future publications. Teaching and learning in medicine. 2011 Jan;23(1):62–67. doi: 10.1080/10401334.2011.536895. [DOI] [PubMed] [Google Scholar]
- 6.Vinci RJ, Bauchner H, Finkelstein J, Newby PK, Muret-Wagstaff S, Lovejoy FH., Jr Research during pediatric residency training: outcome of a senior resident block rotation. Pediatrics. 2009 Oct;124(4):1126–1134. doi: 10.1542/peds.2008-3700. [DOI] [PubMed] [Google Scholar]
- 7.Ozuah PO. Residency research requirement as a predictor of future publication productivity. The Journal of pediatrics. 2009 Jul;155(1):1–2. 2 e1. doi: 10.1016/j.jpeds.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 8.Roth DE, Chan MK, Vohra S. Initial successes and challenges in the development of a pediatric resident research curriculum. The Journal of pediatrics. 2006 Aug;149(2):149–150. doi: 10.1016/j.jpeds.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Shin AY, Almond CS, Mannix RC, et al. The Boston Marathon Study: a novel approach to research during residency. Pediatrics. 2006 May;117(5):1818–1822. doi: 10.1542/peds.2005-1249. [DOI] [PubMed] [Google Scholar]
- 10.Seehusen DA, Asplund CA, Friedman M. A point system for resident scholarly activity. Family medicine. 2009 Jul-Aug;41(7):467–469. [PubMed] [Google Scholar]
- 11.Desbiens NA. A departmental experience in promoting oral and poster presentations. Teaching and learning in medicine. 2008 Jul-Sep;20(3):254–260. doi: 10.1080/10401330802199575. [DOI] [PubMed] [Google Scholar]
- 12.Crownover B, Crawford PF. Areas of concentration increase scholarly activity: a 15-month experience. Family medicine. 2008 Feb;40(2):87–90. [PubMed] [Google Scholar]
- 13.Chesney RW, Dungy CI, Gillman MW, et al. Promoting education, mentorship, and support for pediatric research. Pediatrics. 2001 Jun;107(6):1447–1450. [PubMed] [Google Scholar]
- 14.Lovejoy FH, Jr, Zuckerman BS, Fleisher GR, Vinci RJ. Creating an academic culture during residency training. The Journal of pediatrics. 2008 May;152(5):599–600. 600 e591. doi: 10.1016/j.jpeds.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Levine RB, Hebert RS, Wright SM. Resident research and scholarly activity in internal medicine residency training programs. J Gen Intern Med. 2005 Feb;20(2):155–159. doi: 10.1111/j.1525-1497.2005.40270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neale AV. A national survey of research requirements for family practice residents and faculty. Family medicine. 2002 Apr;34(4):262–267. [PubMed] [Google Scholar]
- 17.Crawford P, Seehusen D. Scholarly Activity in Family Medicine Residency Programs: A National Survey. Family medicine. 2011 May;43(5):311–317. [PubMed] [Google Scholar]
- 18.Ledley FD, Lovejoy FH., Jr Factors influencing the interests, career paths, and research activities of recent graduates from an academic, pediatric residency program. Pediatrics. 1993 Sep;92(3):436–441. [PubMed] [Google Scholar]
- 19.The American Board of Pediatrics. Training Requirements for Subspecialty Certification. North carolina: 2004. [Google Scholar]
- 20.Frintner MP, Cull WL. Pediatric training and career intentions, 2003–2009. Pediatrics. 2012 Mar;129(3):522–528. doi: 10.1542/peds.2010-3603. [DOI] [PubMed] [Google Scholar]
- 21.Fraker LD, Orsay EM, Sloan EP, Bunney EB, Holden JA, Hart RG. A novel curriculum for teaching research methodology. J Emerg Med. 1996 Jul-Aug;14(4):503–508. doi: 10.1016/0736-4679(96)00090-x. [DOI] [PubMed] [Google Scholar]
- 22.Morris BA, Kerbel D, Luu-Trong N. Family practice residents' attitudes toward their academic projects. Family medicine. 1994 Oct;26(9):579–582. [PubMed] [Google Scholar]
- 23.Hayward RA, Taweel F. Data and the internal medicine houseofficer: alumni's views of the educational value of a residency program's research requirement. J Gen Intern Med. 1993 Mar;8(3):140–142. doi: 10.1007/BF02599759. [DOI] [PubMed] [Google Scholar]
- 24.DeHaven MJ, Wilson GR, O'Connor-Kettlestrings P. Creating a research culture: what we can learn from residencies that are successful in research. Family medicine. 1998 Jul-Aug;30(7):501–507. [PubMed] [Google Scholar]
- 25.Nemergut EC. Resident research and graduate medical education funding. Anesthesiology. 2013 Mar;118(3):757–758. doi: 10.1097/ALN.0b013e3182837db5. [DOI] [PubMed] [Google Scholar]