Abstract
Objectives
Phase II trial to assess flurpiridaz F 18 for safety and compare its diagnostic performance for PET myocardial perfusion imaging (MPI) to Tc-99m SPECT-MPI regarding image quality, interpretative certainty, defect magnitude and detection of coronary artery disease (CAD)(≥ 50% stenosis) on invasive coronary angiography (ICA).
Background
In preclinical and phase I studies, flurpiridaz F 18 has shown characteristics of an essentially ideal MPI tracer.
Methods
143 patients from 21 centers underwent rest-stress PET and Tc-99m SPECT-MPI. Eighty-six patients underwent ICA, and 39 had low-likelihood of CAD. Images were scored by 3 independent, blinded readers.
Results
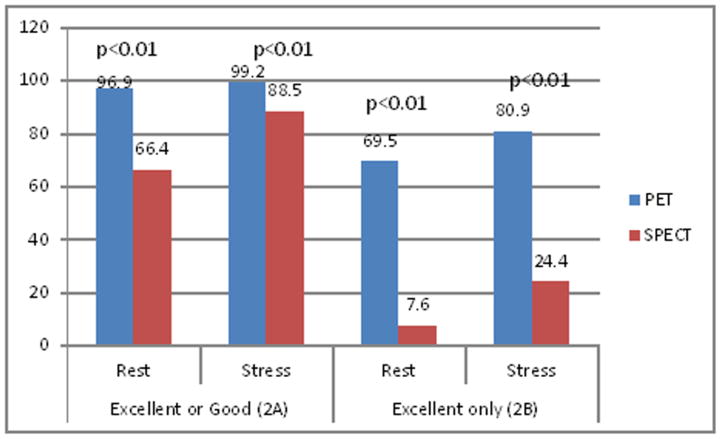
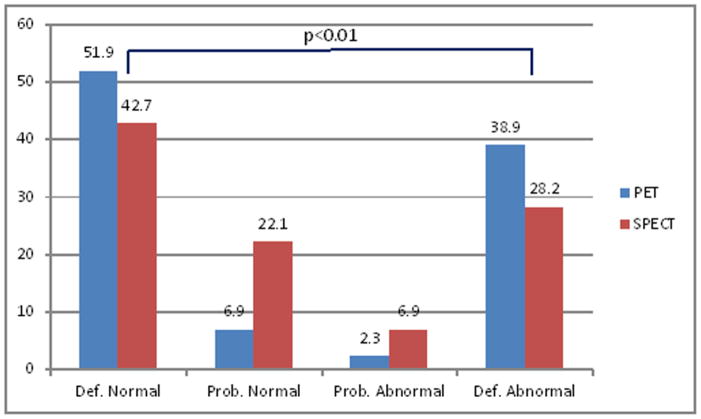
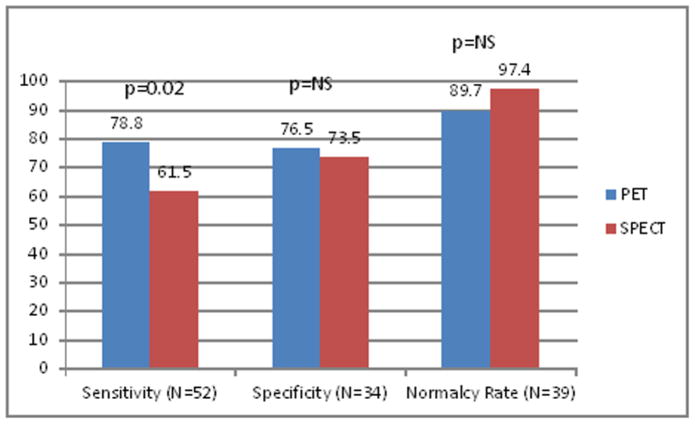
A higher % of images were rated as excellent/good on PET vs. SPECT on stress (99.2% vs. 88.5%, p<0.01) and rest (96.9% vs. 66.4, p<0.01) images. Diagnostic certainty of interpretation (% cases with definitely abnormal/normal interpretation) was higher for PET vs. SPECT (90.8% vs. 70.9%, p<0.01). In 86 patients who underwent ICA, sensitivity of PET was higher than SPECT [78.8% vs. 61.5%, respectively (p=0.02)]. Specificity was not significantly different (PET:76.5% vs. SPECT:73.5%). Receiver operating characteristic curve area was 0.82±0.05 for PET and 0.70±0.06 for SPECT (p=0.04). Normalcy rate was 89.7% with PET and 97.4% with SPECT (p=NS). In patients with CAD on ICA, the magnitude of reversible defects was greater with PET than SPECT (p=0.008). Extensive safety assessment revealed that flurpiridaz F 18 was safe in this cohort.
Conclusions
In this Phase 2 trial, PET MPI using flurpiridaz F 18 was safe and superior to SPECT MPI for image quality, interpretative certainty, and overall CAD diagnosis.
Keywords: Flurpiridaz F18, Myocarial Perfusion, SPECT
Introduction
Over the past four decades, radionuclide myocardial perfusion imaging (MPI) has become the mainstay of stress imaging for the evaluation of patients with suspected or known coronary artery disease (CAD). The method offers objective means of detecting stress induced perfusion defects due to hemodynamically significant coronary stenoses, thereby providing an important tool in risk-stratification and guiding patient management (1–3). While the radiopharmaceuticals commonly used for MPI are distributed to the myocardium in proportion to myocardial perfusion, a limitation of widely available radiopharmaceuticals used for this purpose has been a “roll-off” of their uptake at higher levels of coronary flow. (4–7) (8,9). As a consequence, mild reductions in maximal achievable coronary flow may not result in corresponding decreases in myocardial tracer uptake. Furthermore, these agents have lower spatial resolution than the PET agents F-18 and N-13. These limitations have long been the impetus toward the development of radiopharmaceuticals that would have superior uptake vs. flow relationships at peak flow rates as well as higher image resolution. Short-lived cyclotron produced PET myocardial perfusion imaging agents, including oxygen-15 water and N-13 ammonia, have excellent flow vs. uptake characteristics at high flow rates(10,11); however, these tracers are not practical for widespread clinical use due to the requirement that they be used in very close proximity to medical cyclotrons.
Flurpiridaz F 18, labeled with positron emitting isotope fluorine-18 (F-18), has recently been developed as an MPI radiopharmaceutical for use with PET(12–17). In preclinical as well as phase I studies, flurpiridaz F 18 has been shown to have essentially linear myocardial uptake throughout the range of flow(13,17). It also has high myocardial retention, low background in adjacent organs, and other characteristics that suggest it may be close to an ideal myocardial perfusion tracer(7,15,16). The purpose of this phase II trial was to assess the clinical safety of flurpiridaz F 18 and to compare the diagnostic performance of this agent to those of standard Tc-99m MPI tracers with respect to image quality, certainty of interpretation, magnitude of reversible perfusion defects, and diagnostic efficacy for detection of CAD.
Methods
Study Population
Patients were eligible for the study if they were referred for clinically indicated SPECT MPI or if they had undergone invasive coronary angiography (ICA) without percutaneous coronary intervention (PCI) within 60 days. Patients were recruited from 21 centers in the United States. All potential child-bearing female patients underwent pregnancy testing within 24 hours before receiving the PET tracer. Patients were not eligible for the study if they were less than 18 years of age, had PCI or coronary artery bypass grafting (CABG) within 6 months prior to either PET or SPECT, had non-ischemic cardiomyopathy or an ejection fraction of <35%, or were unable to undergo exercise or pharmacologic stress testing. The study was approved by the Institutional Review Boards of all participating centers and all patients provided written informed consent.
Study Design
All patients underwent SPECT MPI within 90 days before or 60 days after flurpiridaz F 18 PET MPI. If SPECT MPI had been performed prior to enrollment on an accepted SPECT camera, repeat SPECT examination was not performed. In those without such a SPECT study, both SPECT and PET scans were performed for purposes of the research trial during the study. In patients who had ICA, the ICA was performed within 60 days of PET MPI.
All patients were evaluated for flurpiridaz F 18 safety. Patients who underwent any imaging were evaluated for image quality and diagnostic certainty. Patients who underwent ICA were evaluated for test performance characteristics, while those who did not undergo ICA but who could be classified as low CAD likelihood were evaluated for normalcy rate.
Stress testing protocols
Stress tests were performed using either exercise or pharmacologic stress according to American Society of Nuclear Cardiology (ASNC) Guidelines (18), with intention to have the same stress test for both procedures. Exercise testing was performed using a standard Bruce exercise treadmill protocol, and the radiopharmaceutical was injected at the same time-point during the SPECT and PET procedures. Pharmacologic stress tests for flurpiridaz F 18 PET MPI were conducted using adenosine, regadenoson or dipyridamole. Patients were instructed to have no caffeine intake for 24 hours prior to pharmacologic stress testing and were on the same cardiac active medications at the time of both SPECT and PET studies.
SPECT Imaging Protocol
Tc-99m agents were used for all SPECT imaging (73 Tc-99m sestamibi and 35 Tc-99m tetrofosmin in 1-day protocol; 10 Tc-99m sestamibi and 6 Tc-99m tetrofosmin in 2-day protocol). There were 19 cases performed using the rest Tl-201 and stress Tc-99m dual isotope MPI protocol. All PET and SPECT cameras used in the study were subjected to and passed quality control procedures reviewed by the core laboratory for purposes of the study. SPECT scanning was performed using standard ASNC Guidelines using either rest/stress or a stress/rest protocol (18).
PET Imaging Protocol
All PET imaging was performed at rest and stress in accordance with the predefined study protocol using either PET/CT systems (n=140) or dedicated PET scanners (n=3). All PET cameras used in the study were subjected to quality control procedures for the purpose of this study. For PET/CT, attenuation correction CT scans were obtained prior to rest and stress examinations. For dedicated PET, transmission scans for attenuation correction scans were performed with a radioisotope source. Imaging was performed in list-mode. Rest imaging began at the time of the flurpiridaz F 18 injection and was continuously acquired over 20 minutes. Stress dosing began 73.4 ± 12.1 minutes after rest studies in patients undergoing exercise stress and 52.9 ± 11.2 minutes after stress in patients undergoing pharmacologic stress testing. One patient undergoing exercise stress had rest and stress procedures completed on different dates and was not included in the above summary of the rest/stress dose interval. In the pharmacologic stress group, 2.91 ± 0.70 mCi of flurpiridaz F 18 was injected at rest and 6.76 ± 1.78 mCi was injected at stress. In the exercise group, these doses were 1.93 ± 0.37 and 6.48 ± 1.23 respectively. The mean effective radiation dose to the patients from these injections is estimated to be approximately 6.4 mSv and 4.8 mSv for the pharmacologic and exercise rest/stress protocols respectively (14).
MPI image interpretation
All images were interpreted in an imaging core laboratory (Les Services Nucmed, Montreal, Canada). Both overall qualitative diagnosis and semi-quantitative 17 segment with 5 point (0=normal, 4=absent tracer uptake) scoring were employed in the independent blinded read by three expert readers who were experienced in both SPECT and PET MPI interpretation. The same three readers interpreted all of the SPECT and PET studies in independent cross-over reading sessions. The readers were blinded to which study was being performed, the type of stress, the patients’ gender, and all clinical data as well as to the reading of other readers. Image quality was classified as excellent, good, fair, poor, or uninterpretable. Certainty of overall interpretation was classified definitely normal, probably normal, probably abnormal and definitely abnormal.
For purpose of assessing diagnostic efficacy, each blinded reader rated the rest/stress perfusion and gated images as normal, ischemic, ischemic and scar, or scar. A patient was considered MPI negative if the rating was normal. Summed stress scores (SSS), summed rest scores (SRS), and summed difference scores (SDS) were calculated by the core laboratory(18). A patient was considered to have a reversible defect when the SDS was ≥2. For patients who underwent attenuation corrected SPECT or both supine and prone SPECT acquisitions, only the supine, readers assessed only the non-attenuation corrected, supine SPECT images.
Coronary angiography interpretation
All coronary angiograms were interpreted using quantitative coronary analysis (QCA) in a coronary angiography core laboratory (Perfuse, Boston, MA) blinded to the clinical or imaging results. A coronary stenosis was considered present when there was ≥ 50% diameter stenosis in any epicardial coronary artery. The presence of one or more coronary stenosis defined the presence of significant CAD. The core laboratory had no knowledge of history of myocardial infarction. Presence or absence of wall motion abnormality was not considered in interpreting the presence or absence of CAD. The determination of the presence or absence of CAD was strictly related to coronary stenosis in the native coronary arteries; arteries with patent stents were classified as no significant CAD, regardless of evidence of prior myocardial infarction. Arteries with patent bypass grafts but native coronary stenosis were classified as significant CAD.
Safety analysis
Safety assessments included blood and urine testing as well as clinical monitoring for possible adverse events (AEs). Patients were monitored for 30 minutes after the rest injection and for 60 minutes after the stress injections for clinical symptoms, vital signs and ECG changes. They were followed for 2 weeks after the drug administration for AEs. All AEs were adjudicated by the site principal investigator, including whether they were considered to be related to the drug or to the stress test. A serious adverse event (SAE) was defined as any AE considered life threatening, resulting in death, requiring in-patient hospitalization or persistent or significant disability/incapacity.
Statistical analysis
Continuous variables were expressed as mean (or median) and range or standard deviations. Paired continuous variables that were not normally distributed were compared using the Wilcoxon signed-ranks test for matched pairs, or the paired t-test if normally distributed. Categorical variables were expressed as frequencies. Primary diagnostic efficacy measures were sensitivity and specificity, and were assessed following blinded and independent reads of PET MPI and SPECT MPI data using ICA as the truth standard (n=86). Efficacy estimates for PET MPI and SPECT MPI were compared individually using a 2-sided paired test of proportions (McNemar’s test) at 5% level of significance. Normalcy rate was determined in the patients with a low likelihood of CAD and no ICA and was calculated as % of patients with normal/probably normal studies. Analysis of diagnostic efficacy was performed by reader as well as using majority rule, and the results of majority rule analysis were used in the overall efficacy analysis. Where majority rule was used for the comparison between PET and SPECT MPI, the estimate was obtained using the rating obtained by 2 of 3 blinded readers in each patient. The analysis of diagnostic certainty used a modified majority rule in which the median rating was used when 3 readers have 3 different ratings. Similarly, summaries and comparisons of SRS, SSS and SDS measures used the median of the results of 3 blinded readers. Receiver operating characteristic (ROC) curve analysis was performed in the 86 patients undergoing ICA using the comparison of area under ROC between PET MPI and SPECT MPI diagnostic efficacy. The area under ROC and confidence intervals used the empirical approach developed by DeLong, et al. (19)
The inter-reader agreement between 3 blinded readers was estimated by comparison of dichotomized ratings (normal/abnormal) and was presented using kappa and percent agreement. Intra-reader agreement in each of the reader was performed by randomizing 10% of the repeat images in the blinded read and was estimated using kappa and percent agreement.
Results
Patient population characteristics (Table 1)
Table 1.
Patient Characteristics
| Efficacy Population (N = 125) | Total (N = 143) | |
|---|---|---|
|
| ||
| Age [mean (min-max)] | 62.3 (29–85) | 62.5 (29–88) |
|
| ||
| Age >= 65 yrs | 59 (47.2%) | 67 (46.9%) |
|
| ||
| Race | ||
| White | 97 (77.6%) | 108 (75.5%) |
| Asian | 3 (2.4%) | 3 (2.1%) |
| African American | 13 (10.4%) | 16 (11.2%) |
| Other | 12 (9.6%) | 16 (11.2%) |
|
| ||
| Gender | ||
| Male | 92 (73.6%) | 107 (74.8%) |
| Female | 33 (26.4%) | 36 (25.2%) |
|
| ||
| BMI [mean (min-max)] | 28.6 (18 – 42) | 28.3 (17–42) |
|
| ||
| Prior MI | 22 (17.6%) | 26 (18.2%) |
|
| ||
| CABG | 14 (11.2%) | 17 (11.9%) |
|
| ||
| PCI | 28 (22.4%) | 31 (21.7%) |
|
| ||
| CABG or PCI | 42 (33.6%) | 48 (33.6%) |
|
| ||
| Prior MI or Revascularization | 43 (34.4%) | 50 (40.0%) |
|
| ||
| Family history of CAD | 56 (44.8%) | 66 (46.2%) |
|
| ||
| Diabetes | 29 (23.2%) | 32 (22.4%) |
|
| ||
| Tobacco use | 53 (42.4%) | 60 (42.0%) |
|
| ||
| Pre-test Likelihood of CAD | ||
| Low | 41 (32.8%) | 45 (31.5%) |
| Intermediate | 58 (46.4%) | 68 (47.6%) |
| High | 26 (20.8%) | 30 (21.0) |
There were 143 patients enrolled into the overall study population, 107 males, and the mean age was 62.5 years. The mean BMI was 28.3. There were 108 white, 3 Asian, 16 African-American, and 16 who classified themselves as “other”. Patients were stratified into 3 pre-test CAD likelihood categories: low (n=45), intermediate (n=68) and high (n=30) (18,20), the latter including patients with known CAD. In the angiographic cohort (n=86), 52 patients had significant CAD by QCA, and 34 patients had no significant CAD or normal coronary arteriograms. In this cohort, 70 patients had SPECT studies performed prior to PET and ICA; 15 patients had ICA prior to PET and SPECT studies and 1 patient had PET study completed prior to ICA and SPECT study. In this cohort, 22 had prior MI, 42 prior revascularizations, and 43 had prior MI or revascularization. Figure 1 depicts the manner in which the 143 patients were enrolled and evaluated. Eleven patients were excluded for the reasons listed, leaving 132 patients who had both SPECT MPI and PET MPI studies evaluable for image quality and diagnostic certainty comparison. Seven patients of the 132 with an intermediate or high likelihood of CAD did not undergo ICA. The remaining 125 patients were evaluable for diagnostic efficacy, and included 86 with ICA evaluated for sensitivity and specificity for angiographic CAD and 39 patients with a low likelihood of CAD assessed for normalcy rate.
Figure 1.
Summary of Patient Enrollment and Disposition
MPI=myocardial perfusion imaging; ICA=invasive coronary6 angiography
Stress tests were performed using either exercise (n=76) or pharmacologic (n=67) stress. Pharmacologic stress tests for flurpiridaz F 18 PET MPI were conducted using adenosine (n=128), regadenoson (n=7) or dipyridamole (n=8). A total of 5 of 143 patients had different stress test types between two MPI procedures.
Clinical Safety
Among the 132 patients in the safety population, two patients reported a total of 3 SAEs (dizziness, hypertension, and knee effusion) that were judged to be unrelated to study drug. Sixty-one patients (42.7% of the 143) reported 108 AEs. Thirty-six of these 61 patients received pharmacologic stress with a total of 75 AEs, and the remaining 25 patients received exercise stress with a total of 33 AEs. One hundred of the 108 AEs were considered not related to study drug. Of the remaining 8 AEs judged as possibly or probably related to the study drug, all were of either mild or moderate severity and resolved without any complications. Five of these 8 were also judged as possibly or probably related to the stress test itself. The remaining three of the 8 patients had the following: transient hypertension, mild cough, and a metallic taste. AEs associated with the Tc-99m and Tl-201 injections were not obtained. There was no evidence of clinically relevant flurpiridaz F 18 effect on QT interval in this study. An independent data monitoring committee (DMC) that reviewed safety data at regular intervals did not raise any significant safety concerns.
Image Quality
Among the 132 patients assessed for image quality, image quality was judged to be superior with flurpiridaz F 18 for both stress and rest (Figure 2). On the stress studies, 99.2% were considered to be good or excellent with flurpiridaz F 18 vs. 88.5% with Tc-99m (p<0.01). On the rest studies, image quality was considered to be good or excellent in 96.9% with flurpiridaz F 18 vs. 66.4% with Tc-99m (p<0.01). Excellent image quality alone was observed on stress images in 80.9% with flurpiridaz F 18 and in 24.4% with Tc-99m (p< 0.01) and on rest studies in 69.5% with flurpiridaz F 18 vs. 7.6% with Tc-99m (p< 0.01).
Figure 2.
Image Quality Comparing Flurpiridaz F 18 PET MPI and SPECT MPI (N = 132) Shown are the proportion of patients with excellent or good image quality (left) and excellent only (right)
Diagnostic Certainty
In the overall efficacy population of 132 patients, diagnostic certainty was greater with flurpiridaz F 18 than with Tc-99m (Figure 3). Certainty of interpretation was classified as definitely normal or definitely abnormal in 90.8% of patients by flurpiridaz F 18 and in 70.9% of patients by Tc-99m (p<0.01), with approximately a three-fold reduction in the patients in the probably normal and probably abnormal groups.
Figure 3.
Diagnostic Certainty Comparing Flurpiridaz F 18 PET MPI and SPECT MPI (N = 132)
Detection of CAD
In the 86 patients who underwent ICA and thus had a truth standard for coronary stenosis, 52 had significant CAD on ICA. The sensitivity of PET was higher than that of SPECT [78.8% vs. 61.5%, respectively (p=0.02)]. The specificity was not significantly different (76.5% for PET vs. 73.5 % for SPECT) (Figure 4). The area under the ROC curve was 0.82 ± 0.05 for PET and 0.70 ± 0.06 for SPECT (p=0.04) (Figure 5). In the 39 patients with a low likelihood of CAD, the normalcy rate was 89.7% with PET and 97.4% with SPECT (p=NS).
Figure 4.
Sensitivity and specificity comparing Flurpiridaz F 18 PET MPI and SPECT MPI for Detection of CAD
Figure 5.
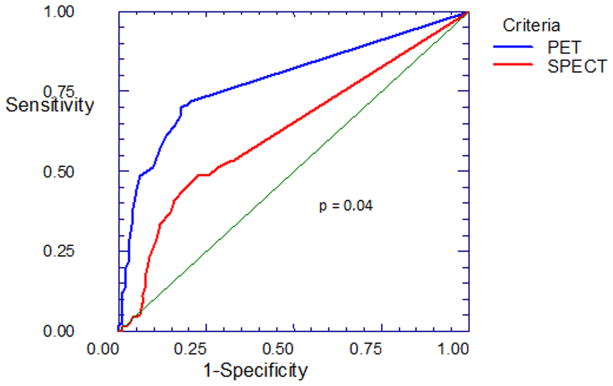
Receiver operating characteristics (ROC) analysis
Magnitude of Stress and Rest Perfusion Defect
The SSS and SRS scores in the patients who underwent ICA are shown in Table 2 according to the number of vessels abnormal on ICA. In patients with one and two vessel stenosis, the median SSS was greater with PET than with SPECT.
Table 2.
Summary of median SSS and SRS among readers by number of vessels with coronary stenosis
| SSS | SRS | |||||
|---|---|---|---|---|---|---|
| # vessels involved | PET | SPECT | p-value | PET | SPECT | p-value |
| 0 (n=34) | 2.3 | 3.6 | NS | 1.0 | 1.5 | NS |
| 1 (n=16) | 9.7 | 6.5 | <0.05 | 3.0 | 2.8 | NS |
| 2 (n=19) | 10.5 | 5.1 | <0.05 | 1.3 | 2.2 | NS |
| 3 (n=17) | 13.1 | 14.3 | NS | 2.6 | 3.8 | NS |
Magnitude and Frequency of Reversible Perfusion Defect
The magnitude of reversible perfusion defect on PET and SPECT in the patients who underwent ICA is shown in Tables 3 and 4. In the patients with coronary stenosis (Table 3), the mean SDS and the proportion of patients with SDS >2 was higher with PET than SPECT as interpreted by each reader. In the patients without coronary stenosis (Table 4), the mean SDS and the proportion of patients with SDS >2 was not significantly different between the two MPI modalities for any of the readers.
Table 3.
Summary of SDS in patients with angiography positive results (N=52)
| Reader | Statistic | PET | SPECT | p-value |
|---|---|---|---|---|
| 1 | Mean (SD) | 8.9 (7.98) | 4.8 (5.61) | 0.01 |
| SDS ≥ 2 [N(%)] | 37 (71.2%) | 28 (53.8%) | 0.06 | |
| 2 | Mean (SD) | 9.4 (7.51) | 5.7 (6.51) | 0.01 |
| SDS ≥ 2 [N(%)] | 36 (69.2%) | 26 (50.0%) | 0.02 | |
| 3 | Mean (SD) | 6.8 (5.75) | 4.1 (4.75) | 0.02 |
| SDS ≥ 2 [N(%)] | 37 (71.2%) | 26 (50%) | 0.01 |
Table 4.
Summary of SDS in patients with angiography negative results (N=34)
| Reader | Statistic | PET | SPECT | p-value |
|---|---|---|---|---|
| 1 | Mean (SD) | 2.4 (5.26) | 3.1 (5.50) | 0.24 |
| SDS ≥ 2 [N(%)] | 8 (23.5%) | 14 (41.2%) | 0.11 | |
| 2 | Mean (SD) | 1.2 (3.57) | 2.7 (5.34) | 0.13 |
| SDS ≥ 2 [N(%)] | 4 (11.8%) | 9 (26.5%) | 0.06 | |
| 3 | Mean (SD) | 1.4 (2.85) | 1.6 (3.97) | 0.91 |
| SDS ≥ 2 [N(%)] | 8 (23.5%) | 6 (17.6%) | 0.48 |
Reader agreement
Inter-reader agreement rates for presence of abnormality were ≥90% in PET MPI between 3 readers with kappa values of ≥ 0.80 between readers. Intra-reader agreement rates were slightly lower for SPECT MPI (≥80%) and kappa values of at least 0.60. Intra-reader agreement rates were 80% or greater for both imaging modalities.
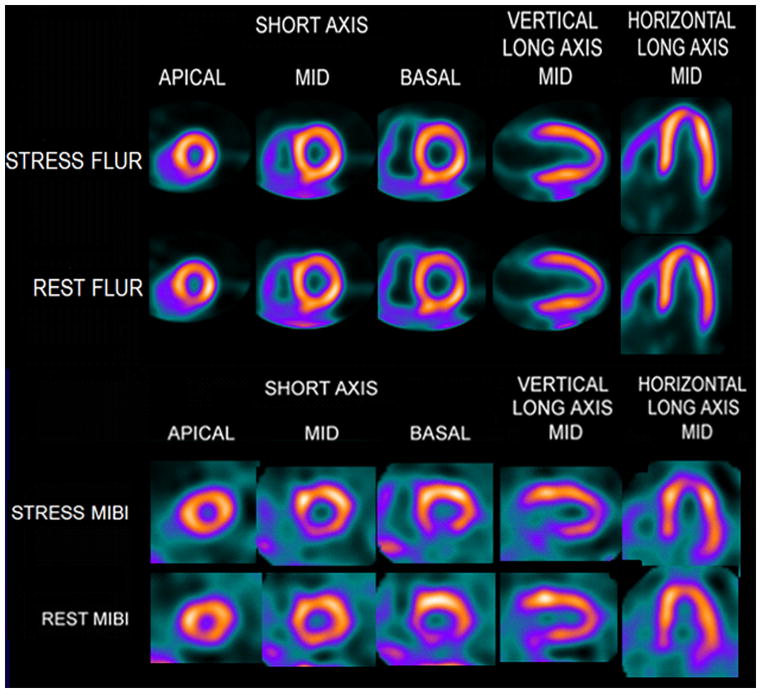
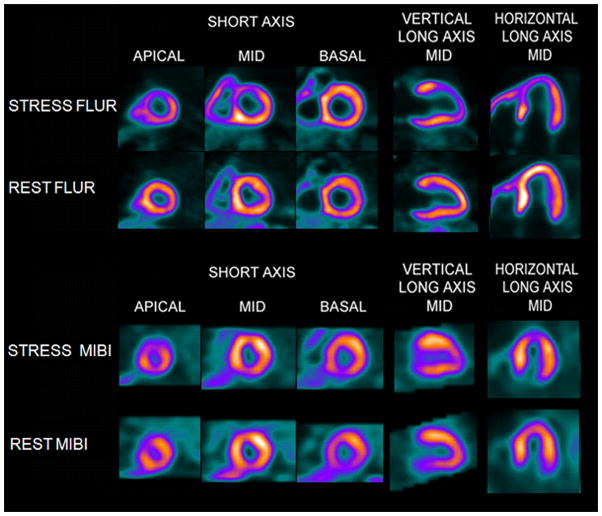
Case examples
Examples of PET and SPECT images from a patient with no coronary stenosis on ICA are shown in Figure 6 and from a patient with LAD stenosis in Figure 7.
Figure 6.
Flurpiridaz F 18 (FLUR) PET (top) and Tc-99m sestamibi (MIBI) SPECT (bottom) images from a 75 year old male, with a BMI of 32.6 and no CAD on ICA. The FLUR images were interpreted as normal, while the MIBI images were interpreted as probably abnormal with a possible reversible defect in the basal inferior wall.
Figure 7.
Flurpiridaz F 18 (FLUR) PET(top) and Tc-99m sestamibi (MIBI) SPECT(bottom) images from an 82 year old man with shortness of breath and an occluded native proximal left anterior descending (LAD) coronary artery and an occluded left internal mammary graft to the LAD and no other significant native coronary artery disease. The FLUR images show a severe reversible perfusion defect throughout the territory of the occluded proximal LAD, while the MIBI images show only a moderate perfusion defect in the distal LAD territory (apical slices).
Discussion
This is the first multicenter clinical trial comparing the diagnostic performance of a new myocardial perfusion PET tracer, flurpiridaz F-18, with conventional Tc-99m SPECT, using rigorous core laboratory image analysis. The findings show that flurpiridaz F 18 can detect hemodynamically significant obstructive CAD with greater sensitivity, superior image quality and with greater diagnostic certainty compared to SPECT MPI. The radiation doses associated with the flurpiridaz F-18 injections were approximately two times lower than those associated with standard rest/stress Tc-99m SPECT MPI protocols. Importantly, in patients with significant coronary stenosis, the frequency and magnitude of reversible perfusion defect was greater with PET than SPECT. The extensive safety assessment conducted in this Phase II study revealed that flurpiridaz F 18 was safe and well tolerated in this study.
Image quality and diagnostic certainty
Variation of image quality and image interpretation has been considered one of the limitations of conventional SPECT-MPI. In this study, image quality and diagnostic certainty were both higher with flurpiridaz F 18 PET than with SPECT. Image quality was good to excellent in a greater proportion of PET than SPECT scans, and excellent in a far greater proportion of patients, both at stress and at rest. This superior image quality was associated with a higher diagnostic certainty with flurpiridaz F-18 by independent readers. The improved image quality and diagnostic certainty are likely due to the greater conspicuity of perfusion defects, improved resolution associated with F-18 PET, as well as to the improved diagnostic certainty associated with the use of PET compared to SPECT and the use of attenuation correction for the PET studies (21). Of note, inter-reader agreement rates were high with both PET and SPECT, and were higher with the PET examinations.
Sensitivity and specificity for detection of CAD and magnitude of perfusion defects
In this study we show that flurpiridaz F18 PET was associated with improved sensitivity when compared to SPECT, with specificity similar to SPECT. Improved diagnostic accuracy was confirmed by a significantly greater ROC curve area for flurpiridaz F18 PET compared with SPECT. Several factors might explain this improved sensitivity for CAD detection, including the higher extraction fraction of the tracer, the improved spatial resolution of PET vs. SPECT, and the use of attenuation correction in the PET studies.
Magnitude of perfusion defects
The magnitude of stress and reversible perfusion defect with flurpiridaz F 18 PET was nearly double that of the Tc-99m SPECT studies in patients with coronary stenosis. The increased magnitude of perfusion defects in patients with angiographic stenosis was seen with each of the individual readers, as was the proportion of patients with disease manifesting significant amounts of ischemia (SDS ≥ 2). The magnitude of perfusion defect was not different between the tracers in the patients without significant stenosis.
Potential explanations for greater stress perfusion defect magnitude and higher sensitivity for CAD detection
Flurpiridaz F 18 exhibits near linear myocardial extraction and retention across the range of achievable myocardial blood flow (17). In contrast, a “roll off” of extraction at high myocardial perfusion rates has been reported for the commonly used single photon emission computed tomography (SPECT) agents Tc-99m-sestamibi, Tc-99m-tetrofosmin and Tl-201 (4–7) as well as for the generator produced positron emission tomography (PET) agent Rb-82 (8,9). The higher extraction fraction of flurpiridaz F 18 compared to the SPECT tracers (17) at high flow rates is likely to be an important factor explaining the differences in magnitude of perfusion defect as well as higher sensitivity for perfusion defect detection observed in this study. During maximal exercise or with maximal coronary vasodilation, areas of the myocardium supplied by vessels without stenosis demonstrate myocardial perfusion rates in the range of 3–4 ml/min/gram (8,22). These are perfusion rates at which a marked difference in uptake between tracers with high extraction fraction and low extraction fraction has been observed (4,5,17). In contrast, areas of the myocardium supplied by vessels with high grade coronary stenosis have lower levels of maximal myocardial perfusion, which would manifest similar uptake between tracers with high and low extraction fractions (4). These factors would result in a greater magnitude of a stress perfusion defect with the more highly extracted agent. In regions supplied by a vessel with mild coronary stenosis, maximal myocardial perfusion would be expected only slightly reduced compared to those supplied by vessels without stenosis. This mild reduction in myocardial perfusion might be detectable with the more highly extracted tracer, but may be insufficient to be detected by radiopharmaceuticals with lower extraction fraction (7), potentially contributing to the higher sensitivity observed with than with the Tc-99m SPECT agents in this study. Improved spatial resolution of PET compared to SPECT and the use of attenuation correction with the PET studies may have contributed to the higher accuracy of flurpiridaz F 18 PET studies. In patients who had attenuation corrected SPECT or both supine and prone SPECT imaging, only the supine SPECT imaging was assessed. Of note, the greater magnitude of reversible perfusion defect noted with flurpiridaz F18 PET raises the possibility that reassessment of the threshold for ischemia used clinically to consider a study as indicating potential benefit from revascularization may have to be recalibrated in future studies.
Limitations
This study has several limitations. Not all patients underwent ICA. The overall sensitivity of SPECT MPI in this study was generally lower than that reported in clinical literature. These results are consistent with recent well-controlled SPECT MPI studies that implemented independent blinded read using multiple readers and have been conducted for regulatory purposes (23,24). Several factors may have led to this low sensitivity in both imaging modalities. Patient selection is likely to have been a significant contributor. Since the majority of the patients underwent both SPECT and PET prior to ICA, it is possible that patients with greater amounts of ischemia by SPECT or with greater symptoms may have been more likely to have been not referred for this trial, due to the clinician’s or the patient’s desire not to have an additional stress test prior to ICA. Since patients with recent coronary intervention were excluded from the trial, patients undergoing the PET examinations after ICA are more likely to have had angiographic lesions of only borderline significance at ICA, thus potentially reducing the sensitivity of both SPECT and PET. Additionally, in individuals with prior myocardial infarction, the use of 50% stenosis QCA criteria may have led to a misclassification of patients, since a fixed perfusion defects in these patients would be expected even if the infarct related artery had been successfully opened at a prior PCI; i.e., if vessels in patients with prior PCI did not show ≥ 50% stenosis, the patients were categorized as normal, even if the vessels were supplying a region of myocardial infarction. In this regard, 48 patients had undergone prior revascularization greater than 6 months prior to the MPI studies and 26 had prior myocardial infarction. The determination of the presence or absence of CAD was based on coronary stenosis in the native coronary arteries; arteries with patent bypass grafts but native coronary stenosis were classified as significant CAD. The acceptance of patients into this trial who completed SPECT before ICA and had the PET study after ICA may have biased the population toward lower specificity by SPECT. The use of the >50% stenosis by ICA as the criterion for abnormality may have included patients as abnormal for the truth standard who do not have flow limiting stenosis, falsely lowering the sensitivity of stenosis detection. The absence of flow limiting stenosis in a substantial proportion of patients with > 50% stenosis has been documented in studies comparing angiographic stenosis to abnormalities of coronary flow reserve as measured invasively by fractional flow reserve(25). Higher spatial resolution associated with PET compared to SPECT imaging methods may have contributed to the results. Attenuation correction was applied in the PET studies and not in the SPECT studies. Although this is the largest group of patients to be studied with this novel perfusion agent, the number of patients is still relatively small, and this may affect the statistical significance of our results.
Conclusion
Flurpiridaz F 18 PET, when compared with Tc-99m SPECT has better image quality and higher diagnostic certainty. In patients with coronary stenosis by invasive coronary angiography, flurpiridaz F 18 PET manifests higher sensitivity than SPECT for detection of patients with coronary stenosis as well as greater magnitude of ischemia. These findings suggest that this new tracer may significantly improve the assessment of patients with radionuclide myocardial perfusion imaging compared to the standard SPECT MPI methods.
Acknowledgments
The authors thank Mr. Mark Hyun, CNMT, for his technical assistance in the preparation of this manuscript.
Abbreviations
- MPI
Myocardial Perfusion Imaging
- CAD
Coronary Artery Disease
- SPECT
Single Photon Emission Computed Tomography
- PET
Positron Emission Tomography
- PCI
Percutaneous Coronary Intervention
- CABG
Coronary Artery Bypass Grafting
- ASNC
American Society of Nuclear Cardiology
- CT
Computed Tomography
- SSS
Summed Stress Score
- SRS
Summed Rest Score
- SDS
Summed Different Score
- QCA
Quantitative Coronary Analysis
- AE/SAE
Adverse Event/Serious Adverse Event
- ECG
Electrocardiogram
- ICA
Invasive coronary angiography
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berman DS, Hachamovitch R, Shaw LJ. Nuclear Cardiology. In: VFROR, RWPP-W, editors. Hurst’s the Heart. 12. McGraw Hill; 2008. pp. 544–576. [Google Scholar]
- 2.Hachamovitch R, Rozanski A, Shaw LJ, et al. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J. 2011;32:1012–24. doi: 10.1093/eurheartj/ehq500. [DOI] [PubMed] [Google Scholar]
- 3.Hendel RC, Berman DS, Di Carli MF, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53:2201–29. doi: 10.1016/j.jacc.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Glover DK, Ruiz M, Edwards NC, et al. Comparison between 201Tl and 99mTc sestamibi uptake during adenosine-induced vasodilation as a function of coronary stenosis severity. Circulation. 1995;91:813–20. doi: 10.1161/01.cir.91.3.813. [DOI] [PubMed] [Google Scholar]
- 5.Glover DK, Ruiz M, Yang JY, Smith WH, Watson DD, Beller GA. Myocardial 99mTc-tetrofosmin uptake during adenosine-induced vasodilatation with either a critical or mild coronary stenosis: comparison with 201Tl and regional myocardial blood flow. Circulation. 1997;96:2332–8. doi: 10.1161/01.cir.96.7.2332. [DOI] [PubMed] [Google Scholar]
- 6.Glover DK, Gropler RJ. Journey to find the ideal PET flow tracer for clinical use: are we there yet? J Nucl Cardiol. 2007;14:765–8. doi: 10.1016/j.nuclcard.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Maddahi J. Properties of an ideal PET perfusion tracer: New PET tracer cases and data. J Nucl Cardiol. 2012;19:S30–37. doi: 10.1007/s12350-011-9491-8. [DOI] [PubMed] [Google Scholar]
- 8.Lortie M, Beanlands RS, Yoshinaga K, Klein R, Dasilva JN, DeKemp RA. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging. 2007;34:1765–74. doi: 10.1007/s00259-007-0478-2. [DOI] [PubMed] [Google Scholar]
- 9.Mullani NA, Goldstein RA, Gould KL, et al. Myocardial perfusion with rubidium-82. I. Measurement of extraction fraction and flow with external detectors. J Nucl Med. 1983;24:898–906. [PubMed] [Google Scholar]
- 10.Schelbert HR, Phelps ME, Huang SC, et al. N-13 ammonia as an indicator of myocardial blood flow. Circulation. 1981;63:1259–72. doi: 10.1161/01.cir.63.6.1259. [DOI] [PubMed] [Google Scholar]
- 11.Bergmann SR, Herrero P, Markham J, Weinheimer CJ, Walsh MN. Noninvasive quantitation of myocardial blood flow in human subjects with oxygen-15-labeled water and positron emission tomography. J Am Coll Cardiol. 1989;14:639–52. doi: 10.1016/0735-1097(89)90105-8. [DOI] [PubMed] [Google Scholar]
- 12.Huisman MC, Higuchi T, Reder S, et al. Initial characterization of an 18F-labeled myocardial perfusion tracer. J Nucl Med. 2008;49:630–6. doi: 10.2967/jnumed.107.044727. [DOI] [PubMed] [Google Scholar]
- 13.Nekolla SG, Reder S, Saraste A, et al. Evaluation of the novel myocardial perfusion positron-emission tomography tracer 18F-BMS-747158-02: comparison to 13N-ammonia and validation with microspheres in a pig model. Circulation. 2009;119:2333–42. doi: 10.1161/CIRCULATIONAHA.108.797761. [DOI] [PubMed] [Google Scholar]
- 14.Maddahi JBF, Huang S-C, Czernin J, Schelbert H, Zhu Q. Phase 1 rest-stress study of F-18 labeled BMS747158 myocardial perfusion PET tracer: Human safety, dosimetry, biodistribution, and myocardial imaging characteristics. J Nucl Med. 2009;50:1. doi: 10.2967/jnumed.111.092528. [DOI] [PubMed] [Google Scholar]
- 15.Maddahi J, Czernin J, Lazewatsky J, et al. Phase I, first-in-human study of BMS747158, a novel 18F-labeled tracer for myocardial perfusion PET: dosimetry, biodistribution, safety, and imaging characteristics after a single injection at rest. J Nucl Med. 2011;52:1490–8. doi: 10.2967/jnumed.111.092528. [DOI] [PubMed] [Google Scholar]
- 16.Yalamanchili P, Wexler E, Hayes M, et al. Mechanism of uptake and retention of F-18 BMS-747158-02 in cardiomyocytes: a novel PET myocardial imaging agent. J Nucl Cardiol. 2007;14:782–8. doi: 10.1016/j.nuclcard.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 17.Yu M, Guaraldi MT, Mistry M, et al. BMS-747158-02: a novel PET myocardial perfusion imaging agent. J Nucl Cardiol. 2007;14:789–98. doi: 10.1016/j.nuclcard.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Holly TA, Abbott BG, Al-Mallah M, et al. Single photon-emission computed tomography. J Nucl Cardiol. 2010;17:941–73. doi: 10.1007/s12350-010-9246-y. [DOI] [PubMed] [Google Scholar]
- 19.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45. [PubMed] [Google Scholar]
- 20.Gibbons RJ, Abrams J, Chatterjee K, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina) Circulation. 2003;107:149–58. doi: 10.1161/01.cir.0000047041.66447.29. [DOI] [PubMed] [Google Scholar]
- 21.Bateman TM, Heller GV, McGhie AI, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol. 2006;13:24–33. doi: 10.1016/j.nuclcard.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Slomka PJ, Alexanderson E, Jacome R, et al. Comparison of clinical tools for measurements of regional stress and rest myocardial blood flow assessed with 13N-ammonia PET/CT. J Nucl Med. 2012;53:171–81. doi: 10.2967/jnumed.111.095398. [DOI] [PubMed] [Google Scholar]
- 23.Senior R, Monaghan M, Main ML, et al. Detection of coronary artery disease with perfusion stress echocardiography using a novel ultrasound imaging agent: two Phase 3 international trials in comparison with radionuclide perfusion imaging. Eur J Echocardiogr. 2009;10:26–35. doi: 10.1093/ejechocard/jen321. [DOI] [PubMed] [Google Scholar]
- 24.Arnstein NB. An Open-Label Study to Evaluate the Use of a One-Day, Dipyrimadole-Tc-99m Tetrofosmin Imaging Protocol in the Assessment of Coronary Artery Disease. 2000 [Google Scholar]
- 25.Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med. 1994;330:1782–8. doi: 10.1056/NEJM199406233302503. [DOI] [PubMed] [Google Scholar]