The authors conducted a retrospective review of the charts of patients in a large academic practice who underwent select surgical procedures and they contacted those patients’ families by telephone 2 weeks after intervention. Six months after implementation, overall postoperative appointments decreased from 55.5% to 35.5%, and 62.6% of patients had a successful postoperative phone call follow-up. A satisfaction survey revealed that 93% of patients were highly satisfied.
Abstract
Context:
Typical follow-up for surgical procedures consists of an interim history and brief focused physical examination. These appointments occupy clinic resources, require a time investment by the family, and rarely identify problems. Previous studies have demonstrated the safety of a postoperative phone call.
Objective:
Compare a traditional in-person clinic postoperative visit with postoperative phone call follow-up regarding patient satisfaction, rate of successful follow-up, and clinic resource utilization in a large academic practice.
Design:
A retrospective review of charts of patients who underwent select surgical procedures, along with a review of the clinic schedule for the same time period.
Main Outcome Measures:
Efficacy, patient/family satisfaction, and impact on the clinic.
Methods:
Families were contacted by telephone two weeks after select surgical procedures to assess for complications and questions. Cohorts of patients six months before and six months after implementation were assessed for main outcome measures.
Results:
Before implementation, 55.5% of patients (427/769) who had one of the select surgical procedures were seen in the clinic postoperatively, and 62.6% (435/695) had a successful postoperative phone call follow-up. There were also 1090 overall scheduled postoperative appointments. Six months after implementation, overall postoperative appointments decreased 35.5% to 703. Overall, postoperative-scheduled visits decreased by 6% compared with new visits and other general follow-up visits, which each increased by 3%. A satisfaction survey revealed that 93% of patients (n = 231) were highly satisfied with the process. A hospital cost analysis suggested an 89% cost savings ($101.75 per patient for clinic visit vs $12.50 per patient for phone call follow-up).
Conclusion:
Postoperative phone call follow-up is an effective tool that improves patient and physician efficiency and satisfaction.
INTRODUCTION
Postoperative follow-up of the patient who has undergone pediatric general surgery is important for ensuring and maintaining optimal patient outcomes. A postoperative phone call follow-up for select procedures offers potential advantages to the patient, family, and surgeon without sacrificing patient safety. The traditional postoperative visit after most general surgery procedures consists of an in-person clinic visit two to four weeks after the operation. Follow-up typically occurs in a defined clinic that requires the investment of substantial amounts of time by the family and the physician, requires hospital or practice resources to maintain and staff the clinic, and results in lost productivity at school and work for the family. In contrast, a postoperative phone call offers more efficient use of time and increased accessibility to postoperative follow-up for the family, decreased use of clinic space and resources, and potential major cost savings for the institution.
The purpose of this study is to evaluate the utility and effectiveness of a postoperative phone call compared with a traditional in-person clinic postoperative visit for a select group of general surgery procedures. The factors assessed include the success rate of contacting families, the time savings achieved from removing some postoperative patients from the clinic, the parent/family satisfaction rates, and the financial implications for the institution.
METHODS
A postoperative phone call protocol was developed for common, low-risk surgical procedures. Data were collected regarding the number of patients successfully contacted, family satisfaction, and the impact of the change on the utilization of the physicians’ outpatient clinic, including the change in follow-up and new visits and the potential financial impact of the change. Prospective data were collected for six months beginning in August 2011 and compared with historical data from the preceding six months. Procedures were selected for inclusion in the protocol on the basis of low overall complication rates and potential complications characterized by simple wound issues or subjective symptoms easily assessed by the family. The procedures selected for inclusion in the study included appendectomy for treatment of uncomplicated appendicitis, cholecystectomy, pyloromyotomy, umbilical and inguinal hernia repair, simple lesion excision, circumcision, gastrocutaneous fistula closure, and central venous catheter placement.
Education of surgical faculty, surgery nurse practitioners (NPs), staff nurses who perform phone call follow-up, and surgery residents and fellows was provided before initiating the postoperative phone call protocol. Education included the specific surgical procedures to be included; educating parents and families about the follow-up process, including the option for a traditional in-person clinic postoperative visit; and entering a default order for a postoperative phone call in the electronic medical record (EMR) ordering system. The EMR was then used to create a work queue of patients due for a postoperative phone call.
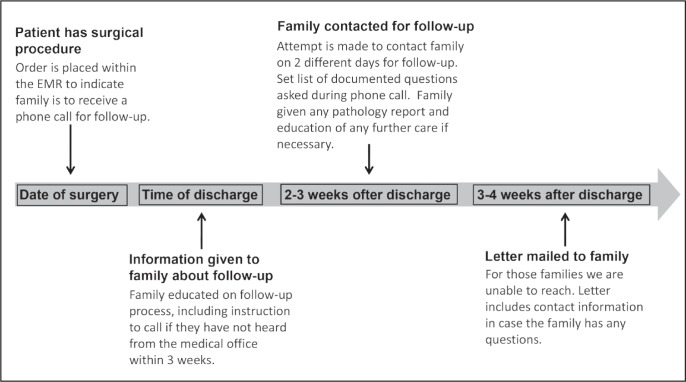
Patients, or their parents depending on age, received a telephone call from an advanced practice nurse approximately two to three weeks after the date of surgery (Figure 1). At minimum, two attempts were made to contact each patient or his/her parent. The postoperative phone call included a detailed template of questions designed to identify complications or potential concerns requiring further evaluation. Data from the phone interview were incorporated into the EMR and became a permanent part of the patient’s record. The template questions covered general patient condition, assessment of surgical wound, level of pain, the need for and/or use of pain medications, activity level, diet intake, bowel and urinary function, and discussion of pathology results if indicated. The postoperative phone call also allowed parents to voice any other concerns or questions they may have had related to their child and his/her surgery. Last, the postoperative phone call gave the option for a clinic follow-up visit if the parent desired, and it encouraged the parent to call back with any questions or concerns.
Figure 1.
Phone follow-up protocol.
EMR = electronic medical record.
When no one was reached, a voice message was left indicating that the surgery NP was calling to conduct the postoperative phone call. A second attempt to reach the parent by telephone was made the following day. All families received at least two calls on two different days of the week. Parents were able to call back at their leisure and speak with the NP to conduct the postoperative phone call.
Finally, for parents or patients who did not return the call or for those found to have telephone numbers that were disconnected or where it was not possible to leave voice messages, a detailed letter was mailed to the home. The letter indicated the Surgery Department’s attempts to call and conduct a postoperative phone call as well as contact numbers for the parent or patient to return the call.
For the purposes of the study, a successful traditional in-person, clinic postoperative visit was defined as the parent making an appointment and following through with the visit. A successful postoperative phone call was defined as successful family contact and completion of the questionnaire template.
RESULTS
We reviewed the clinic schedule for all patients coming to see the General Surgery Department from March 2011 through February 2012. In the 6 months before the implementation of the postoperative phone call follow-up, there were 1090 scheduled postoperative appointments made. Six months after implementation, the number of scheduled postoperative appointments was 703, or a 35.5% decrease. This created an overall change in the makeup of scheduled clinic appointments. There was a 6% decrease in all postoperative scheduled visits, from 27% to 21%. This increased the percentage of both new visits and other general follow-up visits by 3% each (Figure 2) during the same period.
Figure 2.
Schedule clinic appointment by type.
A total of 1464 charts were reviewed of patients undergoing the selected procedures from the same period. We compared the rate of successful follow-up in clinic with postoperative phone calls. Before the postoperative phone call follow-up, 55.5% of patients (427/769) had a successful clinic follow-up after their surgical procedure. The number of patients who had a successful postoperative phone call for the same selected surgical procedures increased to 62.6% (435/695). A satisfaction survey was performed with families at the time they received their postoperative phone call from June 2012 to September 2012, with 93% (n = 231) reporting being satisfied with the process compared with making a clinic appointment.
The administrative cost of the telephone protocol was based on the average salary of an NP for time to complete the postoperative phone call. This cost was compared with the calculated fixed costs of running the clinic per patient, which is based on staffing and a proportionate share of other expenses for the clinic (supplies, purchased services, etc). There was an 89% cost savings ($101.75 vs $12.50 per patient) for the institution when we performed a financial comparison looking at the decrease in administrative cost for the phone call follow-up (Table 1). The financial assessment did not account for the potential cost to the family of travel expenses or the lost time from work and school.
Table 1.
Comparison of before and after implementation of telephone postoperative follow-up
| Measure | Before | After | Outcome |
|---|---|---|---|
| Number of scheduled postoperative clinic appointments | 1090 | 703 | 36% decrease |
| Successful completion of follow-up (%) | 56 | 63 | p < 0.01 (χ2 test) |
| Cost (US $) per completed encounter: clinic vs phone | 101.75 | 12.50 | 88% cost savings |
DISCUSSION
Telephone contact with patients has been demonstrated to be a useful tool in managing chronic illnesses, providing reassurance, monitoring disease status, and providing a means for questions and concerns to be addressed in the critical time for patients and families after surgery.1 A study in the adult population showed telephone communication after discharge assisted in recognizing and facilitating compliance in patients who required help in understanding their treatment plan and medications.2 This same study also reported significantly higher satisfaction rates among patients receiving postoperative phone calls vs the control group. A study conducted at the Arkansas Children’s Hospital, Little Rock, demonstrated the postoperative phone call as a safe means of postoperative follow-up.3 Although this study included many of the same surgeries our retrospective study addressed, it did not make or show direct comparisons of postoperative phone calls to actual traditional in-person clinic postoperative visits as related to the number of successful follow-ups between the 2 methods. Furthermore, the previous study included 3 pediatric surgeons and 563 patient charts. Our study was conducted on a much larger scale, with a substantially greater number of pediatric general surgeons involved and number of patient charts reviewed. Our protocol allows for taking advantage of the EMR to order, to track, and to record the follow-up process, making it possible to involve 19 pediatric general surgeons and 1464 patient charts over the study period. Incorporating the process into our standard work flow has created a sustainable process with minimal cost.
A Cochrane review of postoperative phone call follow-ups conducted by various health care professionals for patients discharged from the hospital found that postoperative phone calls made by hospital-based health professionals was considered a good means of information exchange for symptom management, patient instruction and education, provision of reassurance, and early recognition of potential complications.4 However, the review underscored the lack of methodologic quality of the reviewed studies. In addition, the effectiveness of postoperative phone calls compared with control groups was lacking, with no statistically significant differences demonstrated. Our current study clearly demonstrates the efficacy and utility of postoperative phone calls to achieve a significantly higher number of follow-ups compared with traditional in-person clinic postoperative visits. In addition, using postoperative phone calls as an alternative to the traditional in-person clinic postoperative visit allowed clinic time and space that would have otherwise been used for the postoperative visits to instead be available for new and other general follow-up surgical visits. This shift in clinic utilization is beneficial to the surgical practice without sacrificing patient satisfaction or safety.
A study in the Netherlands compared cost-effectiveness of clinic follow-up visits vs telephone follow-up after breast cancer surgery.5 A number of factors, including patient-related costs, loss of productivity, and hospital-level costs were evaluated. The study found hospital or clinic follow-up to be more costly overall vs postoperative phone call. Our study showed a substantial institutional financial savings of 88% when clinic follow-ups were replaced with telephone follow-ups for a specified number of surgical procedures. Although not directly measured in the study, a theoretical cost savings for the family may be extrapolated related to time saved from missed work and school, as well as travel time and expense.
There are several limitations of this study. First, the question of family satisfaction was asked at the end of the telephone follow-up call, which could cause possible bias. This could be addressed in a future study with a separate follow-up survey of families who could be reached, as well as those whom we were unable to reach for a postoperative telephone follow-up. Second, reviewing a full year for each method of follow-up could reduce any potential impact that school or family work schedules may have had on our rate of follow-up. It would have also been useful to track the average time of clinic visits compared with the average time of postoperative calls. Finally, we did not track the number of patients and families we failed to reach via our postoperative phone call who later came to the Emergency Department or clinic for problems related to their surgical procedure.
CONCLUSION
Postoperative phone calls after select surgical procedures provide a higher rate of follow-up with patients and families compared with traditional in-person clinic postoperative visits. Along with an increased rate of follow-up, there was a noted decrease in direct cost to the institution and an inferred cost savings for families and patients. These were achieved with a high level of reported family satisfaction.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Basic Facts
There is a side to human behavior in health and disease which is not a thing of the intellect, which is irrational and emotional but important. It is the mainspring of most of what we do and a great deal of what we think, but is in danger of being neglected by clinical science … How often, indeed, do we physicians omit to enquire about the basic facts of happiness and unhappiness in our patients’ lives. Yet all this is just as much the live fabric of medicine as biochemistry and applied physiology.
— Platt R. Reflections on medicine and humanism: Linacre lecture. Higher Education Quarterly 1963 Aug;17(4):327–40
References
- 1.Kassmann BP, Docherty SL, Rice HE, Bailey DC, Jr, Schweitzer M. Telephone follow-up for pediatric ambulatory surgery: parent and provider satisfaction. J Pediatr Nurs. 2012 Dec;27(6):715–24. doi: 10.1016/j.pedn.2012.02.004. DOI: http://dx.doi.org/10.1016/j.pedn.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Braun E, Baidusi A, Alroy G, Azzam ZS. Telephone follow-up improves patients satisfaction following hospital discharge. Eur J Intern Med. 2009 Mar;20(2):221–5. doi: 10.1016/j.ejim.2008.07.021. DOI: http://dx.doi.org/10.1016/j.ejim.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 3.McVay MR, Kelley KR, Mathews DL, Jackson RJ, Kokoska ER, Smith SD. Postoperative follow-up: is a phone call enough? J Pediatr Surg. 2008 Jan;43(1):83–6. doi: 10.1016/j.jpedsurg.2007.09.025. DOI: http://dx.doi.org/10.1016/j.jpedsurg.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 4.Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD004510. doi: 10.1002/14651858.CD004510.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimman ML, Dirksen CD, Voogd AC, et al. Economic evaluation of four follow-up strategies after curative treatment for breast cancer: result of an RCT. Eur J Cancer. 2011 May;47(8):1175–85. doi: 10.1016/j.ejca.2010.12.017. DOI: http://dx.doi.org/10.1016/j.ejca.2010.12.017. [DOI] [PubMed] [Google Scholar]