Abstract
There have been constant searches and researches which are taking place in the field of dental materials to best suit the ideal selection criteria to satisfy the functionality, biocompatibility, aesthetics as well as the durability as a maxillofacial material. Among all the different materials, Silicone is the most popularly used, but still studies are carried out to overcome their weaknesses and to come out with a material which can be labeled as the “ideal maxillofacial prosthetic material”. This article comprises the materials which were and are in use and the reason for their unpopularity. It also gives us a scope to understand the major fields where the materials lack and thus needs improvement to render an individual with the best maxillo-facial prosthesis.
Keywords: Heat-vulcanized silicones, Maxillo-facial materials, Room temperature vulcanized, Silicones
Introduction
Acquired and congenital defects of the face create an unfortunate condition for an individual to lead a comfortable life and these individuals require rehabilitation using maxillofacial prosthesis. The history of masking maxillofacial defects dates centuries back when the Egyptians and Chinese used wax and resins to reconstruct missing portion of the head and neck region [1]. This journey of searching an ideal material was started since 1500 A.D (when facial prostheses were described by French surgeon Ambrose Pare in 1575 [2] ) and have evolved from earlier prosthesis, made from gold, silver, paper, cloth, leather, wrought, metals, ceramics, vulcanite, acrylic to latex, polyvinyl chloride and copolymers, chlorinated polyethylene, polyurethane elastomers, medical grade silicones and polyposphazines.
Silicones, were introduced in 1946, but were used for the first time by Barnhart (1960) for extra-oral prosthesis [3]. and became more popular over other materials but possess some questionable properties. Thus an ideal maxillofacial material is yet to be discovered.
Quintessential Yardstick
While the new materials have exhibited some excellent properties, they have also exhibited frustrating deficiencies and thus lack the paradigmatic paradigm to best restore a maxillofacial defect.
The exemplar material should be biocompatible and stable chemically. Aesthetically the colour, texture, form and translucency should duplicate the part to be replaced as well as match the adjacent skin.
The critical Physical and mechanical properties are:
-
Tear strength –Defined as the resistance of a material to tearing force and is important in thin sections such as the areas surrounding the nasal and eye prosthesis. The thin glued prosthesis is susceptible to tearing while removal, permanently damaging the prosthesis. It is generally measured by “Pants Tear Energy” where a thin sheet of the elastomer is made in the shape of a pair of pants. The legs of the pants are then pulled slowly apart and the energy required to propagate a tear is measured. The tear energy (T) is a measure of the energy per unit area of newly torn surface and is determined from the load (F) required to propagate a tear in a trouser-shaped specimen as follows:
T = (F / t) (λ + 1)
Where ‘t’ is the specimen thickness and λ is an extension ratio [4].
The strength should preferably be in 30 to 100 psi (53 to175 N/cm) range to resist rupture at the edge for daily use [5].
-
Ultimate Tensile Strength and Percent (Maximum) Elongation: The total percent elongation, which includes both the elastic and plastic elongation, is helpful as different parts of the face have different requirements in terms of stretching the elastomers to accommodate the facial movements. Thus it also gives us an idea about the flexibility of the material. Tensile strength is in the range 300 to 1,000 psi (2.0 to 7 MPa) [5].
It is believed that a high percentage elongation and high tear strength produce most desirable combination [6].
Dynamic Modulus- The dynamic modulus (ED) is defined as the ratio of stress to strain for small cyclical deformations at a given frequency and at a particular point on the stress-strain curve. It is an important property for materials showing non linearity in a stress – strain graph. The maxillofacial materials should be flexible in nature i.e should possess low dynamic modulus. Dynamic resilience, which is the ratio of energy lost to energy expended, is also determined. The dynamic modulus decreases and the dynamic resilience increases as the temperature increases [4].
Hardness- Broadly defined as the resistance to abrasion and it is preferred that the prosthesis possess the same hardness as that of the missing facial structure.It should be soft having a hardness of less than about 40 preferably in the range 25-35 Shore A scale and resilient enough to respond to facial motion [4].
Stiffness - The materials should also possess low glass transition temperature in order to prevent the stiffening of material when exposed to cold temperatures [4].
Wettability- It may be assessed by measuring the advancing contact angle of water on the surface of the set material or by using a tensiometer to measure forces as the material is immersed and removed. Wettability is influenced by factors like cleanliness of the surfaces involved and their surface energies. Low surface energy of the adherend (for eg.maxillofacial elastomeric materials) produces a high contact angle with water, saliva or adhesives and therefore prevents the spreading of these materials over their surface. Poor surface wettability leads to poor boundary lubrication and thus causes patient discomfort [4,7].
Water Sorption- Represents the amount of water adsorbed on the surface and into the body of the material during fabrication or whiles the restoration is in service. Prosthesis may absorb saliva, sweat or water while washing the prosthesis which may affect the physical properties including the colour perception [7]. The prostheses should not distort when boiled in water or sterilized in steam.
Weight – The materials should be light weighted so that they are comfortable for the patient and aids in the retention of the prosthesis.
The material should be dimensionally stable when exposed to insults like sunlight, ultraviolet rays, and extreme conditions or to the adhesives and their solvents.
Fabrication aspect should be user friendly like easy processing, low polymerization temperature, sufficient working time and also are easily adaptable to both intrinsic and extrinsic staining procedures.
The Evolution – A search for the ideal
-
Acrylic resins (1940- 1960) - Particularly used in cases where there is least movement of tissue bed during function. Various advantages being, its ready availability, colour stability, can be relined and repaired, have good strength, can be fabricated with feather margin and a good shelf life of about two years. However, they are rigid, have water absorption and duplication is not possible [3,8].
Acrylic copolymers with elastic properties have disadvantages like poor edge strength, poor durability and degradation when exposed to sunlight. The restoration often becomes tacky and predisposes to dust collection and staining.
New generation of acrylic monomers, oligomers and macromeres are thermal, chemical and photo initiated and can eliminate the short comings of traditional acrylic co-polymers [8].
Polyvinylchloride and copolymer- A clear, tasteless and odorless material and has been used widely for maxillo-facial applications with advantages like being flexible, adaptable to both intrinsic and extrinsic staining. Plasticizers are added to produce an elastomeric effect at room temperature. Other ingredients include cross-linking agents for added strength and ultraviolet stabilizers for colour stability.
Chlorinated polyethylene- Processing involves high heat curing pigmented sheets in metal molds. Dow chemicals’ chlorinated polyethylene elastomer is an industrial grade thermoplastic elastomer. It is less irritating to the mucosa than silicone, less toxic than thermosetting silicone materials and non carcinogenic. Chlorinated polyethylene elastomer appears to be a suitable substitute for silicones for the fabrication of extraoral maxillofacial prosthesis in situations where cost of silicone is prohibitive.
-
Polyurethane elastomers (1970 to 1990)- This material is chemically composed of an extended segment of aliphatic diisocyanate groups and a segment of polyol groups (a mixture of polyesters) and an organotin catalyst for the polymerization process to occur.
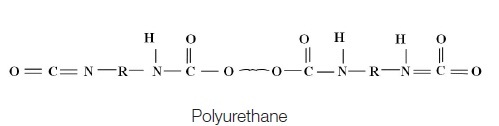
As these segments are varied in proportion to each other, so varies the softness of the end- product for its intended application, because maxillofacial prosthetics tend to require greater softness and flexibility.
Epithane-3 and Calthane are the only polyurethanes currently available for fabricating facial prostheses. These are three-component, room-temperature curing system [9]. These can be used to restore defects with mobile tissue beds as the positive qualities of this material pertain to its flexibility without losing strength at the edges, which allows margins to be made thin to obtain optimal esthetics. These have inherent environmental stability; higher tear resistance, low modulus without use of plasticizers, good ultimate strength and elongation. They can accept intrinsic colouration and are amenable to maxillofacial processing technique. Their disadvantages include poor colour stability, poor compatibility with adhesive systems and moisture sensitivity leading to gas bubbles during processing, this due to presence of diisocynates which also account for the toxicity of the material. Reaction must be carried out in dry atmosphere or carbon dioxide will be produced and porous elastomer results [10].
Thermoset urethane elastomers are produced through introduction of primary chemical crosslinks. If reactants are combined in Stoichiometric ratios and reactions are preferentially catalysed, a known controlled morphology can be developed. In one study polyurethane was greatly affected by aging [11].
Silicones (1960 to 1970), also known as polydimethyl siloxane is the most successful maxillofacial prosthetic material till now and the new advances are being made to this material to overcome their weaknesses. These became more popular over other materials as they have a range of good physical properties (such as excellent tear and tensile strength) over a range of temperature, easier to manipulate, high degree of chemical inertness, low degree of toxicity, and high degree of thermal and oxidative stability. Further they can be stained intrinsically and/or extrinsically to give them more lifelike natural appearance. When adequately cured, silicones elastomers resist absorbing organic materials that lead to bacterial growth and so with simple cleaning these materials are relatively safe and sanitary compared to other materials [12].
Silicone is a combination of organic and inorganic compounds and chemically they are termed as polydimethyl siloxane. The inorganic backbone makes the unique difference of this material as siloxane bonds Si—O—Si in the main chains, as well as Si—C bonds where side groups are bonded to silicone, are extremely flexible and have a great freedom of motion. This is reflected in their lower viscosity, lower surface tension, lower melting point and glass transition temperatures, and is responsible for the elastomeric behaviors of many polysiloxanes.
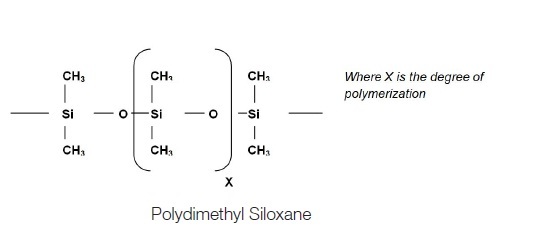 |
Silicone and methyl chloride react to form dimethyldichlorosilane. When water is added to dimethyldichlorosilane, a fluid polymer, polydimethyl siloxane (PDMS), is formed that is white and translucent and of varying viscosity, which is determined by the length of the polymer [9]. The PDMS chains and the silica fillers and the interactions between these two components affect the overall strength and service life of the silicone based maxillofacial prosthetic material. To increase the strength various types of fillers are added to reinforce the elastomers. Fumed silica, precipitated silica, aero gels are the most frequently used silica with the silicones.
Polysiloxanes must be cross-linked to form solid elastomer materials. Antioxidants and vulcanizing agents are added to change the raw mass into rubbery resins during processing and the process of cross linking is known as vulcanizing.
Depending whether the vulcanizing process uses heat or not, silicones are available as heat vulcanized (HTV) or room temperature vulcanized (RTV) and both exhibits advantages and disadvantages.
HTV silicone
Heat-vulcanized silicones are used occasionally for maxillofacial prostheses. It is usually a white, opaque material with a highly viscous, and putty like consistency. It is available as one component or two component putty. The vulcanization mechanism is achieved by an addition reaction.
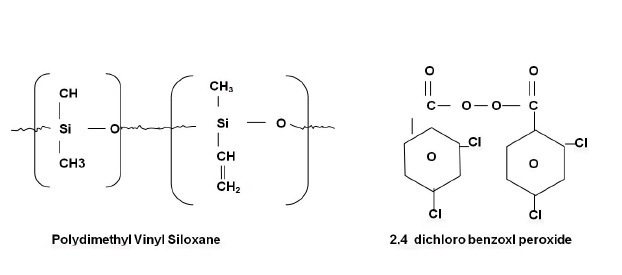
The components of heat-vulcanized silicones are a polydimethylvinyl siloxane copolymer with approximately 0.5% vinyl side chains, 2,4-dichlorobenzoyl peroxide as an initiator(vulcanizing agent), and a silica filler obtained from burning methyl silane. Catalyst of HTV is platinum salt (salt of chloroplatinic acid).
 |
The desired physical and mechanical properties can be achieved by altering the ratio of the matrix and the filler particles. Addition of opaque fillers increases strength but can compromise with translucency of prosthesis.
Vulcanization/ cross linking is by free radical addition polymerization (so no by product), which results from thermal decomposition of the initiator to form free radicals that cross-link the copolymer into a three dimensional resilient structure. The processing temperature is 180°C- 220°C [13] for about 30 min under pressure using metal molds. The copolymer is supplied as a rubbery solid with a high viscosity. The pigments are incorporated into the polymer with roller mills. Although this material is more difficult to pigment and process, excellent results can be obtained.
Advantages:-
- Excellent tear strength and highest tensile strength at 5.87 MPa (polyurethane the lowest at 0.83 MPa.).
- Excellent thermal, colour and chemical stability (rendering it more biologically inert).
- High percent elongation.
Disadvantages:-
- Poor esthetics due to opacity.
- Less elasticity.
- Low edge strength.
- Technique sensitive.
Examples: Silastic S-6508, 370, 372, 373,382, 379, Q7-4635, Q7-4650, Q7-4735, and SE-4524U.
RTV silicone (Room temperature vulcanizing)
There are two types:
Cross linking by condensation reaction: They have reactive groups such as silariols (hydroxyl- terminated polysiloxanes). This method of cross-linking requires a cross linking agent, eg. tetraethyl silicate, and a catalyst, e.g. dibutyltin dilaurate.
Eg.: Medical Adhesive Type A (Dow Corning), where methyl triacetoxy silane (II) is used as the cross-linking agent. The cross-linking, however, requires water molecules to hydrolyze the silane and produces acetic acid (an irritant) as the by-product. The use has therefore been limited to that of an extrinsic colourant carrier applied to the surface of the prosthesis.
Disadvantages:-
- Produces by- products.
- Curing time is excessively long making it impractical for curing the material inside a mold.
- Degradation reactions such as hydrolysis.
- Relatively low tear strength and are incapable of maintaining edge resistance.
b. Cross-linking of polysiloxanes by addition reactions
The reactions generally involve the addition of silyl hydride groups (—SiH) to vinyl groups (CH2=CH—) attached to the silicone with the aid of a platinum containing catalyst.
These silicones are not truly room vulcanized silicones. The curing of these silicones, in fact, requires heating the material at 150°C for a time, possibly an hour.
These materials have improved tear strength over the first type of RTV silicones.
Disadvantages:-
- Very hydrophobic.
- Selective adhesive property.
- No extrinsic colouration.
- Cure of the materials may be inhibited by traces of amines, sulfur, nitrogen oxides and organo-tin compounds.
Room-temperature-curing silicones are supplied as single-component materials that cure by evaporation of acetic acid. They are characterized” by a natural flesh-like appearance by using dyed rayon fibers, dry earth pigments, and/or oil paints. Prostheses are polymerized by bulk multiple packing. Recently epoxy resins and stainless steel molds are being used [13].
The top three advantages of the RTV silicone material were the use of stone molds, ease of manipulation and ease of colouring. Other advantages are colour stability and biological inertness.
Examples: Silastic 382, 399, 891, MDX4-4210, Cosmesil, A-2186, and A-2186F.
MDX4-4210, a clear-to-translucent two part (10:1, base: catalyst) silicone was introduced to the maxillofacial prosthetics field in the 1970s.
Introduced in 1986 by Factor II (Lakeside, AZ), A- 2186 was the first commercial platinum-catalyzed silicone elastomer. It is a clear-to-translucent two-part (10:1 base:catalyst) pourable silicone. A fast polymerization rate version of A-2186 with higher platinum content, “A-2186F,” became commercially available in 1987, though it was not a very preferred material for prosthesis purpose.
In 2000, Factor II introduced A-2000 as the first generation of a 1:1mixture platinum silicone followed by A-2006 in 2006.
Several other commercially available silicone products have been introduced since 1992, including Cosmesil, Realastic, VerSil- Tal (VST), and Liquid Silicone Rubber (LSR) Systems to name a few.
Colours- There are intrinsic and extrinsic methods of colouring.
Dry earth pigments, rayon flocking fibers (most commonly used), artist’s oil pigments, or a combination of these materials for intrinsic tinting. Kaolin material was commonly used as an opacifier.
The most-used extrinsic colouring method was Medical Adhesive Type-A mixed with Xylene as a retarder/thinner tinted with dry earth pigments or artist’s oil pigments applied to the surface of the prosthesis in a thin layer.
The introduction of silicone colourant technology began in 1992 with Factor II’s silicone intrinsic colourants. In 1999, the silicone colourants were further refined using a cross-linking fluid to maintain viscosity to allow drop-by-drop dispensing. Silicone extrinsic paste pigments (Factor II) with additional pigment to the cross-linking fluid were introduced shortly after [14].
Properties of HTV and RTV [Table/Fig-1]
[Table/Fig-1]:
Static and dynamic properties of the two types of silicone materials The comparison of properties of HTV and RTV are summarized in the above table
| S.no. | Properties | HTV | RTV |
|---|---|---|---|
| 1 | Ultimate tensile strength (MPa) | 5.87 | 4.20 |
| 2 | Maximum Elongation (%) | 441 | 445 |
| 3 | Pants tear strength (dynes/cmx 106) | Does not tear but stretches, as in tensile elongation | Does not tear but stretches, as in tensile elongation |
| 4 | Dynamic Modulus (MPa) | 4.66 | 2.12 |
RTV silicones are not as strong as the HTV silicones, and they are generally monochromatic. In comparison to other materials, both HTV and RTV have high tear resistance, because the samples do not tear but stretch, as in tensile elongation and high percent elongation ranging from 422% to 445%.
Dynamic Modulous is an important property because of the non-linearity of the stress-strain properties of these materials, they function differently at high and low rates of loading. Elastomers with a high dynamic modulus are rather rigid materials. RTV has the lowest dynamic modulus of 2.12 MPa [10]. Hardness values of Shore A for the Silicones maxillofacial elastomer is 25.
Medical grade silicone adhesives have been combined with RTV silicone based in various ratios to control the elastic properties.
According to a survey conducted by PC Montgomery et al., to review the extraoral maxillofacial materials, MDX4-4210 and A-2186 RTV silicones along with Silastic Medical Adhesive Type A (for extrinsic colouring of prostheses.) were the most preferred maxillofacial prosthetic materials used [14]. Due to hydrophobic nature, these have low adhesion to non- silicone adhesive material and suffers from limited working time [15].
The expected half-life of maxillofacial prosthesis is approximately six months and degradation of physical and colour properties of silicones are the most common reasons for re-fabrication.
Surface-treated silica fillers with an increased surface area and a small particle size are an important factor to enhance the physical and mechanical properties of silicone elastomers. Lately, researchers have found even stronger enhancement through the use of nano silica powder, which has an even larger surface area than micrometer-size silica powder [16].
In a constant effort made to improve the stress- strain property, various studies were conducted and are summarized in [Table/Fig- 2].
[Table/Fig-2]:
Summery of studies conducted in silicones
| S.no | Name of author (year) | Study conducted | Materials used | Conclusion |
|---|---|---|---|---|
| 1. | Andreopoulos et al., (1994) [17] | Effect of fillers on the mechanical properties (tensile strength and modulous) of poly(dimethyl siloxane) rubber (C-50, Bayer AG, Leverkusen, Germany) maxillofacial material. | -Silica -Fiber fillers (Short aramid fibers, glass fibers, high modulus polyethylene fibers). | Instead of Ultra high modulus fibers silica fillers should be used. |
| 2. | JH Lai et al., (1996) [5] | Invention of Polysiloxane aterials including methacry oxyalkyl-terminated olydimethylsiloxanes (MPDS) to reduces the ydrophobicity of silicones. | Modification of polydimethylsiloxanes. Thermal initiator- Lauroyl peroxide preferred over benzoyl peroxide. Filler - Amorphous silica. Crosslinker- XA-Ol, TEGDMA. Thermal curing of the polysiloxane MPDS was conducted in a stainless steel mold to minimize the effects of oxygen inhibition. | MPDS has following advantages over MDX4-4210: - Very long working time. - Extended shelf life- - Higher in tear and tensile strength - Incorporation of metharylate group in the silicones reduces the hydrophobicity of the silicones enhances the adhesive bond strength to the non- silicone based adhesives. However the ultimate elongation is slightly lower than that of MDX4-4210. |
| 3. | Andreopoulos et al., (1998) [18] | Effect of reinforcement of silica powder up to 50- percent concentration on the mechanical properties of silicone maxillofacial materials. | Silica powder up to 50% concentration. | Tensile strength improved with increasing silica fillers up to 35% significantly. |
| 4. | JH Lai et al., (2002) [15] | Introduction of new organosilicone MPDS- MF 606 | Modified Methacry loxyalkyl-terminated polydimethylsiloxanes (MPDS) and comparing the properties with A-2186 | The hardness is similar to A-2186 whereas Tear, tensile strength, ultimate elongation and adhesive bond to non- silicones are higher than A-2186. Suitable for use in fabrication of clinical prosthesis. |
| 5. | Aziz et al., (2003) [19] | Effect of different parameters on the development of new improved maxillofacial material C50. | Silica fillers- R104, R106, R202, R972, R974, and R812. Silica filler concentrations- 0 - 25 wt%. Cross-linker concentration- 0.12 g- 0.72 g (per 10 g of base polymer). Ratio of high and low molecular weight polymers. | Increasing the R812 silica filler concentration from 15 wt% to20 wt% and having cross-linker of 0.28 percent was associated with significant increase in tear strength. |
| 6. | Karayazgan et al., (2003) [20] | Effect of tulle in increasing the tear strength of maxillofacial prosthesis at the edges. | Tulle | Tulle resulted in having more stable, and tear resistant silicone prosthesis which is less likely to deform during application or removal of adhesives, cosmetics or cleaning agents. |
| 7. | Tariq Aziz et al., (2003) [7] | Analysis of the properties of commonly used silicone rubber materials. | -Cosmesil HC and Nusil (MED-4920) -Prestige (Premium facial and body elastomer) -Factor II (A 2186) | None of the commercially available materials have adequate properties. Cosmesil HC and Nusil (MED-4920) had adequate mechanical properties along with good translucency but have high viscosity. Prestige (Premium facial and body elastomer) was a soft material however together with Cosmesil St it had extremely high water absorption and low tears strength. Factor II (A 2186) had well all round mechanical properties and had the highest tear strength. |
| 8. | Gunay et al., (2008) [21] | Investigation on the incorporation of tulle in silicone maxillofacial prosthesis. | Tulle | Tensile and tear strengths were significantly higher. |
| 9. | Mirabedini et al., (2008) [22] | Effect of TiO2 on the mechanical and adhesion properties of RTV silicone elastomer coatings. | TiO2 fillers-5.0 wt%, 10.0 wt%, 15.0 wt% and 20.0 wt%. | Tensile stress, modulus, and abrasion resistance increased with increasing the filler content up to 15.9 wt%. Hardness was increased with increasing filler contents up to 25.0 wt%, but on the contrary, elongation to fracture was decreased with increasing filler content. |
| 10. | Sharif A. Mohammad et al., (2010) [12] | Effect of POSS on the mechanical properties, of maxillofacial material (Factor II A- 2000). | POSS - pohedral silsesquioxane | The POSS loading had a significant effect on the tear and tensile properties of the materials. |
| 11. | Liu Q, Shao LQ et al., (2013) [23] | Effect of silicone elastomers filled with hollow microspheres. | Hollow microspheres were mixed with MDX4-4210 silicone elastomer using Q7-9180 silicone fluid as diluents. Volume fractions of microspheres were 0, 5, 15, and 30% v/v (volume ratio to the total volume of MDX4-4210 and microspheres) were used. | The microspheres dispersed well in the matrix. Shock absorption was the greatest by the 5% v/v composite, and decreased with increasing concentrations of microspheres. Other properties except elongation at break decreased with increasing concentration. Tear strength of all composites was markedly lower than that of pure silicone elastomer. Has good biocompatibility. Novel light and soft material with good flexibility, biocompatibility and properties at 5% holds a promising prospect for clinical application as maxillofacial prosthesis. |
Alternative Materials
Foaming silicones: Silastic 386 – in it is a type of RTV material. The basic silicone has an additive which release gas when the catalyst (stannous octoate) is introduced. The purpose of the foam forming silicones is to reduce the weight of the prosthesis. However, the major disadvantage of foamed material is reduced strength and is susceptible to straining, leading to weakening of the material. This weakness can be overcome partially by coating foam with another silicone which adds strength but increase stiffness. Purpose of the foam silicon is to reduce the weight of the prosthesis.
Siphenylenes: These are siloxane copolymers that contain methyl and phenyl groups. These exhibit improved edge strength, low modulus of elasticity and colour stability over the more conventional polydimethyl siloxane [24].
Silicone Block Copolymers: In this blocks of polymers other than siloxane are positioned with the traditional siloxane polymers. The hydrophobic nature and foreign nature of silicones has been proven to cause problems, especially with regard to the interaction with the body on a molecular level. This can lead to the induction of foreign body reactions and the development of infections particularly at the interface between silicone and tissue. These silicone block copolymers can to some extent overcome these problems as the more hydrophilic part of these amphiphilic polymers provides improved wettability and thus tissue compatibility. An example of this is the intertwining of poly methyl methacrylate into the chains of siloxane [25].
Polyphosphazenes: Researchers in New Orleans dealt with maxillofacial prosthesis, have found that compounding Polyphosphazenes with little or no fillers and decreasing the ratio of acrylic to rubber yields a softer rubber, with a HDA of 25, similar to human skin. The rubber is compounded with pigments for appropriate matching with the patients’ skin.
Creative uses in prosthetics dentistry include implant denture retention and stability by processing the rubber over the implant head. The major advantage of these over the mechanical devices is being the freedom of movements of the denture towards the tissue similar to periodontal membrane around natural tooth.
When a stable and reasonably priced source of polymer becomes available, these might become the material of choice for many biomedical uses.
Summary
With the growing number of head and neck cancers diagnosed each year, the demand for both intraoral and extra oral prosthetic rehabilitation continues to rise. Although prosthetic rehabilitation is not always considered a necessary course of treatment, but it should be noted that it is not a vanity issue; rather, it is a psychological issue that impacts more and more people throughout the world each year. To date, none of the commercially available materials satisfy all the requirements of the ideal maxillo-facial material. Each material has its own advantages and disadvantages. It might be a dream but the possibility of fabricating a high quality lifelike prosthesis directly on the face which requires an excellent skill of the Prosthodontist and the role of a dental material scientist who can help by providing a perfect material with improved properties and colour stable colouring agents to rehabilitate the patient with maxillo-facial defect who deserves the best we can offer.
Financial or Other Competing Interests
None.
References
- [1].Anusavice Kenneth J, Shen Chiayi, Rawls H. Ralph. Phillips’ Science of Dental Materials. 12th ed. Elsevier; 2013. [Google Scholar]
- [2].Mahajan Harsh, Gupta Kshiliz. Maxillofacial prosthetic material: A literature review. J Orofac Res. 2012;2(2):87–90. [Google Scholar]
- [3].Khindria SK, Bansal S, Kansal M. Maxillofacial prosthetic materials- Review Article. J Indian Prosthodont Soc. 2009;9(1):2–5. [Google Scholar]
- [4].Sakaguchi Ronald L, Powers John M. Craigs’s Restorative Dental Materials. 13th ed. Philadelphia: Mosby, Inc; 2012. [Google Scholar]
- [5].Lai Juley H. Maxillofacial Prosthetic Materials. US patent no.5. Dec.17,1996;584(886) [Google Scholar]
- [6].Begum Z, Kola Z, Joshi P. Analysis of properties of commercially available silicone elastomers for maxillofacial prostheses. Int. Journal of Contemporary Dentistry. 2011;2(4):1–5. [Google Scholar]
- [7].Aziza T, Watersa M, Jaggerb Robert. Analysis of the properties of silicone rubber maxillofacial prosthetic materials. Journal of Dentistry. 2003;31:67–74. doi: 10.1016/s0300-5712(02)00084-2. [DOI] [PubMed] [Google Scholar]
- [8].Maller Udita S, Karthik KS, Maller Sudhakara V. Maxillofacial Prostheric Materials - Past & Present Trends. J Acquir Immune Defic Syndr. 2010;1(2):26–30. [Google Scholar]
- [9].Huber H, Studer Stephan P. Materials and techniques in maxillofacial prosthodontic rehabilitation. Oral Maxillofacial Surg Clin N Am. 2002;14:73–93. doi: 10.1016/s1042-3699(02)00018-3. [DOI] [PubMed] [Google Scholar]
- [10].Craig Robert G, Powers John M. Restorative Dental Materials. 11th ed. Philadelphia: Mosby, Inc; 2002. [Google Scholar]
- [11].Yu R, Koran A, Craig RG. Physical properties of maxillofacial elastomers under conditions of accelerated aging. J Dent Res. 1980;59(6):1041–47. doi: 10.1177/00220345800590060601. [DOI] [PubMed] [Google Scholar]
- [12].Mohammad Sharif A, Wee Alvin G, Rumsey Deborah J, Schricker Scott R. Maxillofacial materials reinforced with various concentrations of Polyhedral Silsesquioxanes. J Dent Biomech. 2010:1–9. doi: 10.4061/2010/701845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Anusavice Kenneth J. Phillips’ science of dental materials. 11th ed. St.Louis: Saunders Elsevier; 2009. [Google Scholar]
- [14].Montgomery Patricia C, Kiat-Amnuay Sudarat. Survey of Maxillofacial Prostheses Materials Used. J Prosthodont. 2010;19:482–90. doi: 10.1111/j.1532-849X.2009.00538.x. [DOI] [PubMed] [Google Scholar]
- [15].Lai JH, Wang LL. New organosilicon maxillofacial prosthetic materials. Dent Mater. 2002;18:281–86. doi: 10.1016/s0109-5641(01)00050-1. [DOI] [PubMed] [Google Scholar]
- [16].Han Y, Kiat-Amnuay S, Powers JM, Zhao Y. Effect of nano-oxide concentration on the mechanical properties of a maxillofacial silicone elastomer. J Prosthet Dent. 2008;100(6):465–73. doi: 10.1016/S0022-3913(08)60266-8. [DOI] [PubMed] [Google Scholar]
- [17].Andreopoulos AG, Evangelatou M. Evaluation of various reinforcements for maxillofacial silicone elastomers. J Biomater Appl. 1994;8(4):344–60. doi: 10.1177/088532829400800403. [DOI] [PubMed] [Google Scholar]
- [18].Andreopoulos AG, Evangelatou M, Tarantili PA. Properties of maxillofacial silicone elastomers reinforced with silica powder. J Biomater Appl. 1998;13(1):66–73. doi: 10.1177/088532829801300104. [DOI] [PubMed] [Google Scholar]
- [19].Aziz T, Waters M, Jagger R. Development of a new poly (dimethylsiloxane) maxillofacial prosthetic material. J Biomed Mater Res B Appl Biomater. 2003;65(2):252–61. doi: 10.1002/jbm.b.10559. [DOI] [PubMed] [Google Scholar]
- [20].Karayazgan B, Gunay Y, Evlioglu G. Improved edge strength in a facial prosthesis by incorporation of tulle: a clinical report. The Journal of Prosthetic Dentistry. 2003;90(6):526–29. doi: 10.1016/j.prosdent.2003.08.002. [DOI] [PubMed] [Google Scholar]
- [21].Gunay Y, Kurtoglu C, Atay A, Karayazgan B, Gurbuz CC. Effect of tulle on the mechanical properties of a maxillofacial silicone elastomer. Dent Mater J. 2008;27(6):775–79. doi: 10.4012/dmj.27.775. [DOI] [PubMed] [Google Scholar]
- [22].Mirabedini SM, Mohseni M, Pazokifard SH, Esfandeh M. Effect of TiO2 on the mechanical and adhesion properties of RTV silicone elastomer coatings. Colloids Surf A Physicochem Eng Asp. 2008;317:80–86. [Google Scholar]
- [23].Liu Q, Shao LQ. Biomechanical characterization of a low density silicone elastomer filled with hollow microspheres for maxillofacial prostheses. J Biomater Sci Polym Ed. 2013;24(11):1378–90. doi: 10.1080/09205063.2012.762292. [DOI] [PubMed] [Google Scholar]
- [24].Lewis DH, Castleberry DJ. An assessment of recent advances in external maxillofacial materials. J ProsthetDent. 1980;43:426–29. doi: 10.1016/0022-3913(80)90215-2. [DOI] [PubMed] [Google Scholar]
- [25].Tsai FH, et al. Synthesis of silicone blocks copolymers for use as maxillofacial materials. Proceedings of Conference on Materials Research in Maxillofacial Prosthetics. Transactions of the Academy of Dental Materials. 1992;5:126. [Google Scholar]


