Abstract
The present study aimed to clarify the effects of inspiratory muscle training (IMT) and expiratory muscle training (EMT) on ventilatory muscle strength, pulmonary function and responses during exercise testing. Young healthy women were randomly assigned to 3 groups: IMT (n=16); EMT (n=16); or untrained normal controls (NC, n=8). Subjects in the IMT and EMT groups trained for 15 minutes twice daily over 2 weeks at loads of 30% maximal inspiratory and expiratory muscle strength, respectively. Ventilatory muscle strength (maximal inspiratory and expiratory muscle strength; PImax and PEmax, respectively), pulmonary function and progressive exercise testing was performed. Both PImax and PEmax increased in the IMT group, and PEmax increased in the EMT group. Neither trained group demonstrated any change in pulmonary function or peak values during exercise testing. In the IMT group, exercise-induced increases in heart rate, oxygen uptake (VO2/kg) and rating of perceived exertion (RPE) decreased with training, as did increases in VO2/kg and RPE in the EMT group. The increased ventilatory muscle strength in both IMT and EMT groups might improve ventilatory efficacy during exercise, and increased inspiratory muscle strength might facilitate oxygen delivery through improved circulatory responses.
Keywords: inspiratory muscle training, expiratory muscle training, ventilatory muscle strength, exercise tolerance, dyspnea
Ventilatory muscle training (VMT) represents one component of respiratory rehabilitation1)2). The rationale behind VMT is that enhancing respiratory muscle function can potentially reduce the severity of breathlessness and improve exercise tolerance1). From evidence-based guidelines produced by a joint panel of the American College of Chest Physicians (ACCP) and the American Assoc ia tion of Cardiovascular and Pulmonary Rehabilitation (AACVPR)1), VMT may be considered for individual patients with chronic obstructive pulmonary disease (COPD) who remain symptomatic despite optimal therapy, although scientific evidence does not support routine use of VMT in pulmonary rehabilitation. After a meta-analysis of VMT by Smith and coworkers3), whose analysis was referred to in the evidence-based guidelines, Lötters and colleagues4) concluded that VMT significantly increases respiratory muscle strength and respiratory muscle endurance, decreases sensations of dyspnea at rest and during exercise, and tends to improve functional exercise capacity. Conversely, Salman and colleagues5) undertook meta-analysis, and concluded that VMT did not improve walking distance or sensation of dyspnea.
All the above studies of VMT referred to inspiratory muscle training (IMT). However, respiratory muscle fatigue is generated in both expiratory and inspiratory muscles6), and experiments have attempted to verify the effects of expiratory muscle training (EMT)7)8). Suzuki et al.7) reported that EMT increased expiratory muscle strength and decreased sensation of respiratory effort during exercise, and Akiyoshi et al.8) indicated that EMT increased both expiratory and inspiratory muscle strength.
To clarify the effects of EMT and IMT on ventilatory muscle strength measured by mouth pressure, pulmonary function and responses during exercise testing, both methods were examined in young healthy subjects.
Methods
Subjects
A total of 40 young healthy women participated in this study. Mean (± SD) age, height, weight and body mass index (BMI) were 19.3 ± 1.4 years, 158.7 ± 4.6 cm, 54.5 ± 7.6 kg and 21.6 ± 2.6 kg/m2 respectively. Subjects were randomly assigned to the IMT group (n=16), EMT group (n=16) or untrained normal control (NC) group (n=8). Informed consent was obtained from each subject. Table 1 presents characteristics and peak values during exercise testing for each group before the trial. No significant difference in age, physique, pulmonary function or peak values during exercise testing were observed among the three groups.
Table 1. Characteristics and peak values during exercise testing for each group at baseline.
| IMT group (n=16) | EMT group (n=16) | NC group (n=8) | ANOVA (significance) | |
|---|---|---|---|---|
| Age (years) | 18.8 ± 0.7 | 19.3 ± 1.0 | 20.4 ± 2.3 | N.S. |
| BMI (kg/m2) | 20.5 ± 1.4 | 22.7 ± 3.0 | 21.5 ± 2.8 | N.S. |
| PImax (cmH2O) | 68.6 ± 19.8 | 75.4 ± 18.6 | 76.1 ± 16.0 | N.S. |
| PEmax (cmH2O) | 68.6 ± 21.2 | 76.6 ± 18.6 | 72.8 ± 15.6 | N.S. |
| VC (l) | 3.2 ± 0.4 | 3.4 ± 0.4 | 3.3 ± 0.4 | N.S. |
| FEV1.0 (l) | 2.8 ± 0.5 | 3.0 ± 0.3 | 2.9 ± 0.3 | N.S. |
| Peak VE (l/min) | 37.3 ± 6.7 | 43.1 ± 8.9 | 38.9 ± 2.4 | N.S. |
| Peak TV (l) | 1.3 ± 0.2 | 1.4 ± 0.3 | 1.3 ± 0.3 | N.S. |
| Peak RR (breaths/min) | 29.3 ± 4.6 | 31.2 ± 4.5 | 31.0 ± 5.1 | N.S. |
| Peak VO2/kg (ml/kg/min) | 25.5 ± 3.7 | 26.4 ± 4.1 | 25.2 ± 3.4 | N.S. |
| Peak RPE | 6.8 ± 1.9 | 7.6 ± 2.4 | 6.3 ± 2.1 | N.S. |
mean ± SD, IMT; inspiratory muscle training, EMT; expiratory muscle training, NC; normal control, BMI; body mass index, PImax; maximal inspiratory pressure, PEmax; maximal expiratory pressure, VC; vital capacity, FEV1.0; forced expiratory volume in one second, VE; minute ventilation, TV; tidal volume, RR; respiratory rate, VO2/kg; oxygen uptake/body weight, RPE; rating of perceived exertion, N.S.; not significant.
Device for VMT
Subjects in the IMT group used Threshold-IMT (HealthScan, New Jersey, USA) (Fig. 1A). This device comprises a plastic tube incorporating a spring-loaded valve occluding the inspiratory orifice at one end and a mouthpiece at the other end. When the subject breathes through the mouthpiece, they must generate sufficient vacuum pressure to open the spring-loaded valve and initiate airflow; exhalation is unloaded. The amount of resistance can be adjusted by varying the compression of the spring-loaded valve. Adjustment from 7 cmH2O to 41 cmH2O is possible.
Fig 1.
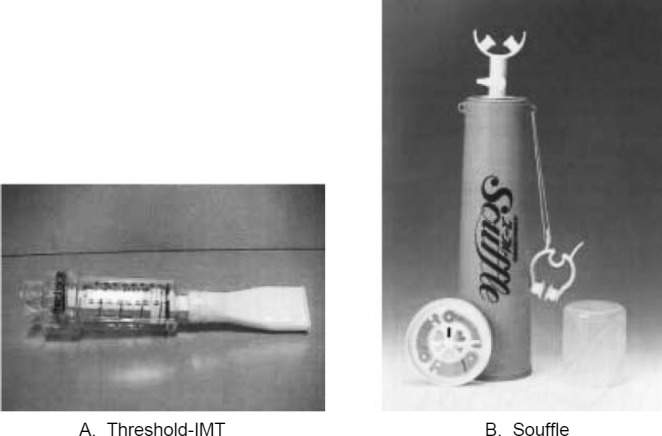
Training devices.
Subjects in the EMT group used Souffle (Kayaku, Tokyo, Japan) (Fig. 1B). This device comprises a central container with a dead space of 400 or 800 ml, a mouthpiece and a metal positive end-expiratory pressure (PEEP) plate elastic-loaded valve occluding the expiratory orifice. When subjects exhale through the mouthpiece they must generate positive pressure equivalent to 5, 10 or 15 cmH2O to open the PEEP plate elastic-loaded valve. As subjects re-inhale a portion of the expired gas in the container during inhalation, ventilation is promoted. The present study utilized the 800-ml container, adjusted to an appropriate pressure by modifying load pressure and measuring inner pressure of the Souffle during expiration using a manometer (Bird; 3M, Tokyo, Japan).
Experimental protocol
IMT subjects trained using a Threshold-IMT at 30% of maximal inspiratory muscle strength for 15 minutes twice daily. EMT subjects trained using Souffle at 30% of maximal expiratory muscle strength for 15 minutes twice daily. Training was continued for two weeks, and no training was undertaken by the NC group. Subjects in the two training groups predominantly performed under supervision by an examiner, and trained at home on holidays. After the trial period, a record of performance was made to indicate state of training.
Measurement of ventilatory muscle strength, pulmonary function testing (using spirometry) and progressive exercise testing were undertaken before and after training. Ventilatory muscle strength was measured using Vitalopower KH-101 equipment (Chest, Tokyo, Japan), and mouth pressure was considered as ventilatory muscle strength. According to the methods of Black and Hyatt9), subjects utilized a nose-clip and mouthpiece, and maintained inspiratory and expiratory effort against a closed valve at least 1 second from residual volume (RV) and total lung capacity (TLC), respectively. In addition, both efforts were measured at functional residual capacity (FRC). All efforts were repeated three times, with peak values recorded as maximal inspiratory and expiratory muscle strength (PImax and PEmax, respectively). Pulmonary function testing was performed using an Autospiro AS-300 electrical spirometer (Minato Medical Science, Osaka, Japan), using vital capacity (VC) and forced expiratory volume in one second (FEV1.0). Exercise tolerance testing involved a progressive walking exercise test on a treadmill (Rehabilitation Tread Mill; BIODEX, New York, USA). A modification of the 3MPH protocol by Balk10) was selected for the exercise testing protocol. This protocol was up to stage 7, with slope increasing every 2 minutes from 0% to 2%, 5%, 7%, 10%, 12% and 15% at a steady speed of 3 miles/hour after a 3-minute warm-up at 2 miles/hour. Subjects lay quietly on a platform for at least 20 minutes prior to exercise testing. The exercise test was performed after fitting a transmitter for electrocardiography (Life Scope 8; Nihon Kohden, Tokyo, Japan) and mask for an expiratory gas analyzer (Metabolic Measurement System 2900c; Sensor Medics, California, USA). Baseline data were measured in the standing position on the treadmill. Target heart rate was considered (220 − age) × 85%, and testing was ceased when target heart rate was reached. The air conditioner was set at 23°C, so the environmental temperature in the experiment room could be kept relatively constant.
Statistical analysis
All values were reported as mean ± SD. For ventilatory muscle strength (PImax and PEmax) and pulmonary function (VC and FEV1.0), pre- and post-training comparisons were analyzed using paired t-tests. Differences in changes with training between groups were analyzed using two-way repeated measures analysis of variance (ANOVA). Heart rate (HR), minute ventilation (VE), tidal volume (TV), respiratory rate (RR), oxygen uptake/body weight (VO2/kg) and rating of perceived exertion (RPE) using the Borg score11) were selected as parameters of exercise testing. For these parameters, comparisons of peak values between preand post-training were analyzed using paired t-tests, and differences in exercise-induced increases between pre- and post-training within each group were analyzed using two-way repeated measures ANOVA.
Results
The trained state in the training groups and the lifestyle in all subjects
Based on training state records, while of 28 times in the trial period, subjects were performing training 26.6 times on the average (range ; 24–28 times) in IMT group, and 27.1 times on the average (range ; 25–28 times) in EMT group. Those who have a movement custom from the investigation in question paper were one competition level and two recreation levels. The number of those with a smoking custom was eight. All subjects were reported to have been changeless to which lifestyle during the trial.
Changes in ventilatory muscle strength
Changes in ventilatory muscle strength with training are shown Table 2. In the NC group, neither PImax nor PEmax changed over the two weeks. In the IMT group, PImax differed significantly compared to that in the NC group (df 1, F=10.844, p<0.01), and had increased significantly from 68.6 ± 19.8 cmH2O to 79.7 ± 20.4 cmH2O (p<0.01). PEmax in the IMT group increased significantly from 68.6 ± 21.2 cmH2O to 73.6 ± 22.2 cmH2O (p<0.05). In the EMT group, PEmax increased significantly from 76.6 ± 18.6 cmH2O to 84.5 ± 22.1 cmH2O (p<0.05), whereas no changes in PEmax were observed compared to the NC group. PImax was unchanged in the EMT group.
Table 2. Change of ventilatiory muscle strength for ventilation muscle training.
| IMT group (n=16) | EMT group (n=16) | NC group (n=8) | ANOVA (interaction) | |
|---|---|---|---|---|
| PImax (cmH2O) | ||||
| Pre | 68.6 ± 19.8 | 75.4 ±18.6 | 76.1 ± 16.0 | |
| Post | 79.7 ± 20.4 | 81.4 ±17.9 | 78.0 ± 19.6 | p<0.01 |
| t test | p<0.01 | N.S. | N.S. | |
| PEmax (cmH2O) | ||||
| Pre | 68.6 ± 21.2 | 76.6 ± 18.6 | 72.8 ± 15.6 | |
| Post | 73.6 ± 22.2 | 84.5 ± 22.1 | 76.9 ± 11.4 | N.S. |
| t test | p<0.05 | p<0.05 | N.S. |
mean ± SD, IMT; inspiratory muscle training, EMT; expiratory muscle training, NC; normal control, PImax; maximal inspiratory muscle strength, PEmax; maximal expiratory muscle strength, N.S.; not significant.
Changes in pulmonary function
Changes in pulmonary function with training are shown in Table 3. In the NC group, changes were observed in neither VC (pre; 3.3 ± 0.4 l, post; 3.2 ± 0.4 l) nor FEV1.0 (pre; 2.9 ± 0.3 l, post; 2.9 ± 0.3 l) over the training period. In both trained groups, no changes in pulmonary function were identified compared to the NC group and pre- and post-training.
Table 3. Change of pulmonary function for ventilation muscle training.
| IMT group (n=16) | EMT group (n=16) | NC group (n=8) | ANOVA (interaction) | |
|---|---|---|---|---|
| VC (l) | ||||
| Pre | 3.2 ± 0.4 | 3.4 ± 0.4 | 3.3 ± 0.4 | |
| Post | 3.2 ± 0.4 | 3.4 ± 0.3 | 3.2 ± 0.4 | N.S. |
| t test | N.S. | N.S. | N.S. | |
| FEV1.0 (l) | ||||
| Pre | 2.8 ± 0.5 | 3.0 ± 0.3 | 2.9 ± 0.3 | |
| Post | 2.9 ± 0.5 | 3.1 ± 0.3 | 2.9 ± 0.3 | N.S. |
| t test | N.S. | N.S. | N.S. |
mean ± SD, IMT; inspiratory muscle training, EMT; expiratory muscle training, NC; normal control, VC; vital capacity, FEV1.0; forced expiratory volume in one second, N.S.; not significant.
Changes in peak values during exercise testing
In the NC group, peak values during progressive exercise testing were unchanged for all parameters: VE (pre; 38.9 ± 2.4 l, post; 39.5 ± 6.8 l); RR (pre; 31.0 ± 5.1 breaths/min, post; 29.8 ± 3.2 breaths/min); VO2/kg (pre; 25.2 ± 3.4 ml/kg/min, post; 24.5 ± 5.6 ml/kg/min); and RPE (pre; 6.3 ± 2.1, post; 6.4 ± 2.7). In both trained groups, no changes in peak values during exercise testing were observed compared to the NC group and pre- and post-training (Table 4).
Table 4. Change of peak values during exercise testing for ventilation muscle training.
| IMT group (n=16) | EMT group (n=16) | NC group (n=8) | ANOVA (interaction) | |
|---|---|---|---|---|
| Peak VE (l) | ||||
| Pre | 37.3 ± 6.7 | 43.1 ± 8.9 | 38.9 ± 2.4 | |
| Post | 39.2 ± 5.8 | 44.8 ± 7.0 | 39.5 ± 6.8 | N.S. |
| t test | N.S. | N.S. | N.S. | |
| Peak TV (l) | ||||
| Pre | 1.3 ± 0.2 | 1.4 ± 0.3 | 1.3 ± 0.3 | |
| Post | 1.4 ± 0.1 | 1.5 ± 0.3 | 1.3 ± 0.3 | N.S. |
| t test | N.S. | N.S. | N.S. | |
| Peak RR (breaths/min) | ||||
| Pre | 29.3 ± 4.6 | 31.2 ± 4.5 | 31.0 ± 5.1 | |
| Post | 28.9 ± 4.3 | 30.8 ± 6.0 | 29.8 ± 3.2 | N.S. |
| t test | N.S. | N.S. | N.S. | |
| Peak VO2/kg (ml/kg/min) | ||||
| Pre | 25.5 ± 3.7 | 26.4 ± 4.1 | 25.2 ± 3.4 | |
| Post | 25.9 ± 4.2 | 27.1 ± 3.2 | 24.5 ± 5.6 | N.S. |
| t test | N.S. | N.S. | N.S. | |
| Peak RPE | ||||
| Pre | 6.8 ± 1.9 | 7.6 ± 2.4 | 6.3 ± 2.1 | |
| Post | 6.1 ± 2.3 | 6.7 ± 2.0 | 6.4 ± 2.7 | N.S. |
| t test | N.S. | N.S. | N.S. |
mean ± SD, IMT; inspiratory muscle training, EMT; expiratory muscle training, NC; normal control, VE; minute ventilation, TV; tidal volume, RR; respiratory rate, VO2/kg; oxygen uptake/body weight, RPE; rating of perceived exertion, N.S.; not significant.
Changes in exercise-induced increases for parameters during exercise testing
Changes in exercise-induced increases for each parameter during progressive exercise testing are shown in Figs. 2–4. Since all subjects could reach stage 4, data up to this stage was analyzed. In the IMT group, magnitude of increases in HR decreased from pre- to post-training (df 5, F=2.503, p<0.05). In the other groups, no change in HR increases was identified (Fig. 2). Increases in ventilatory parameters (VE, RR and TV) during exercise were unchanged by training. In the IMT group, the magnitude of exercise-induced increases in VO2/kg decreased from preto post-training (df 5, F=2.693, p<0.05). In the EMT group, VO2/kg was lower at all stages in post-training compared with pre-training (df 1, F=5.584, p<0.05). In the NC group, no changes were identified (Fig. 3). Transitions of RPE decreased in both the IMT and EMT groups (df 1, F=4.201, p<0.05 and df 1, F=7.527, p<0.05, respectively) (Fig. 4).
Fig. 2.
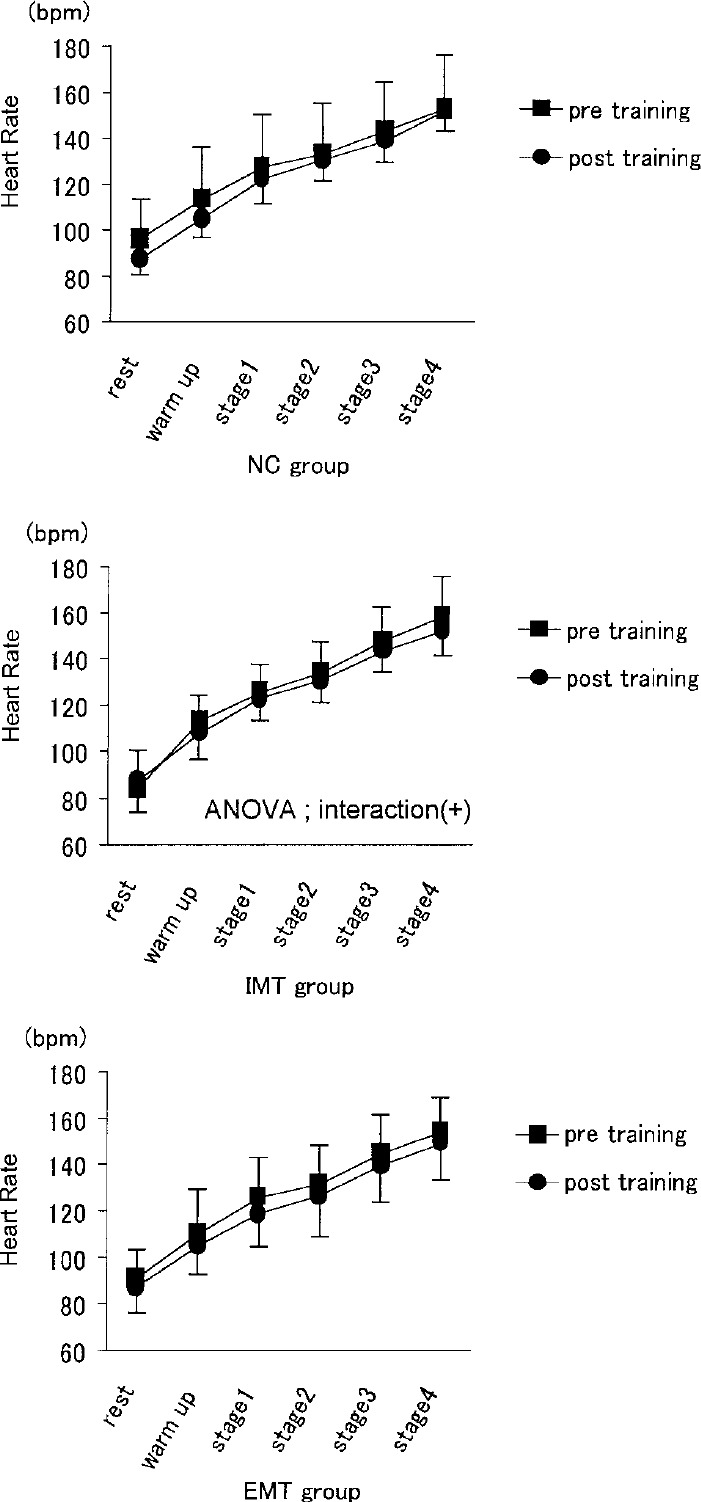
Change of heart rate increment during exercise testing for ventilation muscle training.
Fig. 4.
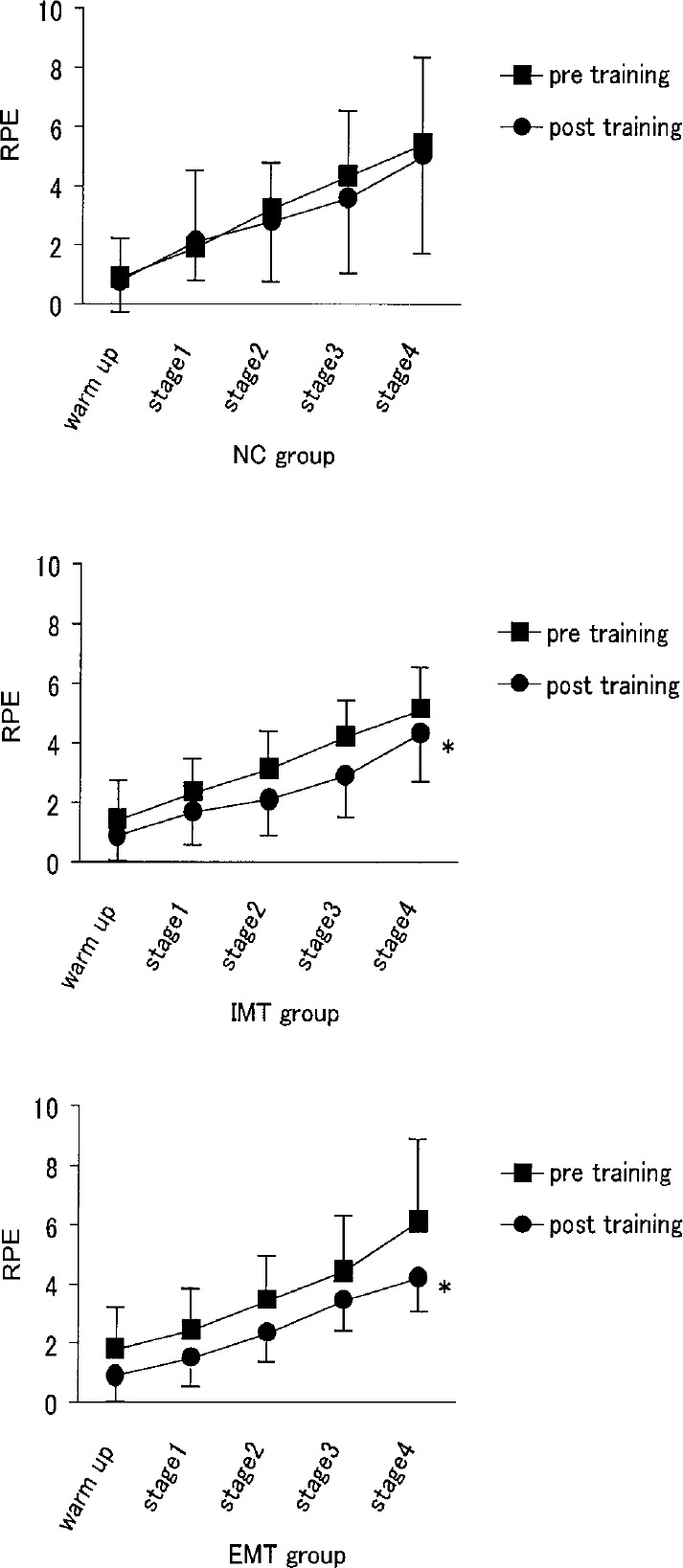
Change of rating of perceptive exertion (RPE) increment during exercise testing for ventilation muscle training. * p<0.05; comparison with increment during exercise testing at pre training.
Fig. 3.
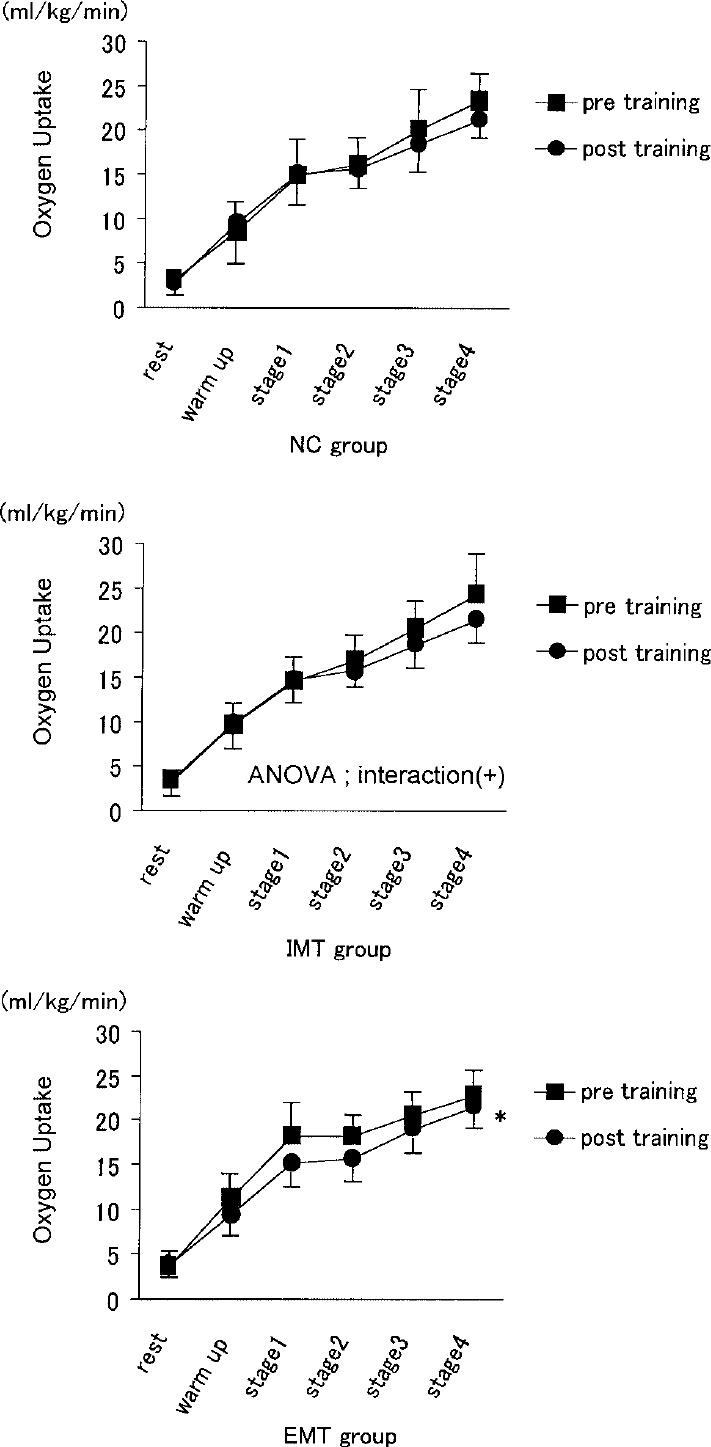
Change of oxygen uptake/body weight increment during exercise testing for ventilation muscle training. * p<0.05; comparison with increment during exercise testing at pre training.
Discussion
Both training methods were found to strengthen ventilatory muscles. In the IMT group, in which both inspiratory and expiratory muscles were strengthened, HR, VO2/kg and RPE at the same exercise intensity were decreased after training. In the EMT group, in which only expiratory muscles were strengthened, VO2/kg and RPE at the same exercise intensity were decreased after training, despite no change in HR.
Effect of ventilatory muscle strengthening
Inspiratory muscle training increased both inspiratory and expiratory muscle strength. Studies of patients with respiratory disease (including many with COPD) have variously reported that IMT does not12)13) and does14–20) strengthen inspiratory muscles. In a meta-analysis of 11 studies, Smith and coworkers3) concluded that inspiratory muscle training does not offer significant treatment effects. However, meta-analysis of only five of the 11 studies controlled for training flow rate found positive training effects. Joint guidelines in the USA1) have indicated that adequate training loads (i.e., intensity ≥30% of PImax) are needed acquire treatment effects. In the studies which found the effect of inspiratory muscle strengthening by IMT, patients trained for 30 minutes once15)16) or 15 minutes twice14)18)20) daily. Since the meta-analysis by Smith et al., most studies21–26) have revealed effects of increased inspiratory muscle strength, and a recent metaanalysis4) has established this effect. Also in the relative recent studies24–26), the training setting was prescribed at 30% or more of the maximal inspiratory muscle strength for 30 minutes once or 15 minutes twice daily.
In patients with COPD, no increases in expiratory muscle strength have been found with IMT12)18)26). A study of healthy subjects by Akiyoshi et al.8) reported that no significant change was observed in expiratory muscle strength following IMT for two weeks at 30% of PImax, although expiratory muscle strength increased by about 18 cmH2O. Sato and colleagues27) found expiratory muscle strength significantly increased by about 39 cmH2O after IMT for three weeks at 40% of PImax. Intercostal interni muscles, which are generally considered muscles of expiration, also function in inspiration during forced ventilation. In the present study, depth expiration reached to approximately RV may have been promoted at introduction of inspiration during training. This effect, which would not be expected in patients with COPD due to increased compensatory participation of muscles assisting ventilatory and pulmonary hyperinflation, could probably appear in healthy individuals.
In our study, only expiratory muscle strength increased after EMT, whereas inspiratory muscle strength was unchanged. Akiyoshi and coworkers8) revealed that EMT significantly increases not only expiratory but also inspiratory muscle strength. This may be attributable to the function of abdominal muscles in inspiration, as well as expiration8)27). EMT did not increase inspiratory muscle strength in studies by Suzuki et al.7) and Sato et al.27), in which training was performed at 30% or 40% of PEmax for four weeks, respectively.
Influence of VMT on pulmonary function
Most studies15)18)19)28) have reported that IMT does not influence pulmonary function in patients with respiratory disease. Meta-analysis3) confirmed this, and subsequent studies21)23)25) found that pulmonary function was unaffected if inspiratory muscle strength was also increased. These reports correspond to our results.
The effect of EMT on pulmonary function was examined in healthy subjects. In all three studies investigating this effect7)8)27), EMT leading to increased ventilatory muscle strength exerted no influence on pulmonary function. Again, these results correspond to our data.
Influence of VMT on exercise tolerance and dyspnea
Many studies16)18)20–24) have stated that exercise tolerance and dyspnea during exercise can be improved by increasing ventilatory muscle strength. A recent metaanalysis4) concluded that VMT improves dyspnea during exercise and may tend to increase exercise capacity. Many subsequent studies25)26) have also demonstrated that increased ventilatory muscle strength improves exercise tolerance. Wanke et al.23) analyzed expiratory gases during exercise testing, and found that VO2max during bicycle ergometry increased with increased inspiratory muscle strength. Conversely, most studies14)15)19)25) have found that peak values of expiratory gas data during exercise testing remain unchanged. Suzuki and coworkers7) examined the effects of EMT on exercise capacity. In their report, VO2 at each stage tended to decrease and Borg scale at each stage was decreased during progressive exercise testing. Findings such as these are basically in accordance with the results of the present study.
In relation to mechanisms behind the effects of increased ventilatory muscle strength on exercise capacity and dyspnea in patients with respiratory disease, Wanke et al.23) suggested that conditioning of the respiratory muscles might enable patients to tolerate higher PaCO2 levels, and improved inspiratory muscle performance might increase ventilatory efficacy for physiological dead space/tidal volume (VD/VT). Furthermore, Larson et al.16) suggested that IMT might desensitize patients to fear of dyspnea, while Preusser et al.22) considered that IMT might improve ventilatory limitation during endurance exercises in patients. However, since these mechanisms do not apply to the subjects of the present study, who were healthy individuals, other factors were considered responsible, such as improved neuromuscular coordination16), changes to ventilatory patterns24), reduced inspiration time and longer expiration time7)16), and delayed ventilatory muscle fatigue20).
In our study, the magnitude of HR increases with increasing exercise intensity reduced following IMT. As this result was likely associated with reduced VO2/kg increases, exercise load might be assumed to decrease through reduced oxygen demand with improvements in ventilatory efficacy. However, EMT did not influence HR, despite reduced oxygen demand during exercise. As a contrast between the two types of VMT, we consider that strengthening inspiratory muscles might increase intra-thoracic negative pressure during exercise, while stroke volume increases with improved venous return, thus contributing to reduced HR following IMT.
Limitations of the present study
Subjects in this study were selected young healthy women, because we thought that it was easy to recruit them as participants in our study. They were students of a physical and occupational therapy school whose male-to-female ratio of students was about 1:4. In patients with respiratory disease, however, there are more males than females and most of them are elder. Healthy subjects could take effects by training term only for two weeks. But patients with respiratory disease will need the longer training period in order to acquire the training effects. In addition, the effects of VMT on respiratory muscle strengthening may differ by healthy subjects and patients, since ventiratory phase in total lung capacity is not same in both subjects during VMT.
Another limitation is the difference between both subjects of the mechanism to which the effects of ventiratory muscle strengthening affects the responses during exercise testing. Generally, it is unthinkable that a healthy individual's exercise limitation factors are abnormality of artery blood gas, alveolar hypoventilation, fear of dyspnea and so on. We mentioned above, when the factors of change of the responses during exercise testing by VMT might be an improvement of respiratory efficacy. In this study, however, since we could not present data of respiratory pattern and ventiration cycle during exercise, thus was still a matter of conjecture.
We are confident that the further study for respiratory disease patients will prove the result of this study.
Conclusion
We examined the effects of IMT and EMT on ventilatory muscle strength, pulmonary function and responses during exercise testing in young healthy subjects. Both types of training increased ventilatory muscle strength, but did not affect pulmonary function or peak values during exercise testing. However, significant reductions were observed in HR, VO2/kg and RPE at same load during exercise testing after IMT, and in VO2/kg and RPE after EMT. Increased ventilation muscle strength might improve ventilatory efficacy during exercise in both IMT and EMT, and increased inspiratory muscle strength might facilitate oxygen delivery through advantageous circulation responses.
References
- 1). ACCP/AACVPR pulmonary rehabilitation guidelines panel: Pulmonary rehabilitation: joint ACCA/AACVPR evidencebased guidelines. Chest 112: 1363-1396, 1997. [PubMed] [Google Scholar]
- 2). Siafakas NM, Vermeire P, Pride NB, Paoletti P, Gibson J, Howard P, Yernault JC, Decramer M, Higenbottam T, Postma DS, Rees J: Optimal assessment and management of chronic obstructive pulmonary disease (COPD): a consensus statement of the European Respiratory Society (ERS). Eur Respir J 8: 1398-1420, 1995. [DOI] [PubMed] [Google Scholar]
- 3). Smith K, Cook D, Guyatt GH, Madhavan J, Oxman AD: Respiratory muscle training in chronic airflow limitation: a meta-analysis. Am Rev Respir Dis 145: 533-539, 1992. [DOI] [PubMed] [Google Scholar]
- 4). Lötters F, van Tol B, Kwakkel G, Gosselink R: Effects of controlled inspiratory muscle training in patients with COPD: a meta-analysis. Eur Respir J 20: 570-576, 2002. [DOI] [PubMed] [Google Scholar]
- 5). Salman GF, Mosier MC, Beasley BW, Calkins DR: Rehabilitation for patients with chronic obstructive pulmonary disease: meta-analysis of randomized controlled trials. J Gen Intern Med 18: 213-221, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Suzuki S, Suzuki J, Ishii T, Akahori T, Okubo T: Relationship of respiratory effort sensation to expiratory muscle fatigue during expiratory threshold loading. Am Rev Respir Dis 145: 461-466, 1992. [DOI] [PubMed] [Google Scholar]
- 7). Suzuki S, Sato M, Okubo T: Expiratory muscle training and sensation of respiratory effort during exercise in normal subjects. Thorax 50: 366-370, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Akiyoshi F, Takahashi H, Sugawara K, Satake M, Shioya T: The effect of expiratory muscle training on respiratory muscle strength. Rigaku Ryohogaku, 28: 47-52, 2001. (In Japanese). [Google Scholar]
- 9). Black LF, Hyatt RE: Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 99: 696-702, 1969. [DOI] [PubMed] [Google Scholar]
- 10). Naughton J, Haider R: Method of exercise testing. In: Naughton JP, Hellerstein HK. (eds) Exercise Training in Coronary Heart Disease. Academic Press, 1973, pp 79-91. [Google Scholar]
- 11). Borg G: Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med 2: 92-98, 1970. [PubMed] [Google Scholar]
- 12). Goldstein R, Rosie JD, Long S, Dolmage T, Avendano MA: Applicability of a threshold loading device for inspiratory muscle testing and training in patients with COPD. Chest 96: 564-571, 1989. [DOI] [PubMed] [Google Scholar]
- 13). Guyatt G, Keller J, Sinser J, Halcrow S, Newhouse M: Controlled trial of respiratory muscle training in chronic airflow limitation. Thorax 47: 598-602, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Asher MI, Pardy RL, Coates AL, Thomas E, Macklem PT: The effects of inspiratory muscle training in patients with cystic fibrosis. Am Rev Respir Dis 126: 855-859, 1982. [DOI] [PubMed] [Google Scholar]
- 15). Chen H, Dukes R, Martin BJ: Inspiratory muscle training in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 131: 251-255, 1985. [DOI] [PubMed] [Google Scholar]
- 16). Larson Jl, Kim MJ, Sharp JT, Larson DA: Inspiratory muscle training with a pressure threshold breathing device in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 138: 689-696, 1988. [DOI] [PubMed] [Google Scholar]
- 17). Belman MJ, Shadmehr R: Targeted resistive ventilatory muscle training in chronic obstructive pulmonary disease. J Appl Physiol 65: 2726-2735, 1988. [DOI] [PubMed] [Google Scholar]
- 18). Harver A, Mahler DA, Daubenspeck JA: Targeted inspiratory muscle training improves respiratory muscle function and reduces dyspnea in patients with chronic obstructive pulmonary disease. Ann Intern Med 111: 117-124, 1989. [DOI] [PubMed] [Google Scholar]
- 19). Flynn MG, Barter CE, Nosworthy JC, Pretto JJ, Rochford PD, Pierce RJ: Threshold pressure training, breathing pattern, and exercise performance in chronic airflow obstruction. Chest 95: 535-540, 1989. [DOI] [PubMed] [Google Scholar]
- 20). Dekhuijzen PNR, Folgering HTM, van Herwaarden CLA: Target-flow inspiratory muscle training during pulmonary rehabilitation in patients with COPD. Chest 99: 128-133, 1991. [DOI] [PubMed] [Google Scholar]
- 21). Weiner P, Azgad Y, Ganam R: Inspiratory muscle training combined with general exercise reconditioning in patients with COPD. Chest 102: 1351-1356, 1992. [DOI] [PubMed] [Google Scholar]
- 22). Preusser BA, Winningham ML, Clanton TL: High- vs low-intensity inspiratory muscle interval training in patients with COPD. Chest 106: 110-117, 1994. [DOI] [PubMed] [Google Scholar]
- 23). Wanke T, Formanek D, Lahrmann H, Brath H, Wild M, Wagner C, Zwick H: Effects of combined inspiratory muscle and cycle ergometer training on exercise performance in patients with COPD. Eur Respir J 7: 2205-2211, 1994. [DOI] [PubMed] [Google Scholar]
- 24). Lisboa C, Muñoz V, Beroiza T, Leiva A, Cruz E: Inspiratory muscle training in chronic airflow limitation: comparison of two different training loads with a threshold device. Eur Respir J 7: 1266-1274, 1994. [DOI] [PubMed] [Google Scholar]
- 25). Riera HS, Rubio TM, Ruiz FO, Ramos PC, Otero DDC, Hernandez TE, Gomez JC: Inspiratory muscle training in patients with COPD: effect on dyspnea, exercise performance, and quality of life. Chest 120: 748-756, 2001. [DOI] [PubMed] [Google Scholar]
- 26). Covey MK, Larson JL, Wirtz SE, Berry JK, Pogue NJ, Alex CG, Patel M: High-intensity inspiratory muscle training in patients with chronic obstructive pulmonary disease and severely reduced function. J Cardiopulm Rehabil 21: 227-230, 2001. [DOI] [PubMed] [Google Scholar]
- 27). Sato M, Satake M, Shioya T, Sugawara K, Takahashi H, Sato K, Kawatani M: The study on effective load pressure for the respiratory muscle training. Rigaku Ryohogaku 29: 37-42, 2002. (In Japanese). [Google Scholar]
- 28). Noseda A, Carpiaux JP, Vandeput W, Prigogine T, Schmerber J: Resistive inspiratory muscle training and exercise performance in COPD patients: a comparative study with conventional breathing retraining. Bull Eur Physiopathol Respir 23: 457-463, 1987. [PubMed] [Google Scholar]


