Abstract
Introduction
Resident operative autonomy and case volume is associated with posttraining confidence and practice plans. Accreditation Council for Graduate Medical Education requirements for graduating general surgery residents are four liver and three pancreas cases. We sought to evaluate trends in resident experience and autonomy for complex hepatopancreatobiliary (HPB) surgery over time.
Methods
We queried the Accreditation Council for Graduate Medical Education General Surgery Case Log (2003–2012) for all cases performed by graduating chief residents (GCR) relating to liver, pancreas, and the biliary tract (HPB); simple cholecystectomy was excluded. Mean (±SD), median [10th–90th percentiles] and maximum case volumes were compared from 2003 to 2012 using R2 for all trends.
Results
A total of 252,977 complex HPB cases (36% liver, 43% pancreas, 21% biliary) were performed by 10,288 GCR during the 10-year period examined (Mean = 24.6 per GCR). Of these, 57% were performed during the chief year, whereas 43% were performed as postgraduate year 1–4. Only 52% of liver cases were anatomic resections, whereas 71% of pancreas cases were major resections. Total number of cases increased from 22,516 (mean = 23.0) in 2003 to 27,191 (mean = 24.9) in 2012. During this same time period, the percentage of HPB cases that were performed during the chief year decreased by 7% (liver: 13%, pancreas 8%, biliary 4%). There was an increasing trend in the mean number of operations (mean ± SD) logged by GCR on the pancreas (9.1 ± 5.9 to 11.3 ± 4.3; R2 = .85) and liver (8.0 ± 5.9 to 9.4 ± 3.4; R2 = .91), whereas those for the biliary tract decreased (5.9 ± 2.5 to 3.8 ± 2.1; R2 = .96). Although the median number of cases [10th:90th percentile] increased slightly for both pancreas (7.0 [4.0:15] to 8.0 [4:20]) and liver (7.0 [4:13] to 8.0 [5:14]), the maximum number of cases preformed by any given GCR remained stable for pancreas (51 to 53; R2 = .18), but increased for liver (38 to 45; R2 = .32). The median number of HPB cases that GCR performed as teaching assistants (TAs) remained at zero during this time period. The 90th percentile of cases performed as TA was less than two for both pancreas and liver.
Conclusion
Roughly one-half of GCR have performed fewer than 10 cases in each of the liver, pancreas, or biliary categories at time of completion of residency. Although the mean number of complex liver and pancreatic operations performed by GCR increased slightly, the median number remained low, and the number of TA cases was virtually zero. Most GCR are unlikely to be prepared to perform complex HPB operations.
Surgical training has long sought to impart graduating residents with a sense of confidence and autonomy in performing operations. The paradigm of a stepwise increase in responsibility and independence has been used to train thousands of surgeons over the past century. Recent factors, however, including patient dictums, the Accreditation Council for Graduate Medical Education (ACGME) duty hour regulations, and attending surgeon perceptions,1–3 may have decreased the ability of general surgery residents to gain autonomy due to fewer cases being performed during training. A large body of literature has shown repeatedly that greater procedural volumes of attending surgeons are associated with improved perioperative4–16 and long-term17,18 outcomes. In fact, based on these volume-outcome relationships, organizations such as the Leapfrog Group, a coalition of health care purchasers in the United States, have encouraged patients to consider individual surgeon volumes when deciding where to undergo a complex surgical procedure.19–21 As such, data on operative volumes during surgical residency may help shed light on how well residents are being prepared for independent practice.
For many specialized surgical disciplines, exposure to a given field during general surgery residency is minimal. To that end, integrated residencies in cardiothoracic, plastic, and vascular surgery are becoming more common. Hepatopancreatobiliary (HPB) surgery remains, however, an important domain within the general surgery residency training itself. Although some residents choose to pursue further training in HPB surgery, no further training beyond general surgery is required to practice HPB surgery via HPB fellowships. Furthermore, some individuals have argued that fellowship training in HPB may not be necessary for graduating residents who want to practice HPB surgery post residency.22 Currently, the ACGME requires that chief residents participate in at least four pancreatic and three hepatic operations during their residency in order to graduate, while biliary operations are not specified.23
Information on the case volume of the graduating chief residents (GCRs) for HPB surgical procedures may not only inform assessments of resident training but also may help elucidate the current appropriateness of the training of future HPB surgeons. The purpose of the present study was to characterize procedure volumes of complex HPB procedures among GCRs. In addition, we sought to identify relative trends in operative volumes of HPB cases performed at both the chief and junior levels among GCRs during a 10-year period.
METHODS
The ACGME maintains a database that provides aggregate data on resident procedural volume.24 The database contains data on all procedures performed by the resident as part of their training. For each year, the case load of the GCR is tabulated and labeled as: surgeon chief (reserved for cases performed during chief year), surgeon junior (all cases performed in the preceding years in which the resident was the primary surgeon), teaching assistant (where the senior resident guides a junior resident through the case), first assistant (where the resident is minimally involved in the operation), and surgeon total (the aggregate number of cases for all 5 years). Each of these categories is subdivided into average number of cases, standard deviation and maximum case volume (the greatest number of cases in any category performed by a specific resident for a given year). In addition, the number of each type of operation (eg, pancreatoduodenectomy, distal pancreatectomy, partial hepatectomy, right hepatectomy, etc) is tabulated and stratified by resident operative role (ie, surgeon chief, surgeon junior, etc.) The ACGME database provides values as medians, overall percentiles, and stratified percentiles (10th, 30th, 50th, 70th, and 90th). In turn, on the basis of these data, the total number of operations, mean number of operations, and standard deviations can be derived for any given operative procedure.
In the current study, the ACGME database was queried for all pancreatic, hepatic, and biliary operations performed by graduating chief residents between 2003 and 2012. HPB cases were categorized as liver, pancreas, or biliary. Liver cases were subdivided as anatomic (eg, hemihepatectomy or extended hepatectomy), wedge resection, or other; pancreas procedures were categorized as pancreatoduodenectomy, distal pancreatectomy, or other; biliary procedures were subdivided as common bile duct exploration, choledochoenterostomy, or other. Laparoscopic versus open cholecystectomy was not distinguished for the majority of the years available. In the years in which it was distinguishable (2003–2004, 2010–2012), the overwhelming majority of cholecystectomy operations (92%) were recorded as laparoscopic. Therefore, to focus on complex HPB operations, cholecystectomy was excluded from all analyses that examined total case numbers, means, and standard deviations; however, because of the restrictive nature of the database, cholecystectomy could not be separated from median and percentile data, and so cholecystectomies were included under biliary operations when discussing median and percentile data.
Standard measures of operative volume such as mean (± standard deviation [SD]), median (10th and 90th percentiles), and maximum case volumes were reported. Median data also were reported; however, the ACGME dataset does not provide 25th and 75th percentiles. Therefore, the interquartile range was not reported, but rather the 10th and 90th percentiles were available and were reported. Trends in overall HPB operative volume, as well as changes in operative volume stratified by resident role (eg, surgeon chief, surgeon junior, etc) were examined over time (2003–2013). Raw data were not available through the ACGME, preventing certain statistical models from being used. However, linear trends in the data were examined by assessing goodness of fit model based on the means presented and were reported as the value of R2 (range 0–1). Data were analyzed using SAS 9.3 (SAS Corp., Cary, NC).
RESULTS
Between 2003 and 2013, there were 10,288 GCRs with reported data in the ACGME database. During this period, graduating chief residents logged 252,977 complex HPB operations as either the surgeon chief or surgeon junior. In turn, the mean number of HPB cases performed by a graduating chief resident during the 5 years of training was 24.6 (SD ± 5.9) (Table I). The majority of HPB cases (n = 143,516; 56.7%) were performed during the final chief year. HPB cases performed during training included pancreatectomy (109,477; 43.2%), liver resection (91,145; 36.0%), and biliary procedures (52,355; 20.7%). Mean HPB procedure case numbers were pancreatectomy (10.6 ± 4.2), liver resection (8.8 ± 3.7), and biliary procedure (5.1 ± 2.2). Regarding the specific type of HPB cases, most pancreatic procedures involved either a pancreatoduodenectomy (n = 49,980; 45.7%) or distal pancreatectomy (n = 28,144: 25.7%), whereas most liver procedures were an anatomic (n = 47,132; 51.7%) or wedge (n = 30,314; 33.3%) resection (Table II).
Table I.
Mean and total number of cases performed during the Chief (PGY-5) and Junior (PGY 1-4) years of residency in each category of complex hepatopancreatobiliary surgery
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Total | Overall mean | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ||||||||||||
| Liver (Chief) | 4.4 | 4.2 | 4.3 | 4.4 | 4.5 | 4.5 | 4.7 | 4.6 | 4.6 | 4.5 | 44.7 | 4.5 |
| Anatomic | 2.4 | 2.5 | 2.5 | 2.5 | 2.7 | 2.8 | 3.0 | 2.9 | 2.8 | 2.8 | 26.9 | 2.7 |
| Wedge | 1.4 | 1.3 | 1.3 | 1.4 | 1.3 | 1.2 | 1.2 | 1.1 | 1.0 | 0.9 | 12.1 | 1.2 |
| Other | 0.6 | 0.4 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.6 | 0.8 | 0.8 | 5.7 | 0.6 |
| Liver (Junior) | 3.7 | 4.0 | 3.7 | 4.0 | 4.2 | 4.4 | 4.7 | 4.6 | 5.0 | 5.0 | 43.3 | 4.3 |
| Anatomic | 1.3 | 1.5 | 1.4 | 1.6 | 1.8 | 1.9 | 2.2 | 2.2 | 2.3 | 2.4 | 18.6 | 1.9 |
| Wedge | 1.8 | 1.9 | 1.7 | 1.8 | 1.7 | 1.8 | 1.8 | 1.6 | 1.7 | 1.4 | 17.2 | 1.7 |
| Other | 0.6 | 0.6 | 0.6 | 0.6 | 0.7 | 0.7 | 0.7 | 0.8 | 1.0 | 1.2 | 7.5 | 0.8 |
| Pancreas (Chief) | 6.3 | 6.5 | 6.5 | 6.6 | 7.0 | 7.3 | 7.6 | 7.4 | 7.5 | 7.2 | 69.9 | 7.0 |
| Pancreatoduodenectomy | 2.9 | 3.1 | 3.2 | 3.4 | 3.6 | 3.8 | 4.0 | 3.6 | 3.7 | 3.7 | 35.0 | 3.5 |
| Distal | 1.4 | 1.4 | 1.6 | 1.7 | 1.8 | 2.0 | 2.1 | 2.1 | 2.0 | 2.0 | 18.1 | 1.8 |
| Other | 2.0 | 2.0 | 1.7 | 1.5 | 1.8 | 1.5 | 1.5 | 1.7 | 1.8 | 1.5 | 17.0 | 1.7 |
| Pancreas (Junior) | 2.9 | 3.2 | 3.1 | 3.6 | 3.6 | 3.5 | 4.0 | 4.2 | 4.2 | 4.2 | 36.5 | 3.7 |
| Pancreatoduodenectomy | 0.9 | 1.1 | 1.0 | 1.4 | 1.4 | 1.4 | 1.6 | 1.6 | 1.6 | 1.6 | 13.6 | 1.4 |
| Distal | 0.6 | 0.7 | 0.7 | 0.9 | 0.9 | 0.9 | 1.1 | 1.1 | 1.2 | 1.2 | 9.3 | 0.9 |
| Other | 1.4 | 1.4 | 1.4 | 1.3 | 1.3 | 1.2 | 1.3 | 1.5 | 1.4 | 1.4 | 13.6 | 1.4 |
| Biliary (Chief) | 2.8 | 2.7 | 2.8 | 2.6 | 2.5 | 2.4 | 2.4 | 2.2 | 2.1 | 2.0 | 24.5 | 2.5 |
| CBDE | 1.1 | 1.1 | 0.9 | 0.9 | 0.9 | 0.9 | 0.9 | 0.8 | 0.8 | 0.7 | 9.0 | 0.9 |
| CDE | 1.6 | 1.5 | 1.6 | 1.4 | 1.3 | 1.2 | 1.2 | 1.1 | 1.0 | 1.0 | 12.9 | 1.3 |
| Other | 0.1 | 0.1 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 2.6 | 0.3 |
| Biliary (Junior) | 3.1 | 3.1 | 2.8 | 2.7 | 2.6 | 2.5 | 2.7 | 2.5 | 2.5 | 2.4 | 26.9 | 2.7 |
| CBDE | 1.9 | 1.8 | 1.5 | 1.4 | 1.3 | 1.2 | 1.3 | 1.2 | 1.2 | 1.2 | 14.0 | 1.4 |
| CDE | 1.1 | 1.1 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 0.9 | 0.9 | 0.9 | 9.9 | 1.0 |
| Other | 0.1 | 0.2 | 0.3 | 0.3 | 0.3 | 0.3 | 0.4 | 0.4 | 0.4 | 0.3 | 3.0 | 0.3 |
| Subtotal | 23.2 | 23.7 | 23.2 | 23.9 | 24.4 | 24.6 | 26.1 | 25.5 | 25.9 | 25.3 | 245.8 | 24.6 |
| Total | ||||||||||||
| Liver (Chief) | 4,915 | 4,876 | 4,947 | 4,889 | 4,660 | 4,571 | 4,473 | 4,354 | 4,387 | 4,248 | 46,320 | 4,632 |
| Anatomic | 3,058 | 2,968 | 3,033 | 3,104 | 2,847 | 2,741 | 2,570 | 2,529 | 2,573 | 2,387 | 27,810 | 2,781 |
| Wedge | 983 | 1,060 | 1,190 | 1,286 | 1,272 | 1,323 | 1,374 | 1,345 | 1,364 | 1,338 | 12,535 | 1,254 |
| Other | 874 | 848 | 724 | 499 | 5,41 | 507 | 529 | 480 | 450 | 523 | 5,975 | 598 |
| Liver (Junior) | 5,460 | 5,300 | 4,818 | 4,861 | 4,484 | 4,265 | 4,150 | 3,854 | 4,060 | 3,573 | 44,825 | 4,483 |
| Anatomic | 2,621 | 2,438 | 2,320 | 2,298 | 1,940 | 1,804 | 1,660 | 1,443 | 1,557 | 1,241 | 19,322 | 1,932 |
| Wedge | 1,529 | 1,802 | 1,690 | 1,841 | 1,844 | 1,755 | 1,849 | 1,784 | 1,910 | 1,775 | 17,779 | 1,778 |
| Other | 1,310 | 1,060 | 808 | 722 | 700 | 706 | 641 | 627 | 593 | 557 | 7,724 | 772 |
| Pancreas (Chief) | 7,862 | 7,950 | 7,737 | 7,963 | 7,339 | 7,028 | 6,741 | 6,652 | 6,651 | 6,089 | 72,012 | 7,201 |
| Pancreatoduodenectomy | 4,040 | 3,922 | 3,776 | 4,149 | 3,826 | 3,627 | 3,409 | 3,286 | 3,122 | 2,836 | 35,993 | 3,599 |
| Distal | 2,184 | 2,120 | 2,156 | 2,163 | 1,989 | 1,761 | 1,732 | 1,619 | 1,466 | 1,335 | 18,525 | 1,853 |
| Other | 1,638 | 1,908 | 1,805 | 1,651 | 1,524 | 1,640 | 1,600 | 1,747 | 2,063 | 1,918 | 17,494 | 1,749 |
| Pancreas (Junior) | 4,586 | 4,452 | 4,269 | 4,185 | 3,656 | 3,523 | 3,495 | 3,178 | 3,289 | 2,832 | 37,465 | 3,747 |
| Pancreatoduodenectomy | 1,747 | 1,696 | 1,680 | 1,690 | 1,467 | 1,361 | 1,361 | 1,045 | 1,103 | 837 | 13,987 | 1,399 |
| Distal | 1,310 | 1,272 | 1,113 | 1,113 | 957 | 923 | 857 | 738 | 732 | 604 | 9,619 | 962 |
| Other | 1,529 | 1,484 | 1,476 | 1,382 | 1,232 | 1,239 | 1,277 | 1,395 | 1,454 | 1,391 | 13,859 | 1,386 |
| Biliary (Chief) | 2,184 | 2,226 | 2,272 | 2,425 | 2,439 | 2,467 | 2,613 | 2,873 | 2,843 | 2,842 | 25,184 | 2,518 |
| CBDE | 764 | 848 | 783 | 901 | 933 | 887 | 897 | 958 | 1,095 | 1,110 | 9,176 | 918 |
| CDE | 1,092 | 1,060 | 1,188 | 1,242 | 1,228 | 1,302 | 1,393 | 1,593 | 1,569 | 1,591 | 13,258 | 1,326 |
| Other | 328 | 318 | 301 | 282 | 278 | 278 | 323 | 322 | 179 | 141 | 2,750 | 275 |
| Biliary (Junior) | 2,621 | 2,650 | 2,532 | 2,754 | 2,511 | 2,575 | 2,781 | 2,817 | 2,996 | 2,934 | 27,171 | 2,717 |
| CBDE | 1,310 | 1,272 | 1,259 | 1,361 | 1,249 | 1,303 | 1,418 | 1,481 | 1,781 | 1,789 | 14,223 | 1,422 |
| CDE | 983 | 954 | 940 | 1,054 | 974 | 993 | 1,020 | 1,047 | 1,093 | 1,046 | 10,104 | 1,010 |
| Other | 328 | 424 | 333 | 339 | 288 | 279 | 343 | 289 | 122 | 99 | 2,844 | 284 |
| Subtotal | 27,628 | 27,454 | 26,575 | 27,077 | 25,089 | 24,429 | 24,253 | 23,728 | 24,226 | 22,518 | 25,2977 | 25,298 |
Anatomic, Lobectomy or segmentectomy; CBDE, common bile duct exploration; CDE, choledochoenterostomy; Chief, case volume performed during the fifth year of surgical residency; Junior, case volume performed over years 1–4; Other, other major.
Table II.
Total number and percentages of complex hepatopancreatobiliary cases logged by graduating chief residents, 2003–2012
| Procedure | n | % |
|---|---|---|
| Liver resection | ||
| Anatomic | 47,132 | 51.7 |
| Wedge | 30,314 | 33.3 |
| Other | 13,699 | 15.0 |
| Subtotal | 91,145 | 36.0 |
| Pancreatectomy | ||
| Pancreatoduodenectomy | 49,980 | 45.7 |
| Distal | 28,144 | 25.7 |
| Other | 31,353 | 28.6 |
| Subtotal | 109,477 | 43.3 |
| Biliary | ||
| CBDE | 23,399 | 44.7 |
| CDE | 23,362 | 44.6 |
| Other | 5,594 | 10.7 |
| Subtotal | 52,355 | 20.7 |
| Total | 252,977 | |
CBDE, Common bile duct exploration; CDE, choledochoenterostomy.
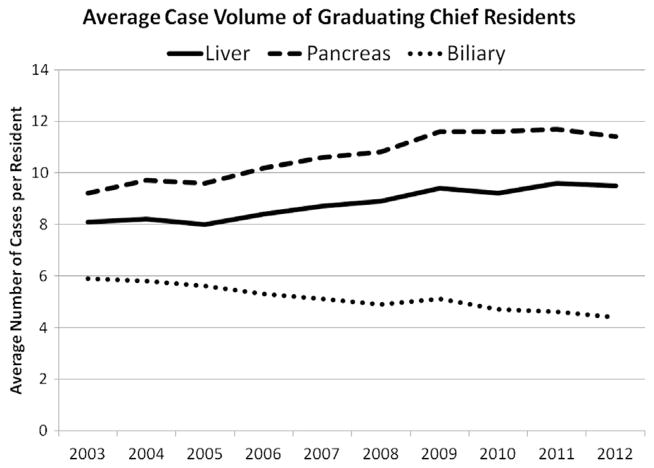
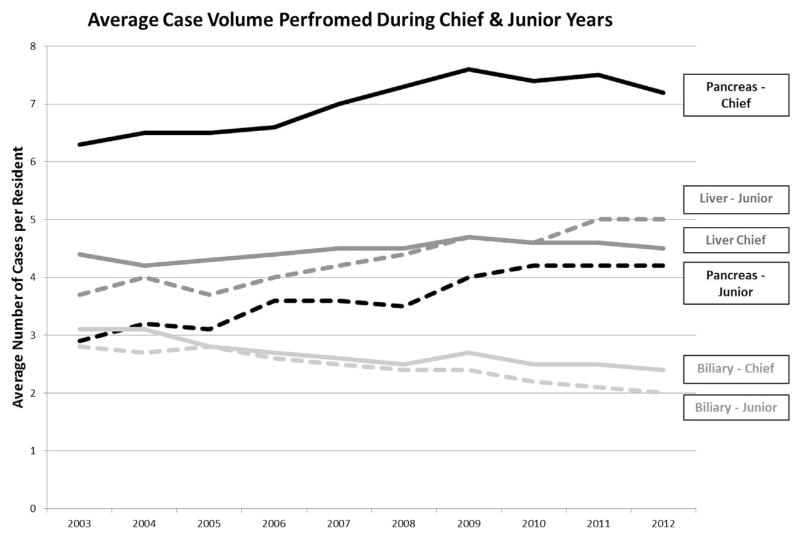
The total number of complex HPB cases performed by GCRs increased from 22,516 in 2003 to 27,191 in 2012. During this period, the mean number of HPB cases increased from 23.0 cases per resident to 24.9 (R2 = .88). The median number of pancreatic cases performed increased minimally from 7.0 to 8.0 (Fig 1), and the 10% and 90% percentile number of cases increased slightly (2003: 4 and 15 vs 2012: 4 and 20, respectively). During the study, there was an increasing trend in the mean number of pancreas operations logged by graduating chief residents (9.2 ± 5.9 to 11.4 ± 4.3; R2 = .85) (Fig 2). Of these, the mean number of major pancreatic resections (distal pancreatectomy, proximal pancreatoduodenectomy, and total pancreatectomy) also increased (5.9 ± 3.2 to 8.7 ± 4.1; R2 = .86) (Fig 3). Regarding liver cases, the median number of cases slightly increased from 7.0 in 2003 to 8.0 in 2012 (Fig 1), with the 10% and 90% percentile number of cases similarly increasing by one (2003: 4.0 and 13.0 vs 2012: 5.0 and 14.0). When we examined the mean number of liver cases performed, GCRs performed slightly more liver cases over time (8.1 ± 5.9 to 9.5 ± 3.4; R2 = 0.91). Overall, the total maximum number of operations performed by a GCR on the pancreas (2003: 51 vs 2012: 53; R2 = 0.18) and liver (2003: 38 vs 2012: 45; R2 = 0.32) increased somewhat over time, albeit with low R2 values. In contrast, the mean number of complex biliary operations decreased over time (5.9 ± 2.5 to 4.4 ± 2.1; R2 = .96), whereas the maximum could not be determined from the data available.
Fig 1.
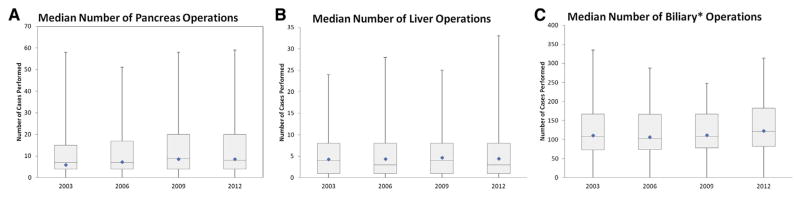
Box plots showing the median (with 10th and 90th percentiles) as well as the range (whiskers) and means (diamond), of (A) pancreas, (B) liver, and (C) biliary cases* performed over 5 years of training by graduating chief residents (2003–2012). *Includes cholecystectomy.
Fig 2.
The mean number of HPB cases performed over 5 years of training by graduating chief residents (2003–2012).
Fig 3.
The mean number of HPB cases performed by GCRs during their chief (solid line) and junior (dotted line) years (2003–2012).
Although the overall number of cases during resident training increased to some extent over the time periods examined, the proportion of HPB cases performed during the chief year decreased by 7%. Specifically, the total number of cases performed by residents went from 920,376 cases (244,360 chief year/676,016 junior years) in 2003 to 1,072,636 cases (261,104 chief/811,532 junior) in 2012. The largest decreased in HPB cases performed in the chief year was in complex liver operations (13% decrease) followed by pancreas (8%) and biliary (4%) operations. The mean number of pancreas, liver, and biliary operations performed in the chief resident year was 7.0 ± 3.3, 4.5 ± 2.5, and 2.5 ± 1.6, respectively. Of note, the median number of cases in which the GCR participated as a teaching assistant (Table III) remained zero for liver cases during the 10-year period, varied between 0 and 1 for pancreatic operations and varied between three and four for biliary operations—the majority of which were likely laparoscopic cholecystectomy. Furthermore, the 90th percentile of graduating chief residents performed few if any liver or pancreas operations as a teaching assistant.
Table III.
Median and 90th percentile of cases performed by graduating chief residents in the role of teaching assistant, 2003–2012
| Year
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
| 50th percentile | ||||||||||
| Liver | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pancreas | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biliary* | 3 | 4 | 3 | 3 | 3 | 3 | 3 | 4 | 4 | 4 |
| 90th percentile | ||||||||||
| Liver | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pancreas | 0 | 0 | 1 | 0 | 0 | 1 | 2 | 1 | 0 | 1 |
| Biliary* | 14 | 12 | 11 | 11 | 11 | 19 | 19 | 12 | 13 | 15 |
Includes laparoscopic and open cholecystectomy.
DISCUSSION
The concept and parameters of modern surgical training were first introduced by William Stewart Halsted at the turn of the century.25 At the Johns Hopkins Hospital, Halsted started the first surgical residency program with an emphasis on formal, structured integration of anatomic and physiologic principles with intensive technical training. For years, the Halsted model emphasized operative case experience to allow residents the opportunity to develop their operative skills, technical abilities, as well as intraoperative judgment. In the past, surgical residency was characterized by long hours, a large amount of repetition, and high operative volumes. In recent years, important changes in ACGME regulations have limited resident work hours and have potentially decreased the opportunity for residents to participate in operative cases.26,27 Although these changes were deemed to be appropriate and necessary, the impact on resident operative experience warrants attention and study. Previous papers have documented a well-established, volume-outcomes relationship among attending surgeons—with increasing case volume yielding improved perioperative results.7,28,29 As such, an “adequate” volume of operative cases would similarly seem to be necessary for residents to acquire competency around certain procedures, especially technically challenging operations like HPB cases. The current report is important because we were able to characterize and quantify the procedural volumes of complex HPB procedures among GCRs. Of note, the mean number of complex HPB cases preformed by a GCR was only about 25. Furthermore, the mean number of pancreas or liver cases performed at the time of residency completion was less than 10 for either type of procedure. In examining trends over time, we noted a modest increase in the mean overall number of HPB cases performed (2003: 23.2 vs 2012: 25.3). Perhaps more interestingly, however, was the finding that the proportion of HPB cases performed during the chief year decreased by 7%, and the 90th percentile of GCRs performed few, if any, liver or pancreas operations as a teaching assistant.
Currently, the ACGME requires chief residents to participate in at least seven complex HPB operations in order to graduate as a “competent” surgeon in this domain. HPB operations are, however, complex and technically demanding. Several investigators have demonstrated that a learning curve exists even among HPB surgeons who have completed their training.30 Specifically, with increased operative experience there is a dramatic decrease in operative time, estimated blood loss, and duration of stay. Importantly, Tseng et al30 reported that the number of cases needed before the learning curve plateaued was 60. In the current study, we noted that the mean number of complex HPB cases logged by a GCR was 24.6, well below the 60 cases suggested as necessary. Although the goal of residency is not necessarily to ensure “mastery” of any one domain of surgery, the low mean number of HPB cases (liver: 8.8 and pancreas: 10.6) calls into question whether residents with such low case numbers are competent to perform these types of operations after graduation. Although the average number of cases increased slightly over time, the medians changed very little, suggesting the increase was driven by a small percentage among GCRs who were at high-volume HPB centers. Furthermore, the increases seen in liver and pancreas operations were mostly during the junior years, whereas a decrease was seen more recently in the chief year. This decrease may reflect an effect of duty hours restriction; indeed, as others have noted that duty hour restrictions may affect adversely operative case number.31 In sum, data from the current study suggest that few—if any—GCR have great-enough case numbers to handle complex HPB cases without further training.
In turn, this apparent lack of target case numbers has perhaps led to a lack of confidence—real or perceived—by graduating residents.32 This finding may explain in part why the percentage of GCRs continuing on to fellowship is increasing and now approaches 80%.33 The self-confidence, autonomy, and competency that was traditionally gained in residency seems to have shifted toward fellowship training.34,35 This shift effectively has extended clinical surgery training from 5 years to 7 or more, depending on the fellowship chosen. Recently, the Flexibility in Surgical Training (FIST) program of the American Board of Surgery has begun to examine the benefit of earlier subspecialization. FIST deviates from the focus of traditional residencies by allowing up to 12 months of flexible rotations in the last 36 months of general surgery training. FIST provides an opportunity for a more focused learning experience for residents and may foster an experience that leads to more emphasis and operative exposure to certain subspecialties such as HPB and advanced gastrointestinal, as well as vascular or cardiac surgery. Regardless of an individual’s training experience, there remains, however, a steep learning curve for complex gastrointestinal operations during the first several years of practice. As such, all surgeons (fellowship trained or not) should seek appropriate mentor-ship until they are well beyond this curve whatever the number of cases required.
The role of teaching assistant is important role for a GCR to experience. Acting as a teaching assistant provides the chief resident the opportunity to “set up” the case, take initiative in directing the operation, while also leading junior residents through the steps of the procedure.36 Providing chief residents a “safe and supervised” environment to act as teaching assistant during challenging operative cases can be an important pedagogic exercise to enhance independence. Unfortunately, in recent years, the number of teaching assistant cases performed by GCRs has decreased by as much as 66% percent across all disciplines.31 For example, Feanny et al37 noted a 42% overall decrease in teaching assistant cases for senior residents, which increased to 82% when only major abdominal trauma procedures were considered. In a separate study, Carlin et al38 noted a 78% reduction in teaching assistant cases among PGY-5 residents, whereas Kairys et al31 noted a 67% decrease. In the current study, we noted a similar paucity of HPB cases in which the chief resident acted as a teaching assistant. Given the frequent complexity of HPB cases, one might expect a relative low number of teaching assistant cases. We found that the median number of cases in which the GCR participated as a teaching assistant (Table III) remained zero for liver cases during the 10-year period, varied between 0 and 1 for pancreatic operations and varied between 3 and 4 for biliary operations, which were likely all laparoscopic cholecystectomy. Perhaps more surprisingly was the finding that even the 90th percentile of GCRs performed few if any liver or pancreas operations as a teaching assistant. In aggregate, these data strongly suggest that virtually all GCRs have never experienced the role of primary “teacher” in the operating room during an HPB case.
The current paper has several limitations. As with all retrospective studies, there were certain limitations to the analyses of the ACGME database. For example, operative logs were dependent on the accuracy and reliability of the residents entering these data into the ACGME database. Any reporting bias was, however, likely a failure to log operative cases (eg, an underreporting bias). As such, if anything, the point estimates for HPB cases reported may have been an underestimation of operative volumes among graduating chief residents. For example, residents may have under-reported or failed to log cases in which they participated as a teaching assistant in particular. As such, these data need to be interpreted with this in mind. Another limitation of the dataset was the lack of more specific data on operative cases during the PGY1 through PGY4, which are only summarily referred to as “junior surgeon” in the ACGME database. Finally, data on biliary procedures also were somewhat limited as medians and percentiles for complex biliary operations exclusive of laparoscopic cholecystectomy were not available.
In conclusion, residency training requires exposure to a robust operative experience with an adequate volume of cases to ensure competency. HPB cases can be particularly complex and technically challenging with a steep learning curve even for attending surgeons.30,39,40 Data from the current paper demonstrate that many surgical residents are graduating with a low number of HPB cases (<25). In addition, the number of cases logged by GCRs as teaching assistant was extremely low, suggesting few, if any, graduating chief residents have successfully performed an HPB operation in the “attending” role. Consideration of data presented herein may help to focus efforts on training paradigms, as well as tailor mentoring programs, for those graduating residents interested in HPB surgery.
Footnotes
Presented at the 9th Annual Academic Surgical Congress in San Diego, CA, February 4–6, 2014.
References
- 1.Pellegrini CA, Warshaw AL, Debas HT. Residency training in surgery in the 21st century: a new paradigm. Surgery. 2004;136:953–65. doi: 10.1016/j.surg.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Picarella EA, Simmons JD, Borman KR, Replogle WH, Mitchell ME. “Do one, teach one” the new paradigm in general surgery residency training. J Surg Ed. 2011;68:126–9. doi: 10.1016/j.jsurg.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Dutta S, Dunnington G, Blanchard MC, Spielman B, DaRosa D, Joehl RJ. And doctor, no residents please! J Am Coll Surg. 2003;197:1012–7. doi: 10.1016/j.jamcollsurg.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Gordon TA, Burleyson GP, Tielsch JM, Cameron JL. The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann Surg. 1995;221:43–9. doi: 10.1097/00000658-199501000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lieberman MD, Kilburn H, Lindsey M, Brennan MF. Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg. 1995;222:638–45. doi: 10.1097/00000658-199511000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choti MA, Bowman HM, Pitt HA, et al. Should hepatic resections be performed at high-volume referral centers? J Gastrointest Surg. 1998;2:11–20. doi: 10.1016/s1091-255x(98)80098-x. [DOI] [PubMed] [Google Scholar]
- 7.Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–51. doi: 10.1001/jama.280.20.1747. [DOI] [PubMed] [Google Scholar]
- 8.Sosa JA, Bowman HM, Gordon TA, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998;228:429–38. doi: 10.1097/00000658-199809000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES. Effect of hospital volume on inhospital mortality with pancreaticoduodenectomy. Surgery. 1999;125:250–6. [PubMed] [Google Scholar]
- 10.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 11.Finlayson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg. 2003;138:721–5. doi: 10.1001/archsurg.138.7.721. discussion 726. [DOI] [PubMed] [Google Scholar]
- 12.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–27. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 13.Dimick JB, Cowan JA, Jr, Knol JA, Upchurch GR., Jr Hepatic resection in the United States: indications, outcomes, and hospital procedural volumes from a nationally representative database. Arch Surg. 2003;138:185–91. doi: 10.1001/archsurg.138.2.185. [DOI] [PubMed] [Google Scholar]
- 14.Dimick JB, Pronovost PJ, Cowan JA, Jr, Lipsett PA. Postoperative complication rates after hepatic resection in Maryland hospitals. Arch Surg. 2003;138:41–6. [PubMed] [Google Scholar]
- 15.Dimick JB, Wainess RM, Cowan JA, Upchurch GR, Jr, Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. J Am Coll Surg. 2004;199:31–8. doi: 10.1016/j.jamcollsurg.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 16.McPhee JT, Hill JS, Whalen GF, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246:246–53. doi: 10.1097/01.sla.0000259993.17350.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Birkmeyer JD, Warshaw AL, Finlayson SR, Grove MR, Tosteson AN. Relationship between hospital volume and late survival after pancreaticoduodenectomy. Surgery. 1999;126:178–83. [PubMed] [Google Scholar]
- 18.Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg. 2007;245:777–83. doi: 10.1097/01.sla.0000252402.33814.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birkmeyer JD, Lucas FL, Wennberg DE. Potential benefits of regionalizing major surgery in Medicare patients. Eff Clin Pract. 1999;2:277–83. [PubMed] [Google Scholar]
- 20.Birkmeyer JD, Sun Y, Goldfaden A, Birkmeyer NJ, Stukel TA. Volume and process of care in high-risk cancer surgery. Cancer. 2006;106:2476–81. doi: 10.1002/cncr.21888. [DOI] [PubMed] [Google Scholar]
- 21.Nathan H, Cameron JL, Choti MA, Schulick RD, Pawlik TM. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg. 2009;208:528–38. doi: 10.1016/j.jamcollsurg.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Chang YJ, Mittal VK. Hepato-pancreato-biliary training in general surgery residency: is it enough for the real world? Am J Surg. 2009;197:291–5. doi: 10.1016/j.amjsurg.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 23.ACGME. Procedures in Defined Categories. Accreditation Council for Graduate Medical Education; Available from: http://www.acgme.org/acgmeweb/tabid/150/ProgramandInstitutionalAccreditation/SurgicalSpecialties/Surgery.aspx. [Google Scholar]
- 24.ACGME. Case Log Statistical Reports. Available from: http://www.acgme.org/acgmeweb/tabid/274/DataCollectionSystems/ResidentCaseLogSystem/CaseLogsStatisticalReports.aspx.
- 25.Halsted WS. Medicine: A treasury of art and literature. New York: Harkavy Publishing Service; 1991. The training of the surgeon; pp. 267–71. [Google Scholar]
- 26.Lindeman BM, Sacks BC, Hirose K, Lipsett PA. Multifaceted longitudinal study of surgical resident education, quality of life, and patient care before and after July 2011. J Surg Educ. 2013;70:769–76. doi: 10.1016/j.jsurg.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 27.Sadaba JR, Urso S. Does the introduction of duty-hour restriction in the United States negatively affect the operative volume of surgical trainees? Interact Cardiovasc Thorac Surg. 2011;13:316–9. doi: 10.1510/icvts.2011.270363. [DOI] [PubMed] [Google Scholar]
- 28.Swisher SG, Deford L, Merriman KW, et al. Effect of operative volume on morbidity, mortality, and hospital use after esophagectomy for cancer. J Thoracic Cardiovasc Surg. 2000;119:1126–32. doi: 10.1067/mtc.2000.105644. [DOI] [PubMed] [Google Scholar]
- 29.Schrag D, Panageas KS, Riedel E, et al. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann Surg. 2002;236:583–92. doi: 10.1097/00000658-200211000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tseng JF, Pisters PW, Lee JE, et al. The learning curve in pancreatic surgery. Surgery. 2007;141:694–701. doi: 10.1016/j.surg.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Kairys JC, McGuire K, Crawford AG, Yeo CJ. Cumulative operative experience is decreasing during general surgery residency: a worrisome trend for surgical trainees? J Am Coll Surg. 2008;206:804–11. doi: 10.1016/j.jamcollsurg.2007.12.055. discussion 811–13. [DOI] [PubMed] [Google Scholar]
- 32.Fillmore WJ, Teeples TJ, Cha S, Viozzi CF, Arce K. Chief resident case experience and autonomy are associated with resident confidence and future practice plans. J Oral Maxillofacial Surg. 2013;71:448–61. doi: 10.1016/j.joms.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. J Am Coll Surg. 2008;206:782–8. doi: 10.1016/j.jamcollsurg.2007.12.012. discussion 788–9. [DOI] [PubMed] [Google Scholar]
- 34.Ellis MC, Dhungel B, Weerasinghe R, Vetto JT, Deveney K. Trends in research time, fellowship training, and practice patterns among general surgery graduates. J Surg Educ. 2011;68:309–12. doi: 10.1016/j.jsurg.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 35.Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258:440–9. doi: 10.1097/SLA.0b013e3182a191ca. [DOI] [PubMed] [Google Scholar]
- 36.Kairys JC, DiMuzio PJ, Crawford AG, Grabo DJ, Yeo CJ. Changes in operative case experience for general surgery residents: has the 80-hour work week decreased residents’ operative experience? Adv Surg. 2009;43:73–90. doi: 10.1016/j.yasu.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 37.Feanny MA, Scott BG, Mattox KL, Hirshberg A. Impact of the 80-hour work week on resident emergency operative experience. Am J Surg. 2005;190:947–9. doi: 10.1016/j.amjsurg.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 38.Carlin AM, Gasevic E, Shepard AD. Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg. 2007;193:326–9. doi: 10.1016/j.amjsurg.2006.09.014. discussion 329–30. [DOI] [PubMed] [Google Scholar]
- 39.Traverso LW, Shinchi H, Low DE. Useful benchmarks to evaluate outcomes after esophagectomy and pancreaticoduodenectomy. Am J Surg. 2004;187:604–8. doi: 10.1016/j.amjsurg.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 40.Schmidt CM, Turrini O, Parikh P, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010;145:634–40. doi: 10.1001/archsurg.2010.118. [DOI] [PubMed] [Google Scholar]