Abstract
Purpose: The obstacle negotiation gait (ONG) is a fundamental activity of daily living. In cerebrovascular hemiplegic patients (stroke patients), the weight-bearing rate (WBR) on the paretic limb necessary for an independent ONG was studied. Methods: One hundred and seventeen stroke patients were involved. The patients' average age at the time of the study was 67 years, and the average time from stroke onset was 102 days. There were 68 men and 49 women. Seventy patients were right hemiplegics, and 47 were left hemiplegics. The correlations between ONG and age, sex, body mass index (BMI), time from stroke onset, muscle strength of both the paretic and non-paretic limbs, Brunnstrom stage of the lower limbs, deep sensation, and the WBR on both the paretic and non-paretic limbs were studied. Patients who could perform ONG independently and safely were categorized as the independent group (IG), and those who needed observation or any assistance were categorized as the dependent group (DG). Results: The BMI, muscle strength of both the paretic and non-paretic limbs, Brunnstrom stage of the lower limbs, deep sensation and the WBR for both the paretic and non-paretic limbs were significantly different between the IG and DG groups. In particular, the WBR on the paretic limb was found to correlate significantly with the ONG, and a WBR value of 80.5% on the paretic limb gave a clear cut-off value. Conclusion: Although multiple factors influenced the ONG of stroke patients, the WBR on the paretic limb was the most influential.
Keywords: weight-bearing rate, cerebrovascular hemiplegic patients, obstacle negotiation gait
The purpose of rehabilitation after stroke is to improve gait disorders to maximize the subject's function in the home and community1,2). The obstacle negotiation gait (ONG) is a fundamental activity of daily living. Foster reported that 10% of cerebrovascular hemiplegic patients (stroke patients) at home fell down because of a failure to negotiate obstacles3).
It has been found that older subjects and stroke subjects have smaller toe clearance than healthy subjects when crossing an obstacle4–5). However, independent ONG requires stable support and balance of the lower limbs, as well as toe clearance. Numerous studies have shown that muscle weakness is associated with poor gait and falls in older adults6–7). A study found significant associations between lower muscle strength and the ability of elderly individuals to cross obstacles8). In stroke patients, motor paralysis, sensory disturbance and muscle weakness interfere with balancing ability. Therefore, in addition to lower limb strength, balancing ability is necessary for independent ONG.
The weight-bearing rate (WBR) on the paretic limb as a measure of balance capacity has been shown to significantly correlate with Brunnstrom stage of the lower limbs, muscle strength of the paretic limb, and deep sensation9). Numerous reports describe the weight bearing status of stroke patients; the characteristics typically describe weight bearing asymmetries during comfortable stance, not the magnitude of weight bearing during efforts to maximally weight bear on the paretic lower limb10–12). A certain level of WBR on the paretic limb must be achieved to go up and down stairs stably13). This is also true with the ONG.
If the level of WBR on the paretic limb for independent ONG could be clarified, this would be useful information for physiotherapists selecting therapeutic exercises, and attaining the target value for the independent ONG becomes the motivation for participating in rehabilitation.
The purpose of this study was to determine the level of the WBR on the paretic limb that should be achieved for the ONG.
Methods
Participants
One hundred and seventeen stroke patients without a higher cortical function disorder were involved. All patients were able to maintain a standing position without any supporting devices. Informed consent was obtained from all patients. The average ± standard deviation (SD) age at the time of the study was 67.2 ± 11.1 (range, 33–88) years. There were 68 men and 49 women; 70 patients were right hemiplegics, and 47 were left hemiplegics. The average time ± SD from stroke onset was 101.9 ± 64.3 days.
Procedure
Age, sex, body mass index (BMI), time from stroke onset, muscle strength of both the paretic and non-paretic limbs, Brunnstrom stage of the lower limbs, deep sensation and the WBR on both the paretic and non-paretic limbs were the variables studied.
The WBR was taken using two commercially available scales (TANITA bathroom scales RAINBOW THA-528). Each scale has a precision of 1.0 kg, and the measurement range is 0–120 kg. The scales were placed side by side. The angle between the right and left feet was 15 degrees, and the distance between the two calcaneal regions was 10 cm. The patients were asked to stand evenly with one foot on each scale, and they were then asked to shift as much of their weight as possible to the non-paretic side and then to the paretic side, and to then hold that position stably for a minimum of 5 seconds. The scale measured the value (in 1-kg units) during which the patient stood still for 5 seconds. The WBR was defined as the percentage of the weight shown on each scale compared to the whole body weight.
To measure the muscle strength of the lower limb, quadriceps muscle strength was measured using a handheld dynamometer (ANIMA, µ-Tas MT-01)14). With the patients sitting upright on a mat platform, with both upper extremities crossing in front of the trunk, without back support, and keeping the knees flexed 90 degrees, the dynamometer was attached to the front of the distal crus. The patients were then asked to make a maximum isometric contraction of the quadriceps for 5 seconds, twice, with a time interval of more than 30 seconds. The stronger value (kgf) of the two was divided by the body weight, and this value (kgf/kg) was defined as the muscle strength of the lower limb.
Joint sensation was used as a measure of deep sensation. First, the patient's hip joint, knee joint and ankle were moved passively, and then the patient was asked to imitate the movements on the non-paralyzed side. Each joint was evaluated five times; a difference of up to 10 degrees in the joints was considered normal, while a difference of ≥ 11 degrees at least once was considered abnormal.
For obstacles, 10 wooden blocks, with dimensions of 10 × 10 × 55 cm3 each, were placed 50 cm apart on the floor. The height of the obstacle was set at 10 cm, because, in a standard Japanese house, a ridge about 10 cm high are constructed to prevent water leaking at the entrance to a bathroom or a lavatory15). The patients were asked to make five walking rounds at the usual speed, negotiating the obstacles. The patients who could do so independently and safely were categorized as the independent group (IG), and those who needed observation or any assistance by a staff member were the dependent group (DG).
The patients who could walk indoors independently and safely were evaluated as independent.
The differences between the IG and DG groups were compared using the t-test, the χ2 - test, and the Mann-Whitney U test. The usefulness of the WBR on the paretic limb for predicting an independent ONG was studied using a receiver operating characteristic (ROC) curve, and the cut-off value necessary for an independent ONG was determined. Predictability was evaluated using the sensitivity, false-positive rate (1-specificity), predictive accuracy, and the positive predictive value. The results were defined as being statistically significant when the possibility of error (p) was less than 5%.
Results
Of the 117 patients, 49 were categorized as IG and 68 as DG. Seventeen DG patients could walk independently indoors.
The results of the univariate analysis are shown in Table 1. There were no significant differences in age, sex and time from stroke onset between the IG and DG groups. The BMI, muscle strength of both the paretic and nonparetic limbs, Brunnstrom stage of the lower limbs, deep sensation and the WBR on both the paretic and non-paretic limbs were significantly different between the IG and DG groups (p<0.05).
Table 1. Comparison of valuables between IG and DG.
| IG (n=49) | DG (n=68) | p value | |
|---|---|---|---|
| Age (year) | 65.8 ± 11.7 | 68.3 ± 10.7 | 0.243a) |
| Sex (Male / female) (n) | 30/19 | 38/30 | 0.350b) |
| BMI (kg/m2) | 23.5 ± 3.9 | 22.1 ± 3.0 | 0.036a) |
| Time from stroke onset (day) | 96.3 ± 66.5 | 105.9 ± 63.4 | 0.431a) |
| Muscle strength of the paretic limb (kgf/kg) | 0.41 ± 0.17 | 0.22 ± 0.14 | 0.000a) |
| Muscle strength of the non-paretic limb (kgf/kg) | 0.52 ± 0.19 | 0.45 ± 0.15 | 0.031a) |
| Brunnstrom stage of lower limbs (n) | IV:2, V:11, VI:36 | II:3, III:18, IV:19, V:16, VI:12 | 0.000c) |
| Deep sensation (normal/ abnormal) (n) | 40/9 | 29/39 | 0.000b) |
| WBR on the paretic limb (%) | 89.7 ± 5.6 | 53.7 ± 21.9 | 0.000a) |
| WBR on the non-paretic limb (%) | 91.6 ± 5.8 | 86.0 ± 10.7 | 0.001a) |
NOTE. Values are mean ± SD or n.
t-test,
χ2- test,
Mann-Whitney U test
All patients with WBR>90% on the paretic limb and 71% of the patients with WBR ranging from 80–89% on the paretic limb were in the IG group. All patients with WBR<79% on the paretic limb were in the DG group.
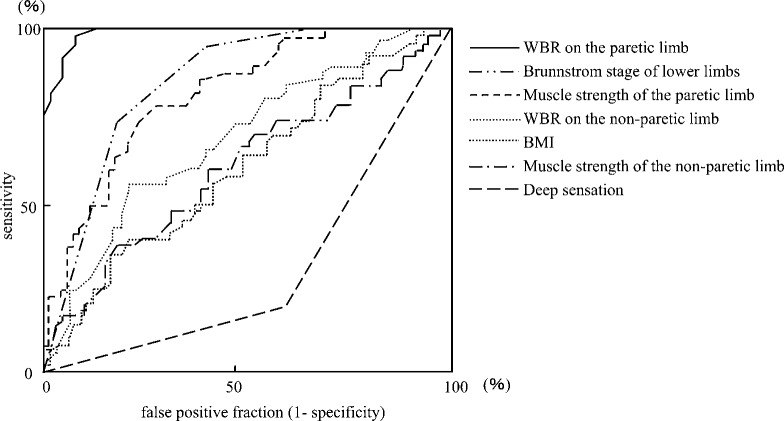
The results of the ROC curve analysis are shown in Fig. 1. The areas under the curve for the BMI, muscle strength of the paretic limb, muscle strength of the non-paretic limb, Brunnstrom stage of the lower limbs, deep sensation, WBR on the paretic limb and WBR on the non-paretic limb were 0.600, 0.812, 0.599, 0.847, 0.305, 0.989 and 0.686, respectively (p<0.05). A WBR of 80.5% on the paretic limb gave a clear cut-off value, with a sensitivity of 97.9%, a false-positive rate (1-specificity) of 7.6%, a predictive accuracy of 94.7%, and a positive predictive value of 97.9%.
Fig. 1.
ROC Curve for prediction of independence ONG
Discussion
In 117 stroke patients, age, sex, BMI, time from stroke onset, muscle strength of both the paretic and non- paretic limbs, Brunnstrom stage of the lower limbs, deep sensation, and the WBR on both the paretic and non-paretic limbs were examined. The correlations between these variables and the ONG were also studied in order to determine the cut-off value of the WBR on the paretic limb necessary for an independent ONG.
The ONG is one of the important activities that a stroke patient must achieve to be safely discharged home from the hospital. With normal elderly individuals, it has been reported that lower limb muscle strength correlates significantly with one leg standing time16); the stronger the muscle strength of the lower limb, the greater the balancing ability and the more successful the ONG. On the other hand, a stroke patient has not only weakened muscle strength but also impaired deep sensation and voluntary movements, which have more than a little influence on standing stability and decreasing the WBR on the paretic limb, making the ONG difficult.
The present study showed that the BMI, muscle strength of both the paretic and non-paretic limbs, Brunnstrom stage of the lower limbs, deep sensation and the WBR on both the paretic and non-paretic limbs were significantly different between the IG and DG groups. Analyzing the ROC curve, the WBR on the paretic limb was found to be the most useful factor for predicting an independent ONG. Although multiple factors influenced the ONG of stroke patients, the WBR on the paretic limb was the most influential.
We previously reported that a 71% WBR on the paretic limb gave a clear cut-off value for an independent indoor gait with a sensitivity of 93.3%, a false-positive rate (1-specificity) of 14.7%, a predictive accuracy of 89.9%, and a positive predictive value of 89.4%9). In the present study, no patients with a WBR < 79% on the paretic limb succeeded in the independent ONG, and 17 (25%) of the 68 independent indoor ambulant stroke patients in the DG group did not succeed in the independent ONG. This means that the ONG is more challenging than the usual indoor gait, and 71% WBR on the paretic limb would not guarantee an independent ONG, but an 80.5% WBR would.
Limitations: The results of our study are applicable only to patients without a higher cortical function disorder and to situations with obstacles less than 10 cm high.
Acknowledgements
We would like to thank all of the patients who participated for their cooperation.
References
- 1). Ingrid G, Gert K, et al. : Community ambulation in patients with chronic stroke: how is it related to gait speed? J Rehabil Med 40: 23-27, 2008. [DOI] [PubMed] [Google Scholar]
- 2). Goldie PA, Matyas TA, et al. : Deficit and change in gait velocity during rehabilitation after stroke. Arch Phys Med Rehabil 77: 1074-1082, 1996. [DOI] [PubMed] [Google Scholar]
- 3). Forster A, Young J: Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ 311: 83-86, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4). Chou L-S, Draganich LF: Stepping over an obstacle increases the motions and moments of the joints of the trailing limb in young adults. J Biomech 30: 331-337, 1997. [DOI] [PubMed] [Google Scholar]
- 5). Mc Fadyen BJ, Prince F: Avoidance and accommodation of surface height changes by healthy, community-dwelling, young, and elderly men. J Gerontol Ser 57: B166-174, 2002. [DOI] [PubMed] [Google Scholar]
- 6). Lord SR, Ward JA, et al. : Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc 42: 1110-1117, 1994. [DOI] [PubMed] [Google Scholar]
- 7). Rantanen T, Guralnik JM, et al. : Association of muscle strength with maximum walking speed in disabled older women. Am J Phys Rehabil 77: 299-305, 1998. [DOI] [PubMed] [Google Scholar]
- 8). Lamoureux EL, Sparrow WA, et al. : The relationship between lower body strength and obstructed gait in community-dwelling older adults. J Am Geriatr Soc 50: 468-473, 2002. [DOI] [PubMed] [Google Scholar]
- 9). Akezaki Y, Yamasaki H, et al. : Weight bearing ratio on affected lower extremity which is necessary for walking independence in hemiparetic stroke patients. Journal of kochi rehabilitation institute 8: 27-31, 2006. (in Japanese). [Google Scholar]
- 10). Bohannon RW: Gait performance of hemiparetic stroke patients: selected variables. Arch Phys Med Rehabil 68: 777-781, 1987. [PubMed] [Google Scholar]
- 11). Bohannon RW, Larkin PA: Lower extremity weight bearing under various standing conditions in independently ambulatory patients with hemiparesis. Phys Ther 65: 1323-1325, 1985. [DOI] [PubMed] [Google Scholar]
- 12). Winstein CJ, Gardner ER, et al. : Standing balance training: effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil 70: 755-762, 1989. [PubMed] [Google Scholar]
- 13). Akezaki Y, Yamasaki H, et al. : Relationship between weight bearing rate on the affected limb and an ability of going up and down stairs of the stroke patients. The Society of Physical Therapy Science 23: 301-305, 2008. (in Japanese). [Google Scholar]
- 14). Kato M, Yamasaki H, et al. : Measurements of isometric knee extension force with a hand-held dynamometer-Effect for interrater reliability using fixing-belt. Sogo Rihabiriteshon 29: 1047-1050, 2001. (in Japanese). [Google Scholar]
- 15). Shionaka M, Uematsu M, et al. : Gait in the elderly people at the house. Journal of Physical Therapy 18: 393-399, 2001. (in Japanese). [Google Scholar]
- 16). Kasahara M, Yamasaki H, et al. : Relationship between one leg standing time and knee extension strength in elderly patients. Jpn J Phys Fitness Sports Med 50: 369-374, 2001. (in Japanese). [Google Scholar]