Abstract
Purpose: To investigate improvement in various impairments by exercise interventions in patients with knee osteoarthritis (OA). Methods: We collected data on randomized controlled trials (RCTs) comparing the effects of exercise intervention with those of either nonintervention or psychoeducational intervention in patients with knee OA. Data on pain, stiffness, muscle strength, range of motion, flexibility, maximal oxygen uptake, and position sense were synthesized. The Grading of Recommendations Assessment, Development, and Evaluation system was used to determine the quality of the evidence. Results: Thirty-three RCTs involving 3,192 participants were identified. Meta-analysis provided highquality evidence that exercise intervention improves maximal oxygen uptake, and moderate-quality evidence that exercise intervention also improves pain, stiffness, knee extensor and flexor muscle strength, and position sense. The evidence that exercise intervention improves knee extension and flexion range of motion was deemed as undetermined-quality. Conclusion: In patients with knee OA, improvement in pain, stiffness, muscle strength, maximal oxygen uptake, and position sense with the use of exercise intervention can be expected. Although the quality of evidence of the effect of exercise intervention on range of motion was inconclusive, exercise intervention should be recommended for patients with knee OA to improve various impairments.
Keywords: knee osteoarthritis, exercise, evidence
Knee osteoarthritis (OA) is the most common type of OA1), and its prevalence is rising in parallel with the increasing age of the population2). The condition is associated with pain and inflammation of the joint capsule3), impaired muscular stabilization4), reduced range of motion5), and disability. Treatment of knee OA is focused on reducing joint pain and stiffness, and improving muscular stabilization and joint mobility6).
According to Osteoarthritis Research Society International (OARSI) recommendations on the management of hip and knee OA6), patients with symptomatic knee OA may benefit from referral to a physical therapist for evaluation and instruction in appropriate exercises to reduce pain and improve functional capacity. In OARSI guideline7), patients with knee OA should be encouraged to undertake and continue regular aerobic, muscle strengthening, and range-ofmotion exercises. This recommendation is also supported by a systematic review and meta-analysis8–11). Therefore, there is consensus that exercise therapy, including strengthening and aerobics, is an effective intervention method for treating knee OA.
Cochrane review reported by Fransen and McConnell12), which examined the effect of exercise interventions in the patients with knee OA, showed that land-based therapeutic exercise has at least short term benefit in terms of reduced knee pain and improved physical function for people with knee OA. However, the effects on impairments except for pain, such as stiffness, muscle weakness, limited range of motion and sensory disturbance remain unclear. In fact, although several previous systematic reviews and meta-analyses8,9,11) have reported the effect of exercise interventions on pain and impairment, the effect sizes for synthesized data of stiffness, muscle strength, or joint mobility have not been reported in their reviews. Devos-Comby et al.10) synthesized these data together with swelling of the knee, joint effusion, peak oxygen uptake, body weight, and quadriceps muscle strength; however, the effect on each outcome has never been examined with meta-analysis. Therefore, regardless of the OARSI recommendations mentioned above6), high-quality evidence that exercise interventions improve impairments in patients with knee OA has yet to be confirmed.
The purpose of this systematic review and meta-analysis was to search for evidence of improvement in various impairments by exercise interventions in patients with knee OA.
Methods
Search Strategy
The study design was a systematic review and metaanalysis. The electronic databases PubMed, Cochrane Central Register of Controlled Trials, Physiotherapy Evidence Database (PEDro), and Cumulative Index to Nursing and Allied Health Literature (CINAHL) were used. All studies until February 2012 included in our search. The 2 concepts of “population” and “intervention” were combined with the “AND” operator. Population was defined as participants with OA of the knee. Intervention was defined as an exercise intervention for the treatment of OA. The design was a randomized controlled trial (RCT) to achieve the most valid information on the effectiveness of the interventions. For each concept, synonyms and Medical Subject Headings (MeSH) terms were combined with the “OR” operator (Table 1).
Table 1. Search strategy.
| (1) PubMed | #1 osteoarthritis, knee[MeSH Terms] |
| #2 exercise[MeSH Terms] | |
| #3 exercise therapy[MeSH Terms] | |
| #4 (#1 AND (#2 OR #3)) | |
| Limits: Randomized Controlled Trial | |
| (2) CENTRAL | #1 osteoarthritis, knee[MeSH Terms] |
| #2 exercise[MeSH Terms] | |
| #3 exercise therapy[MeSH Terms] | |
| #4 (#1 AND (#2 OR #3)) | |
| (3) PEDro | ·Advance search |
| Title or Abstract: osteoarthritis, knee, exercise | |
| Method: clinical trial | |
| (4) CINAHL | #1 osteoarthritis, knee[MeSH Terms] |
| #2 exercise[MeSH Terms] | |
| #3 exercise therapy[MeSH Terms] | |
| #4 (#1 AND (#2 OR #3)) | |
| Limits: Randomized Controlled Trial |
Two reviewers independently screened the articles by title and abstract, utilizing predetermined eligibility criteria. Any disagreements were resolved by discussion. Full-text copies of articles that were not definitely excluded based on title or abstract were retrieved, and the criteria were reapplied. Uncertain cases were discussed by the reviewers to achieve consensus. Database searching was supplemented by hand searching the reference lists of past systematic reviews.
Eligibility Criteria
The studies were included if (1) participants had knee OA, (2) the intervention was exercise, (3) the control was no intervention or psychoeducational intervention, (4) the researchers assessed pain or impairments, (5) an RCT design was used, and (6) the paper was written in English. In the outcome measures for pain, since we knew that the visual analog scale (VAS) or the Western Ontario and Mc- Master Universities Osteoarthritis Index (WOMAC) were frequently used to evaluate pain12), we included the studies using these outcome measures only.
The studies were excluded if (1) participants had hip OA or rheumatic disease, (2) patients had undergone total knee arthroplasty, (3) the intervention included intra-articular injections (e.g., sodium hyaluronate), (4) sufficient data for the synthesis of results were not reported, or (5) key outcome measure was already different significantly at baseline between groups. After screening for paper title and abstract, the studies using a minor outcome measurement that was not used in other extracted studies were excluded.
Data Collection Process
Predesigned spreadsheets were used to extract data on participants, interventions, outcome measurements, and results.
Risk of Bias in Individual Studies
Two researchers independently applied a validated scale (PEDro) to rate the methodological quality of all the trials13). The 11 items are based upon the Delphi list14). Each item is scored “yes” or “no,” with a maximum score of 10, as criterion 1 is not scored. The PEDro score has demonstrated moderate interrater reliability (intraclass correlation coefficient = 0.68 [95% CI, 0.57–0.76]) for clinical trials15). A trial with a score of 6 or more was considered to be high quality, which is consistent with previous reviews16).
Synthesis of Results
Standardized mean differences (SMDs) (effect sizes) and 95% confidence intervals (CIs) were calculated from postintervention means and SDs. When the standard error or 95% CI was provided, this was converted to SDs. Secondly, the P value was used for estimating the SD.
The data were coded so that a positive effect size indicated improvement and a negative effect size indicated worsening of impairment. Values of 0.2–0.5 indicated a small effect size, 0.5–0.8 a moderate effect size, and >0.8 a large effect size17).
Meta-analysis was performed using an inverse variance method and random effects analysis. The Review Manager Version 5.1 (The Cochrane Collaboration, Freiburg, Germany) was used for the meta-analysis. Combining data in a meta-analysis was planned, in which a minimum of 2 trials were clinically homogenous. A trial was considered clinically homogenous if a common population and outcome measurement were used. In the intervention, there were no restrictions with respect to type, frequency, duration, or intensity of exercise.
Quality of Evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach18) was applied to each meta-analysis performed to determine the quality of the evidence. This approach entailed downgrading the evidence from high quality to moderate quality to low quality and to very-low quality based on certain criteria. Down-grading the evidence one place (e.g., from high to moderate quality) would occur if (1) the PEDro score was ≤5 for the majority of trials (more than 50%) in the meta-analysis, (2) there was greater than low levels of statistical heterogeneity between the trials (l2 >25%)19), or (3) there were large CIs, indicating a small number of participants. If there were serious issues with the methodological quality, such as all trials in the meta-analysis had a PEDro score <6 without allocation concealment and blinded assessors, then a double downgrade would occur (e.g., from high to low quality). A footnote was used to explain the reasons for the grade applied to each meta-analysis. If the number of selected trials measuring a certain outcome was only 1 and that trial included multiple intervention groups, we synthesized the data but did not determine the quality of evidence for that outcome.
Results
Study Selection
The combined database search yielded 668 trials (inclusive of duplicates). A total of 33 trials fulfilled the inclusion criteria (Fig. 1).
Fig. 1.
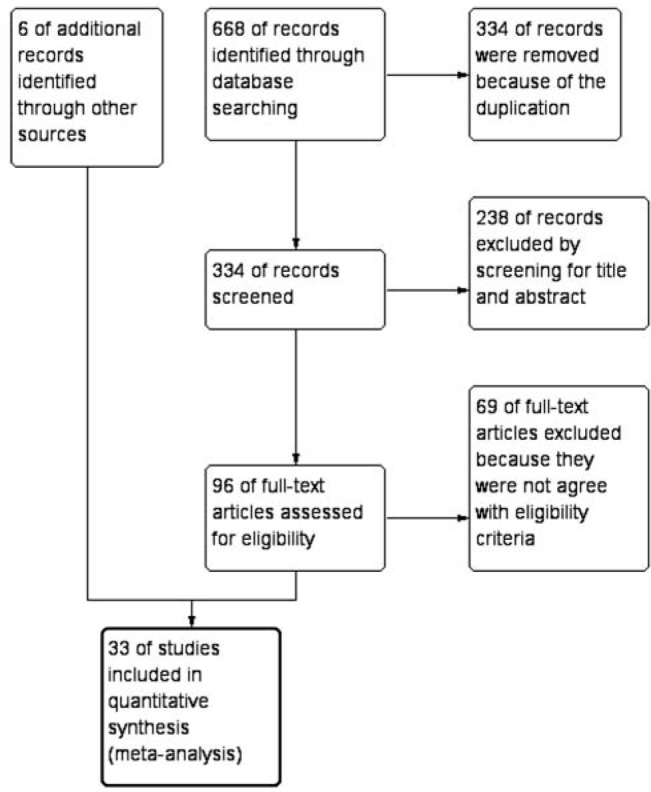
Study flow diagram
Study Characteristics
1. Participants
The included studies involved 3,192 participants (1,878 interventions and 1,314 comparisons). From available data in the interventions, the participants were aged from 55 to 74 years, and the female ratio was from 48.9% to 100%. A summary of included trials is shown in Table 2.
Table 2. Summary of included trials.
| Study | Participants (Exercise group) | Participants (Control group) | Exercise intervention | Frequency (per a week) | Duration (weeks) |
|---|---|---|---|---|---|
| Aglamis et al. 2009 | n = 16 Age (yrs) = 56.8 (4) Female (%) = 100 | n = 9 Age (yrs) = 54.4 (12) Female (%) = 100 | Aerobic, functional strengthening, and flexibility exercises | 3 | 12 |
| An et al. 2008 | n = 14 Age (yrs) = 65.4 (8.2) Female (%) = 100 | n = 14 Age (yrs) = 64.6 (6.7) Female (%) = 100 | Baduanjin | 5 | 8 |
| Baker et al. 2001 | n = 23 Age = 69 (6) Female (%) = 73.9 | n = 23 Age = 68 (6) Female (%) = 82.6 | Two functional exercises (squats and step-ups) | 3 | 16 |
| Bautch et al. 1997 | n = 17 Age (yrs) = 69 | n = 17 Age (yrs) = 69 | Range of motion exercises and an individualized low intensity walking | 3 | 12 |
| Bennell et al. 2010 | n = 45 Age (yrs) = 64.5 (9.1) Female (%) = 48.9 | n = 44 Age (yrs) = 64.6 (7.6) Female (%) = 54.5 | Six exercises to strengthen hip abductor and adductor muscles | 5 | 12 |
| Brismee et al. 2007 | n = 22 Age (yrs) = 70.8 (9.8) Female (%) = 86.4 | n = 19 Age (yrs) = 68.8 (8.9) Female (%) = 78.9 | Tai Chi exercise | 3 | 6 |
| Doi et al. 2008 | n = 71 Age (yrs) = 66.8 (12.8) Female (%) = 77.5 | n = 70 Age (yrs) = 68.9 (21.1) Female (%) = 74.6 | Quadriceps strengthening exercises | 7 | 8 |
| Ettinger et al. 1997 | Group 1 n = 144 Age (yrs) = 69 (6) Female (%) = 69 Group 2 n = 146 Age (yrs) = 68 (6) Female (%) = 73 | n = 149 Age (yrs) = 69 (6) Female (%) = 69 | Group 1: Facility-based walking Group 2: Resistive exercise (9 exercises) | 3 | 72 |
| Fransen et al. 2001 | Group 1 n = 43 Age (yrs) = 68.5 (8.7) Female (%) = 74 Group 2 n = 40 Age (yrs) = 65.3 (7.1) Female (%) = 78 | n = 43 Age (yrs) = 66.1 (10.3) Female (%) = 67 | Group 1: The choice, frequency, and duration of individual treatments at the discretion of the treating physical therapist Group 2: Quadriceps muscle strengthening exercise, stretching, aerobic exercise, and patella taping | 2 | 8 |
| Hale et al. 2012 | n = 23 Age (yrs) = 73.6 (1.5) Female (%) = 74 | n = 16 Age (yrs) = 75.7 (1.1) Female (%) = 75 | In water-based class, warm-up/ warm-down exercises (stretching, walking forward, backward, sideways, calf and toe raises), balance exercises | 2 | 12 |
| Huang et al. 2003 | Group 1: n = 33 Group 2: n = 33 Group 3: n = 33 | n = 33 | Group 1: Isokinetic musclestrengthening exercise Group 2: Isotonic musclestrengthening exercise Group 3: Isometric musclestrengthening exercise | 3 | 8 |
| Age (yrs) = 62 (4.5) Female (%) = 70 | |||||
| Hay et al. 2006 | n = 109 Age (yrs) = 67.9 (8.5) Female (%) = 65 | n = 108 Age (yrs) = 68.2 (8.0) Female (%) = 65 | Aerobic exercise, muscle strengthening exercises and stretching exercises | 3–6 sessions / 10 weeks | 10 |
| Jan et al. 2008 | Group 1 n = 34 Age (yrs) = 63.3 (6.6) Female (%) = 79.4 Group 2 n = 34 Age (yrs) = 61.8 (7.1) Female (%) = 79.4 | n = 34 Age (yrs) = 62.8 (6.3) Female (%) = 83.3 | Group 1: The high-resistance exercise (60% of 1 RM) Group 2: The low-resistance exercise (10% of 1 RM) | 3 | 8 |
| Jan et al. 2009 | Group 1 n = 36 Age (yrs) = 62.0 (6.7) Female (%) = 66.7 Group 2 n = 36 Age (yrs) = 63.2 ( 6.8) Female (%) = 71.4 | n = 36 Age (yrs) = 62.2 (6.7) Female (%) = 68.6 | Group 1: The weight-bearing exercise in a sitting position with 1 foot fixed on the center of the pedal of an EN-Dynamic resistance device Group 2: The nonweight-bearing exercise | 3 | 8 |
| Lee et al. 2009 | n = 29 Age (yrs) = 70.2 (4.8) Female (%) = 93 | n = 15 Age (yrs) = 66.9 (6.0) Female (%) = 93 | Tai Chi exercise | 2 | 8 |
| Lim et al. 2008 | n = 26 Age (yrs) = 67.2 (6.7) Female (%) = 50 | n = 26 Age (yrs) = 64.1 (9.3) Female (%) = 63 | Quadriceps strengthening exercises (5 exercises) | 5 | 12 |
| Lin et al. 2007 | Group 1 n = 29 Age (yrs) = 61.6 (8.1) Female (%) = 69 Group 2 n = 26 Age (yrs) = 61.0 (7.7) Female (%) = 77 | n = 26 Age (yrs) = 62.8 (6.3) Female (%) = 77 | Group 1: Computerized proprioception facilitation exercise Group 2: Closed kinetic chain exercise with resistance device | 3 | 8 |
| Lin et al. 2009 | Group 1 n = 36 Age (yrs) = 63.7 (8.2) Female (%) = 69.4 Group 2 n = 35 Age (yrs) = 61.6 (7.2) Female (%) = 66.7 | n = 36 Age (yrs) = 62.2 (6.7) Female (%) = 72.2 | Group 1: Computer game footstepping exercise Group 2: The strength training in non—weight-bearing position | 3 | 8 |
| Lund et al. 2008 | Group 1 n = 25 Age (yrs) = 68 (9.5) Female (%) = 88 Group 2 n = 27 Age (yrs) = 65 (12.6) Female (%) = 83 | n = 27 Age (yrs) = 70 (9.9) Female (%) = 66% | Group 1: Strengthening/endurance exercise, balance exercise and stretching exercise (land-based) Group 2: Strengthening/endurance exercise, balance exercise and stretching exercise (aquatic based) | 2 | 8 |
| Messier et al. 2004 | Group 1 n = 80 Age (yrs) = 69 (0.8)† Female (%) = 74 Group 2 n = 76 Age (yrs) = 69 (0.8)† Female (%) = 74 | n = 78 Age (yrs) = 69 (0.1)† Female (%) = 68 | Group 1: Aerobic training and resistance training Group 2: Diet, aerobic training and resistance training | 3 | 72 |
| Miller et al. 2006 | n = 44 Age (yrs) = 69.7 (0.9)† Female (%) = 63.6 | n = 43 Age (yrs) = 69.3 (0.9)† Female (%) = 60.5 | Aerobic exercise and strengthening exercise | 3 | 24 |
| O'Reilly et al. 1999 | n = 78 Age (yrs) = 61.9 (10.0) | n = 113 Age (yrs) = 62.2 (9.7) | Isometric quadriceps contraction, Isotonic quadriceps contraction, Isotonic hamstring contraction, and Dynamic stepping exercise | 7 | 24 |
| Peloquin et al. 1999 | n = 59 Age (yrs) = 65.6 (7.4) Female (%) = 71.2 | n = 65 Age (yrs) = 66.4 (8.3) Female (%) = 69.2 | Aerobic exercises, musclestrengthening exercises, stretching exercises | 3 | 12 |
| Quilty et al. 2003 | n = 43 Age (yrs) = 66.8 (9.5) | n = 44 Age (yrs) = 66.7 (11.2) | Patellar taping, 7 exercises, posture correction, and footwear advice | 1 | 10 |
| Salli et al. 2010 | Group 1 n = 25 Age (yrs) = 55.7 (8.2) Female (%) = 82.6 Group 2 n = 25 Age (yrs) = 57.1 (6.8) Female (%) = 83.3 | n = 25 Age (yrs) = 58.3 (6.7) Female (%) = 79.2 | Group 1: Combined concentriceccentric exercise Group 2: Isometric exercise (progressive) | 3 | 8 |
| Schilke et al. 1996 | n = 10 Age (yrs) = 64.5 (59-74)‡ | n = 10 Age (yrs) = 68.4 (53-85)‡ | Isotonic muscle-strengthening exercise | 3 | 8 |
| Female (%) = 85 | |||||
| Song et al. 2003 | n = 38 Age (yrs) = 64.8 (6.0) Female (%) = 100 | n = 34 Age (yrs) = 62.5 (5.6) Female (%) = 100 | Tai Chi exercise | 3 | 12 |
| Song et al. 2010 | n = 30 Age (yrs) = 63 (7.3) Female (%) = 100 | n = 35 Age (yrs) = 61 (8.0) Female (%) = 100 | Tai Chi exercise | 7 | 24 |
| Thorstensson et al. 2005 | n = 26 Age (yrs) = 54.8 (7.1) Female (%) = 50 | n = 23 Age (yrs) = 57.3 (4.7) Female (%) = 50 | Ergometer cycling, trampoline, stepboard, floor exercises, and pulley | 2 | 6 |
| Topp et al. 2002 | Group 1 n = 32 Age (yrs) = 65.6 (1.8)† Female (%) = 80 Group 2 n = 35 Age (yrs) = 63.5 (1.9)† Female (%) = 71 | n = 35 Age (yrs) = 60.9 (1.8)† Female (%) = 66 | Group 1: Resistance-training exercises across a functional range of motion Group 2: Resistance-training exercises at discrete joint angles | 3 | 16 |
| Topp et al. 2009 | n = 26 Age (yrs) = 64.1 (7.1) n = 28 | Age (yrs) = 63.5 (6.6) | Resistance training | 3 | 5 |
| Female (%) = 68 | |||||
| Wang et al. 2007 | n = 40 Age (yrs) = 69.9 (5.7) Female (%) = 62.5 | n = 33 Age (yrs) = 68.8 (5.7) Female (%) = 63.6 | Diet, aerobic training and strength training | 3 | 24 |
| Wang et al. 2011 | Group 1 n = 26 Age (yrs) = 67.7 (5.6) Female (%) = 84.6 Group 2 n = 26 Age (yrs) = 68.3 (6.4) Female (%) = 88.5 | n = 26 Age (yrs) = 67.9 (5.9) Female (%) = 84.6 | Group 1: Flexibility training, aerobic training, lower body training, upper body training (aquatic based) Group 2: Flexibility training, aerobic training, lower body training, upper body training (land-based) | 3 | 12 |
†: Standard error,
‡: Range
2. Interventions
Trials included in our study used muscle strengthening exercise with or without weight bearing, balance exercise, muscle stretching exercise, walking, Tai chi exercise, Baduanjin, functional exercise, computerized proprioception facilitation exercise, or range of motion exercise. Some trials added diet20,21) or patellar taping21,22) with exercise, or performed water-based exercise23–25).
3. Outcome
Trials included in our study measured pain, stiffness, muscle strength, range of motion, flexibility, maximal oxygen uptake, or position sense as the outcome of body function and structure. Stiffness was evaluated with the WOMAC. Muscle strength was measured for knee extensors or flexors, and the majority of trials used peak torque at concentric isokinetic contraction as muscle strength. Range of motion was measured at maximum knee extension or flexion. Flexibility was measured by asking the patient to bend at the waist and stretch both hands toward the feet without bending the knees, and the distance between the hands and feet was measured. Maximal oxygen uptake was measured as the volume of oxygen taken up in 1 minute per kilogram of body weight at peak exercise. Position sense was evaluated by the reposition error test.
Risk of Bias within Studies
There were 23 higher-quality trials (PEDro score > 5/10), and the average score across all trials was 6.2/10. The most adhered to items on the PEDro scale were random allocation, measurements of variability for at least one key outcome, and between group comparisons, which were evident in almost all of the trials. None of the trials blinded participants or therapists, which was expected given these items are the most difficult to adhere to in trials of interventions, such as exercise. Seventeen trials used allocation concealment and 18 had blinded outcome assessors. Sixteen trials reported intention-to-treat analysis, and 27 trials had measurements of at least one key outcome from >85% of participants (Table 3).
Table 3. Methodological quality of the trials (PEDro).
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total (/10) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aglamis et al. 2009 | Yes | No | No | No | No | No | No | No | Yes | Yes | 3 |
| An et al. 2008 | Yes | No | Yes | No | No | No | No | No | Yes | Yes | 4 |
| Baker et al. 2001 | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 7 |
| Bautch et al. 1997 | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes | 5 |
| Bennell et al. 2010 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Brismee et al. 2007 | Yes | No | Yes | No | No | Yes | No | No | Yes | Yes | 5 |
| Doi et al. 2008 | Yes | Yes | Yes | No | No | No | Yes | No | Yes | Yes | 6 |
| Ettinger et al. 1997 | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 6 |
| Fransen et al. 2001 | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | 7 |
| Hale et al. 2012 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Huang et al. 2003 | Yes | Yes | Yes | No | No | No | Yes | No | Yes | Yes | 6 |
| Hay et al. 2006 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Jan et al. 2008 | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 7 |
| Jan et al. 2009 | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 7 |
| Lee et al. 2009 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Lim et al. 2008 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Lin et al. 2007 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Lin et al. 2009 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Lund et al. 2008 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Messier et al. 2004 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Miller et al. 2006 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| O'Reilly et al. 1999 | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | 7 |
| Peloquin et al. 1999 | Yes | No | Yes | No | No | Yes | Yes | No | Yes | Yes | 6 |
| Quilty et al. 2003 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Salli et al. 2010 | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | 6 |
| Schilke et al. 1996 | Yes | No | No | No | No | No | Yes | No | Yes | Yes | 4 |
| Song et al. 2003 | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | 6 |
| Song et al. 2010 | Yes | No | Yes | No | No | Yes | No | Yes | Yes | Yes | 6 |
| Thorstensson et al. 2005 | Yes | Yes | Yes | No | No | No | Yes | No | Yes | Yes | 6 |
| Topp et al. 2002 | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Topp et al. 2009 | Yes | No | Yes | No | No | No | Yes | No | No | Yes | 4 |
| Wang et al. 2007 | Yes | No | Yes | No | No | No | No | No | Yes | Yes | 4 |
| Wang et al. 2011 | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | 7 |
PEDro Criteria: (1) Random allocation. (2) Allocation concealed. (3) Groups similar at baseline. (4) Participant blinding. (5) Therapist blinding. (6) Assessor blinding. (7) Measures of at least one key outcome were obtained from >85% of subjects. (8) Data were analyzed by intention to treat. (9) Results reported for at least one key outcome. (10) Point measures and measures of variability provided.
Synthesis of Results
Synthesis of the results of exercise intervention are shown in Figs. 2–11, and Tables 4.
Fig. 2.
SMD (95% CI) of effect of exercise intervention on pain (VAS)
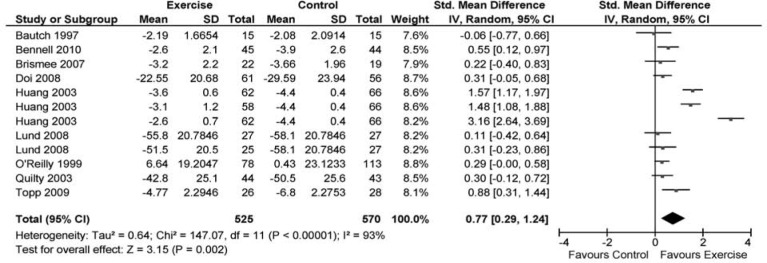
Fig. 11.
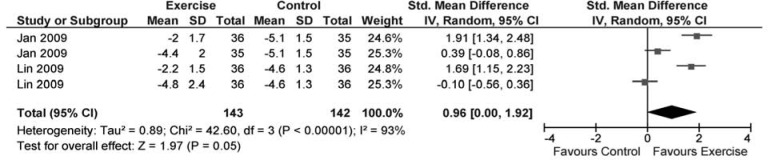
SMD (95% CI) of effect of exercise intervention on position sense
Table 4. Meta-analyses for the effect of exercise intervention.
| No. of trials (No. of groups) | Ratio of trials (PEDro <6) | No. of participants | SMD [95% CI] | l2 | Quality of the evidence (GRADE) | |
|---|---|---|---|---|---|---|
| Pain (VAS) | 9(12) | 33% | 1,095 | 0.77 [0.29, 1.24] | 93% | Moderate§ |
| Pain (WOMAC) | 16(20) | 25% | 1,667 | 0.43 [0.29, 0.57] | 48% | Moderate§ |
| Stiffness (WOMAC) | 8(9) | 63% | 424 | 0.24 [0.05, 0.44] | 0% | Moderate// |
| Muscle strength (knee extension) | 13(18) | 38% | 1,692 | 0.37 [0.24, 0.50] | 38% | Moderate§ |
| Muscle strength (knee flexion) | 9(14) | 22% | 1,503 | 0.59 [0.42, 0.77] | 58% | Moderate§ |
| ROM (knee extension) | 1(2) | 0% | 104 | 0.89 [0.49, 1.30] | 0% | — |
| ROM (knee flexion) | 1(2) | 0% | 104 | 0.51 [0.12, 0.90] | 0% | — |
| Flexibility | 2(2) | 0% | 167 | 0.34 [-0.32, 1.01] | 73% | Low¶ |
| Maximal oxygen uptake | 3(4) | 0% | 680 | 0.22 [0.07, 0.37] | 0% | High |
| Position sense | 2(4) | 0% | 285 | 0.96 [0.00, 1.92] | 93% | Moderate§ |
GRADE = GRADE working group grades of evidence.
VAS: Visual Analogue Scale, WOMAC: Western Ontario and McMaster Universities Arthritis Index, ROM: Range of Motion.
§ Reason for downgrade: Statistical heterogeneity (l2 > 25%)
// Reason for downgrade: Less than 6 PEDro score for the majority of trials (more than 50%)
¶ Reason for downgrade: Large confidence intervals, statistical heterogeneity (l2 > 25%)
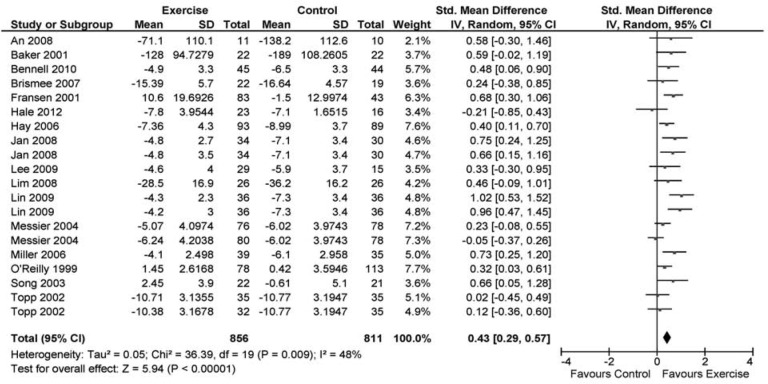
Fig. 3.
SMD (95% CI) of effect of exercise intervention on pain (WOMAC)
Fig. 4.
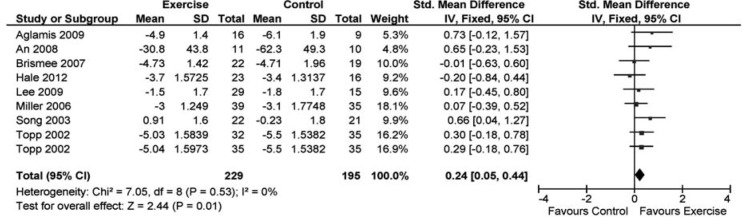
SMD (95% CI) of effect of exercise intervention on stiffness (WOMAC)
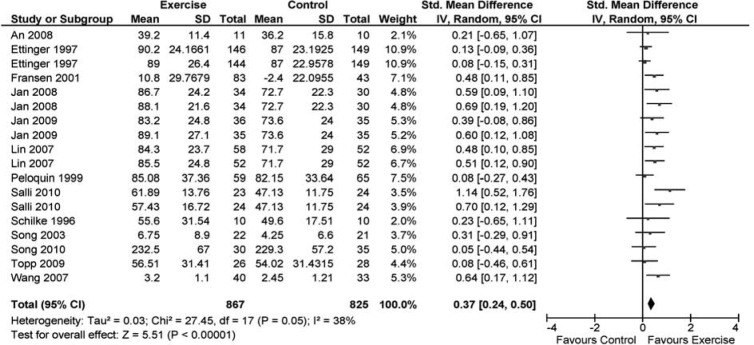
Fig. 5.
SMD (95% CI) of effect of exercise intervention on knee extensors muscle strength
Fig. 6.
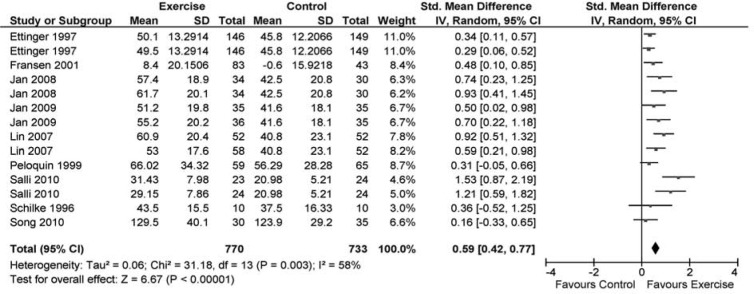
SMD (95% CI) of effect of exercise intervention on knee flexors muscle strength
Fig. 7.
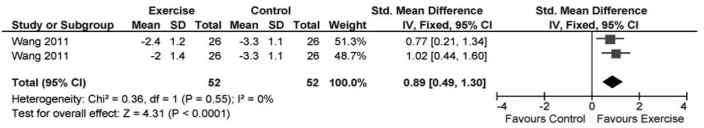
SMD (95% CI) of effect of exercise intervention on knee extension range of motion
Fig. 8.
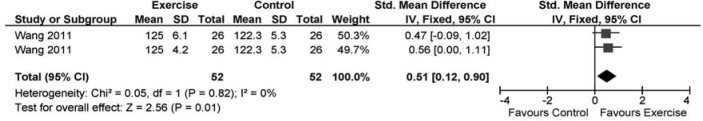
SMD (95% CI) of effect of exercise intervention on knee flexion range of motion
Fig. 9.
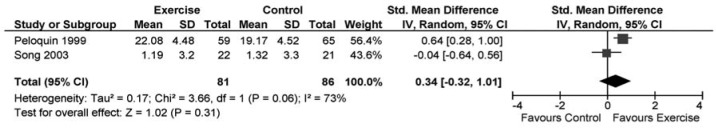
SMD (95% CI) of effect of exercise intervention on flexibility
Fig. 10.
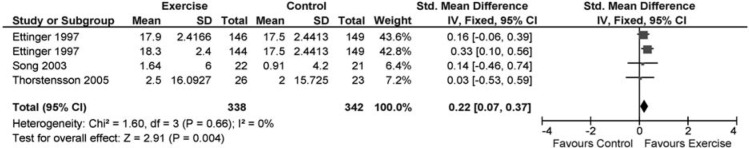
SMD (95% CI) of effect of exercise intervention on maximal oxygen uptake
1. Pain
Meta-analysis of 9 trials23,26–33) with 1,095 participants provided moderate-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at reducing pain, as measured by the VAS. Meta-analysis of 16 trials20,22,24,27,28,31,34–43) with 1,667 participants provided moderate-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at reducing pain, as measured by the WOMAC.
2. Stiffness
Meta-analysis of 8 trials24,28,34,38,41–44) with 424 participants provided moderate-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at reducing stiffness, as measured by the WOMAC.
3. Muscle strength
Meta-analysis of 13 trials21,22,33,34,37,42,45–51) with 1,692 participants provided moderate-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at improving knee extensor muscle strength. Meta-analysis of 9 trials22,37,45–51) with 1,503 participants provided moderate-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at improving knee flexor muscle strength.
4. Range of motion
Meta-analysis of 1 trial25) with 104 participants (2 intervention groups) provided undetermined-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at improving knee extension and flexion range of motion.
5. Flexibility
Meta-analysis of 2 trials42,47) with 167 participants provided low-quality evidence showing that compared with no exercise intervention, exercise intervention was not effective at improving flexibility.
6. Maximal oxygen uptake
Meta-analysis of 3 trials42,51,52) with 680 participants provided high-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at improving maximal oxygen uptake.
7. Position sense
Meta-analysis of 2 trials40,45) with 285 participants provided moderate-quality evidence showing that compared with no exercise intervention, exercise intervention was effective at improving position sense.
Discussion
Summary of Evidence
To the best of our knowledge, this is the first report to investigate the effectiveness of exercise intervention to individual impairments on OA patients by meta-analysis. The results of this systematic review provide moderate- to high-quality evidence that exercise intervention can have a small to large effect on knee OA by reducing pain and stiffness, and improving muscle strength, maximal oxygen uptake, and position sense. However, sufficient evidence of the effects on range of motion and flexibility were not shown in exercise intervention.
1. Pain
In several systematic reviews, the effect of exercise intervention has been supported with a high level of evidence12,53). In our reviews, that is confirmed with a moderate level of evidence. Additionally, in high-quality RCTs only (PEDro score > 5), of 9 exercise groups measured by VAS and 13 exercise groups measured by WOMAC, 9 exercise groups (100%) and 11 exercise groups (84.6%) showed more pain relief than control groups respectively. Therefore, we believe firmly in the effect of exercise intervention on pain. Although a variance in effect size was observed in our study, this may be explained by the lack of similarity in exercise interventions among trials, which also was shown in past meta-analysis studies8,54,55), including the Cochrane reports12). At present, the factors that influence the variance in effect size remain unclear.
2. Stiffness
In the systematic review by Lange et al.11), 5 studies measured stiffness; of which, 2 demonstrated significant improvement in the strength training group, compared with the control group. However, they did not perform a meta-analysis, and could not confirm the effect of exercise intervention on stiffness. We synthesized the data from 8 studies that examined the effect of exercise intervention on stiffness, as measured by the WOMAC, and confirmed a small effect size, which tends to be less than the effect on pain. To our knowledge, this evidence has not been reported previously. Our findings might indicate a difficulty in improving stiffness with exercise intervention in contrast to pain relief.
3. Muscle strength
With regard to muscle strength (not as is the case of pain), there are few systematic reviews that confirmed strong evidence of the effectiveness of exercise intervention. According to Lange et al.11), there were 14 RCTs that examined the effect of strength training on muscle strength; of which, 9 (64%) showed significant improvement in the strength training group, compared with the control group. They concluded that resistance training improved muscle strength. Our results also demonstrated that exercise intervention, including strength training, was effective at improving the muscle strength of either knee extensors or knee flexors. Additionally, this positive effect was supported by a moderate-quality evidence. This finding is additional evidence to recommend exercise in patients with weak muscle strength caused by knee OA.
4. Range of motion
Except for the report by Lange et al.11), there were no systematic reviews or meta-analysis studies that examined the effect of exercise intervention on range of motion. According to Lange et al.11), the number of studies measuring the effect on range of motion was 6; of these studies, only 1 showed significant improvement in the strength training group, compared with the control group. According to our synthesized data, the effect on extension or flexion range of motion was positive; however, the data were extracted from only 2 exercise groups in 1 study25). Therefore, we could not judge the effect of exercise intervention on range of motion with a strong evidence level.
5. Flexibility
The effect of exercise intervention on flexibility has been investigated in past systematic review56). In the present review, the number of studies examining the effect on flexibility was only 2. Although we could synthesize the data from the 2 studies, the results did not show a positive effect in exercise groups, and this evidence level was low. Thus, we could not support the effect on flexibility positively.
6. Maximal oxygen uptake
Brosseau et al.57) reviewed and judged the efficacy of aerobic exercise for respiratory capacity for the reason of the positive results by only one RCT of Minor58). We believe attention should be given to this judgment. The reason is that the RCT by Minor58) included data from patients with rheumatoid arthritis and OA, and lacked concealed allocation, blind assessors, adequate follow-up, and intention-to-treat analysis, which corresponded to a PEDro score of 4. In contrast, 3 studies selected in our meta-analysis included patients with OA only and had a PEDro score >6. The synthesized data for 3 studies that examined the effect of exercise intervention on maximal oxygen uptake were positive, and the quality of this evidence was high. However, 2 RCTs42,52) showed no positive effect of exercise intervention, synthesized data might be reflected strongly from 1 RCT51) because of its large sample size compared with those in the other 2 RCTs42,52). Additionally, exercise intervention duration in this RCT51) was longer (72 weeks) than in the other 2 RCTs42,52) (6 weeks and 12 weeks, respectively). This information suggests that improvement in maximal oxygen uptake might require long-term exercise intervention. Accordingly, at present, the effect of exercise intervention on maximal oxygen uptake should be recognized with caution.
7. Position sense
The effect of exercise intervention on position sense has not been confirmed with strong evidence; therefore, there is no consensus on its efficacy. A positive effect was revealed in 2 previous high-quality RCTs, and the synthesized data in our meta-analysis was of a significantly large effect size. However, a statistical heterogeneity was detected between the 2 studies40,45) (4 exercise groups). In these studies, the effect size was significantly large in the exercise groups that performed weight-bearing exercise, whereas no significant effect was detected in the exercise groups that performed non-weight-bearing exercise. Therefore, the effect on position sense might depend on weight-bearing condition during exercise.
Strong Points and Limitations of the Study
Our study has 2 strong points. First, we synthesized the objective outcome data from multiple studies. Previously, high-quality evidence of the effect of exercise intervention was obtained from self-reported outcomes (e.g., VAS, WOMAC) in some meta-analysis studies (e.g., Roddy et al.8), Fransen and McConnell12)). We obtained moderate- to high-quality evidence from objective outcomes (e.g., muscle strength, maximal oxygen uptake, and position sense), which are difficult to be influenced by psychological bias. Second, we revealed the evidence level of various types of outcomes. Previously, the evidence level was judged for each type of exercise (e.g., muscle strengthening exercise and aerobic exercise). In our studies, we judged the evidence level of each outcome according to the GRADE approach, which is recognized as a general system for practice guidelines.
We can identify 2 research limitations. First, subject characteristics were not identical among the studies included in our study. The inclusion criteria on OA grade and severity of impairment were not established in detail. For example, exercise intervention might not be effective in patients with severe OA grade, pain, or impairments. Clarification of the effective exercise intervention corresponding to subject characteristics could be a research objective in future studies. Second, statistical heterogeneity between studies (groups) was observed in pain, muscle strength, flexibility, and position sense. The effect of exercise intervention might be influenced by factors such as exercise type or intention; previous studies could not identify the influencing factors. If these factors could be clarified, clinicians could achieve a more effective exercise intervention program.
Conclusion
There is high-quality evidence that exercise intervention is effective at improving maximal oxygen uptake. There is moderate-quality evidence that exercise intervention is effective at improving pain, stiffness, knee extensor and flexor muscle strength, and position sense. There is low-quality evidence that exercise intervention is not effective at improving flexibility. There is no strong evidence that exercise intervention is effective at improving knee extension and flexion range of motion.
References
- 1). Andrianakos A, Trontzas P, Christoyannis F, Dantis P, Voudouris C, Georgountzos A, Kaziolas G, Vafiadou E, Pantelidou K, Karamitsos D, Kontelis L, Krachtis P, Nikolia Z, Kaskani E, Tavaniotou E, Antoniades C, Karanikolas G, Kontoyanni A: Prevalence of rheumatic diseases in Greece: a crosssectional population based epidemiological study. The ESORDIG Study. J Rheumatol. 2003, 30: 1589-1601. [PubMed] [Google Scholar]
- 2). Felson DT, Lawrence RC, Hochberg MC, McAlindon T, Dieppe PA, Minor MA, Blair SN, Berman BM, Fries JF, Weinberger M, Lorig KR, Jacobs JJ, Goldberg V: Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med. 2000, 133: 726-737. [DOI] [PubMed] [Google Scholar]
- 3). Naredo E, Cabero F, Palop MJ, Collado P, Cruz A, Crespo M: Ultrasonographic findings in knee osteoarthritis: a comparative study with clinical and radiographic assessment. Osteoarthritis Cartilage. 2005, 13: 568-574. [DOI] [PubMed] [Google Scholar]
- 4). Brandt KD, Heilman DK, Slemenda C, Katz BP, Mazzuca S, Braunstein EM, Byrd D: A comparison of lower extremity muscle strength, obesity, and depression scores in elderly subjects with knee pain with and without radiographic evidence of knee osteoarthritis. J Rheumatol. 2000, 27: 1937-1946. [PubMed] [Google Scholar]
- 5). Steultjens MP, Dekker J, van Baar ME, Oostendorp RA, Bijlsma JW: Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology (Oxford). 2000, 39: 955-961. [DOI] [PubMed] [Google Scholar]
- 6). Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P: OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidencebased, expert consensus guidelines. Osteoarthritis Cartilage. 2008, 16: 137-162. [DOI] [PubMed] [Google Scholar]
- 7). Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P: OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage. 2007, 15: 981-1000. [DOI] [PubMed] [Google Scholar]
- 8). Roddy E, Zhang W, Doherty M: Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis. 2005, 64: 544-548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Pisters MF, Veenhof C, van Meeteren NL, Ostelo RW, de Bakker DH, Schellevis FG, Dekker J: Long-term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review. Arthritis Rheum. 2007, 57: 1245-1253. [DOI] [PubMed] [Google Scholar]
- 10). Devos-Comby L, Cronan T, Roesch SC: Do exercise and self-management interventions benefit patients with osteoarthritis of the knee? A metaanalytic review. J Rheumatol. 2006, 33: 744-756. [PubMed] [Google Scholar]
- 11). Lange AK, Vanwanseele B, Fiatarone Singh MA: Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis Rheum. 2008, 59: 1488-1494. [DOI] [PubMed] [Google Scholar]
- 12). Fransen M, McConnell S: Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2008, CD004376. [DOI] [PubMed] [Google Scholar]
- 13). de Morton NA: The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009, 55: 129-133. [DOI] [PubMed] [Google Scholar]
- 14). Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, Knipschild PG: The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998, 51: 1235-1241. [DOI] [PubMed] [Google Scholar]
- 15). Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M: Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003, 83: 713-721. [PubMed] [Google Scholar]
- 16). Wallis JA, Taylor NF: Pre-operative interventions (nonsurgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery—a systematic review and meta-analysis. Osteoarthritis Cartilage. 19: 1381-1395. [DOI] [PubMed] [Google Scholar]
- 17). Cohen J: Quantitative methods in psychology. Psychological Bulletin. 1992, 112: 155-159.19565683 [Google Scholar]
- 18). Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O'Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer TT, Varonen H, Vist GE, Williams JW, Jr., Zaza S: Grading quality of evidence and strength of recommendations. BMJ. 2004, 328: 1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19). Higgins JP, Thompson SG, Deeks JJ, Altman DG: Measuring inconsistency in meta-analyses. BMJ. 2003, 327: 557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, Ettinger WH, Jr., Pahor M, Williamson JD: Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004, 50: 1501-1510. [DOI] [PubMed] [Google Scholar]
- 21). Wang X, Miller GD, Messier SP, Nicklas BJ: Knee strength maintained despite loss of lean body mass during weight loss in older obese adults with knee osteoarthritis. J Gerontol A Biol Sci Med Sci. 2007, 62: 866-871. [DOI] [PubMed] [Google Scholar]
- 22). Fransen M, Crosbie J, Edmonds J: Physical therapy is effective for patients with osteoarthritis of the knee: a ran domized controlled clinical trial. J Rheumatol. 2001, 28:156-164. [PubMed] [Google Scholar]
- 23). Lund H, Weile U, Christensen R, Rostock B, Downey A, Bartels EM, Danneskiold-Samsoe B, Bliddal H: A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. J Rehabil Med. 2008, 40: 137-144. [DOI] [PubMed] [Google Scholar]
- 24). Hale LA, Waters D, Herbison P: A randomized controlled trial to investigate the effects of water-based exercise to improve falls risk and physical function in older adults with lower-extremity osteoarthritis. Arch Phys Med Rehabil. 2012, 93: 27-34. [DOI] [PubMed] [Google Scholar]
- 25). Wang TJ, Lee SC, Liang SY, Tung HH, Wu SF, Lin YP: Comparing the efficacy of aquatic exercises and land-based exercises for patients with knee osteoarthritis. J Clin Nurs. 2011, 20: 2609-2622. [DOI] [PubMed] [Google Scholar]
- 26). Bautch JC, Malone DG, Vailas AC: Effects of exercise on knee joints with osteoarthritis: a pilot study of biologic markers. Arthritis Care Res. 1997, 10: 48-55. [DOI] [PubMed] [Google Scholar]
- 27). Bennell KL, Hunt MA, Wrigley TV, Hunter DJ, McManus FJ, Hodges PW, Li L, Hinman RS: Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: a randomised controlled trial. Osteoarthritis Cartilage. 2010, 18: 621-628. [DOI] [PubMed] [Google Scholar]
- 28). Brismee JM, Paige RL, Chyu MC, Boatright JD, Hagar JM, McCaleb JA, Quintela MM, Feng D, Xu KT, Shen CL: Group and home-based tai chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007, 21: 99-111. [DOI] [PubMed] [Google Scholar]
- 29). Doi T, Akai M, Fujino K, Iwaya T, Kurosawa H, Hayashi K, Marui E: Effect of home exercise of quadriceps on knee osteoarthritis compared with nonsteroidal antiinflammatory drugs: a randomized controlled trial. Am J Phys Med Rehabil. 2008, 87: 258-269. [DOI] [PubMed] [Google Scholar]
- 30). Huang MH, Lin YS, Yang RC, Lee CL: A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Semin Arthritis Rheum. 2003, 32: 398-406. [DOI] [PubMed] [Google Scholar]
- 31). O'Reilly SC, Muir KR, Doherty M: Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis. 1999, 58: 15-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32). Quilty B, Tucker M, Campbell R, Dieppe P: Physiotherapy, including quadriceps exercises and patellar taping, for knee osteoarthritis with predominant patello-femoral joint involvement: randomized controlled trial. J Rheumatol. 2003, 30: 1311-1317. [PubMed] [Google Scholar]
- 33). Topp R, Swank AM, Quesada PM, Nyland J, Malkani A: The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM R. 2009, 1: 729-735. [DOI] [PubMed] [Google Scholar]
- 34). An B, Dai K, Zhu Z, Wang Y, Hao Y, Tang T, Yan H: Baduanjin alleviates the symptoms of knee osteoarthritis. J Altern Complement Med. 2008, 14: 167-174. [DOI] [PubMed] [Google Scholar]
- 35). Baker KR, Nelson ME, Felson DT, Layne JE, Sarno R, Roubenoff R: The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomized controlled trial. J Rheumatol. 2001, 28: 1655-1665. [PubMed] [Google Scholar]
- 36). Hay EM, Foster NE, Thomas E, Peat G, Phelan M, Yates HE, Blenkinsopp A, Sim J: Effectiveness of community physiotherapy and enhanced pharmacy review for knee pain in people aged over 55 presenting to primary care: pragmatic randomised trial. BMJ. 2006, 333: 995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37). Jan MH, Lin JJ, Liau JJ, Lin YF, Lin DH: Investigation of clinical effects of high- and low-resistance training for patients with knee osteoarthritis: a randomized controlled trial. Phys Ther. 2008, 88: 427-436. [DOI] [PubMed] [Google Scholar]
- 38). Lee HJ, Park HJ, Chae Y, Kim SY, Kim SN, Kim ST, Kim JH, Yin CS, Lee H: Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clin Rehabil. 2009, 23: 504-511. [DOI] [PubMed] [Google Scholar]
- 39). Lim BW, Hinman RS, Wrigley TV, Sharma L, Bennell KL: Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum. 2008, 59: 943-951. [DOI] [PubMed] [Google Scholar]
- 40). Lin DH, Lin CH, Lin YF, Jan MH: Efficacy of 2 nonweight- bearing interventions, proprioception training versus strength training, for patients with knee osteoarthritis: a randomized clinical trial. J Orthop Sports Phys Ther. 2009, 39: 450-457. [DOI] [PubMed] [Google Scholar]
- 41). Miller GD, Nicklas BJ, Davis C, Loeser RF, Lenchik L, Messier SP: Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity (Silver Spring). 2006, 14: 1219-1230. [DOI] [PubMed] [Google Scholar]
- 42). Song R, Lee EO, Lam P, Bae SC: Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. J Rheumatol. 2003, 30: 2039-2044. [PubMed] [Google Scholar]
- 43). Topp R, Woolley S, Hornyak J, 3rd, Khuder S, Kahaleh B: The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Arch Phys Med Rehabil. 2002, 83: 1187-1195. [DOI] [PubMed] [Google Scholar]
- 44). Aglamis B, Toraman NF, Yaman H: Change of quality of life due to exercise training in knee osteoarthritis: SF-36 and WOMAC. J Back Musculoskelet Rehabil. 2009, 22: 43-45, 47,-48, 46. [DOI] [PubMed] [Google Scholar]
- 45). Jan MH, Lin CH, Lin YF, Lin JJ, Lin DH: Effects of weight-bearing versus nonweight-bearing exercise on function, walking speed, and position sense in participants with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil. 2009, 90: 897-904. [DOI] [PubMed] [Google Scholar]
- 46). Lin DH, Lin YF, Chai HM, Han YC, Jan MH: Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin Rheumatol. 2007, 26: 520-528. [DOI] [PubMed] [Google Scholar]
- 47). Peloquin L, Bravo G, Gauthier P, Lacombe G, Billiard JS: Effects of a Cross-Training Exercise Program in Persons with Osteoarthritis of the Knee A Randomized Controlled Trial. J Clin Rheumatol. 1999, 5: 126-136. [DOI] [PubMed] [Google Scholar]
- 48). Salli A, Sahin N, Baskent A, Ugurlu H: The effect of two exercise programs on various functional outcome measures in patients with osteoarthritis of the knee: A randomized controlled clinical trial. Isokinetics and Exercise Science. 2010, 18: 201-209. [Google Scholar]
- 49). Schilke JM, Johnson GO, Housh TJ, O'Dell JR: Effects of muscle-strength training on the functional status of patients with osteoarthritis of the knee joint. Nurs Res. 1996, 45: 68-72. [DOI] [PubMed] [Google Scholar]
- 50). Song R, Roberts BL, Lee EO, Lam P, Bae SC: A randomized study of the effects of t'ai chi on muscle strength, bone mineral density, and fear of falling in women with osteoarthritis. J Altern Complement Med. 2010, 16: 227-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51). Ettinger WH, Jr., Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, Shumaker S, Berry MJ, O'Toole M, Monu J, Craven T: A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA. 1997, 277: 25-31. [PubMed] [Google Scholar]
- 52). Thorstensson CA, Roos EM, Petersson IF, Ekdahl C: Sixweek high-intensity exercise program for middle-aged patients with knee osteoarthritis: a randomized controlled trial [ISRCTN20244858]. BMC Musculoskelet Disord. 2005, 6: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53). Jamtvedt G, Dahm KT, Christie A, Moe RH, Haavardsholm E, Holm I, Hagen KB: Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews. Phys Ther. 2008, 88: 123-136. [DOI] [PubMed] [Google Scholar]
- 54). Fransen M, McConnell S, Bell M: Therapeutic exercise for people with osteoarthritis of the hip or knee. A systematic review. J Rheumatol. 2002, 29: 1737-1745. [PubMed] [Google Scholar]
- 55). Fransen M, McConnell S: Land-based exercise for osteoarthritis of the knee: a metaanalysis of randomized controlled trials. J Rheumatol. 2009, 36: 1109-1117. [DOI] [PubMed] [Google Scholar]
- 56). Lee MS, Pittler MH, Ernst E: Tai chi for osteoarthritis: a systematic review. Clin Rheumatol. 2008, 27: 211-218. [DOI] [PubMed] [Google Scholar]
- 57). Brosseau L, MacLeay L, Robinson V, Wells G, Tugwell P: Intensity of exercise for the treatment of osteoarthritis. Cochrane database of systematic reviews. 2003, 2: CD004259. [DOI] [PubMed] [Google Scholar]
- 58). Minor MA: Exercise in the management of osteoarthritis of the knee and hip. Arthritis Care Res. 1994, 7: 198-204. [DOI] [PubMed] [Google Scholar]