Abstract
The objective of this study was to assess the effect of comprehensive exercise program widely accepted as a community-based physical intervention for the prevention of falling in the elderly persons on their controlling standing balance. Twenty-six community-dwelling elderly persons (13 males and females; 69.8 ± 2.8 years old) participated in this study. Daily exercise was comprised of walking for more than 30 min, stretching, muscle strengthening and balance exercise without exercise equipments. The intervention was continued for three months. Indicators of standing balance related to static balance, dynamic balance and postural response were measured before and after the intervention. As an effect of the intervention on static balance, the sway of center of pressure (COP) in the static stance significantly increased. In the dynamic balance, significant improvements were observed in one leg standing time, the 10-m gait time, functional reach. Additionally, the maximal movable length of COP which subjects can move voluntarily to right and left significantly increased. In the postural response, the integrated electromyography (IEMG) induced by postural response for sudden postural perturbation significantly decreased in the lower leg muscles. Since less muscular activities were sufficient to maintain posture, it was suggested that postural response was elicited more efficiently following the intervention. This study suggested that the comprehensive exercise program, which has been widely introduced as community-based interventions for the prevention of falling, have extensive effects on the control of standing balance covering static balance, dynamic balance and postural response in the elderly persons.
Keywords: standing balance, elderly person, physical activity
In recent years, falling has become the leading cause of injuries such as bone fractures in elderly persons, and can lead to their becoming bedridden or poor activities of daily living. Thus, various community-based activities have been introduced to prevent falling in elderly persons1).
Standing balance has been considered one of the important physical factors in falling. Therefore, any intervention that improves standing balance is an essential constituent of community-based interventions against falling2). Recent reports describe the efficiency of various exercises in the prevention of falling, such as muscle strengthening exercises, stretching of the muscles, dancing and Tai Chi Chuan3, 4).
Standing balance has been classified into three hierarchical phases: static standing balance; dynamic standing balance; and postural response5, 6). Static balance indicates postural stability in the static stance. Dynamic balance indicates the ability to control posture during active motion; i.e., keeping the center of pressure (COP) of the body mass within the allowable area of the base of support. In controlling dynamic balance, anticipatory postural adjustments are required. Anticipatory adjustments of the posture prepare a person's balance prior to or parallel to postural disturbance induced by any subsequent voluntary motion which follows. Thus, it is important to note that dynamic balance depends on an anticipatory feed-forward adjustment of the posture7–9). When the COP deviates beyond the allowable area in standing balance, the postural response of the whole body is elicited to return the COP to within the controllable area of the base of support10, 11). When this postural response does not function adequately, falling is inevitable. The postural response is therefore the final response acting to prevent falls.
Prevailing community-based intervention in the form of physical activity for elderly persons usually consists of various exercises such as aerobic exercises, muscle strengthening exercises, stretching and balance exercises. Imposed exercise, as a form of intervention, is generally comprehensive rather than focal12). So it is important to precise the effect of such comprehensive exercises on various aspects of standing balance, a prime inner factor of falling in elderly persons. The objective of this study was to clarify the effects of community-based, long-term intervention in the elderly, in the form of comprehensive physical activity, on standing balance composed of static balance, dynamic balance and postural response. We assessed the efficacy of the comprehensive exercise prevailing in community-based interventions for the improvement of balance control in elderly persons through our intervention.
Methods
Subjects
The health-up model project scheduled by the All-Japan Federation of National Health Insurance Organization started in 2001. The main purpose of this project was to prevent adult disease by promoting physical exercise. Kake City in Hiroshima Prefecture, Japan, was recruited as one of the model cities for this project. At first, the project in Kake City was scheduled as a medical follow-up based on biochemical examinations concerning adult disease. However, the aging population of Kake City was so high that not only the prevention of adult disease but also the improvement of motor function in elderly persons was expected as an effect of physical exercise. So the health and social welfare department of Kake City offered our group kinesiological assessment to elucidate the contribution of their comprehensive intervention to motor function especially in the standing balance of elderly participants. Thus, our kinesiological study was designed as an additional portion of the health-up model project based on biochemical examinations.
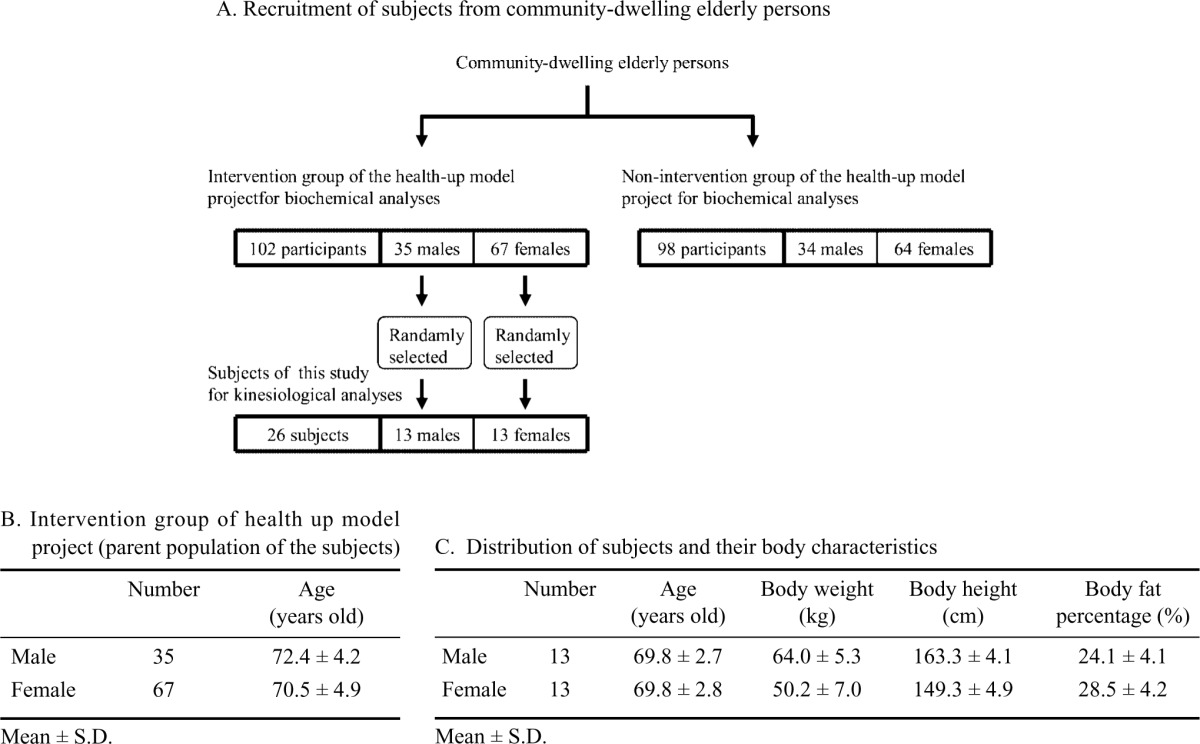
A hundred and two elderly persons were recruited from community-dwelling elderly persons as participants in the intervention group of the health-up model project as in Table1A. A corresponding number of elderly persons were also recruited as non-intervention group for the medical assessment in biochemical examinations by other research group in the health-up model project. Thus, we did not follow non-intervention group in our study. The criteria for the recruitment of intervention and non-intervention group in the health-up model project were as follows: 1) age of the participants was from 65 to 79 years old; 2) the participants had to be able to walk safely without the need of support; 3) the participants had no symptom of motor paresis, sensory deficits, vertigo or uncorrectable visual defects. The recruitment was announced in a public relations magazine published by the health and social welfare department of Kake City. The 102 elderly persons (71.1 ± 4.7 years old) that served as the intervention group were composed of thirty-five males (72.4 ± 4.2 years old) and sixty-seven females (70.5 ± 4.9 years old) as shown in Table 1A and 1B. Respectively, twenty-six elderly persons consisting of thirteen males (69.8 ± 2.7 years old) and the same number of females (69.8 ± 2.8 years old) were selected randomly as the subjects of our study from each gender population of the elderly intervention group to assess the effect of intervention on kinesiological sites as shown in Table 1A and 1C. The 102 participants in the intervention group including the 26 subjects of our study attended the same physical intervention for three months. In this study, our group took charge of the kinesiological assessment of 26 subjects for the initial 3 months, respectively.
Table 1. Recruitment of twenty-six subjects who participated in the community-based physical exercise and kinesiological assessment in standing balance.
 |
Since the ratio between male and female subjects finally recruited for this study was not identical to that in their parent population, the result of this study may not appreciate the effect of the intervention on the parent population. However, by avoiding unbalance in the ratio of gender of the subjects, it is possible to deduce the more general tendency of the intervention effect, regardless of the difference in gender. Participation described above was strictly voluntary. Informed consent was obtained, and subjects signed a document stating that they were not forced to participate and that they could cease participating at any time. All ethical processes concerning this study were accepted by a committee composed of members of Kake City, Kokuho Kake City Hospital and other outside committees.
Intervention in physical activities in elderly persons
The intervention of this study, overlapping that of the health-up model project constituted a twice-monthly meeting of subjects for group program and daily home exercises for three months. Subjects attended a group program held twice a month by health and social welfare workers, which was aimed at preventing falling. Three groups were made up of approximately 30 elderly persons. In this program, subjects practiced the exercises in Table 2 in the presence of an athletic trainer for one hour. The exercise program consisted of stretching, muscle strengthening, and balance exercises. Most exercises were performed slowly in a sitting or standing position while holding something for support. The light load of exercises was based on individual weight. As the home exercise, in addition to exercises III and IV in Table 2, we asked subjects to walk for more than 30 min at their usual pace every day. Exercise regimens were continued for three months.
Table 2. Physical exercises introduced as daily home exercise to the subjects in the group program.
| I. Abdominal breathing exercise for approximately 15 min |
| II. Preparatory active stretching of the whole body for approximately 20 min |
| III. Muscle strengthening and balance exercises for approximately 20 min While sitting on a chair While standing with the hands on the backrest of a chair |
IV. Approach to the plantar
|
a total of eight times each side.
Subjects were asked to complete a questionnaire every day to determine whether they were actually carrying out these exercises. This questionnaire was checked at their next meeting with the athletic trainer. Days attended was divided by six (total days of the program) to calculate the attendance rate of a participant at the twice-monthly program. To calculate the degree of attainment of home exercise, the number of the days when a subject did the home exercise was divided by the number of total days for three months. The average attendance rate at the program was 94.5% and the degree of attainment of home exercise was on average 83.0%.
Measurement of standing balance
The following parameters concerning standing balance were measured to assess the effect of the physical activities before our intervention and once again three months later.
Static standing balance: In order to assess static standing balance, the COP was measured during static stance using a force plate (MG-100, ANIMA Co. Ltd., Tokyo, Japan). Subjects stood on the force plate with their eyes open and their arms relaxed at their sides, and the COP was measured for 30 sec just one time. The COP was also measured, in the same way, in subjects with their eyes closed just one time. The total length of the trajectory of COP (excursion of COP) was calculated, and the ratio of the length with eyes closed to that with eyes open was also calculated (Romberg's ratio).
Dynamic standing balance: It has been reported that the Berg Balance Scale (BBS) composed of 14 active movement tests correlates to the incidence of falling13). The score of each test of BBS is graded to four levels. However, the subjects in our study achieved an almost perfect score in every BBS test because the physical level of the subjects was too high to be evaluated by the four grades of BBS. We therefore selected the following tests from BBS that were easier to quantify: 1) one leg standing time (OLS)13) and 2) functional reach13,14). Additionally, we measured 3) the 10-m gait time, 4) the maximal step length and 5) the timed up and go test (TUG)15). Conventionally OLS has been used in the category of static standing balance. However, OLS requires anticipatory postural adjustment prior to raising one leg8), and postural perturbation induced by raising one leg can trigger shortening of OLS in some cases. So it can be reasonable to place OLS into the category of dynamic balance. OLS and functional reach was measured according to the method of BBS13), although the imposed time in OLS was limited to 30 sec. In the measurement of the maximal step length, the vertical distance between the tip of the great toe of one foot and that of the opposite side was measured in maximal step. Just a time of OLS13), functional reach13, 14) and the maximal step length were analyzed for right side respectively. Functional reach and the maximal step length were normalized for the height of the subject. 10-m gait time was measured at normal and fastest speed just one time. For measurement of the 10-m gait time, subjects were asked to walk once at their usual and at their fastest speed for 20 m. The time required to walk the intermediate 10 m was recorded as 10 m gait time. In the measurement of TUG15), the experimenter showed the subjects how to perform this process prior to the trial and asked them to do it as fast as possible followed by just one measurement.
In addition, the voluntarily movable lengths of COP forwards, backwards, to the right and to the left were measured just one time for each direction. Subjects stood on the force plate (situated on our original platform for postural sway), and moved their COP to each direction as far as possible. The soles of their feet were placed in a specific position on the force plate during the measurement. As a marker of the foot positions, two linear lines were drawn on the force plate. The length between the starting points of the lines was 10 cm. Each line was inclined at 10 degrees to the fore direction. To reproduce the initial stance, subjects placed the center of each heel at the staring point of the line and each hallux on the line. The maximal movable length of COP to each direction was measured just one time.
Postural response: Postural sway was induced by fore-aft horizontal perturbation of our original platform with a force plate as in the method of Nashner and Horak10, 11). Trials consisted of five forward and five backward perturbations of the platform (100 mm/sec, 50 mm in each direction). Prior to each perturbation, subjects were asked to place their soles according to the lines drawn on the force plate as mentioned above. Subjects looked at a fixed marker in front of them, and COP was monitored to be consistent with that of the initial stance in the previous trial. The sequences of trials were randomized, so that subjects could not anticipate the direction and onset of the next perturbation. There was a break of one minute between each trial. Forward postural sway induced by backward perturbation of the platform was extensively smaller compared with the reverse one due to the support by the foot length. Thus, we analyzed backward postural response induced by forward perturbation of the platform respectively.
Postural responses were assessed based on the analyses of COP and electromyography (EMG). Surface EMG was measured for the tibia anterior muscle (TA), rectus femoris muscle (RF), gastrocnemius muscle (GAS) and interior hamstrings muscle (HAM) of the right lower leg. Each subject was fitted with surface electrodes (Vitrode disposable electrodes; NIHON KODEN Co., Ltd., Tokyo, Japan) spaced 2 cm apart on each muscle. Impedance of the skin was adjusted so that it was lower than 5 kohm. EMG signals were filtered (time constant of low cut is 0.03 s and high cut is 200 Hz) and full-wave rectified using an amplifier (RMP-6004M; NIHON KODEN Co., Ltd., Tokyo, Japan). Excursion of the COP was also measured from force plate, without filtration. All EMG and COP data were sampled at 2 kHz using a PowerLab system (PowerLab/8 s, AD Instruments Japan Inc., Nagoya, Japan). From the COP data, maximal movement of the COP from the initial stance (COP excursion) and period required to reach maximal movement after the onset of perturbation of the platform (COP recovery time) were measured. In the EMG data, the integrated value of EMG (IEMG) for one second from the activation of the muscle was measured and normalized by that of a steady state in isometric maximal contraction.
All EMG and COP data were analyzed using wave-analyzing software (Chart v4.0.4; AD Instruments Japan Inc., Nagoya, Japan). An average value of five trials was calculated in each parameter regarding COP and EMG.
Statistical analysis
In this study, we assessed the effect of our program composed of physical activity on each category of standing balance, static balance, dynamic standing balance, and postural response5,6) by comparing the paired data between pre- and post-intervention. Thus, the statistical significance of differences in measured parameters before and after intervention was assessed using the paired t-test. A p value less than 0.05 indicated statistical significance. All data in Table 3 were shown in average ± standard deviation.
Table 3. The effect of the intervention on standing balance in elderly persons.
| Before intervention | After intervention | p value | ||
|---|---|---|---|---|
| Static balance | ||||
| Excursion of COP with eyes open (mm) | 12.3 ± 4.3 | 20.8 ± 5.3 | p<0.001* | |
| Excursion of COP with eyes closed (mm) | 18.3 ± 7.9 | 26.8 ± 9.9 | p<0.001* | |
| Romberg's ratio | 1.54 ± 0.37 | 1.31 ± 0.34 | p<0.01* | |
| Dynamic standing balance | ||||
| BBS | 55.6 ± 0.8 | 55.6 ± 1.0 | 1 | |
| OLS (s) | 24.4 ± 8.1 | 24.7 ± 9.0 | 0.417 | |
| Functional reach (%) | 19.8 ± 2.4 | 21.4 ± 2.9 | p<0.05 * | |
| 10-m gait time: normal speed (s) | 7.16 ± 0.82 | 6.40 ± 0.73 | p<0.001 * | |
| 10-m gait time: the fastest speed (s) | 5.53 ± 0.55 | 5.11 ± 0.45 | p<0.001 * | |
| The maximal step length (%) | 64.9 ± 7.1 | 66.3 ± 7.0 | 0.142 | |
| TUG (s) | 7.52 ± 0.97 | 7.29 ± 0.67 | 0.233 | |
| Movable length of COP (mm) | forward | 72.6 ± 15.6 | 72.6 ± 17.4 | 0.959 |
| backward | 50.7 ± 19.1 | 58.9 ± 9.7 | 0.096 | |
| right | 57.2 ± 15.1 | 65.0 ± 13.4 | p<0.05 * | |
| left | 60.3 ± 16.9 | 64.6 ± 28.0 | p<0.05 * | |
| Postural response | ||||
| COP excursion (mm) | 72.0 ± 9.6 | 63.6 ± 22.2 | 0.061 | |
| COP recovery time (ms) | 384 ± 50 | 384 ± 52 | 0.882 | |
| TA IEMG | 0.307 ± 0.131 | 0.241 ± 0.083 | p<0.01 * | |
| RF IEMG | 0.271 ± 0.224 | 0.181 ± 0.131 | p<0.05 * | |
| GAS IEMG | 0.650 ± 0.418 | 0.792 ± 0.803 | 0.35 | |
| HAM IEMG | 0.158 ± 0.121 | 0.102 ± 0.084 | p<0.05 * | |
All data were shown in mean ± S.D. of 26 subjects. COP, center of pressure; BBS, Berg balance scale; OLS, one leg standing time; TUG, timed up and go test; TA, tibia anterior muscle; RF, rectus femoris muscle; GAS, gastrocnemius muscle; HAM, interior hamstrings muscle; IEMG, the integrated electromyography.
Results
Effect of intervention on static standing balance
Movements of COP both with eyes open and closed increased following intervention unexpectedly. Furthermore, Romberg's ratio, which reflects dependency on visual feedback in static balance, decreased following the intervention (Table 3).
Effect of intervention on dynamic standing balance
Many quantifiable items of dynamic standing balance were improved as a result of the intervention (Table 3). 10-m gait times both at normal and the fastest speed were significantly shortened following the intervention. Functional reach also significantly increased following the intervention. Furthermore, the movable length of COP increased significantly in lateral directions.
Effect of intervention on postural response
In the effects of intervention on postural response induced by forward perturbation of the platform (Table 3), significant change was not detected in COP data, whereas IEMG of agonist muscles (TA and RF) and antagonist muscle (HAM) decreased following the intervention.
Discussion
Our results indicate that the intervention, in the form of comprehensive physical exercise, has effects on various aspects of standing balance in elderly persons covering static balance, dynamic balance and postural response.
While a randomized controlled trial is preferable to detect the effect of any intervention, this study is limited to elderly persons participating in the intervention. Additionally, the subjects of this study were limited to healthy elderly persons whose physical activity was relatively good as described in the recruitment of subjects and shown in the result of BBS. However, within such limitations, our results showed that the comprehensive exercises widely accepted in the program for elderly persons can affect multilaterally on controlling standing balance.
Effect of intervention on static standing balance
It has been widely accepted that the smaller the postural sway is, the better the static standing balance is. We, therefore, expected the decrease of postural sway in static stance following the intervention. Contrary to our expectation, movements of COP both with eyes open and closed increased following the intervention (Table 3), suggesting the increase of postural sway in static stance as the result of intervention. A report16) describes similar results to ours regarding the increased sway of COP as the result of physical exercises for the prevention of falling in elderly persons. Thus, we suppose that the increase of postural sway in static stance is, in fact, acquired function meaningful for controlling static balance as an effect of physical exercises. However, further studies are required to elucidate its physiological meaning.
Furthermore, Romberg's ratio, which reflects dependency on visual feedback in static balance, decreased following the intervention (Table 3), suggesting that vestibular or somatosensory feedback came to be substituted for visual feedback in static stance through the intervention. We adopted exercises that focused on the plantar aspect of the foot as in exercise IV in Table.2. It has been reported that such an approach to the plantar results in an increase in the sensitivity of the plantar mechanoreceptors, making afferent input from such proprioceptive sensors more efficient17). We suggest that the introduction of such a plantar foot exercise may be contributed to the facilitation in the dependency of somatosensory feedback from the plantar foot.
Effect of intervention on dynamic standing balance
We found that many indicators of dynamic standing balance were improved following the intervention. Every indicator for dynamic standing balance in this study requires voluntary movements controlled by the higher central nervous system. These voluntary demands accompany anticipatory postural control, prior to or parallel to voluntary movements. These voluntary movements and complimentary anticipatory postural responses function as a feed forward system to control the COG7–9). Thus, we suppose that the physical exercises introduced in this study can facilitate in part such a feedforward system for the movement.
Previous reports suggest that functional reach is correlated to many indicators of standing balance and that it can be used as a predictive index of falling in the elderly14). Interestingly, functional reach was improved following our intervention. We should appreciate such effects on the items in dynamic standing balance, because falling in elderly persons occurs especially during their transfer18). Thus we speculate that our intervention may contribute to the prevention of falls in elderly persons.
Effect of intervention on postural response
In postural response (Table 3), less muscular activity (IEMG) was sufficient to recover the same level of postural sway (COP excursion) following the intervention, which indicates that postural response became more efficient following the intervention. However, postural response is composed of several postural strategies like ankle strategy or hip strategy as described by Nashner and Horak10, 11). Thus, we can not rule out the possibility that such a modification as the recruitment of postural strategy is also affecting muscular activity (IEMG). Thus, to elucidate physiological meaning of the decreased IEMG in postural response, further EMG analyses based on the timing of muscular activation among lower leg muscles are required additional to the analyses of the amplitude of EMG.
Shimada and Uchiyama19) report that targeted postural exercise has an effect on only a specific aspect of standing balance. Dynamic postural exercise improves only dynamic balance and static postural exercise improves only static balance. Similar results were reported by Wolf20). Gauchard21) also compared the effects of proprioceptive and bioenergic physical activities on postural control. Bioenergic physical activities only improved muscular strength, whereas proprioceptive activities only improved postural control. These reports suggest that the knock-on effects of specific balance exercises may not be as expected, and that the introduction of a comprehensive program is required for improvements in total aspects of postural control. Our intervention comprised walking and a variety of physical exercises, including exercises stimulating proprioceptive receptors. The program actually affected extensive aspects of standing balance.
The physical exercise introduced in our study consisted of daily walking and low-loaded bodily exercise comprising stretching, muscle strengthening and balance exercises. Furthermore, such program required no equipment or specific space for physical exercise. It is therefore useful as a community-based intervention. In fact, similar activities are widely accepted in many community-based interventions. This study suggests that the comprehensive exercise program widely accepted as community-based interventions in elderly persons are useful and efficient in improving standing balance extensively.
Acknowledgements
This study was supported in part by a grant for the health up model project in 21st century of the Japan Federation of National Health Insurance from Kake City, Hiroshima, Japan. We would like to thank Dr. Akihiro Kishi, (Kokuho Kake city Hospital) Katsuko Kikkawa (Welfare Division of Kake City), Naoko Matsumoto (Fitness Club Co. Ltd) and all staff of Kake city, Hiroshima.
References
- 1). Otaka Y, Liu M, et al. : The effectiveness of fall prevention program: a review—1. Fall prevention in narrow sense—. Jpn J Rehabil Med 40: 374-388, 2003. (in Japanese with English abstract). [Google Scholar]
- 2). Rawsky E: Review of the literature on falls among the elderly. Image J Nurs Sch 30: 47-52, 1998. [DOI] [PubMed] [Google Scholar]
- 3). Wong AM, Lin YC, et al. : Coordination exercise and postural stability in elderly people: Effect of Tai Chi Chuan. Arch Phys Med Rehabil 82: 608-612, 2001. [DOI] [PubMed] [Google Scholar]
- 4). Lord SR, Castell S, et al. : The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. J Am Geriatr Soc 51: 1685-1692, 2003. [DOI] [PubMed] [Google Scholar]
- 5). Shumway C, Horak F: Balance rehabilitation in the neurologic patient. Course syllabus Seattle, NERA, 1992. [Google Scholar]
- 6). Uchiyama Y: Equilibrium function and falls in the elderly. Journal of Physical Therapy 18: 858-864, 2001. (in Japanese with English abstract). [Google Scholar]
- 7). Cordo PJ, Nashner LM: Properties of postural adjustments associated with rapid arm movements. J Neurophysiol 47: 287-302, 1982. [DOI] [PubMed] [Google Scholar]
- 8). Crenna P, Frigo C: A motor programme for the initiation of forward-oriented movements in humans. J Physiol (Lond) 437: 635-653,1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Bouisset S, Richardson J, et al. : Do anticipatory postural adjustments occurring in different segments of the postural chain follow the same organisational rule for different task movement velocities, independently of the inertial load value? Exp Brain Res 132, 79-86, 2000. [DOI] [PubMed] [Google Scholar]
- 10). Nashner L, Woollacott M: The organization of rapid postural adjustments of standing humans: an experimental conceptural model. In: Talbott R, Humphrey D. (eds) Posture and Movement. 1st ed, Raven Press, 1979, pp243-257. [Google Scholar]
- 11). Horak FB, Nashner LM: Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol 55: 1369-1381, 1986. [DOI] [PubMed] [Google Scholar]
- 12). Barnett A, Smith B, et al. : Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing 32: 407-414, 2003. [DOI] [PubMed] [Google Scholar]
- 13). Berg K, Wood-Dauphinee S: Measuring balance in the elderly: preliminary development of an instrument. Physiother Canada 41: 304-308,1989. [Google Scholar]
- 14). Duncan PW, Weiner DK, et al. : Functional reach: a new clinical measure of balance. J Gerontol 45, M192-M197, 1990. [DOI] [PubMed] [Google Scholar]
- 15). Podsiadlo D, Richardson S: The timed Up and Go test: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39: 142-148, 1991. [DOI] [PubMed] [Google Scholar]
- 16). Tanaka N, Komatsu Y: The change of “degree of healthy lower legs” and “sway of center of gravity” after “Program for the prevention of falling”. Rigaku Ryohogaku 26 (S1) : 114, 1999. (in Japanese). [Google Scholar]
- 17). Kobayashi R, Hosoda M, et al. : Effect of grasp training for the aged on spontaneous postural sway. J Phys Ther Sci 11: 31-34, 1999. [Google Scholar]
- 18). Milisen K, Detroch E, et al. : Falls among community-dwelling elderly: a pilot study of prevalence, circumstances and consequences in Flanders. Tijdschr Gerontol Geriatr 35: 15-20, 2004. [PubMed] [Google Scholar]
- 19). Shimada H, Uchiyama Y: The effect of three-month program of static and dynamic postural balance exercise for the elderly. Rigaku Ryohogaku 28: 38-46, 2001. (in Japanese with English abstract). [Google Scholar]
- 20). Wolf S, Barnhart H, et al. : The effect of Thai Chi Quan and computerised balance training on postural stability in older subjects. Phys Ther 77: 371-381, 1997. [DOI] [PubMed] [Google Scholar]
- 21). Gauchard GC, Jeandel C, et al. : Beneficial effect of proprioceptive physical activities on balance control in elderly human subjects. Neurosci Lett 273: 81-84, 1999. [DOI] [PubMed] [Google Scholar]


