Abstract
We investigated the changes of an 8-week cardiac rehabilitation (CR) program on physiological outcomes and health-related quality of life (HRQL) in Japanese cardiac surgery patients. Subjects were 47 consecutive outpatients (32 men, 15 women; mean age 59.4 ± 12.6 years) recovering from cardiac surgery. Patients performed both aerobic exercise on a treadmill at anaerobic threshold intensity and moderate resistance training 2 days per week, 60 min per session, from 1 to 3 months after cardiac surgery. Differences in the eight SF-36 subscale scores and physiological outcomes within the patient group at 1 month and at 3 months after cardiac surgery were analyzed. Peak oxygen uptake, handgrip strength, and knee extension strength were used as physiological outcome measures. HRQL was assessed with the Japanese version Medical Outcome Study Short Form 36 (SF-36). Significant change in overall physiological outcome from 1 month to 3 months was observed. There was also significant change in seven of the eight SF-36 health status subscale scores (physical functioning, role-physical, bodily pain, general health, vitality, role-emotional, and mental health). However, with the exception of physical functioning and mental health scores, values did not reach those of the average healthy Japanese. In conclusion, we found that CR exercise training for Japanese cardiac surgery patients during the recovery phase changes not only physiological outcomes but also HRQL as assessed by the SF-36.
Keywords: cardiac rehabilitation, health-related quality of life, cardiac surgery
Cardiac rehabilitation (CR) is an established treatment in patients who have undergone cardiac surgery. CR is designed to provide a range of lifestyle and medical interventions to reduce cardiac mortality and morbidity through promotion of a healthy lifestyle and reduction of coronary artery disease risk factors1)2). Stern et al.3) reported a positive effect of improving exercise tolerability through aerobic exercise therapy in convalescing cardiac patients, and the beneficial effects have been made clear by many researchers4)5). Muscle strength exercise, is also reported to have a beneficial effect. There are many the reports with the 20 to 30% training strength improvement of 40 to 50% of the maximum muscle force6)7). The scientific reasons are given in detail in the CR guidelines published by the Agency for Health Care Policy and Research (AHCPR) on the effect of improved exercise tolerance and the effect of enhanced muscle strength1). In addition, Yamasaki et al.8) described for the useful training that combined muscle strength training and aerobic exercise for myocardial infarction patients and reported that the effect was similar to that obtained by other researchers9). Therefore, convalescence exercise therapy that combines muscle strength training and reinforcement aerobic exercise therapy for cardiac patients, is a useful method of CR exercise therapy.
Another important objective of CR is improvement in health-related quality of life (HRQL). Reports from many countries discuss HRQL in relation to CR10–13). Several studies have examined HRQL in patients with coexisting acute myocardial infarction (AMI), cardiac surgery, and heart failure10)12). Jette et al.10) reported an association between heart disease and reduced HRQL. Morrin et al.12) studied CR patients who had completed baseline, 3-, and 6-month evaluations of coronary risk factors, and HRQL outcomes showed various rates of improvement. Recent studies indicate that participation in CR improves not only physiological HRQL factors but also psychological HRQL factors in patients with AMI and a coronary artery bypass graft (CABG)14).
No reports exist on the combined changes of strength training and aerobic exercise on HRQL in Japanese patients, i.e., in patients whose cultural background likely differs from that of Western patients.
Therefore, the purpose of the present study was to determine 1) the change of an 8-week CR program on physiological outcomes and HRQL and 2) the relations between the percentages of change in physiological outcomes and the eight subscale scores of HRQL at 3 months in comparison to 1 month in Japanese patients after cardiac surgery.
Methods
Study design and subjects
This was a prospective observational study. Study patients were selected from among 157 consecutive patients who were admitted to St. Marianna University School of Medicine Hospital for evaluation after cardiac surgery between July 1999 and November 2002. Of these 157 patients, 73 who completed exercise testing and an HRQL test 1 month after cardiac surgery and a routine 4-week CR program while still hospitalized were included in the study. The remaining 84 patients were excluded because they did not complete the exercise test due to cerebrovascular disease, an orthopedic disorder, severe heart failure, or STsegment changes or because they experienced uncontrolled arrhythmia during the 4-week CR program. We first offered the 73 outpatients the chance to participate in an 8-week recovery phase CR program after the 4-week CR program. The outpatients chose either to participate in the recovery phase CR program or to undergo physiological and HRQL examinations without undergoing exercise training. All study outcomes were determined at 1 month and 3 months after cardiac surgery. Twenty-two of the 73 outpatients quit of their own accord for reasons unrelated to the study. Four outpatients were excluded from the analysis because their Japanese version Medical Outcome Study Short Form 36 (SF-36) scores were incorrect. Thus, a total of 47 outpatients were included in the analysis (Fig. 1). We evaluated several outpatient characteristics, including age, sex, body mass index (BMI), education (<12 yrs. vs ≥12 yrs.), marital status, and primary diagnosis.
Fig. 1.
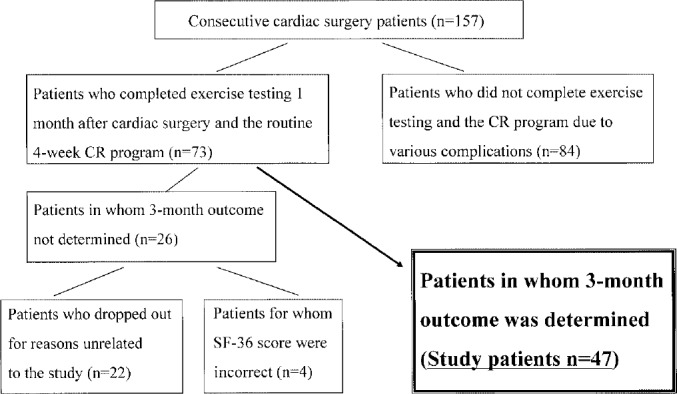
Extraction of the subject in this study.
Ethical matters
The study protocol was approved by the St. Marianna University School of Medicine Institutional Committee on Human Research. The aim of the study and the protocol were explained to each patient or an appropriate family member by a member of the health care staff. The protocol was also presented in detail in written form, and signature was obtained 1 month after cardiac surgery.
Study Protocol
Exercise capacity
All subjects underwent cardiopulmonary exercise testing (CPX) under a ramp treadmill protocol 1 month after cardiac surgery15). Peak oxygen uptake ( O2) as an index of exercise capacity was determined. Direct measures of expired gases were used as indices of cardiovascular dynamics during exercise. CPX was performed on two occasions, at 1 month and at 3 months after cardiac surgery. Symptom-limited exercise testing was performed on a MAT-2500 treadmill (Fukuda Denshi Co., Tokyo, Japan). Patients rested initially for 2 minutes sitting and 1 minute standing on the treadmill. Exercise began with a 3-minute warm-up (speed, 1.0 mph; gradient, 0%), which was followed by an increase in the load (speed or gradient) every 60 seconds. Throughout the test, 12-lead continuous ECG monitoring was performed, and heart rate (HR) was measured from the R-R interval (ML-5000, Fukuda Denshi Co.). Systolic blood pressure was determined by the cuff method via an automatic blood pressure monitor (Stress Test System, STBP-780, Colin Co., Aichi, Japan) at 1-minute intervals. V. O2, carbon dioxide production (
O2) as an index of exercise capacity was determined. Direct measures of expired gases were used as indices of cardiovascular dynamics during exercise. CPX was performed on two occasions, at 1 month and at 3 months after cardiac surgery. Symptom-limited exercise testing was performed on a MAT-2500 treadmill (Fukuda Denshi Co., Tokyo, Japan). Patients rested initially for 2 minutes sitting and 1 minute standing on the treadmill. Exercise began with a 3-minute warm-up (speed, 1.0 mph; gradient, 0%), which was followed by an increase in the load (speed or gradient) every 60 seconds. Throughout the test, 12-lead continuous ECG monitoring was performed, and heart rate (HR) was measured from the R-R interval (ML-5000, Fukuda Denshi Co.). Systolic blood pressure was determined by the cuff method via an automatic blood pressure monitor (Stress Test System, STBP-780, Colin Co., Aichi, Japan) at 1-minute intervals. V. O2, carbon dioxide production ( CO2), minute ventilation (
CO2), minute ventilation ( E), tidal volume (TV), end tidal CO2 (ETCO2), and the ventilatory equivalent for CO2 (
E), tidal volume (TV), end tidal CO2 (ETCO2), and the ventilatory equivalent for CO2 ( E/
E/ CO2) were measured throughout the exercise period with an AE-300S AERO Monitor (Minato Ikagaku Co., Tokyo, Japan). The measurement system for CPX was carefully calibrated before the start of each test. Expired gas was sampled breath-by-breath. The endpoint of exercise testing was determined according to the criteria of the American College of Sports Medicine16). The appearance of a leveling-off of
CO2) were measured throughout the exercise period with an AE-300S AERO Monitor (Minato Ikagaku Co., Tokyo, Japan). The measurement system for CPX was carefully calibrated before the start of each test. Expired gas was sampled breath-by-breath. The endpoint of exercise testing was determined according to the criteria of the American College of Sports Medicine16). The appearance of a leveling-off of  O2 (
O2 ( O2 plateau despite increased exercise intensity) assisted in determination of the exercise endpoint. Ventilatory equivalents for O2 (
O2 plateau despite increased exercise intensity) assisted in determination of the exercise endpoint. Ventilatory equivalents for O2 ( E/
E/ O2) and CO2 (
O2) and CO2 ( E/
E/ CO2) and the gas exchange ratio (GER) (
CO2) and the gas exchange ratio (GER) ( CO2/
CO2/ O2) were calculated on a personal computer (Pentium 98 SE, EPSON Co., Nagano, Japan). Anaerobic threshold (AT) was determined by the original V-slope method17) as well as conventionally by determining the point at which
O2) were calculated on a personal computer (Pentium 98 SE, EPSON Co., Nagano, Japan). Anaerobic threshold (AT) was determined by the original V-slope method17) as well as conventionally by determining the point at which  E/
E/ O2 increases after holding constant or decreases while
O2 increases after holding constant or decreases while  E/
E/ CO2 remains constant or decreases and by determining the period at which GER starts to increase steeply18).
CO2 remains constant or decreases and by determining the period at which GER starts to increase steeply18).
Handgrip strength measurement
A standard adjustable-handle JAMAR dynamometer (Bissell Healthcare Co., Michigan, USA) was used for measuring of handgrip strength as an index of upper limb muscle power and was set at the second grip position for all subjects. To measure grip strength, subjects were seated with their shoulder adducted and neutrally rotated, elbow flexed at 90°, forearm in the neutral position, and wrist between 0° and 30° of dorsiflexion and between 0° and 15° of ulnar deviation19). Attention was paid to a possible Valsalva effect, and measurements were made three times each on both the right and left hands. We used the highest value measured as the index of handgrip strength.
Knee extension strength measurement
The Biodex System 2 isokinetic dynamometer (Biodex Medical Systems, Inc., New York, NY, USA) was used to measure knee extension strength as an index of lower limb muscul strength. The machine was calibrated at the start of the study.
Patients were tested in the seated position with hip flexion at 80°, and stabilization straps were applied to the trunk, waist, and thigh. The resistance pad was placed at 10 cm proximal to the medial malleolus. Range of motion during testing was set between 0 and 90° of knee flexion, and all limbs were gravity compensated. All patients performed three submaximal and one maximal warm-up repetition at test speed prior to testing20). Testing was performed at a maximum of 5 repetitions at isokinetic speeds of 60°/sec. Isokinetic test results were analyzed with Biodex System 2 software. We measured the extension peak torque per body weight of both knees and used the highest value as the index of leg strength.
HRQL
General HRQL was measured with the SF-36. The SF-36 consists of 36 items representing 8 subscales that cover physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. The SF-36 is a standardized, generic HRQL measurement instrument that has been validated in the general Japanese population21)22). The eight subscale scores range from a possible 0 to 100, with lower scores indicating poorer and higher scores indicating better levels of function. The completed SF-36 questionnaires were scanned by computer and scored by the Public Health Research Foundation (Tokyo, Japan)23). The subscales scores were converted into a deviation score adjusted for age and sex based on scores of the general Japanese population, which was a mean of 50 with a standard deviation of 1024). In the present study, a score < 50 indicated that the health concept represented by the score was under the Japanese national normal after adjustment was made for age and sex23).
CR program
CR involved an interdisciplinary team approach to rehabilitation and included a cardiologist, nurse, physical therapist, dietician, and pharmacist. Because our hospital does not have a psychologist on staff, we do not help individual patients with stress management. In the acute phase of CR, diet and medication instructions were given to each inpatient at discharge by a dietician and pharmacist, respectively. In addition, inpatients received individual instruction at discharge from a nurse regarding cardiovascular risk factors and smoking cessation. Patient instruction was also performed in the outpatient setting.
In our hospital, physical therapists play a central role in supervising muscle strength and aerobic exercise training in the exercise component of the acute and recovery phases of CR. Various members of the staff took the patient's history, conducted cardiovascular physical examinations, prescribed exercise and training, evaluated cardiovascular risk factors and lab data, and assessed learning needs24).
Exercise therapy in the recovery phase of CR was based on the results of CPX and muscle strength testing and on the rating of perceived exertion ascertained at the end of the acute phase of the inpatient CR program. After baseline testing, outpatients participated in a supervised combined aerobic and resistance exercise program that met twice weekly for 1 hour. Exercise sessions comprised a warm-up period, aerobic exercise, resistance training, and a cooldown period24).
Exercise intensity was maintained at the AT heart rate level during aerobic treadmill exercise. For resistance training, 4 sets of a series of 2 upper extremity exercises (shoulder flexion and abduction from anatomical position) were performed with an array of iron weights at a resistance level that allowed completion of 5 repetitions with a perceived exertion rating of 11 to 13 on the Borg 6 to 20 scale25). Four sets of a series of knee extensions and calf raises were performed for lower extremity exercises. Knee extension was performed with weights strapped to the ankle and resistance that allowed completion of 5 repetitions performed at 50% of the 1 repetition maximum. Exercise intensity during calf raises was maintained at a perceived exertion rating of 11 to 13 on the Borg 6 to 20 scale25) that allowed completion of 5 repetitions. Each session was preceded and followed by a series of upper and lower extremity and body stretches (Table 1). Cardiac medications were continued on the day of the exercise test. CR treatment involved an interdisciplinary team approach to rehabilitation. The team included a cardiologist, nurse, physical therapist, dietician, and pharmacist. Diet and medication instructions were given to each patient at discharge by the dietician and pharmacist, respectively. In addition, patients received individual instruction at discharge from the nurse regarding both cardiovascular risk factors related to heart disease, and smoking cessation24).
Table 1. Cardiac rehabilitation program.
| Warm-up (20 minutes) | Stretch gymnastics (upper and lower limbs) | |||
| Muscle strength exercises 5 repetitions × 4 sets | ||||
| Shoulder flexion and abduction exercises | ||||
| tool: iron weight | ||||
| exertion rating: 11 to 13 on the Borg | ||||
| Knee extension | ||||
| tool: weights strapped | ||||
| intensity: 50% of the 1 repetition maximum | ||||
| Calf raises | ||||
| exertion rating: 11 to 13 on the Borg | ||||
| Aerobic exercise (25 minutes) | Treadmill walking | |||
| warm-up | 2.0 miles × 2 minutes | |||
| aerobic training | anaerobic threshold heart rate ± 5 bpm × 20 minutes | |||
| cool-down | 1.7–2.0 miles × 3 minutes | |||
| Cool-down (15 minutes) | Stretch gymnastics (upper and lower limbs) | |||
Frequency: Twice a week for 8 weeks. bpm, beat per minute.
Statistical analysis
All data were expressed as mean ± SD. Differences in the eight SF-36 subscale scores and physiological outcomes within the patient group at 1 month and at 3 months after cardiac surgery were analyzed by Wilcoxon signed rank test. Relations between the percentages of change in physiological outcomes and the eight subscale scores at 3 months in comparison to 1 month were tested by Pearson correlation coefficients. Statistical analyses were performed with SPSS 9.0J statistical software (SPSS Japan, Inc., Tokyo, Japan), and a p value of < 0.05 was considered significant.
Results
Patient characteristics
Mean age, sex, BMI, education, marital status, and primary diagnosis of subjects are shown in Table 2.
Table 2. Characteristics of study patients (n=47).
| Mean age ± SD (yr) | 59.4 ± 12.6 |
| Sex ratio (M/F) | 32/15 |
| BMI (kg/m2) | 21.6 ± 2.8 |
| Education (<12 yrs. vs ≥12 yrs.) | 12/35 |
| Married (%) | 89 |
| Primary condition | |
| CABG | 32 |
| Valve replacement | 15 |
Numbers are the number of patients unless otherness indicated. BMI, body mass index. CABG, coronary artery bypass graft.
Physiological outcomes
Exercise capacity: The endpoint of the exercise test was leg fatigue, shortness of breath, attainment of the target HR, or GER ≥ 1.20. No patient showed ischemic ST changes or experienced chest pain or serious arrhythmia during exercise testing. Significant improvement in peak  O2 was noted at 3 months versus 1 month in all cases (p<0.05, Table 3).
O2 was noted at 3 months versus 1 month in all cases (p<0.05, Table 3).
Table 3. Changes in Peak  O2, hand grip strength, and knee extension strength.
O2, hand grip strength, and knee extension strength.
| 1 month | 3 months | % change | z statistic | |
|---|---|---|---|---|
Peak  O2 (ml/kg/min) O2 (ml/kg/min) |
20.0 ± 3.5 | 24.1 ± 5.1* | 20.5 | −5.010 |
| Hand grip strength (kg) | 31.3 ± 8.3 | 33.9 ± 9.0* | 8.3 | −2.367 |
| Knee extension strength (Nm/kg) | 1.6 ± 0.4 | 1.9 ± 0.4* | 18.8 | −4.866 |
Mean ± SD values are shown.  O2, peak oxygen uptake.
O2, peak oxygen uptake.
* p<0.05.
Muscle strength: Significant changes in handgrip strength and knee extension strength were noted at 3 months versus 1 month in all cases (p<0.05, Table 4). No patient showed ischemic ST changes or experienced chest pain or serious arrhythmia during muscle strength testing.
Table 4. Changes in health-related quality of life (SF-36 HRQL scores).
| SF-36 subscales | 1 month | 3 months | % change | z statistic |
|---|---|---|---|---|
| Physical functioning | 44.1 ± 10.0 | 50.5 ± 5.5** | 14.5 | −4.006 |
| Role-physical | 32.4 ± 15.6 | 43.0 ± 13.5** | 32.7 | −3.961 |
| Bodily pain | 39.0 ± 12.9 | 46.2 ± 10.8** | 18.5 | −2.980 |
| General health | 45.0 ± 9.4 | 49.1 ± 9.5** | 9.1 | −3.267 |
| Vitality | 41.2 ± 9.2 | 49.2 ± 7.9** | 19.4 | −4.153 |
| Social functioning | 36.7 ± 16.1 | 41.3 ± 12.0 | 12.5 | −1.619 |
| Role-emotional | 35.4 ± 14.8 | 47.5 ± 11.0** | 34.2 | −3.603 |
| Mental health | 42.6 ± 10.3 | 50.2 ± 7.4** | 17.8 | −4.278 |
Data are expressed as mean ± SD.
** p<0.01
HRQL: Statistically significant changes were detected at 3 months versus 1 month in the physical functioning, role-physical, bodily pain, general health, and vitality, role-emotional, and mental health subscales scores of all patients (Table 4). However, with the exception of the physical functioning and mental health scores, values did not reach those of average healthy Japanese.
Correlation between changes in physiological outcomes and HRQL
The relations between physiological outcomes and HRQL are shown for the total study group in Table 5-1,5-2. Only the peak  O2 value was weakly associated with the SF-36 physical functioning score (r=0.41; p<0.01). Muscle strength was not associated with any of the SF-36 subscale scores.
O2 value was weakly associated with the SF-36 physical functioning score (r=0.41; p<0.01). Muscle strength was not associated with any of the SF-36 subscale scores.
Table 5-1. Correlation between changes in physiological outcomes and HRQL.
| SF-36 subscales | Peak  O2 O2
|
Knee extension strength | Hand grip strength |
|---|---|---|---|
| Physical functioning | |||
| 1 month | 0.32* | −0.12 | −0.03 |
| 3 months | 0.11 | −0.06 | 0.07 |
| % Change | 0.41** | 0.02 | 0.19 |
| Role-physical | |||
| 1 month | 0.01 | −0.12 | 0.12 |
| 3 months | −0.13 | 0.02 | −0.12 |
| % Change | −0.18 | 0.08 | −0.11 |
| Bodily pain | |||
| 1 month | −0.03 | 0.12 | −0.08 |
| 3 months | −0.14 | −0.25 | −0.28 |
| % Change | 0.00 | 0.14 | −0.03 |
| General health | |||
| 1 month | 0.21 | −0.16 | −0.13 |
| 3 months | 0.20 | −0.18 | 0.00 |
| % Change | 0.21 | −0.01 | −0.13 |
HRQL, health-related quality of life.  O2, peak oxygen uptake.
O2, peak oxygen uptake.
** p<0.01,
* p<0.05.
Table 5-2. Correlation between changes in physiological outcomes and HRQL.
| SF-36 subscales | Peak  O2 O2
|
Knee extension strength | Hand grip strength |
|---|---|---|---|
| Vitality | |||
| 1 month | −0.19 | −0.12 | −0.30* |
| 3 months | 0.17 | −0.18 | −0.20 |
| % Change | 0.19 | 0.02 | −0.03 |
| Social functioning | |||
| 1 month | −0.06 | 0.11 | −0.09 |
| 3 months | −0.15 | −0.01 | −0.11 |
| % Change | 0.08 | −0.05 | 0.07 |
| Role-emotional | |||
| 1 month | 0.05 | 0.24 | 0.20 |
| 3 months | 0.05 | 0.04 | 0.09 |
| % Change | −0.15 | 0.24 | 0.08 |
| Mental health | |||
| 1 month | −0.17 | −0.18 | −0.30 |
| 3 months | 0.05 | −0.30* | −0.18 |
| % Change | 0.12 | 0.22 | 0.08 |
HRQL, health-related quality of life.  O2, peak oxygen uptake. ** p<0.01,
O2, peak oxygen uptake. ** p<0.01,
* p<0.05
Discussion
This is the first time, to our knowledge, that physiological and HRQL outcomes have been evaluated in relation to moderate intensity resistance training and aerobic exercise training in Japanese patients after cardiac surgery. With regard to physiological outcomes, we found that peak  O2 values were significantly higher in patients at 3 months after cardiac surgery than at 1 month. Exercise capacity increased, indicating considerably improved physical capacity of a magnitude similar to that shown in another study of exercise training in coronary patients24). We also found that muscle strength, grip strength, and knee extension strength improved significantly; the average increase ranged from 8.3% to 16%. The results of our study were similar to the findings reported by Adams et al.26), who evaluated the effects and safety of 8-week muscle strength training combined with aerobic and resistance training in phase II CR patients. In their study, resistance training was performed by 61 phase II CR patients, and muscle strength of the upper and lower body increased from 8.6% to 25% with no abnormal cardiac response or orthopedic injury. These positive outcomes indicate that our CR program was appropriate. Positive improvement in physiological outcomes may enhance the ability of cardiac surgery patients to perform the activities of daily living and occupational tasks. The present study showed that positive effects could be attained with a relatively short-duration CR program.
O2 values were significantly higher in patients at 3 months after cardiac surgery than at 1 month. Exercise capacity increased, indicating considerably improved physical capacity of a magnitude similar to that shown in another study of exercise training in coronary patients24). We also found that muscle strength, grip strength, and knee extension strength improved significantly; the average increase ranged from 8.3% to 16%. The results of our study were similar to the findings reported by Adams et al.26), who evaluated the effects and safety of 8-week muscle strength training combined with aerobic and resistance training in phase II CR patients. In their study, resistance training was performed by 61 phase II CR patients, and muscle strength of the upper and lower body increased from 8.6% to 25% with no abnormal cardiac response or orthopedic injury. These positive outcomes indicate that our CR program was appropriate. Positive improvement in physiological outcomes may enhance the ability of cardiac surgery patients to perform the activities of daily living and occupational tasks. The present study showed that positive effects could be attained with a relatively short-duration CR program.
We also found that significant improvement in HRQL, as assessed by the SF-36 subscale scores, was shown by patients in terms of physical functioning, role-physical, bodily pain, general health, vitality, role-emotional, and mental health. Previous research27) showed a positive change in HRQL in cardiac patients (i.e., patients with AMI, CABG, or congestive heart failure) who participated in an intensive rehabilitation program in comparison to those who received only standard outpatient care. In the present study, significant physiological and HRQL change were observed. However, without comparisons with a control group, it was not possible to assess whether the 1- and 3-month changes were due to CR interventions. We did, however determine how soon the HRQL subscale scores returned to those of age- and sex-matched Japanese. As noted above, only two subscale scores reached the levels of their respective scores in the average healthy Japanese. Morrin et al.12) reported that SF-36 scores improved in cardiac patients throughout the course of the CR program and approached or reached the American norms by 6 months in most areas. In the present study, it was not possible to determine scores for periods longer than 3 months. In future trials, supervised exercise training should continue for longer periods.
Increased muscle strength is widely recommended for older persons because it benefits many aspects of physical health, performance of the activities of daily living, and psychological health28). Resistance training may also improve mood in depressed patients29). One study suggested that muscle strength is not associated with HRQL28). Results of the present study were similar to the above reported findings. In the present study, peak oxygen uptake correlated weakly with all measures of HRQL, except muscle strength.
Our facility is limited in that we can use only  O2 values as an index of physiological outcome and that the only correlation we observed was between
O2 values as an index of physiological outcome and that the only correlation we observed was between  O2 and one SF-36 subscale score. In addition, no mental health specialists in our facility are involved in CR, and doctors and physical therapists who perform exercise therapy do not communicate with the mental health specialists. Thus, more importance is placed on conventional CR and physiological outcomes than on HRQL, which cannot be verified. Furthermore, it has been reported that 1year is needed after cardiac surgery for SF-36 subscale scores of patients to return to normal12). Thus, in a study such as ours, the full change in HRQL can not be observed. However, in regard to this correlation, the estimate of the correlation value may have been low, and because amount of change is used, individual measured values can vary. In the future, detailed examination of this point is necessary.
O2 and one SF-36 subscale score. In addition, no mental health specialists in our facility are involved in CR, and doctors and physical therapists who perform exercise therapy do not communicate with the mental health specialists. Thus, more importance is placed on conventional CR and physiological outcomes than on HRQL, which cannot be verified. Furthermore, it has been reported that 1year is needed after cardiac surgery for SF-36 subscale scores of patients to return to normal12). Thus, in a study such as ours, the full change in HRQL can not be observed. However, in regard to this correlation, the estimate of the correlation value may have been low, and because amount of change is used, individual measured values can vary. In the future, detailed examination of this point is necessary.
According to Bandura30), if individuals lack self-efficacy they will likely behave ineffectually even if they know what to do and how to do it. For example, cardiac patients who previously developed exercise skills and were physiologically capable may lack the self-efficacy to maintain an independent long-term exercise program30). It has been suggested that changes in mood are mediated by self-efficacy rather than by actual physical performance31). Beniamini et al.32) studied 38 cardiac patients in whom various HRQL factors were assessed before and after completion of 12 weeks of either high intensity strength training or flexibility training that was added to the outpatient CR aerobic exercise program. Results of their study suggested increases in strength to be associated with enhanced self-efficacy and improved mood and HRQL32). In the present study, although these outcomes were not assessed specifically, improved HRQL could have been mediated by a change in self-efficacy. Improvements in exercise performance or in perceived self-efficacy might be responsible for the improvement in HRQL that we observed.
The present study was limited in several ways. It included only a small number of subjects who were not randomized to a 1- versus 3-month intervention. Oldridge et al.33) also reported on disease-specific HRQL after 8 weeks of CR exercise and counseling and found the greatest change to be between the start of training and 8 weeks, particularly with respect to emotional state, anxiety, disease-specific HRQL, and exercise capacity. Further studies are needed to evaluate how HRQL is altered by different types of CR programs after cardiac surgery and also in different cardiac populations.
Conclusions
In conclusion, we found that CR exercise training for Japanese cardiac surgery patients during the recovery phase changes not only physiological outcomes but also HRQL as assessed by the SF-36.
Acknowledgements
This study was supported in part by Grant-in-Aid for Scientific Research (A) # 13301006 from the Japanese Society for the Promotion of Science.
References
- 1). Agency for Health Care Policy and Research, and the National Heart, Lung and Blood Institute: “Cardiac rehabilitation”, AHCPR Publication No. 96-0672, 1995. [PubMed] [Google Scholar]
- 2). O'Connor GT, Buring JE, Yusuf S, et al. : An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation 80: 234-244, 1989. [DOI] [PubMed] [Google Scholar]
- 3). Stern MJ, Gorman PA, Kaslow P: The group counseling v exercise therapy study: a controlled intervention with subjects following myocardial infarction. Arch Intern Med 143: 1719-1725, 1983. [PubMed] [Google Scholar]
- 4). Foster C, Pollock ML, Anholm JD, et al. : Work capacity and left ventricular function during rehabilitation after myocardial revascularization surgery. Circulation 69: 748-755, 1984. [DOI] [PubMed] [Google Scholar]
- 5). Sebrechts CP, Klein JL, Ahnve S, et al. : Myocardial perfusion change following 1 year of exercise training assessed by thalium-201 circumferential count profiles. Am Heart J 112: 1217-1226, 1986. [DOI] [PubMed] [Google Scholar]
- 6). Haennel RG, Quinney HA, Kappagoda CT, et al. : Effects of hydraulic circuit training following coronary artery bypass surgery. Med Sci Sports Exerc 23: 158-165, 1991. [PubMed] [Google Scholar]
- 7). Kelemen MH, Stewart KJ, Gillilan RE, et al. : Circuit weight training in cardiac patients. J Am Coll Cardiol 7: 38-42, 1986. [DOI] [PubMed] [Google Scholar]
- 8). Yamasaki H, Yamada S, Tanabe K, et al. : Effects of weight training on muscle strength and exercise capacity in patients after myocardial infarction. J Cardiol 26: 341-347, 1995. [PubMed] [Google Scholar]
- 9). Satou S, Arakawa N, Kamata J, et al. : Changes in exercise tolerance and muscle strength in patients after cardiac surgery: introducing muscle training besides aerobic training at the early stage after cardiac surgery. J Jpn Phys Ther Assoc 29: 24-28, 2002. [Google Scholar]
- 10). Jette DU, Downing J: Health status of individuals entering a cardiac rehabilitation program as measured by the medical outcomes study 36-item short-form survey (SF-36). Phys Ther 74: 521-527, 1994. [DOI] [PubMed] [Google Scholar]
- 11). Lindsay GM, Hanlon WP, Smith LN, et al. : Experience of cardiac rehabilitation after coronary artery surgery: effects on health and risk factors. Int J Cardiol 87: 67-73, 2003. [DOI] [PubMed] [Google Scholar]
- 12). Morrin L, Black S, Reid R: Impact of duration in a cardiac rehabilitation program on coronary risk profile and healthrelated quality of life outcomes. J Cardiopulm Rehabil 20: 115-121, 2000. [DOI] [PubMed] [Google Scholar]
- 13). Ware JE, Jr, Sherbourne CD: The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 30: 473-483, 1992. [PubMed] [Google Scholar]
- 14). Hevey D, Brown A, Cahill A, et al. : Four-week multidisciplinary cardiac rehabilitation produces similar improvements in exercise capacity and quality of life to a 10-week program. J Cardiopulm Rehabil 23: 17-21, 2003. [DOI] [PubMed] [Google Scholar]
- 15). Izawa K, Tanabe K, Ishiguro T, et al. : Cardiopulmonary response abnormalities during exercise in patients with noninsulin-dependent diabetes-mellitus complicated acute myocardial infarction. Cardiovasc Rev Rep 22: 734-742, 2001. [Google Scholar]
- 16). Hanson P: Clinical exercise testing. In: American College of Sports Medicine, Resource Manual for Guidelines for Exercise Testing and Prescription. Philadelphia, Lea & Febiger, 1988, pp 205-222. [Google Scholar]
- 17). Beaver WL, Wasserman K, Whipp BJ: A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60: 2020-2027, 1986. [DOI] [PubMed] [Google Scholar]
- 18). Wasserman K, Hansen JE, Sue DY, et al. : Physiology of exercise. In: Principles of Exercise Testing and Interpretation. Philadelphia, Lea & Febiger, 1987, pp 3-26. [Google Scholar]
- 19). Mathiowetz V, Wiemer DM, Federman SM: Grip and pinch strength: norms for 6- to 19-year-olds. Am J Occup Ther 40: 705-711, 1986. [DOI] [PubMed] [Google Scholar]
- 20). Wilk KE, Romaniello WT, Soscia SM, et al. : The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther 20: 60-73, 1994. [DOI] [PubMed] [Google Scholar]
- 21). Fukuhara S, Ware JE, Jr, Kosinski M, et al. : Psychometric and clinical tests of validity of the Japanese SF-36 health survey. J Clin Epidemiol 51: 1045-1053, 1998. [DOI] [PubMed] [Google Scholar]
- 22). Fukuhara S, Bito S, Green J, et al. : Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 51: 1037-1044, 1998. [DOI] [PubMed] [Google Scholar]
- 23). Fukuhara S, Suzukamo Y, Bito S, et al. : Manual of SF-36 Japanese version 1.2. Tokyo Public Health Research Foundation, 2001. (in Japanese). [Google Scholar]
- 24). Izawa K, Hirano Y, Yamada S, et al. : Improvement in physiological outcomes and health-related quality of life following cardiac rehabilitation in patients with acute myocardial infarction. Circ J 68: 315-320, 2004. [DOI] [PubMed] [Google Scholar]
- 25). Borg G: Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14: 377-381, 1982. [PubMed] [Google Scholar]
- 26). Adams KJ, Barnard KL, Swank AM, et al. : Combined highintensity strength and aerobic training in diverse phase II cardiac rehabilitation patients. J Cardiopulm Rehabil 19: 209-215, 1999. [DOI] [PubMed] [Google Scholar]
- 27). Sledge SB, Ragsdale K, Tabb J, et al. : Comparison of intensive outpatient cardiac rehabilitation to standard outpatient care in veterans: effects on quality of life. J Cardiopulm Rehabil 20: 383-388, 2000. [DOI] [PubMed] [Google Scholar]
- 28). Stewart KJ, Turner MS, Bacher AC, et al. : Are fitness, activity, and fatness associated with health-related quality of life and mood in older persons? J Cardiopulm Rehabil 23: 115-121, 2003. [DOI] [PubMed] [Google Scholar]
- 29). Singh NA, Clements KM, Fiatarone MA: A randomized controlled trial of progressive resistance training in depressed elders. J Gerontol A Biol Sci Med Sci 52: M27-35, 1997. [DOI] [PubMed] [Google Scholar]
- 30). Bandura A: Self-efficacy mechanism in human agency. Am Psychol 37: 122-147, 1982. [Google Scholar]
- 31). Stewart KJ, Kelemen MH, Ewart CK: Relationships between self-efficacy and mood before and after exercise training. J Cardiopulm Rehabil 14: 35-42, 1994. [Google Scholar]
- 32). Beniamini Y, Rubenstein JJ, Zaichkowsky LD, et al. : Effects of high-intensity strength training on quality-of-life parameters in cardiac rehabilitation patients. Am J Cardiol 80: 841-846, 1997. [DOI] [PubMed] [Google Scholar]
- 33). Oldridge N, Gottlieb M, Guyatt G, et al. : Predictors of healthrelated quality of life with cardiac rehabilitation after acute myocardial infarction. J Cardiopulm Rehabil 18: 95-103, 1998. [DOI] [PubMed] [Google Scholar]


