Abstract
This study was undertaken to evaluate the postural effect on ventilatory responses during both supine and sitting exercise. Seven healthy men performed two exercise tests utilizing the ramp protocol (20 watts/min) with a cycle ergometer in each position. The results were as follows: The oxygen uptake and the oxygen pulse measured at 180 watts and at anaerobic threshold in the sitting were significantly higher compared with those in the supine position. The average of carbon-dioxide output, minute ventilation and tidal volume at lower exercise intensities showed higher values in the sitting compared with those in the supine position, whereas there were no significant differences for respiratory rate. There was significant difference in the slope of the minute ventilation to carbon-dioxide output plot between sitting and supine position. In conclusion, the higher minute ventilation in the sitting position was mainly performed by higher tidal volume which may counteract the effects of an increase in physiological dead space. The lower slope of the minute ventilation to carbon-dioxide output plot which shows more effective ventilation in the supine position may be due to decreased physiological dead space and higher diffusion capacity.
Keywords: posture, ventilatory response, exercise
The major differences of cardiopulmonary responses between supine and sitting are caused by circulatory alterations. Due to reduction of hydrostatic pressure, the blood volume shifts toward the heart. In turn, stroke volume and cardiac output increase1). In addition, due to an increase in the volume of blood in the chest, vital capacity and functional residual capacity decrease2). There is general agreement that the vital capacity and the functional reserve volume are less in the supine than in the upright position at rest2).
Many researchers have studied cardiopulmonary responses during supine and sitting exercise from the point of view of cardiac function3–9). However, it is still unclear as to how ventilatory responses are influenced by postural difference during exercise. Some researchers have reported ventilatory responses during exercise; however, these exercises imposed a single constant work and relatively low work load9)13). There is little information available about ventilatory responses during incremental exercise.
We hypothesised that these postural effects may influence metabolic and ventilatory responses during exercise, especially at lower work load, and these postural effects may decrease as exercise work load increases. We therefore, evaluated the postural effects on ventilatory responses and exercise capacity during supine and sitting exercise using ramp incremental exercise protocol.
Methods
Subjects
Seven healthy Japanese men participated in this study. The mean age, weight, and height of the subjects were 20.0 ± 2.0 yr., 67 ± 9 kg, and 173 ± 4 cm, respectively. All subjects were active exercisers. None took medications and no participant had a history of cardiopulmonary disease. The participants were fully informed of any possible risks or discomfort associated with these experiments before volunteering to participate and giving their written informed consent.
Procedure
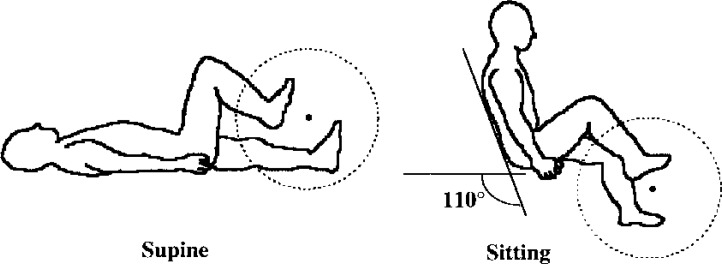
Both exercise tests in the supine and the sitting positions were performed using an electromagnetically braked ergometer (Space cycle SSR, Health Systems Co.). For the supine study, the seat and upper part of the ergometer were set in horizontal and the crank axis was set above the body. The shoulders were stabilised and feet were fixed by forefoot loops and elastic bandaging (Fig. 1). For the sitting study, the upper part of the ergometer was tilted upwards at 110° angle between backrest and floor (Fig. 1). After a warming-up period of 3 minutes at 20 watts, the work rate increased as a ramp protocol at a rate of 20 watts per minute until 180 watts. Pedal frequency was maintained 50 cycles per minute. The same protocol was used for both supine and sitting exercises. These tests were randomised and approximately 1 week apart.
Fig. 1.
Cardiopulmonary exercise testing in supine and sitting position
Instrumentation
Variables including oxygen uptake ( ), carbon dioxide output (
), carbon dioxide output ( ), and other ventilation data were measured at rest and throughout the exercise period with a Respiromonitor RM-300 (Minato Medical Science Co.). The respiromonitor RM-300 consists of a microcomputer, a hot wire flowmeter and a gas analyser. The gas analyser contains a sampling tube, filter, suction pump, O2 analyser made by a zirconium element and an infrared CO2 analyser. The respiromonitor RM-300 calculated breath-by-breath for
), and other ventilation data were measured at rest and throughout the exercise period with a Respiromonitor RM-300 (Minato Medical Science Co.). The respiromonitor RM-300 consists of a microcomputer, a hot wire flowmeter and a gas analyser. The gas analyser contains a sampling tube, filter, suction pump, O2 analyser made by a zirconium element and an infrared CO2 analyser. The respiromonitor RM-300 calculated breath-by-breath for  and
and  . The system was calibrated carefully with room air and certified oxygen/ carbon dioxide concentration before each test. Throughout the test 12–leads ECGs were continuously monitored and heart rate (HR) was measured from the R-R interval of the electrocardiogram (ML-5000, Fukuda Denshi Co.). Peripheral arterial blood pressures (systolic and diastolic blood pressure) were determined every minute using cuff method via automatic blood pressure monitor (Stress test system, STBP-780, Colin Co.). The slope of the minute ventilation (
. The system was calibrated carefully with room air and certified oxygen/ carbon dioxide concentration before each test. Throughout the test 12–leads ECGs were continuously monitored and heart rate (HR) was measured from the R-R interval of the electrocardiogram (ML-5000, Fukuda Denshi Co.). Peripheral arterial blood pressures (systolic and diastolic blood pressure) were determined every minute using cuff method via automatic blood pressure monitor (Stress test system, STBP-780, Colin Co.). The slope of the minute ventilation ( ) to
) to  plot (
plot ( –
– slope) was calculated as a parameter of increased ventilation10)11). The anaerobic threshold (AT) was determined synthetically by criteria of the point of non-linear increase in the ventilatory equivalent for oxygen or end-tidal oxygen which systematically rose without an increase in end- tidal carbon dioxicide12).
slope) was calculated as a parameter of increased ventilation10)11). The anaerobic threshold (AT) was determined synthetically by criteria of the point of non-linear increase in the ventilatory equivalent for oxygen or end-tidal oxygen which systematically rose without an increase in end- tidal carbon dioxicide12).
Statistical analysis
Data were compared using a Wilcoxon signed rank analysis. A p value <0.05 was considered statistically significant. Values are expressed as mean ± standard deviation.
Results
The data ( , HR and oxygen pulse) are shown in Table 1. The
, HR and oxygen pulse) are shown in Table 1. The  and the oxygen pulse measured at 180 watts in the sitting position were significantly higher compared with the supine position. The HR at 180 watts was slightly higher in the sitting position compared with the supine position, but not significant. The
and the oxygen pulse measured at 180 watts in the sitting position were significantly higher compared with the supine position. The HR at 180 watts was slightly higher in the sitting position compared with the supine position, but not significant. The  and the oxygen pulse measured at AT in the sitting position were also significantly higher compared with the supine position. The HR at AT showed slightly higher value in the sitting position compared with the supine exercise, but not significant.
and the oxygen pulse measured at AT in the sitting position were also significantly higher compared with the supine position. The HR at AT showed slightly higher value in the sitting position compared with the supine exercise, but not significant.
Table 1. Comparison of oxygen uptake ( ), heart rate (HR), oxygen pulse, tidal volume (TV), respiratory rate (RR) and minute ventilation (
), heart rate (HR), oxygen pulse, tidal volume (TV), respiratory rate (RR) and minute ventilation ( ) measured at anaerobic threshold (AT) and at peak exercise (n=7).
) measured at anaerobic threshold (AT) and at peak exercise (n=7).
| Supine | Sitting | |
|---|---|---|
 at AT (ml/kg/min) at AT (ml/kg/min) |
17.4 ± 2.8 | 20.8 ± 3.9* |
| HR at AT (bpm) | 113.6 ± 9.1 | 120.1 ± 6.3 |
| Oxygen pulse at AT (ml/beat) | 10.1 ± 0.7 | 11.4 ± 1.5* |
| TV at AT (ml) | 1362.7 ± 165.3 | 1204.6 ± 164.7* |
| RR at AT (bpm) | 25.3 ± 3.4 | 25.3 ± 5.4 |
 at AT (l/min) at AT (l/min) |
34.3 ± 5.2 | 29.7 ± 2.8 |
Peak  (ml/kg/min) (ml/kg/min) |
32.6 ± 3.8 | 35.5 ± 3.2* |
| Peak HR (bpm) | 155.7 ± 17.2 | 162.0 ± 11.8 |
| Peak oxygen pulse (ml/beat) | 14.0 ± 1.6 | 14.6 ± 1.7* |
| maximum TV (ml) | 2042.4 ± 324.6 | 1933.9 ± 240.6 |
| maximum RR (bpm) | 37.2 ± 7.2 | 37.4 ± 7.6 |
maximum  (l/min) (l/min) |
74.2 ± 7.7 | 71.3 ± 10.6 |
Values are reported as mean ± SD.
p<0.05 sitting vs supine.
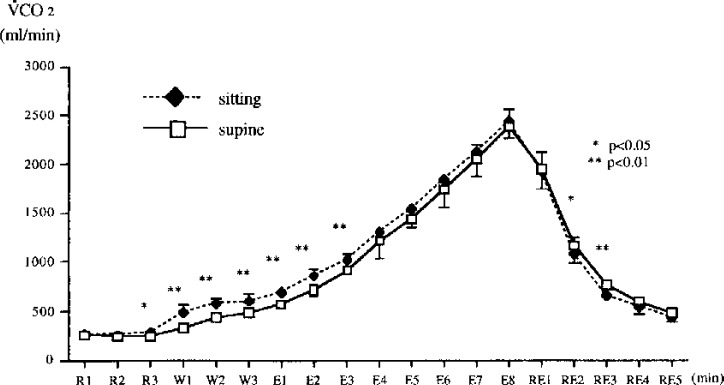
The average values of  at each intensity were slightly higher in the sitting position compared with the supine position, but not significant. The average values of
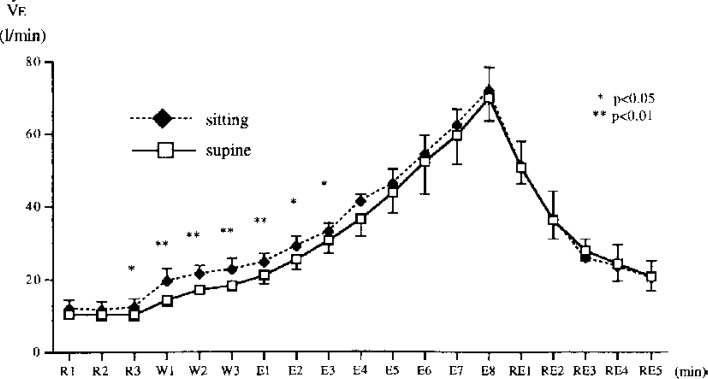
at each intensity were slightly higher in the sitting position compared with the supine position, but not significant. The average values of  (Fig. 2) and
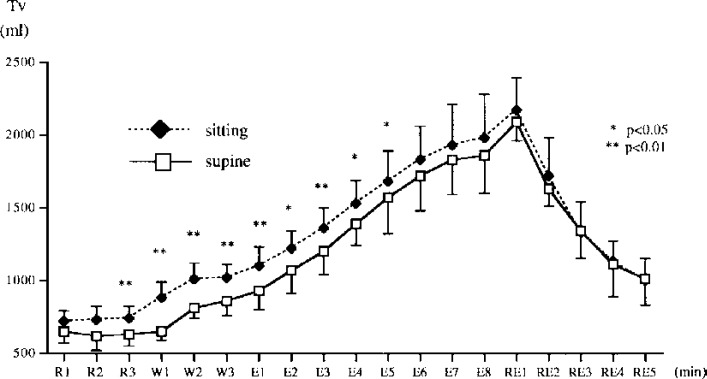
(Fig. 2) and  (Fig. 3) at each intensity were also higher in the sitting position compared with the supine position. In particular the differences were significant from before the warming-up period to 3 minutes after exercise started. There were significant differences in tidal volume (TV) (Fig. 4) between sitting and supine from the pre-warming up period to 5 minutes after exercise start, whereas there were no significant differences in respiratory rate (RR) by position during each testing. The average values of TV at AT and at the end of exercise were significantly higher in the sitting position compared with the supine position (p<0.05) (Table 1). Finally, the
(Fig. 3) at each intensity were also higher in the sitting position compared with the supine position. In particular the differences were significant from before the warming-up period to 3 minutes after exercise started. There were significant differences in tidal volume (TV) (Fig. 4) between sitting and supine from the pre-warming up period to 5 minutes after exercise start, whereas there were no significant differences in respiratory rate (RR) by position during each testing. The average values of TV at AT and at the end of exercise were significantly higher in the sitting position compared with the supine position (p<0.05) (Table 1). Finally, the  -
- slope in sitting exercise was significantly higher than that in supine exercise, 27.0 ± 2.5 and 25.6 ± 1.7, respectively (p<0.05).
slope in sitting exercise was significantly higher than that in supine exercise, 27.0 ± 2.5 and 25.6 ± 1.7, respectively (p<0.05).
Fig. 2.
Mean ± SD of the change in carbon-dioxide output ( ) during cycle exercise in the sitting position and the supine position. R; at rest. W; during warming up. E; during exercise. RE; after exercise.
) during cycle exercise in the sitting position and the supine position. R; at rest. W; during warming up. E; during exercise. RE; after exercise.
Fig. 3.
Mean ± SD of the change in minute ventilation ( ) during cycle exercise in the sitting position and the supine position.
) during cycle exercise in the sitting position and the supine position.
R; at rest. W; during warming up. E; during exercise. RE; after exercise.
Fig. 4.
Mean ± SD of the change in tidal volume (TV) during cycle exercise in the sitting position and the supine position.
R; at rest. W; during warming up. E; during exercise. RE; after exercise.
Discussion
Previous studies have shown that the maximal  , maximal HR and maximal exercise intensity observed during supine exercise tend to be lower than those observed during sitting exercise. This might be caused by mechanical efficiency5) or the weight of the legs which have to be raised against gravity4)6)7). In addition to these, we previously observed lower noradrenaline and angiotensin II during the supine position, which may be taken as a reflection of a lesser degree of activation of the sympathetic nervous system3). Our previous results suggested that a larger blood flow is distributed to active muscles in the sitting position due to the raised peripheral vascular resistance in the non-active muscles and the abdominal cavity. In the present study also, the average values of
, maximal HR and maximal exercise intensity observed during supine exercise tend to be lower than those observed during sitting exercise. This might be caused by mechanical efficiency5) or the weight of the legs which have to be raised against gravity4)6)7). In addition to these, we previously observed lower noradrenaline and angiotensin II during the supine position, which may be taken as a reflection of a lesser degree of activation of the sympathetic nervous system3). Our previous results suggested that a larger blood flow is distributed to active muscles in the sitting position due to the raised peripheral vascular resistance in the non-active muscles and the abdominal cavity. In the present study also, the average values of  and
and  at each intensity and at AT were significantly higher in sitting exercise compared with supine exercise from rest to the end of exercise. These results may be explained by the reasons above.
at each intensity and at AT were significantly higher in sitting exercise compared with supine exercise from rest to the end of exercise. These results may be explained by the reasons above.
The average values of  at each intensity were also significantly higher in the sitting position from the pre-warming up period to relatively lower workloads, and these differences in
at each intensity were also significantly higher in the sitting position from the pre-warming up period to relatively lower workloads, and these differences in  related to increases TV, whereas there were no significant differences in RR. These differences in
related to increases TV, whereas there were no significant differences in RR. These differences in  and TV decreased as the exercise intensity increased. This is in agreement with other published observations that
and TV decreased as the exercise intensity increased. This is in agreement with other published observations that  and TV are higher in the sitting position than in the supine position at low level exercise workloads8)13). It has been observed that, during four levels of exercise (12.5, 25, 37.5, 50 W),
and TV are higher in the sitting position than in the supine position at low level exercise workloads8)13). It has been observed that, during four levels of exercise (12.5, 25, 37.5, 50 W),  and TV were greater in the sitting position, and the greater
and TV were greater in the sitting position, and the greater  observed during sitting was due to greater TV13). The higher
observed during sitting was due to greater TV13). The higher  during sitting exercise may be mainly metabolically mediated, and that this was most likely caused by greater muscle activities which was confirmed by higher
during sitting exercise may be mainly metabolically mediated, and that this was most likely caused by greater muscle activities which was confirmed by higher  and
and  . In particular, in this study, higher
. In particular, in this study, higher  during sitting exercise was mainly performed by higher TV. McGregor et al. observed that
during sitting exercise was mainly performed by higher TV. McGregor et al. observed that  was higher in the sitting position at rest and at moderate workload (50 and 90 watts). He also observed that this was due to a high RR9). The McGregor's result is in variance with our observations that greater
was higher in the sitting position at rest and at moderate workload (50 and 90 watts). He also observed that this was due to a high RR9). The McGregor's result is in variance with our observations that greater  observed during sitting exercise is due to RR. The McGregor's study utilised a mouthpiece with noseclip while our study used a gas sampling mask. Sackner et al. reported the influence of a mouthpiece with noseclip on respiratory responses during exercise14). When subjects performed cycle exercise with the use of a mouthpiece, RR and
observed during sitting exercise is due to RR. The McGregor's study utilised a mouthpiece with noseclip while our study used a gas sampling mask. Sackner et al. reported the influence of a mouthpiece with noseclip on respiratory responses during exercise14). When subjects performed cycle exercise with the use of a mouthpiece, RR and  were greater whereas TV was unaffected. Therefore, the difference in measurement technique between their study and ours may account for the difference in results. In addition, the McGregor's study used cycle rates between 70 and 75 per minute. Thus, the difference between our observation and his may be due to differences in the protocol of exercise.
were greater whereas TV was unaffected. Therefore, the difference in measurement technique between their study and ours may account for the difference in results. In addition, the McGregor's study used cycle rates between 70 and 75 per minute. Thus, the difference between our observation and his may be due to differences in the protocol of exercise.
Possible explanations of the difference in ventilation between supine and sitting are related to the mechanical and physiological differences. In the supine position, the diaphragm is elevated, and the elevated diaphragm alters its mechanical advantage1). In addition, an increased venous return makes lung blood volume increases1). Increased lung blood volume makes the physiological dead space decrease2)15). Craig et al. showed that the VD/VT ratio decreased from a mean value of 34 percent in the upright position to 30 percent in the supine position16). In sitting position, the physiological dead space increases relatively. As a result, subjects would counteract the effects of an increase in physiological dead space by a corresponding increase in the minute ventilation to maintain an alveolar ventilation.
We also observed that the slope of the  -
- was greater during sitting exercise than that during supineexercise. The lower slope of the
was greater during sitting exercise than that during supineexercise. The lower slope of the  -
- shows more effective ventilation. Stokes et al. noted that the lung's diffusion capacity for carbon-dioxide was higher in the supine position than in the sitting position17). Thus, more effective ventilation in the supine position may be due to increased alveolar ventilation following to decreased physiological dead space and higher diffusion capacity for carbon-dioxide.
shows more effective ventilation. Stokes et al. noted that the lung's diffusion capacity for carbon-dioxide was higher in the supine position than in the sitting position17). Thus, more effective ventilation in the supine position may be due to increased alveolar ventilation following to decreased physiological dead space and higher diffusion capacity for carbon-dioxide.
In summary, this study demonstrates that there are significant differences in VE and TV between supine exercise and sitting exercise, in particular, at relatively lower exercise workloads. These differences in  and TV decrease as the exercise intensity increases. There is more effective ventilation in the supine position. Clinically, it is important to consider appropriate exercise positions based on the knowledge of postural effects to ventilation.
and TV decrease as the exercise intensity increases. There is more effective ventilation in the supine position. Clinically, it is important to consider appropriate exercise positions based on the knowledge of postural effects to ventilation.
Acknowledgments.
We are greatly indebted to Professor Kunisato Miyoshi, MD of St. Marianna University School of Medicine.
References
- 1). Rowell LB: Human Circulation —Regulation During Physical Stress—, 7 Adjustments to upright posture and blood loss. Oxford University Press; New York, 1986, pp. 137–173. [Google Scholar]
- 2). Fenn WO: Handbook of physiology, Section 3 Respiration, Chapter 53: Lung volumes. American Physiological Society, Washington D.C., 1965, pp.1345–1379. [Google Scholar]
- 3). Takahashi T, Tanabe K, Nakayama M, Osada N, Yamada S, Ishiguro T, Itoh H, Murayama M: Cardiopulmonary response during supine and sitting bicycle exercise. J Phys Ther Sci 7: 33–38, 1995. [Google Scholar]
- 4). Astrand PO: Textbook of Work Physiology, Japanese version. The Taishukan Publishing Co. Ltd, Tokyo, 1979, pp.83–136. [Google Scholar]
- 5). Astrand PO, Saltin B: Maximal oxygen uptake and heart rate in various types of muscular activity. J Appl Physiol 16: 977–981, 1961. [DOI] [PubMed] [Google Scholar]
- 6). Lorgeril M, Laurier J, Stucki V, Meier B, Righetti A, Bourassa MG: Computerized determination of lactate threshold during three modes of exercise. Heart-Vassels 5: 76–80, 1990. [DOI] [PubMed] [Google Scholar]
- 7). Quinn TJ, Smith SW, Vroman NB, Kertzer R, Olney WB: Physiologic responses of cardiac patients to supine, recumbent, and upright cycle ergometry. Arch Phys Med Rehabil 76(3): 257–261 1995. [DOI] [PubMed] [Google Scholar]
- 8). Convertino V, Hung J, Goldwater D, DeBusk RF: Cardiovascular responses to exercise in middle-aged man after 10 days of bedrest. Circulation 65: 134–140, 1982. [DOI] [PubMed] [Google Scholar]
- 9). McGregor M, Adam W, Sekelj P: Influence of posture on cardiac output and minute ventilation during exercise. Circulation Res 9: 1089–1092, 1961. [Google Scholar]
- 10). Wasserman K, Hansen JE, Sue DY, Whipp BJ: Principles of Exercise Testing and Interpretation, Chapter 3 (Japanese version). 1989, Nankodo, Tokyo, Japan, pp. 36–63. [Google Scholar]
- 11). Davey P, Meyer T, Coats A, Adamopoulos S, Casadei B, Conway J, Sleight P: Ventilation in chronic heart failure: effects of physical training. Br Heart J 68(5): 473–477, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Taniguchi K: Cardiopulmonary Exercise Testing, Chapter 3, O2 Kinetics and AT, 1993, Nankodo, Japan, pp. 155–164. [Google Scholar]
- 13). Weissman C, Askanazi J, Rosenbaum SH, Hyman AI, Milic-Emili J, Kinney JM: The effects of posture on the metabolic and ventilatory response to low level steady state exercise. Clin Sci 71(5): 553–558, 1986. [DOI] [PubMed] [Google Scholar]
- 14). Sackner JD, Nixon S, Davis B, Atkins N, Sackner MA: Effect of breathing through external dead space on ventilation at rest and during exercise. Am Rev Respir Dis 122(6): 933–940, 1980. [DOI] [PubMed] [Google Scholar]
- 15). Rea HH, Withy SJ, Seelye ER, Harris EA: The effects of posture on venous admixture and respiratory dead space in health. Am Rev Resp Dis 115: 571–579, 1977. [DOI] [PubMed] [Google Scholar]
- 16). Craig DB, Wahba WM, Don HF, Couture JG, Becklake MR: ‘Closing volume' and its relationship to gas exchange in seated and supine positions. J Appl Physiol 31(5): 717–721, 1971. [DOI] [PubMed] [Google Scholar]
- 17). Stokes DL, Macintyre NR, Nadel JA: Nonlinear increases in diffusing capacity during exercise by seated and supine subjects. J Appl Physiol: Respirat Environ Exercise Physiol 51(4): 858–863, 1981. [DOI] [PubMed] [Google Scholar]