Abstract
Background
Qualitative data suggest that pruritus is a burdensome symptom in patients with epidermolysis bullosa (EB), but the prevalence of pruritus in children and adults with EB, as well as factors that contribute to pruritus are unknown.
Objective
To quantitatively identify and to characterize pruritus experienced by EB patients using a comprehensive online questionnaire.
Methods
A questionnaire was developed to evaluate pruritus in all ages and types of EB. Questions that characterize pruritus were included, and factors that aggravate symptoms were investigated. Patients from seven North American EB centers were invited to participate.
Results
A total of 146 out of 216 questionnaires were completed (response rate=68%) (73 males, 73 females; median age, 20.0). Using a 5-point Likert scale (1=never, 2=rarely, 3=sometimes, 4=often, 5=always), itchiness was the most bothersome EB complication (mean=3.3). The average daily frequency of pruritus increased with self-reported EB severity. Pruritus was most frequent at bedtime (mean=3.8) and interfered with sleep. Factors that aggravated pruritus included healing wounds, dry skin, infected wounds, stress, heat, dryness, and humidity.
Conclusions
Pruritus is common in EB patients and can be very bothersome. Future studies will need to investigate the most effective treatments given to EB patients for pruritus.
Keywords: Pruritus, itch, pain, epidermolysis bullosa, recessive dystrophic epidermolysis bullosa, dominant dystrophic epidermolysis bullosa, junctional epidermolysis bullosa, epidermolysis bullosa simplex
Introduction
Epidermolysis bullosa (EB) is a group of rare, inherited skin disorders characterized by fragile skin and the development of blisters after minor mechanical trauma. Three major inherited types of EB include dystrophic EB (DEB), junctional EB (JEB), and EB simplex (EBS). DEB is further classified into dominant dystrophic EB (DDEB) and recessive dystrophic EB (RDEB). Each of these types of EB has a different genetic profile, presentation, clinical course, and severity.1
Patients with EB can be confronted with many chronic and complex problems.1–3 Qualitative interviews with eleven children with EB suggested that pruritus can be very bothersome.4 The children described an unbearable, continuous itch, which was not only physically troublesome but also a psychological burden.4 While pruritus is commonly described in dermatological conditions, studies have not evaluated its prevalence among children and adults with EB.5–8 Scratching in EB can irritate and tear already fragile skin, worsen existing wounds, and create new blisters. The objective of this study was to quantify and characterize pruritus experienced by EB patients of all ages and types using a comprehensive online questionnaire. The impact of pruritus on quality of life, as well as factors that aggravate or alleviate symptoms were also investigated.
Methods
Patient Selection
The Epidermolysis Bullosa Clinical Research Consortium (EBCRC) was formed to create a North American database for the clinical characterization of EB. EB patients who presented to an EBCRC center were given the opportunity to enroll in a longitudinal database. Approval for the EBCRC was obtained by the Institutional Review Board at each participating institution. All patients enrolled in the EBCRC and, as appropriate, their parents, signed written informed assent/consent to be contacted for future studies.
The pruritus study protocol was approved by the Institutional Review Board at the Stanford University School of Medicine. Informed consent/assent for participation in the questionnaire was obtained from all participants.
EB patients from seven EBCRC centers were invited to participate in this questionnaire (N = 145). EB patients not enrolled in the EBCRC but who previously had requested to be contacted for participation in research studies were also sent an invitation (N=51). Information about the study was available on the Stanford University EB website.9 An additional 20 EB patients contacted us expressing interest in the questionnaire and were sent an invitation. All participation was voluntary, and English-speaking patients of any age with a diagnosis of EB were included. The questionnaire was available for completion for ten weeks.
Study Protocol
The questionnaire was created and data was collected and stored using the Research Electronic Data Capture application (REDCap) hosted at the Stanford Center for Clinical Informatics (Stanford, CA). REDCap is a secure, web-based application designed to support data capture for research studies.10 A link to the questionnaire was sent via e-mail to participants. Participants without access to email had the option to complete the questionnaire by phone. Patients 12 years or older were asked to complete the questionnaire alone. Patients younger than 12 years old either completed the questionnaire with a caregiver, or the caregiver completed the questionnaire on their behalf. Reminder emails were sent to participants who did not respond. Attempts were made to call all participants who did not respond in order to confirm email addresses and receipt of the questionnaire.
Questionnaire
The questionnaire was developed based on previously validated pruritus survey instruments.11–13 Additional questions were included based on clinical experience with EB patients (Supplement I).
The questionnaire included items about demographics; EB diagnosis and self-reported EB severity; frequency and timing of pruritus; location of pruritus and wounds; effect of wound type on pruritus; effect of pruritus on sleep, daily activities, and mood; sensory descriptors; and effect of pruritus on skin. Responses to frequency-type questions were ranked on a 5-point Likert scale (1=never, 2=rarely, 3=sometimes, 4=often, 5=always). Patients were also asked to rate how much they were bothered by itching in addition to 12 other complications of EB using a 5-point Likert scale (1=not bothersome, 2=a little bothersome, 3=somewhat bothersome, 4=very bothersome, 5=most bothersome). Options to include additional comments were provided throughout the questionnaire. Participants were asked to allow at least 30 minutes for questionnaire completion. Response to each question was not mandatory.
Statistical Analysis
Descriptive statistics, including percentages of total responses and sub-group analyses, were calculated. Overall scores consisting of the averages of responses based on the 5-point Likert scale were tabulated and were fitted into a generalized linear model with multinomial distribution. All tests were two-sided, and statistical significance was set at P < 0.05 for all analyses. Analyses were conducted using statistical software (SAS, Version 9.3, SAS Institute Inc, Cary, NC).
Results
Demographics
Of the 216 questionnaires sent, 146 questionnaires were completed and included in survey analysis (response rate=68%). Demographics and distribution by EB type are shown in Table I. There were 73 male and 73 female patients with an average age of 22.3 years (median, 20.0; range, 0–67 years) (Table I). Self-described EB disease severity is shown in Table II. RDEB and JEB had the highest percentage of patients with severe disease.
Table I.
Subject Demographics
| Patients (N=146) |
|
|---|---|
| Participant-no. (%) | |
| Patient | 90 (61.6) |
| Caregiver for Patient | 36 (24.7) |
| Patient with Caregiver | 20 (13.7) |
| Male-no. (%) | 73 (50.0) |
| Female-no. (%) | 73 (50.0) |
| Age of Patients | |
| Mean, years (range) | 22.3 (0–67) |
| EB Type and Subtype | |
| Dystrophic EB | 97 (66.4) |
| Recessive | 77 (79.4) |
| Dominant | 14 (14.4) |
| Unknown | 6 (6.2) |
| Junctional EB | 14 (9.6) |
| Non-Herlitz | 8 (57.1) |
| Unknown | 6 (42.9) |
| EB Simplex | 31 (21.2) |
| Dowling-Meara | 7 (22.6) |
| Weber-Cockayne | 8 (25.8) |
| Unknown | 16 (51.6) |
| Unknown | 4 (2.7) |
EB, Epidermolysis bullosa
Table II.
Self-Reported Epidermolysis Bullosa Disease Severity
| EB Disease Severity-no. (%)1 | |||
|---|---|---|---|
| Mild | Moderate | Severe | |
| All EB Patients | 38 (26.2) | 69 (47.6) | 38 (26.2) |
| Recessive Dystrophic | 8 (10.4) | 40 (51.9) | 29 (37.7) |
| Dominant Dystrophic | 8 (57.1) | 4 (28.6) | 2 (14.3) |
| Unknown Dystrophic | 2 (33.3) | 3 (50.0) | 1 (16.7) |
| Junctional | 0 (0) | 9 (64.3) | 5 (35.7) |
| EB Simplex | 17 (56.7) | 12 (40.0) | 1 (3.3) |
| Unknown | 3 (75.0) | 1 (25.0) | 0 (0) |
EB, Epidermolysis bullosa
One missing response
Pruritus and Other EB Complications
Participants rated itchiness as the most bothersome EB complication (Table III). When grouped by EB diagnosis, itchiness remained the most bothersome problem for patients with RDEB (mean=3.5), DDEB (mean=3.1), and EBS (mean=2.7). Patients with JEB rated acute pain (mean=3.9) and chronic pain (mean=3.6) as more bothersome than itchiness (mean=3.5). The rating for itchiness was not significantly different among EB types.
Table III.
Epidermolysis Bullosa Complications
| 5-point Likert Average (SD)1 |
|
|---|---|
| How much do the following bother you? | |
| Itchiness | 3.3 (1.1) |
| Acute Pain (e.g. dressing changes, going to the bathroom) | 2.9 (1.3) |
| Chronic Pain (wounds present for over a year) | 2.7 (1.5) |
| Problems Eating (e.g. strictures, mouth ulcers) | 2.7 (1.4) |
| Stomach Problems (e.g. G-tube, heartburn, constipation) | 2.6 (1.4) |
| Dental Problems | 2.6 (1.4) |
| Movement (e.g. hand function) | 2.5 (1.4) |
| Wound Infections | 2.4 (1.2) |
| Feeling Tired (Anemia) | 2.4 (1.4) |
| Surgeries | 2.4 (1.4) |
| Eye Problems (e.g. corneal abrasions) | 2.2 (1.5) |
| Depression/Mood/ Sadness | 2.2 (1.3) |
| Going to the Doctor | 2.1 (1.2) |
1=Not bothersome, 2=A little bothersome, 3=Somewhat bothersome, 4=Very bothersome, 5=Most bothersome
Frequency and Intensity of Pruritus
The daily itch frequency grouped by EB type, severity, and patient age is shown in Table IV. Using the 5-point Likert scale, the average daily itch frequency for all patients was 3.7, between “sometimes” and “often” itchy. Patients with RDEB reported the highest average itch frequency (mean=3.9), which was significantly higher than patients with EBS (p=0.01). Average itch frequency increased with self-reported EB severity (Table IV).
Table IV.
Pruritus Frequency and Daily Occurrence
| 5-Point Likert Average (SD)1 |
|
|---|---|
| On average, how often do you itch per day? | |
| All EB Patients | 3.7 (1.0) |
| By Diagnosis | |
| Recessive Dystrophic | 3.9 (0.8) |
| Dominant Dystrophic | 3.5 (1.2) |
| Junctional | 3.6 (0.8) |
| EB Simplex | 3.1 (1.0) |
| Unknown | 3.3 (1.0) |
| By EB Severity | |
| Mild EB Severity | 3.2 (1.0) |
| Moderate EB Severity | 3.8 (0.9) |
| Severe EB Severity | 4.0 (0.8) |
| By Age Group | |
| 0–9 Years | 3.6 (0.8) |
| 10–19 Years | 3.8 (0.9) |
| 20–29 Years | 3.8 (0.8) |
| 30+ Years | 3.5 (1.2) |
| How often do you itch during the following times of day? | |
| Morning | 3.0 (1.1) |
| Afternoon | 3.1 (0.9) |
| Evening | 3.4 (1.1) |
| Bedtime | 3.8 (1.2) |
EB, Epidermolysis bullosa
1=Never, 2=Rarely, 3=Sometimes, 4=Often, 5=Always
Daily Occurrence
The average itch frequency increased as the day progressed (Table IV). Patients with RDEB (mean=4.0) and JEB (mean=4.1) had the highest average itch frequency at bedtime. Average itch frequency at bedtime for DDEB and EBS was 3.4 and 3.6, respectively.
Sites of Pruritus and Wounds
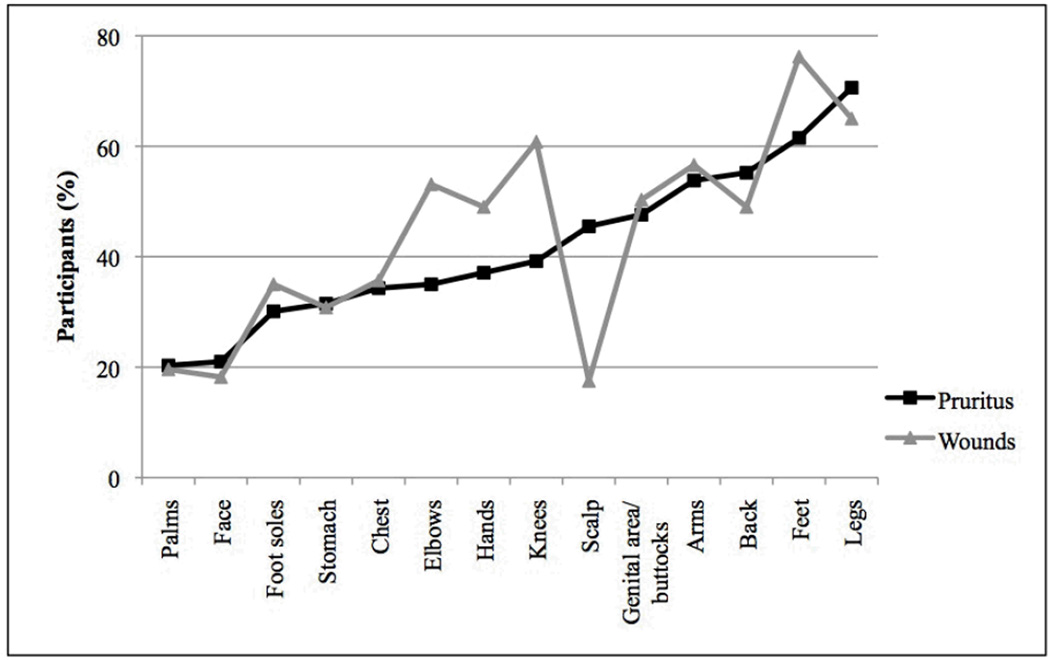
The percentage of patients with pruritus and wounds at each body site is shown in Figure 1. EB patients that identified three or more different wound locations had a significantly higher frequency of pruritus than patients with less than three wounds (P<0.001).
Figure 1. Sites of Pruritus and Wounds.
Epidermolysis Bullosa and sites of pruritus and wounds. Y-axis refers to the percentage of participants. Black line represents sites of pruritus. Gray line represents sites of wounds.
Wound type and Pruritus
Healing wounds were the itchiest of the types of wounds surveyed (mean=4.1). (Table V). Healing wounds (p<0.001), skin around wounds (p<0.001), dry skin (p=0.001), and infected wounds (p=0.002) were affected by pruritus significantly more than non-wounded skin.
Table V.
Wound Type and Pruritus
| 5-Point Likert Average (SD)1 |
P value2 | |
|---|---|---|
| How itchy are the following wounds? | ||
| Healing wounds | 4.1 (0.9) | <0.001* |
| Skin around wounds | 3.6 (1.1) | <0.001* |
| Dry skin | 3.4 (1.2) | 0.001* |
| Infected wounds | 3.3 (1.3) | 0.002* |
| New wounds | 2.9 (1.1) | 0.18 |
| Chronic wounds (present for over one year) | 2.9 (1.4) | 0.16 |
| Non-wounded skin | 2.6 (1.1) | ------ |
| Scars | 2.5 (1.2) | 0.62 |
1=Never, 2=Rarely, 3=Sometimes, 4=Often, 5=Always
In comparison to non-wounded skin
P value is significant at <0.05
Effect of Pruritus on Skin
Patients reported that itch was worse when thinking about it (mean=3.3). Scratching “sometimes” to “often” felt good (mean=3.7) and relieved pruritus (mean=3.3), although it resulted in skin looking red (mean=3.7) and bleeding (mean=3.3).
Sensory and Mood Descriptors
Patients most commonly described pain accompanying with pruritus (mean=3.1). The average frequencies of other sensory descriptors of pruritus and the effects of pruritus on mood are shown in Table VI.
Table VI.
Mood and Sensory Descriptors
| 5-Point Likert Average (SD)1 |
|
|---|---|
| Has your itch caused you to have any of the following feelings? | |
| Agitation (annoyed) | 3.2 (1.2) |
| Feeling like you cannot control the itch | 3.1 (1.3) |
| Frustration | 3.1 (1.4) |
| Anxiety (worried, afraid) | 2.2 (1.3) |
| Decreased self-esteem (feeling bad about yourself) | 2.0 (1.2) |
| Depression | 1.9 (1.1) |
| Do you have these feelings when you are itching? | |
| Pain | 3.1 (1.2) |
| Too deep to scratch | 2.9 (1.3) |
| Stinging | 2.7 (1.2) |
| Burning | 2.7 (1.2) |
| Crawling ants | 2.4 (1.2) |
| Heat sensation | 2.3 (1.2) |
| Tickling | 2.2 (1.2) |
| Sweating | 2.2 (1.2) |
| Stabbing | 1.9 (1.1) |
| Headache | 1.4 (0.7) |
| Cold sensation | 1.4 (0.7) |
1=Never, 2=Rarely, 3=Sometimes, 4=Often, 5=Always
Pruritus and Sleep
Pruritus “sometimes” to “often” interfered with sleep (mean=3.1). Participants reported scratching while sleeping (mean=3.4); experiencing difficulty falling asleep; (mean=2.9), and waking up from the pruritus (mean=2.8).
Effect on Daily Activities
Eighty-seven percent of participants reported itching when not active. Forty-nine participants responded that certain activities worsened the pruritus including bandage changes (65.3%), showers/baths (44.9%), doctor appointments (28.6%), homework (28.6%), and painful bowel movements (16.3%). Sweat and stress increased pruritus in 63.7% and 62.5% of patients, respectively (Table VII).
Table VII.
External Factors and Itch
| No. (%)1 | |||
|---|---|---|---|
| Relieves Itch |
No Change | Increases Itch |
|
| How do the following affect your itch? | |||
| Activity | 54 (37.8) | 50 (35.0) | 39 (27.3) |
| Sweat | 11 (7.5) | 42 (28.8) | 93 (63.7) |
| Stress | 2 (1.4) | 52 (36.1) | 90 (62.5) |
| Dryness | 8 (5.5) | 27 (18.6) | 110 (75.9) |
| Heat | 16 (11.1) | 35 (24.1) | 94 (64.8) |
| Humidity | 28 (19.6) | 40 (28.0) | 75 (52.5) |
| Cold | 64 (43.8) | 49 (33.6) | 33 (22.6) |
Not all participants responded to all questions
Pruritus “rarely” to “sometimes” interfered with wearing certain clothes (mean=2.5), work/school (mean=2.5), ability to concentrate on work/tests (mean=2.4), and having fun with friends (mean=2.3). Pruritus “never” to “rarely” interfered with eating (mean=1.9).
Pruritus and Climate
Participants indicated that dryness (75.9%), heat (64.8%), and humidity (52.5%) increased pruritus. Cold weather relieved pruritus in 43.8% of patients and increased it in 22.6% (Table VII).
Discussion
Our results quantitatively demonstrate that pruritus is common in EB patients and can be very bothersome. To our knowledge, no other study has comprehensively investigated and characterized pruritus in children and adults with EB.
Pruritus frequency increased with EB severity. These results suggest a relationship between EB wounds and pruritus. In burn patients, pruritus has been shown to increase with total body surface area of burns and to occur most commonly in the proliferative and remodeling stages of wound healing.14–17 Similarly, patients with RDEB, a severe form of EB with widespread skin involvement, had a statistically significant higher frequency of pruritus than patients with EBS, a generally milder subtype, and healing wounds were identified as the itchiest type of wound in EB patients.18
Dry skin was also more pruritic than non-wounded skin, a relationship also prevalent in burn patients.14 Although the mechanism is unclear, a disruption in the epidermal barrier in dry skin may facilitate the entry of irritants and itch-causing agents.19 Certain weather conditions including dryness, heat, and humidity may also exacerbate itch by decreasing the hydration of skin. These weather conditions are known to exacerbate pruritus in atopic dermatitis and psoriasis.7, 20 These results highlight the importance of preventing and treating dry skin in EB patients.
Pruritus was more common at bedtime, an observation that has been noted in other dermatologic conditions.6, 21, 22 Although the underlying mechanism responsible for nocturnal pruritus is unclear, several different mechanisms may contribute to increased pruritus at bedtime including circadian rhythms related to skin temperature.19, 23 Heat or an increase in skin temperature during the evening may increase pruritus experienced by patients. Circadian rhythms involving the hypothalamus-pituitary axis, autonomic nervous system, and cytokines have also been proposed to contribute to nocturnal pruritus.19, 24, 25 Psychological components including lack of external stimuli and decreased activity at bedtime may also increase awareness of pruritus.19 Accordingly, 87% of EB patients reported itching when not active, which may have a similar psychological mechanism.
While activity relieved pruritus in 54 (37.8%) patients, certain activities such as bandage changes and showers/baths increased pruritus in some respondents. These activities can be very stressful for patients due to anticipated pain. Given that stress increased pruritus in 62.5% of patients, the use of anxiolytics prior to these activities may help to control pruritus by decreasing stress from such activities.
The location of pruritus tended to coincide with wound location. Variations in the percentage of participants with pruritus at each site as presented in Figure 1 may be explained by the accessibility of the site for scratching. This topographical information may allow patients and caregivers to be more cautious of wounds in these regions.
Pruritus can induce a vicious itch-scratch-blister cycle in EB patients, which can irritate skin, worsen existing wounds, and create new blisters.2 Some patients have learned to be cognizant of this cycle. One patient who reported improved pruritus with age attributed the improvement to “self-control and better awareness of what the ramifications are if I scratch an area too much.” Another patient said it was due to “realizing it’s bad to rub.” These comments suggest that itch may not decrease over time but rather patients learn to develop better self-control in tolerating pruritus.
Limitations of this study include that all findings were based on self-reports and that the questionnaire was not validated. In order to gather information from all ages, caregivers were asked to either help the patient complete the questionnaire or to complete the questionnaire on behalf of the patient. Although some responses did not come from a primary source, caregivers often spend extensive time managing EB patients and are aware of the problems these patients experience. Given that caregivers may not be able to appropriately answer all questions, response to all questions was not mandatory.
The results of this study indicate that pruritus is problematic in EB patients and inadequately controlled. Future studies will need to investigate the most effective treatments given to EB patients for pruritus. An evaluation of these therapies in randomized controlled trials will be necessary in order to develop evidence-based recommendations for treatment of pruritus in EB.
Supplementary Material
Acknowledgements
We would like to thank the Agnes Varis Charitable Trust, the Epidermolysis Bullosa Medical Research Foundation, and the Jackson Gabriel Silver Foundation for funding this study. The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding sources.
Abbreviations
- DEB
Dystrophic Epidermolysis Bullosa
- DDEB
Dominant Dystrophic Epidermolysis Bullosa
- EB
Epidermolysis Bullosa
- EBCRC
Epidermolysis Bullosa Clinical Research Consortium
- EBS
Epidermolysis Bullosa Simplex
- JEB
Junctional Epidermolysis Bullosa
- REDCap
Research Electronic Data Capture Application
- RDEB
Recessive Dystrophic Epidermolysis Bullosa
Footnotes
Financial Disclosure: All authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: All authors have no conflict of interest.
Prior Presentation: This study was presented at the 2013 Society of Pediatric Dermatology in Milwaukee, WI.
References
- 1.Fine JD, Eady RA, Bauer EA, et al. The classification of inherited epidermolysis bullosa (EB): Report of the Third International Consensus Meeting on Diagnosis and Classification of EB. J Am Acad Dermatol. 2008;58:931–950. doi: 10.1016/j.jaad.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Goldschneider KR, Lucky AW. Pain management in epidermolysis bullosa. Dermatol Clin. 2010;28:273–282. doi: 10.1016/j.det.2010.01.008. ix. [DOI] [PubMed] [Google Scholar]
- 3.Pope E, Lara-Corrales I, Mellerio J, et al. A consensus approach to wound care in epidermolysis bullosa. J Am Acad Dermatol. 2012;67:904–917. doi: 10.1016/j.jaad.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Scheppingen C, Lettinga AT, Duipmans JC, et al. Main problems experienced by children with epidermolysis bullosa: a qualitative study with semi-structured interviews. Acta Derm Venereol. 2008;88:143–150. doi: 10.2340/00015555-0376. [DOI] [PubMed] [Google Scholar]
- 5.Duque MI, Yosipovitch G, Chan YH, et al. Itch, pain, and burning sensation are common symptoms in mild to moderate chronic venous insufficiency with an impact on quality of life. J Am Acad Dermatol. 2005;53:504–508. doi: 10.1016/j.jaad.2005.04.079. [DOI] [PubMed] [Google Scholar]
- 6.Zucker I, Yosipovitch G, David M, et al. Prevalence and characterization of uremic pruritus in patients undergoing hemodialysis: uremic pruritus is still a major problem for patients with end-stage renal disease. J Am Acad Dermatol. 2003;49:842–846. doi: 10.1016/s0190-9622(03)02478-2. [DOI] [PubMed] [Google Scholar]
- 7.Dawn A, Papoiu AD, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642–644. doi: 10.1111/j.1365-2133.2008.08941.x. [DOI] [PubMed] [Google Scholar]
- 8.Snauwaert JJ, Yuen WY, Jonkman MF, et al. Burden of itch in epidermolysis bullosa. Br J Dermatol. 2014 doi: 10.1111/bjd.12885. [DOI] [PubMed] [Google Scholar]
- 9.Stanford University Epidermolysis Bullosa Studies & Clinical Trials. 2013 Mar 15; http://dermatology.stanford.edu/gsdc/eb_clinic/trials/index.html. [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elman S, Hynan LS, Gabriel V, et al. The 5-D itch scale: a new measure of pruritus. Br J Dermatol. 2010;162:587–593. doi: 10.1111/j.1365-2133.2009.09586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Majeski CJ, Johnson JA, Davison SN, et al. Itch Severity Scale: a self-report instrument for the measurement of pruritus severity. Br J Dermatol. 2007;156:667–673. doi: 10.1111/j.1365-2133.2006.07736.x. [DOI] [PubMed] [Google Scholar]
- 13.Yosipovitch G, Zucker I, Boner G, et al. A questionnaire for the assessment of pruritus: validation in uremic patients. Acta Derm Venereol. 2001;81:108–111. doi: 10.1080/00015550152384236. [DOI] [PubMed] [Google Scholar]
- 14.Carrougher GJ, Martinez EM, McMullen KS, et al. Pruritus in adult burn survivors: postburn prevalence and risk factors associated with increased intensity. J Burn Care Res. 2013;34:94–101. doi: 10.1097/BCR.0b013e3182644c25. [DOI] [PubMed] [Google Scholar]
- 15.Casaer M, Kums V, Wouters PJ, et al. Pruritus in patients with small burn injuries. Burns. 2008;34:185–191. doi: 10.1016/j.burns.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Goutos I, Dziewulski P, Richardson PM. Pruritus in burns: review article. J Burn Care Res. 2009;30:221–228. doi: 10.1097/BCR.0b013e318198a2fa. [DOI] [PubMed] [Google Scholar]
- 17.Zachariah JR, Rao AL, Prabha R, et al. Post burn pruritus--a review of current treatment options. Burns. 2012;38:621–629. doi: 10.1016/j.burns.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Devries DT, Johnson LB, Weiner M, et al. Relative extent of skin involvement in inherited epidermolysis bullosa (EB): composite regional anatomic diagrams based on the findings of the National EB Registry, 1986 to 2002. J Am Acad Dermatol. 2004;50:572–581. doi: 10.1016/j.jaad.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 19.Patel T, Ishiuji Y, Yosipovitch G. Nocturnal itch: why do we itch at night? Acta Derm Venereol. 2007;87:295–298. doi: 10.2340/00015555-0280. [DOI] [PubMed] [Google Scholar]
- 20.Yosipovitch G, Goon A, Wee J, et al. The prevalence and clinical characteristics of pruritus among patients with extensive psoriasis. Br J Dermatol. 2000;143:969–973. doi: 10.1046/j.1365-2133.2000.03829.x. [DOI] [PubMed] [Google Scholar]
- 21.Yosipovitch G, Goon AT, Wee J, et al. Itch characteristics in Chinese patients with atopic dermatitis using a new questionnaire for the assessment of pruritus. Int J Dermatol. 2002;41:212–216. doi: 10.1046/j.1365-4362.2002.01460.x. [DOI] [PubMed] [Google Scholar]
- 22.Chamlin SL, Mattson CL, Frieden IJ, et al. The price of pruritus: sleep disturbance and cosleeping in atopic dermatitis. Arch Pediatr Adolesc Med. 2005;159:745–750. doi: 10.1001/archpedi.159.8.745. [DOI] [PubMed] [Google Scholar]
- 23.Yosipovitch G, Xiong GL, Haus E, et al. Time-dependent variations of the skin barrier function in humans: transepidermal water loss, stratum corneum hydration, skin surface pH, skin temperature. J Invest Dermatol. 1998;110:20–23. doi: 10.1046/j.1523-1747.1998.00069.x. [DOI] [PubMed] [Google Scholar]
- 24.Hilton MF, Umali MU, Czeisler CA, et al. Endogenous circadian control of the human autonomic nervous system. Comput Cardiol. 2000;27:197–200. [PubMed] [Google Scholar]
- 25.Steinhoff M, Bienenstock J, Schmelz M, et al. Neurophysiological, neuroimmunological, and neuroendocrine basis of pruritus. J Invest Dermatol. 2006;126:1705–1718. doi: 10.1038/sj.jid.5700231. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.