Abstract
Introduction
The magnitude of stress and associated health consequences experienced by caregivers compromises their ability to effectively provide care to children, especially children with disability.
Methods
We used latent class analysis of data from the 2010 Ohio Family Health Survey and identified three distinct classes of caregivers based on patterns of responses to 15 financial and psychological stresses they experienced.
Results
Compared to children residing in households where caregivers experienced very little or no stress, children with disability were twice as likely to reside with caregivers with high levels of financial stress and almost three and half times as likely to reside with caregivers with high levels of financial stress and very high levels of psychological stress than typically developing children.
Discussion
Reducing caregiver stress is a critical step to ensuring the best health outcomes possible for children with disability. We identify the heterogeneity that is present in the population of caregivers by virtue of patterns of responses to various financial and psychological stressors. Children with disability are more likely to live in households where a greater number of stressors affect caregivers. Different confounders are also associated with the latent classes of stress we identify. This is an important implication when determining the right interventions to target to the right subpopulations.
Keywords: disability caregiver stress distress
Introduction
The Family Stress Model developed by Conger (Conger et al., 1992) proposes that poor child health outcomes are directly associated with factors such as poor family financial status, psychological distress, and poor parenting (e.g., ineffective parenting). In addition, psychological distress acts as an intermediary effect between poor family financial status and poor child health outcomes.
McPherson et al. (1998) define children with special health care needs (CSHCN) as children who have or are at increased risk for a chronic physical, developmental, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally. Children with functional limitations or developmental, behavioral, or emotional problems (functional impairment) are a subset of CSHCN. Many of these children have complex multisystem problems. The extensive caregiving “burden”, namely time, money, employment constraints, activity limitations, and general commitment required, is at the root of a diminished level of personal well-being for many caregivers of CSHCN children (Kuo, Cohen, Agrawal, Berry, & Casey, 2011; Majnemer, Shevell, Law, Poulin, & Rosenbaum, 2012; McCann, Bull, & Winzenberg, 2012). Mothers indicate having poorer health (Eisenhower, Baker, & Blacher, 2009), more depressive symptoms, and a diminished level of quality of life (Brehaut et al., 2009; Gupta, 2007; Lach et al., 2009).
Poor financial status is often associated with caring for CSHCN, especially children with disabilities that include functional limitations or impairment. Researchers have found that the more severe the disability, the greater the likelihood of family finance-related problems (Kuhlthau, Hill, Yucel, & Perrin, 2005). Reports show that 25% to 30% of families have to cut back work hours or stop working entirely due to their child's condition, likely exacerbating family financial problems (Emerson, 2003; Parish, Seltzer, Greenberg, & Floyd, 2004; Porterfield, 2002; van Dyck, Kogan, McPherson, Weissman, & Newacheck, 2004). In addition, families of CSHCN have higher out-of-pocket expenses and lower rates of private insurance, compared to families caring for typical children (Davidoff, 2004). Children with disabilities are less likely to live in a home with two married caregivers than typically developing children (Anderson, Larson, Lakin, & Kwak, 2002; Hogan, Rogers, & Msall, 2000), and more likely to live in homes headed by single mothers with less household income (Cohen & Petrescu-Prahova, 2006).
The goals of this study were two-fold. First, we identified subpopulations of caregivers of children based on the type and compounded amount of different financial and psychological stresses they experienced. Second, we tested the hypothesis that children with disability were more likely to live in households with caregivers who experienced many stressors than in households where caregivers experienced little or no stress.
Methodology
Data Source
We used a retrospective cohort design incorporating data from the 2010 Ohio Family Health Survey (OFHS). The 2010 survey emphasized how financial and psychological stresses affected Ohio families and Ohio's health system in general. Data collected were indicators of health insurance coverage, health status, health-risk behaviors, access to care, health care utilization, health care costs, and unmet health needs.
The 2010 OFHS was a stratified telephone survey with a list-assisted sampling frame that identified potential respondents using random digit dialing and surveyed respondents using computer assisted telephone interviewing (CATI) methods. A separate cell phone sample ensured a reliable, representative sample of younger adults, perhaps more easily reached via cell phones. The survey excluded potential respondents if they resided in an institution or group quarters, lived in Ohio for less than one month, did not speak English or Spanish well enough to be interviewed, or had a physical or mental impairment that precluded them from completing an interview and a proxy was not available. OFHS thoroughly vetted the final survey instrument for construct validity in English and Spanish, and professionally trained interviewers mitigated the potential for response bias.
Participants
In total, the OFHS was administered in 8,276 Ohio households between August and October, 2010. Of these households, a total of 2,002 contained at least one child 17 years of age or younger, and the survey interviewer selected one child to participate in the survey. In households with multiple children, the interviewer randomly selected one child.(ICF Macro, 2011) The interviewer asked the adult in the household with the best knowledge of the health insurance coverage of the child to respond as a proxy. Most often a parent responded to questions about these children (86.5%). However, grandparents (8.8%), other relatives (3.4%), and legal guardians or foster parents (1.3%) also acted as child proxy respondents. For the purpose of presenting results in this study, we refer to all child proxy respondents as “caregivers.”
We analyzed secondary, de-identified data and as such an Institutional Review Board at Cincinnati Children's Hospital Medical Center deemed this study exempt from full review.
Definition of Disability
Children were identified as having a disability if they were limited or prevented in any way in their ability to do the things most children of the same age could do due to a medical condition or had any emotional, developmental, or behavioral problems which needed treatment or counseling (CSHCN Screener©; Bethell et al., 2002). We identified children as typically developing if they did not have these limitations or problems, even though they may have met other CSHCN criteria.
Stressor Variables
For financial stressors, a “yes” response to problems paying or inability to pay for medical bills in the previous 12 months triggered questions about the following: 1) inability to pay for basic necessities such as food, heat, or rent; 2) used up most or all of financial savings; 3) had a large credit card debt, had to take a loan, or incur other debts; and 4) had to declare bankruptcy. A “yes” response to problems paying rent, mortgage, or utility bills in the previous 12 months triggered questions about the following: 1) received financial help when not able to pay rent, mortgage, or utility bill, and 2) had to have children move in with others. Caregivers who answered “no” to the lead-in trigger questions had the subsequent follow-up financial stressor questions imputed to “no” as well, even though the interviewer did not explicitly ask those questions. How long savings would cover living at the current address with the same standard of living if the caregiver lost complete income was recoded to represent less than six months or at least six months.
Psychological stressors included questions about how the caregiver usually felt during the past 30 days. These six questions form the Kessler-6 psychological distress battery and included the extent of feeling: sad, nervous, restless or fidgety, hopeless, everything is an effort, and worthless (Kessler et al., 2003). Interviewers coded responses on a Likert scale ranging from 0 (none of the time) to 4 (all of the time). If the six Kessler-6 scores totaled 12 or more, the caregiver was classified as having serious psychological distress. For multivariable analysis, we dichotomized and recoded the individual Kessler-6 responses to none, a little, or some of the time (0, 1, 2) or most or all of the time (3, 4).
Main Predictor and Covariates
Caring for a child with disability or not was the main predictor variable. In multivariable statistical models, we adjusted this predictor for child age groups (0-5, 6-12, and 13-17 years), gender (Male and Female), race/ethnicity (White (non-Hispanic), Black (non-Hispanic), Hispanic, and Other), health insurance status (Job-based private, Medicaid, Other, and Uninsured) and caregiver age groups (18-24, 25-34, 35-44, and 45 years and over), marital status (Married, Single, and Divorced/Separated/Widowed), and education (Less than high school, High school or equivalent, and Some college or higher degree). We profiled the parent-reported health status (Excellent, Very Good, or Good/Fair/Poor) of the child and the household poverty level (<100%, 101%-200%, 201%-300%, or >300% of federal poverty level (FPL)) but do not include these as covariates in the multivariable models due to multicollinearity with other model covariates.
Statistical Analysis
We analyzed the 2010 OFHS data using complex survey statistical procedures contained in SAS Enterprise Guide 4.2 (SAS Institute, Cary, NC) that accounts for population survey weights and strata. We determined differences (unadjusted) between children with disability and non-disability demographic groups, and stressor outcome and covariate categories on the basis of Rao-Scott chi-square tests of association using a significance level of α = 0.05. We used multivariable logistic regression models to determine statistical differences between the two groups, adjusting for child and caregiver characteristics. A 95% confidence interval (CI) for adjusted odds ratios (AOR) that have a range with all values greater than 1 indicated that caregivers of children with disability were more likely to experience the stressor being modeled.
We believe that patterns in the observed response to indicators of financial and psychological stress were due to an underlying mixture of heterogeneous groups of caregivers experiencing no stress or different combinations of stressors. We used latent class analysis (LCA) to determine if there were distinct response patterns across the 15 indicators of financial and psychological stress when child and caregiver characteristics were also taken into account. LCA can be viewed as a way to “unmix” caregivers regarding the incidence and combination of financial and psychological stressors they experienced (Hagenaars & McCutcheon, 2002). LCA is similar to cluster analysis but can incorporate dichotomous indicators and can assign observations to classes based on probability of class assignment. To identify the “optimal” number of distinct classes in the mixture, we used a combination of relative entropy (where values closer to 1 indicate high probability or certainty of assignment to a particular class) and where meaningful labels ascribed to the classes depict latent stress levels of the caregivers assigned to each class. For the main predictor and covariates in the LCA, we compared the likelihood of assignment to one latent class over another. For these analyses, we present AOR and 95% CIs. We conducted LCA using Mplus Version 6 (Muthén & Muthén, 2010) and incorporated child population weights.
Results
In 2010, an estimated 302,598 children in Ohio 0 to 17 years of age met the definition of having a disability, representing 12.3% of all children (Table 1). Compared to typically developing children, those with a disability were disproportionately older, male, covered by Medicaid insurance, and had lower health status (all p<0.001). Caregivers of children with disability tended to be disproportionately single or divorced, had less than a high school education, and were more likely to have income less than the FPL (less than $22,050 for a family of 4 in 2009) compared to caregivers of typically developing children (all p<0.05).
Table 1. Ohio Child and Caregiver Characteristics (2010), Overall and by Child Disability Status.
| Overall | Typically Developing Child | Child with Disability | |||
|---|---|---|---|---|---|
|
|
|||||
| Number of Children Surveyed | 1,824 | 1,614 | 210 | ||
| Weighted Number Representative of Ohio Child Population | 2,467,198 | 2,164,600 | 302,598 | ||
|
| |||||
| Child Characteristics | Category | Categorical Weighted Percentage | p-value | ||
| Age | 0-5 | 30.4 | 32.4 | 16.0 | <0.001 |
| 6-12 | 37.9 | 36.7 | 46.6 | ||
| 13-17 | 31.7 | 30.9 | 37.5 | ||
|
| |||||
| Gender | Male | 53.0 | 51.2 | 65.0 | 0.001 |
| Female | 47.0 | 48.8 | 35.0 | ||
|
| |||||
| Race/Ethnicity | White (non-Hispanic) | 75.8 | 76.2 | 72.9 | 0.255 |
| Black (non-Hispanic) | 16.1 | 15.9 | 17.9 | ||
| Hispanic | 5.4 | 5.0 | 7.8 | ||
| Other | 2.7 | 2.9 | 1.4 | ||
|
| |||||
| Health Insurance | Job-Based | 49.3 | 51.5 | 33.9 | <0.001 |
| Medicaid | 39.7 | 36.7 | 61.3 | ||
| Other | 6.4 | 6.8 | 3.2 | ||
| Uninsured | 4.6 | 5.0 | 1.6 | ||
|
| |||||
| Parent-Reported Health Status | Excellent | 57.2 | 61.4 | 27.8 | <0.001 |
| Very Good | 29.2 | 28.2 | 36.5 | ||
| Good / Fair / Poor | 13.5 | 10.4 | 35.7 | ||
|
| |||||
| Caregiver Characteristics | Category | Categorical Percentage | p-value | ||
|
| |||||
| Age | 18-24 | 7.8 | 8.0 | 6.7 | 0.9365 |
| 25-34 | 26.7 | 26.8 | 26.3 | ||
| 35-44 | 36.3 | 36.3 | 36.0 | ||
| 45 and over | 29.1 | 28.9 | 30.9 | ||
|
| |||||
| Marital Status | Married | 67.6 | 69.1 | 56.9 | 0.016 |
| Single | 14.0 | 13.5 | 17.9 | ||
| Divorced/Separated/Widowed | 18.4 | 17.4 | 25.2 | ||
|
| |||||
| Education Status | Less than High School | 8.9 | 8.1 | 14.8 | 0.033 |
| High School or equivalent | 30.2 | 30.1 | 31.1 | ||
| Some College or higher degree | 60.9 | 61.8 | 54.1 | ||
|
| |||||
| Poverty Level (% FPL) |
< 100% | 32.3 | 30.3 | 46.4 | 0.001 |
| 101% - 200% | 21.2 | 21.3 | 20.5 | ||
| 201% - 300% | 27.4 | 17.1 | 6.4 | ||
| > 300% | 19.2 | 31.2 | 26.7 | ||
Abbreviation: FPL – Federal Poverty Level
Source: 2010 Ohio Family Health Survey
Table 2 shows that with the exception of having incurred large credit card debt or loan, or having to declare bankruptcy, a higher percentage of caregivers for children with disability experienced all other financial and psychological stressors than parents caring for typically developing children (all p<0.05). Individual Kessler-6 psychological stressors were aggregated to identify that approximately one in five caregivers (21.3%) for children with disability had serious psychological distress, a significantly higher percentage than caregivers for typically developing children (9.3%; p<0.01).
Table 2. Percentage of Ohio Caregivers Experiencing Financial and Psychological Stressors in 2010, Overall and by Child Disability Status.
| Percentage Experiencing Stressor | |||
|---|---|---|---|
|
|
|||
| Caring for a… | |||
|
|
|||
| Overall | Typically Developing Child | Child with Disability | |
| Financial Stressors (in the past 12 months …) | |||
|
| |||
| Problems paying or unable to pay for medical bills (if yes …) | 36.9 x | 35.2 | 48.7 |
| … Unable to pay for basic necessities | 14.5 x | 12.6 | 27.8 |
| … Used up most of personal savings | 23.5 x | 21.8 | 35.2 |
| … Incurred large credit card debt or loan | 10.7 | 10.4 | 12.9 |
| … Had to declare bankruptcy | 5.0 | 4.8 | 6.8 |
| Problems paying rent, mortgage, or utility bill (if yes …) | 29.3 x | 27.1 | 44.4 |
| … Received financial help to pay for rent/mortgage/utility bill | 9.5 x | 8.5 | 16.2 |
| … Children moved in with others due to inability to pay bills | 5.8 y | 5.2 | 10.1 |
| Savings will cover expenses for at least 6 months | 24.3 x | 25.6 | 15.1 |
|
| |||
| Psychological Stressors (In the last 30 days felt this way all or most of the time …) | |||
|
| |||
| Sad | 7.8 x | 6.8 | 14.7 |
| Nervous | 9.1 x | 8.1 | 16.4 |
| Restless or fidgety | 11.1 x | 9.3 | 23.7 |
| Hopeless | 6.1 x | 5.4 | 10.9 |
| Everything is an effort | 16.5 x | 15.6 | 23.0 |
| Worthless | 3.8 x | 3.2 | 7.4 |
|
|
|||
| Serious Psychological Distress (Kessler-6 composite score >12) | 10.7x | 9.2 | 21.3 |
Notes:
= difference between percentage of caregivers experiencing stressor significant at α < 0.01
= difference between percentage of caregivers experiencing stressor significant at α < 0.05
Source: 2010 Ohio Family Health Survey
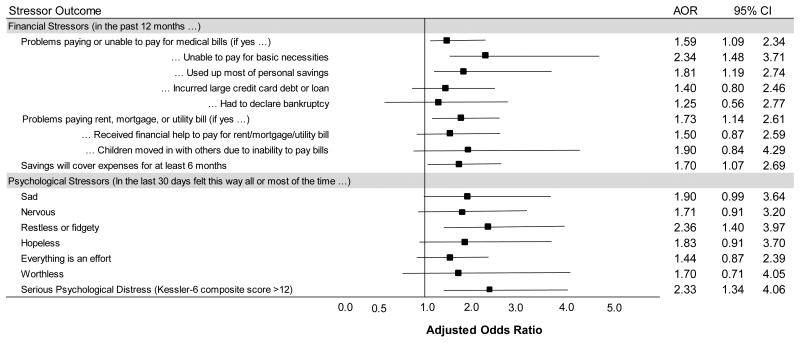
When adjusting for child and caregiver characteristics, caregivers for children with disability still had a higher likelihood of experiencing most types of financial stress compared with caregivers for typically developing children (Figure 1). For psychological stressors, the only difference in an individual category was that caregivers for children with disability experienced an adjusted higher likelihood of feeling restless or fidgety most of the time compared to caregivers for typically developing children (AOR: 2.4; 95% CI: 1.4 - 4.0). However, based on responses to all Kessler-6 manifest stressors, we found caregivers for children with disability 2.3 times (95% CI: 1.3 - 4.1) as likely to have serious psychological distress compared to caregivers for typically developing children.
Figure 1. Adjusted Odds of Experiencing Financial and Psychological Stressors When Caring for a Child with Disability Compared to a Typically Developing Child in Ohio (2010).
Notes: Odds Ratios adjusted (AOR) for child age, gender, race, insurance status and caregiver age, education and marital status.
Abbreviations: AOR = Adjusted Odds Ratio, CI = Confidence Interval
Source: 2010 Ohio Family Health Survey
Based on patterns of responses to stressors and underlying child and caregiver characteristics, we chose a model with three latent classes (Table 3). The LCA model converged to produce global maximum likelihood estimates and fit indices that support a well-fit model with a relative entropy value of 0.935 and latent class labels that are meaningful. The model assigned approximately one in ten (10.2%) caregivers to Latent Class 1. We characterized caregivers in this class as being more likely to have had a higher than average experience with most indicators of stress, especially psychological stressors (Financial and Psychological Stress). The model assigned one out of four (24.9%) caregivers to Latent Class 2 and a greater than average proportion of caregivers assigned to this latent class indicated experiencing financial stressors (Financial Stress). The model assigned the remaining two out of three caregivers (64.9%) to Latent Class 3 where experiencing stress was much lower than average across all stressors (Low Stress).
Table 3. Percent of Ohio Caregivers Responding Yes to Stressors (2010), Overall and by Latent Class Assignment.
| Latent Class Stress Category |
||||
|---|---|---|---|---|
|
|
||||
| Overall | Financial and Psychological | Financial Alone | Low Stress | |
|
|
||||
| Percentage of Caregivers Assigned to Latent Class | 100% | 10.2% | 24.9% | 64.9% |
| Financial Stressors (in the past 12 months …) | ||||
|
| ||||
| Problems paying or unable to pay for medical bills (if yes …) | 37.0 | 67.0 | 100.0 | 7.5 |
| … Unable to pay for basic necessities | 14.5 | 42.2 | 40.2 | 0.0 |
| … Used up most of personal savings | 23.5 | 49.7 | 73.1 | 0.0 |
| … Incurred large credit card debt or loan | 10.7 | 19.0 | 34.6 | 0.0 |
| … Had to declare bankruptcy | 5.0 | 13.3 | 14.6 | 0.0 |
| Problems paying rent, mortgage, or utility bill (if yes …) | 29.3 | 66.1 | 53.7 | 13.8 |
| … Received financial help to pay for rent/mortgage/utility bill | 9.5 | 20.9 | 16.9 | 4.7 |
| … Children moved in with others due to inability to pay bills | 5.8 | 24.7 | 7.7 | 2.1 |
| Savings will cover expenses for at least 6 months | 24.3 | 8.3 | 10.5 | 32.3 |
|
| ||||
| Psychological Stressors (In the last 30 days felt this way all or most of the time …) | ||||
|
| ||||
| Sad | 7.8 | 60.4 | 1.3 | 1.9 |
| Nervous | 9.1 | 69.1 | 3.4 | 1.7 |
| Restless or fidgety | 11.1 | 71.7 | 8.0 | 2.7 |
| Hopeless | 6.1 | 52.1 | 2.9 | 0.0 |
| Everything is an effort | 16.5 | 74.5 | 14.4 | 8.1 |
| Worthless | 3.8 | 35.6 | 0.2 | 0.0 |
Source: 2010 Ohio Family Health Survey
There is an association between caring for a child with disability and the assigned latent class of the caregiver (Table 4). We found caregivers of children with disability 3.4 times (95% CI: 1.8 - 6.7) as likely assigned to the Financial and Psychological Stress over the Low Stress latent class compared to caregivers of typically developing children. Also, caregivers of children with disability are 2.0 times (95% CI: 1.2 - 3.2) as likely assigned to the Financial Stress over the Low Stress latent class compared to caregivers of typically developing children.
Table 4. Adjusted Odds of Latent Class Assignment by 2010 Ohio Child and Caregiver Characteristics.
| Latent Class Stress Category Comparison | ||||
|---|---|---|---|---|
|
|
||||
| Characteristic | Category | Financial and Psychological vs Financial Alone | Financial and Psychological vs Low Stress | Financial Alone vs Low Stress |
| Caring for a Child with Disability | No (REF) | |||
| Yes | 1.73 (0.84, 3.55) | 3.41 (1.75, 6.66) | 1.98 (1.23, 3.19) | |
|
| ||||
| Child's Age | 0-5 (REF) | |||
| 6-12 | 1.17 (0.60, 2.29) | 0.96 (0.51, 1.79) | 0.81 (0.54, 1.23) | |
| 13-17 | 0.86 (0.41, 1.82) | 0.89 (0.43, 1.80) | 1.03 (0.67, 1.58) | |
|
| ||||
| Child's Gender | Male (REF) | |||
| Female | 0.94 (0.55, 1.63) | 0.93 (0.56, 1.54) | 0.98 (0.72, 1.35) | |
|
| ||||
| Race / Ethnicity | White (REF) | |||
| Black | 0.87 (0.40, 1.92) | 0.76 (0.36, 1.58) | 0.87 (0.53, 1.44) | |
| Hispanic | 0.87 (0.25, 3.03) | 0.48 (0.17, 1.39) | 0.56 (0.26, 1.19) | |
| Other | -- | -- | 0.20 (0.04, 1.02) | |
|
| ||||
| Insurance Status | Job-Based (REF) | |||
| Medicaid | 1.51 (0.63, 3.67) | 2.18 (0.97, 4.90) | 1.44 (0.94, 2.19) | |
| Other | 2.53 (0.90, 7.18) | 2.82 (1.09, 7.30) | 1.11 (0.65, 1.92) | |
| Uninsured | 2.87 (0.87, 9.45) | 9.27 (3.05, 28.23) | 3.23 (1.51, 6.92) | |
|
| ||||
| Caregiver's Age | 18-24 (REF) | |||
| 25-34 | 1.10 (0.30, 3.96) | 1.47 (0.44, 4.89) | 1.34 (0.66, 2.69) | |
| 35-44 | 1.80 (0.51, 6.30) | 3.35 (1.05, 10.73) | 1.86 (0.91, 3.79) | |
| 45 or more | 1.76 (0.49, 6.24) | 2.94 (0.92, 9.45) | 1.68 (0.80, 3.53) | |
|
| ||||
| Caregiver's Education | < High School (REF) | |||
| High School or GED | 0.60 (0.23, 1.55) | 1.70 (0.76, 3.79) | 2.82 (1.41, 5.64) | |
| At least some college | 0.53 (0.21, 1.33) | 1.33 (0.61, 2.90) | 2.49 (1.24, 4.98) | |
|
| ||||
| Caregiver's Marital Status | Married/Cohabitating (REF) | |||
| Single | 2.42 (0.98, 5.99) | 1.73 (0.76, 3.79) | 0.72 (0.40, 1.29) | |
| Divorced/Separated | 1.02 (0.52, 2.01) | 1.57 (0.85, 2.91) | 1.54 (1.02, 2.32) | |
|
| ||||
| Poverty Level (% FPL) | <100% (REF) | |||
| 101 – 200% | 0.28 (0.14, 0.56) | 0.50 (0.25, 0.98) | 1.83 (1.18, 2.84) | |
| 201 – 300% | 0.22 (0.08, 0.61) | 0.18 (0.07, 0.46) | 0.81 (0.48, 1.36) | |
| 301% or more | 0.28 (0.09, 0.87) | 0.08 (0.03, 0.23) | 0.29 (0.17, 0.49) | |
Abbreviations: vs = versus, REF = reference category, GED = high school graduate equivalent degree, FPL = Federal Poverty Level
Source: 2010 Ohio Family Health Survey
Poverty level was the covariate most strongly associated with latent class assignment. We noted those with increasingly higher categories of household earning less likely assigned to higher stress latent classes compared to caregivers with incomes at, or lower than the FPL. This association is most apparent for caregivers assigned to the Financial and Psychological Stress over Low Stress latent class. We found those with earnings up to 200% of the FPL half as likely assigned to the Financial and Psychological Stress over Low Stress latent class (AOR: 0.50; 95% CI: 0.25 - 0.98) compared to caregivers with household earnings less than the FPL. Observing a trend, we saw caregivers earning more than 300% FPL less than 10% as likely assigned to the Financial and Psychological Stress over Low Stress latent class (AOR: 0.08; 95% CI: 0.03 - 0.23).
We also noted caregivers of children who were uninsured 3.2 times (95% CI: 1.5 – 6.9) as likely assigned to the Financial Stress latent class and 9.3 times (95% CI: 3.1 – 28.3) as likely assigned to the Financial and Psychological Stress over the Low Stress latent class compared to caregivers of children with job-based insurance.
Discussion
In this study we have identified three distinct subpopulations of caregivers based on the type of financial and psychological stress they experienced (Low, Financial, or Financial and Psychological) and child and household characteristics. Children with disability were twice as likely to reside with caregivers with high levels of financial stress and almost three and half times as likely to reside with caregivers with high levels of financial stress and very high levels of psychological stress, as typically developing children. We also found an association between having an uninsured child and low household poverty level with assignment to a higher stress latent class.
Using the theoretical associations depicted in the Family Stress Model, poor child health outcomes may be associated with children with disability (and their siblings) due to the financial and psychological stress incurred by their caregivers. Our findings are important for health care policymakers because children with disability are living longer and increasingly at home (Reichman, Corman, & Noonan, 2008). Reducing the stress associated with caring for a child with disability and improving the likelihood of optimal health care outcomes for the child with disability will require addressing factors on a system-wide level, such as universal access to timely, coordinated, and comprehensive care, and a healthy-caregiver, healthy-child pediatric health care system delivery philosophy.
We estimated from the 2009/10 National survey of CSHCN (NS-CSHCN) that less than one-third of Ohio children that meet our definition of disability receive care in a medical home (data not shown). Kuhlthau and colleagues (Kuhlthau et al., 2005) found finance-related problems were reduced when CSHCN received coordinated and ongoing comprehensive care in a medical home, had adequate private and/or public insurance, and had community-based service systems that were organized and easy to use. Many children with disability benefit from improved care coordination, which is also associated with reduced overall cost of care (Casey et al., 2011; Gordon et al., 2007; Liptak, Burns, Davidson, & McAnarney, 1998; Peter et al., 2011).
The comprehensive care needs of children with disability and their families' inability to meet or cope with these needs are also major factors contributing to high stress levels among caregivers (Strunk, 2010). There are a number of other system reforms that have been shown to be effective in reducing financial and psychological stress from caregiving. For example, caregivers of CSHCN do not receive needed mental health care services (Ganz & Tendulkar, 2006) despite our findings that they are at high risk for psychological distress. In addition, respite care is an important contribution that offers short breaks to families who care for children with multiple disabilities and appears to result in reductions in psychological distress in caregivers of children with developmental disabilities in particular (Mullins, Aniol, Boyd, Page, & Chaney, 2002). Regardless of the severity of the disability, caregiver's income level, or geographic location, respite is a needed support service for families of CSHCN (Doig, McLennan, & Urichuk, 2009; Macdonald & Callery, 2008; Nageswaran, 2009). Failure to pay attention to the growing need for improved systems of care, which includes respite care services, could lead to an increase in the disintegration of the family structure and an increase in preventable child health care costs for society (Neff, 2009).
Provisions of the Patient Protection and Affordable Care Act (ACA) of 2010 may eventually ensure continuous health insurance coverage for the vast majority of children and caregivers and help families alleviate the inability to pay medical bills and other necessities (Jeffrey & Newacheck, 2006). In addition, Section 2703 of the ACA created an optional benefit plan for State Medicaid programs to create Health Homes for patients with multiple chronic conditions. Health Homes will coordinate care across multiple providers and services, provide comprehensive care management for patients, and also include family support. The results of this study and findings that siblings in households with children with disability also experience disproportionate functional impairment problems (Goudie, Havercamp, Jamieson, & Sahr, 2013) underlie the need for family support. Under the rubric of family support, psychological and mental health screening can be a precursor for obtaining psychological treatment to alleviate stress.
There were limitations to this study. The adult proxy respondent for the child self-selected himself or herself as the best person in the family who had knowledge of the child's health insurance coverage. For single caregivers this is not an issue, but for married caregivers where one parent was in the workplace and was responsible for the child's job-based insurance, the survey may not have identified the primary caregiver. As such, the level of psychological stress associated with the primary caregiver for the child with disability may be under-estimated in our study. Also, the survey interviewer randomly selected one child to participate in the survey from households with more than one child. If the child selected was typically developing and there was also a child with disability in the household, the percentage of caregivers of children with typically developing children experiencing financial and psychological stressors may be over-estimated. In addition, we do not know what percentage of the caregivers of children with disability already have access to a desired care system that includes services such as respite care.
Only Ohio residents were eligible to participate in the survey. Shattuck and Parish found that out-of-pocket expenditures for families of CSHCN vary by state and out-of-pocket expenditures for Ohio were in the middle (3rd) of 5 quintiles (Shattuck & Parish, 2008). It is reasonable to assume that financial and psychological stress experiences of Ohio caregivers do not differ from the United States as a whole.
There is a need for future research to evaluate the potential benefits of an enhanced family-centered medical home that coordinates not only the health care of children with disability, but also the health (including mental health) care of caregivers and other household members. We see the creation of Health Homes as a potential transformative system change in this direction.
Acknowledgments
Anthony Goudie was supported by a grant from the Ohio State University Research Foundation, the Arkansas Biosciences Institute, and the University of Arkansas for Medical Sciences Translational Research Institute #UL1TR000039-04 and KL2TR000063.
Contributor Information
Anthony Goudie, Center for Applied Research and Evaluation, Department of Pediatrics, College of Medicine University of Arkansas for Medical Sciences.
Marie-Rachelle Narcisse, College of Education and Health Professions, University of Arkansas.
David E. Hall, Program for Children with Medically Complex Needs, Department of Pediatrics, Monroe Carell Jr Children's Hospital at Vanderbilt.
Dennis Z. Kuo, Center for Applied Research and Evaluation, Department of Pediatrics, College of Medicine, University of Arkansas for Medical Sciences.
References
- Anderson L, Larson S, Lakin C, Kwak N. Children with disabilities: social roles and family impacts in the NHIS DD Data Brief. Minneapolis, MN: University of Minnesota, Institute on Community Integration; 2002. [Google Scholar]
- Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Brehaut JC, Kohen DE, Garner RE, Miller AR, Lach LM, Klassen AF, Rosenbaum PL. Health among caregivers of children with health problems: findings from a Canadian population-based study. American Journal of Public Health. 2009;99(7):1254–1262. doi: 10.2105/AJPH.2007.129817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey PH, Lyle RE, Bird TM, Robbins JM, Kuo DZ, Brown C, Lal A, Tanios A, Burns K. Effect of hospital-based comprehensive care clinic on health costs for Medicaid-insured medically complex children. Archives of Pediatric and Adolescent Medicine. 2011;165(5):392–398. doi: 10.1001/archpediatrics.2011.5. [DOI] [PubMed] [Google Scholar]
- Cohen PN, Petrescu-Prahova M. Gendered Living Arrangements Among Children With Disabilities. Journal of Marriage and Family. 2006;68(3):630–638. [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Jr, Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Development. 1992;63(3):526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- Davidoff AJ. Insurance for children with special health care needs: patterns of coverage and burden on families to provide adequate insurance. Pediatrics. 2004;114(2):394–403. doi: 10.1542/peds.114.2.394. [DOI] [PubMed] [Google Scholar]
- Doig JL, McLennan JD, Urichuk L. ‘Jumping through hoops‘: parents' experiences with seeking respite care for children with special needs. Child: Care, Health and Development. 2009;35(2):234–242. doi: 10.1111/j.1365-2214.2008.00922.x. [DOI] [PubMed] [Google Scholar]
- Eisenhower AS, Baker BL, Blacher J. Children's delayed development and behavior problems: impact on mothers' perceived physical health across early childhood. Social Science and Medicine. 2009;68(1):89–99. doi: 10.1016/j.socscimed.2008.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson E. Mothers of children and adolescents with intellectual disability: social and economic situation, mental health status, and the self-assessed social and psychological impact of the child's difficulties. Journal of Intellectual and Disability Research. 2003;47(Pt 4-5):385–399. doi: 10.1046/j.1365-2788.2003.00498.x. [DOI] [PubMed] [Google Scholar]
- Ganz ML, Tendulkar SA. Mental health care services for children with special health care needs and their family members: prevalence and correlates of unmet needs. Pediatrics. 2006;117(6):2138–2148. doi: 10.1542/peds.2005-1531. [DOI] [PubMed] [Google Scholar]
- Gordon JB, Colby HH, Bartelt T, Jablonski D, Krauthoefer ML, Havens P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special health care needs. Archives of Pediatric and Adolescent Medicine. 2007;161(10):937–944. doi: 10.1001/archpedi.161.10.937. [DOI] [PubMed] [Google Scholar]
- Goudie A, Havercamp S, Jamieson B, Sahr T. Assessing functional impairment in siblings living with children with disability. Pediatrics. 2013;132:e476–e483. doi: 10.1542/peds.2013-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta VB. Comparison of Parenting Stress in Different Developmental Disabilities. Journal of Developmental and Physical Disabilities. 2007;19(4):417–425. [Google Scholar]
- Hagenaars JA, McCutcheon AL, editors. Applied latent class analysis. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- Hogan DP, Rogers ML, Msall ME. Functional limitations and key indicators of well-being in children with disability. Archives of Pediatric and Adolescent Medicine. 2000;154(10):1042–1048. doi: 10.1001/archpedi.154.10.1042. [DOI] [PubMed] [Google Scholar]
- ICF Macro. 2010 Ohio Family Health Survey Methodology Report. [Last accessed: April 25, 2013];2011 Available at http://grc.osu.edu/omas/datadownloads/ofhsoehspublicdatasets/index.cfm.
- Jeffrey AE, Newacheck PW. Role of insurance for children with special health care needs: a synthesis of the evidence. Pediatrics. 2006;118(4):e1027–1038. doi: 10.1542/peds.2005-2527. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Zaslavsky AM. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Gouin JP, Hantsoo L. Close relationships, inflammation, and health. Neuroscience and Biobehavioral Review. 2010;35(1):33–38. doi: 10.1016/j.neubiorev.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhlthau K, Hill KS, Yucel R, Perrin JM. Financial burden for families of children with special health care needs. Maternal and Child Health Journal. 2005;9(2):207–218. doi: 10.1007/s10995-005-4870-x. [DOI] [PubMed] [Google Scholar]
- Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Archives of Pediatric and Adolescent Medicine. 2011;165(11):1020–1026. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lach LM, Kohen DE, Garner RE, Brehaut JC, Miller AR, Klassen AF, Rosenbaum PL. The health and psychosocial functioning of caregivers of children with neurodevelopmental disorders. Disability and Rehabilitation Journal. 2009;31(9):741–752. doi: 10.1080/08916930802354948. [DOI] [PubMed] [Google Scholar]
- Liptak GS, Burns CM, Davidson PW, McAnarney ER. Effects of providing comprehensive ambulatory services to children with chronic conditions. Archives of Pediatric and Adolescent Medicine. 1998;152(10):1003–1008. doi: 10.1001/archpedi.152.10.1003. [DOI] [PubMed] [Google Scholar]
- Macdonald H, Callery P. Parenting children requiring complex care: a journey through time. Child: Care, Health and Development. 2008;34(2):207–213. doi: 10.1111/j.1365-2214.2007.00790.x. [DOI] [PubMed] [Google Scholar]
- Majnemer A, Shevell M, Law M, Poulin C, Rosenbaum P. Indicators of distress in families of children with cerebral palsy. Disability and Rehabilitation Journal. 2012;34(14):1202–1207. doi: 10.3109/09638288.2011.638035. [DOI] [PubMed] [Google Scholar]
- McCann D, Bull R, Winzenberg T. The daily patterns of time use for parents of children with complex needs: a systematic review. Journal of Child Health Care. 2012;16(1):26–52. doi: 10.1177/1367493511420186. [DOI] [PubMed] [Google Scholar]
- McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck PW, Perrin JM, Shonkoff JP, Strickland B. A new definition of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):137–140. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- Miodrag N, Hodapp RM. Chronic stress and health among parents of children with intellectual and developmental disabilities. Current Opinion in Psychiatry. 2010;23(5):407–411. doi: 10.1097/YCO.0b013e32833a8796. [DOI] [PubMed] [Google Scholar]
- Mullins LL, Aniol K, Boyd ML, Page MC, Chaney JM. The influence of respite care on psychological distress in parents of children with developmental disabilities: A longitudinal study. Children's Services: Social Policy, Research, and Practice. 2002;5(2):123–138. [Google Scholar]
- Muthén LK, Muthén BO. Mplus Users Guide. Sixth Edition. Los Angeles, CA: Muthén & Muthén; 1998-2010. [Google Scholar]
- Nageswaran S. Respite care for children with special health care needs. Archives of Pediatric and Adolescent Medicine. 2009;163(1):49–54. doi: 10.1001/archpediatrics.2008.504. [DOI] [PubMed] [Google Scholar]
- Neff JM. Respite care: an essential yet unmet need for families with children with special health care needs. Archives of Pediatric and Adolescent Medicine. 2009;163(1):89–90. doi: 10.1001/archpediatrics.2008.527. [DOI] [PubMed] [Google Scholar]
- Parish SL, Seltzer MM, Greenberg JS, Floyd F. Economic implications of caregiving at midlife: comparing parents with and without children who have developmental disabilities. American Journal of Mental Retardation. 2004;42(6):413–426. doi: 10.1352/0047-6765(2004)42<413:EIOCAM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Peter S, Chaney G, Zappia T, Van Veldhuisen C, Pereira S, Santamaria N. Care coordination for children with complex care needs significantly reduces hospital utilization. Journal for Specialists in Pediatric Nursing. 2011;16(4):305–312. doi: 10.1111/j.1744-6155.2011.00303.x. [DOI] [PubMed] [Google Scholar]
- Porterfield S. Work choices of mothers in families with children with disabilities. Journal of Marriage and Family. 2002;64:972–981. [Google Scholar]
- Reichman NE, Corman H, Noonan K. Impact of child disability on the family. Maternal and Child Health Journal. 2008;12(6):679–683. doi: 10.1007/s10995-007-0307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Parish SL. Financial burden in families of children with special health care needs: variability among states. Pediatrics. 2008;122(1):13–18. doi: 10.1542/peds.2006-3308. [DOI] [PubMed] [Google Scholar]
- Strunk J. Respite care for families of special health care needs children: A systematic review. Journal of Developmental and Physical Disabilities. 2010;22(6):615–630. [Google Scholar]
- van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Archives of Pediatric and Adolescent Medicine. 2004;158(9):884–890. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]