Abstract
Objective
To pilot an in-home unintentional injury hazard assessment tool and to quantify potential injury risks for young children in a low-income urban setting.
Methods
Two low-income neighbourhoods in Karachi, Pakistan, were mapped, and families with at least one child between the ages of 12 and 59 months were identified. Using existing available home injury risk information, an in-home injury risk assessment tool was drafted and tailored to the local setting. Home injury assessments were done in June–July 2010 after obtaining informed consent.
Results
Approximately 75.4% of mothers were educated through at least grade 12. The main risks identified were stoves within the reach of the child (n=279, 55.5%), presence of open buckets in the bathroom (n=240, 47.7%) within the reach of the child, and pedestal fans accessible to the child (n=242, 48.1%). In terms of safety equipment, a first-aid box with any basic item was present in 70% of households, but only 4.8% of households had a fire extinguisher in the kitchen.
Conclusions
This was the first time that an in-home, all-unintentional injury risk assessment tool was tailored and applied in the context of a low-income community in Pakistan. There was a significant burden of hazards present in the homes in these communities, representing an important opportunity for injury prevention. This pilot may have future relevance to other LMICs where child injury prevention is a critical need.
INTRODUCTION
The home is the most common location for non-fatal injuries in children less than 5 years of age1 in both high-income countries (HIC)2,3 and low and middle-income countries (LMIC).4–7 Children in this age group have extended exposures to the home environment6 and their level of development does not allow their ability to judge danger thus making them prone to unintentional injuries.8
Several studies from HICs have identified various home injury risks for children less than 5 years of age, including: walkers with wheels, lack of gates or barriers for stairs, uncovered electrical outlets and appliances, and accessibility to: kitchen stoves, potential poisoning agents and breakable surfaces.8–13
Some LMICs, such as South Africa,14 India,15 Iran5,16 and Pakistan,17 have assessed home injury hazards to children related to falls, poisoning, burns, absence of stair gates, accessible drugs/chemicals and fire within reach of the child. However, to our knowledge, there is a lack of studies with comprehensive in-home injury hazard identification for children under 5 years of age in lower-income settings; such information is important for informing future studies and interventions related to in-home hazard reduction modifications.
The development of an appropriate home hazard assessment tool in the checklist format for Pakistan has been described elsewhere.18 The primary objective of this study was to pilot this home injury hazard assessment tool, and the secondary objective was to quantify in-home hazards for all unintentional injuries in young children in a lower-income urban setting in Karachi, Pakistan. This study aims to demonstrate potential utility of the risk assessment tool for local injury prevention efforts in Pakistan and in other LMICs for wider application of this tool. This will help to modify and validate the tool for future studies.
METHODS
Study setting
This study was conducted in Karachi, Pakistan, the country’s largest city with a population of ~18 million. It comprises urban and semiurban settlements.19 The communities for this study were chosen due to the lower middle-income status of residents, homes with permanent structures, relatively good literacy level of residents, and ease of access from the research base at the Aga Khan University (AKU) in Karachi.
Eligibility criteria for household enrolment into the study included: having at least one child between the ages of 12 and 59 months, caretakers who were able to read in Urdu (national language of Pakistan), and that the family planned on living in the same house for at least another 3 months. If a household had more than one child between 12–59 months of age, the caretaker selected one child as the index child for this study.
Data collectors were trained by the investigators at AKU. The injury hazard assessment was conducted during June—July 2010. The purpose of the study was explained to each household, and written informed consent was taken from the caretakers who agreed to participate in the study.
Child Home Hazard Assessment Tool
An injury hazard assessment tool, the Child Home Hazard Assessment Tool (CHAAT), was developed specifically for this study; the details of the tool development are given elsewhere.18 This tool was developed based on a thorough review of existing global literature and tools used in other HIC settings; this was modified for local language and then revised based on a pretest for community understanding prior to this pilot study. Approval for the study was obtained from the Ethical Review Committee of AKU, Pakistan and the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health, USA.
The CHHAT tool had three components. The first was related to the basic demographics of the child and caretaker. This included information including the age and gender of the child, relationship of caretaker with the child and the age of the caretaker, gender and level of education of the caretaker. The occupation of mothers who worked outside homes was noted, as well as the number of individuals living in the household and ownership of the house. The second component of the tool recorded the information on injury events in the previous 3 months. These included all injury events irrespective of whether medical treatment was required or not. The information related to the injury event included type, place, mechanism and outcome of injury. Information on changes made in the house after the incident was also elicited. These first two components were obtained by questioning the caretaker directly.
The third component of the tool was a detailed home injury hazard assessment divided by room or living area. The study team, with the permission of the caretaker, visited each area of the house to view and note each home injury hazard on the checklist. The areas of focus included the kitchen, bathroom, bedroom, courtyard, rooftop and the immediate vicinity of the house. For most questions on the checklist, ‘Yes’ was marked in case a hazard was found and ‘No’ in the absence of a hazard.
All data was entered into a Microsoft Access database. Data analysis was carried out using Stata V.10 (Statacorps LP, Texas, USA). The presence of hazards was compared against demographic variables using χ2d or Fisher’s exact test for categorical variables, and a p value<0.05 was assumed to be significant.
RESULTS
Household structure and composition
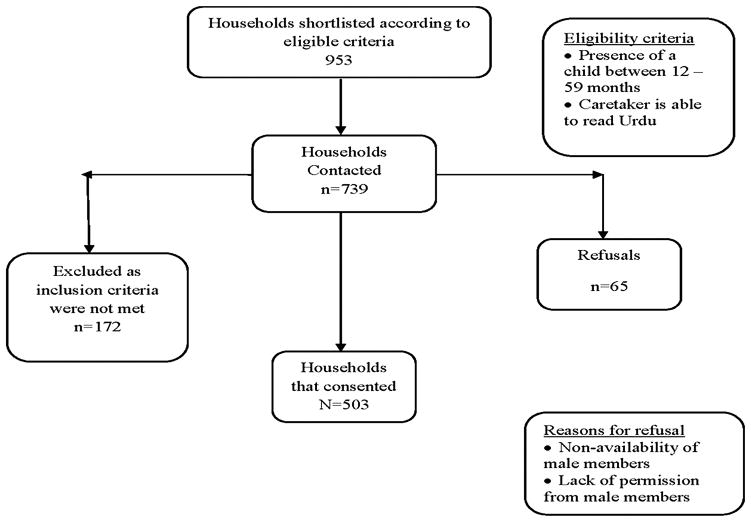
A total of 953 household were shortlisted in these two neighbourhoods of Karachi, out of which 503 (88.7%) consented to participate in the study (figure 1).
Figure 1.
Flow chart of study household enrolment.
The mean number of rooms was 2.9 (±1.5) and the average number of household members was 8.1 (±3.6) giving a mean household density (person/room) of 3.3 (±1.8). Each household had a mean of 5 (±2.8) adults and 2 (±1.0) children less than 5 years of age. One hundred and eighty-three (36.4%) households were government owned. About 87.9% (n=442) of the households had a separate kitchen, and 83.1% (n=418) had an enclosed courtyard/patio. Half the households (n=253, 50.3%) had stairs inside the house and 43 (8.5%) households had a balcony in the house. Approximately 70.4% (n=354) households had any type of first-aid supplies, and 95.2% (n=479) of households lacked a fire extinguisher.
Respondent composition
Among the respondents we interviewed, the majority were mothers (n=404, 80%). More than half were between 20–29 years of age (53.2%). Around 50% of the respondents were educated till grade 8 (n=125, 24.8%) or grade 12 (n=130, 25.8%). Mothers (n=451, 89.7%) were the main caregivers of the child at home (table 1). In about 93.6% (n=471) of the households, mothers were housewives; while n=32 (6.4%) were working. The mean number of years that respondents had been living in the community was 13 years (±12 years). The mean age of the index child in the study was 34.8 (±12.6) months (table 1).
Table 1.
Demographic characteristics of index children and respondents
| Total, n=503, (%)* | |
|---|---|
| Characteristics of child | |
| Age (months) | |
| 12–23 | 97 (19.3) |
| 24–35 | 133 (26.4) |
| 36–47 | 127 (25.2) |
| 48–59 | 146 (29.0) |
| Gender | |
| Male | 255 (50.7) |
| Female | 248 (49.3) |
| Characteristics of respondents | |
| Relationship with Child | |
| Mother | 404 (80.3) |
| Father | 3 (0.6) |
| Grandparent | 31 (6.2) |
| Uncle/aunt | 50 (9.9) |
| Others | 15 (3.0) |
| Gender | |
| Male | 6 (1.2) |
| Female | 497 (98.8) |
| Age (years) | |
| <20 | 14 (2.8) |
| 20–29 | 268 (53.3) |
| 30–39 | 173 (34.4) |
| 40–49 | 30 (6.0) |
| >50 | 18 (3.5) |
| Years in education | |
| No formal education but can read | 38 (7.6) |
| Upto 5 years | 63 (12.5) |
| 6–8 years | 62 (12.3) |
| 9–10 years | 125 (24.9) |
| 11–12 years | 130 (25.8) |
| >12 years | 85 (16.9) |
Percentages may not sum to 100% due to rounding.
Past history of injuries
In the 3 months prior to the study, 93 (18.4%) children had suffered from unintentional injuries (figure 2), out of which 53 (57%) of injuries occurred in boys and 40 (43%) in girls. Around 87% (79/91) injuries had occurred when the child was reportedly not being supervised by an adult. The most frequently occurring injuries were falls (n=64, 69%), taking place mainly in and around home (n=73/92, 79.3%). The most common location within home (64 answered) were stairs (n=19, 29.7%), bedrooms (n=13, 20.3%) and balconies (n=11, 17.2%). Cuts/scrapes (n=44, 48.4%) and bruises (n=23, 25.3%) were the most common outcomes of the injuries (91 answered). Medical care was sought for the majority of the injuries (n=45, 48.9%); 23 injuries (25%) did not require any medical care while 24 (26.1%) required hospitalisation (92 answered). The most common body part affected was the head (n=34, 36.6%).
Figure 2.
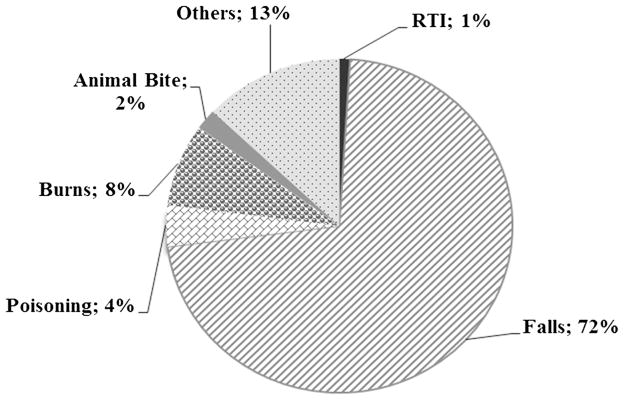
Types of unintentional injuries reported in the index child in the last 3 months (n=93). RTI, road traffic injury.
In only 15 (16.1%) cases, modifications were made in the house to prevent future similar injuries from happening. None of these 93 households had previously received information on home injuries preventive strategies.
Injury risks
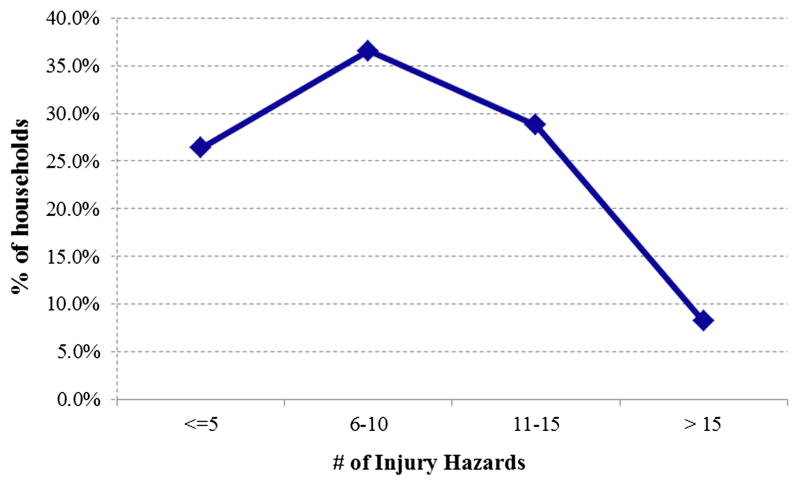
Figure 3 shows that about 35% of the households had between six and 10 injury risks, 29% had between 11 and 15 injury risks. Only 26% households had five or less risks, while 8% had 15 or more risks.
Figure 3.
Distribution of sampled houses by the number of hazards.
Table 2 summarises the presence of childhood home injury risk by area of the home. About half the households with stairs (n=253, 50.3%) did not have a stair gate (n=129, 50.5%). The balcony was not protected by a railing in 41.9% (n=18) of the households that had a balcony (n=43, 8.5%). An accessible rooftop (n=192, 38.2%) lacked a protective barrier in 91 households (47.3%). The main risks identified in the kitchen were cupboards without locks (n=282, 56.1%) and stoves within the reach of the child (n=279, 55.5%). Open buckets in the bathroom within the reach of the child were observed in 47.7% (n=240) households. Pedestal fans (n=242, 48.1%) and trolleys with wheels without wheel locks (n=242, 48.1%) were identified as the main risks in the bedroom area. Water geysers in the courtyards were also within the reach of the child in 70.4% (n=354) of homes. There were no significant differences found in the presence of injury risks by the child’s gender.
Table 2.
Prevalence of home injury hazards for childhood unintentional injuries by room/living area in Karachi, Pakistan
| Childhood home injury hazard | Total, n=503, (%)* |
|---|---|
| Kitchen | |
| Lack of fire extinguisher | 479 (95.2) |
| Lack of cupboards with locks | 282 (56.1) |
| Stove within reach of the child | 279 (55.5) |
| Matches/lighter/cooking fluids within reach of the child | 221 (43.9) |
| Knives or sharp objects within reach of the child | 186 (37.0) |
| Cleaning supplies/chemicals within reach of the child | 170 (33.8) |
| Open fire/fireplace within reach of the child | 84 (16.7) |
| Bathroom | |
| Open buckets of water within reach of the child | 240 (47.7) |
| Shampoos/soaps/acids within reach of the child | 157 (31.2) |
| Water heater (geyser)/pump/machine within reach of the child | 137 (27.2) |
| Uncovered large vat/pool of water within reach of the child | 109 (21.7) |
| Bedroom/sleeping area | |
| Pedestal fan or other sharp appliance within reach of the child | 242 (48.1) |
| Trolley with wheels without wheel locks within reach of the child | 242 (48.1) |
| Iron or other hot appliances within reach of the child | 227 (45.1) |
| Any large breakable objects, for example, perfumes on dressing table within reach of the child | 153 (30.4) |
| Bed/furniture or wall with sharp corners within reach of the child | 145 (28.8) |
| Presence of table with glass top | 136 (27) |
| Cosmetics within reach of the child | 115 (22.9) |
| Other small choking hazards within reach of the child | 97 (19.3) |
| Frayed or loose cords within reach of the child | 86 (17.1) |
| Medicines within reach of the child | 77 (15.3) |
| Presence of toys that are pointed/sharp/choking hazard | 77 (15.3) |
| Access to a walker | 77 (15.3) |
| Courtyard/rooftop/outdoors (street/road) | |
| Water heater (geyser)/pump/machine within reach of the child | 354 (70.4) |
| Structures with sharp/hard protruding components within reach of the child | 263 (52.3) |
| Open buckets of water within reach of the child | 91 (18.1) |
| Stairs without gates (n=253) | 129 (50.5) |
| Balcony without protective railing (n=43) | 18 (41.9) |
| Accessible rooftop without protective railing (n=192) | 91 (47.3) |
Percentage refers to dichotomous response (yes or no).
Supervision
Out of those who were allowed to play outside their houses, about 72.6% (n=189/257) of the caregivers supervised their child during play outside the home. Supervision was done by their mothers (n=106, 55.8%), grandparents (n=20, 10.5%) and fathers (n=12, 6.3%); nearly a quarter (n=40, 21.1%) had older children supervising the younger sibling.
DISCUSSION
The Child Home Hazard Assessment Tool (CHAAT) showed the presence of considerable injury risks for children in a lower-income setting in Karachi, Pakistan. Of note, the high response rate from the community suggests that home visits related to identification of injury risks are feasible in this population, which was also seen in an earlier study in Pakistan.17 We identified risks for falls, drowning, burns and poisoning; these findings in our study are similar to the ones reported from families with young children in other LMICs14 as well as HICs.15,17,20–22 Our study shows that 34% of the households had chemicals that were kept locked up, which is comparable to a study from the USA, where this percentage is said to be between 26% and 32%.20 However, another study from the USA showed that in 4.3% of the households not all the chemicals were locked up,23 which is in contrast with our finding. A Singaporean study showed comparable risks for sharp furniture.7
Our study showed that more than half the households had a barrier for the stairs which is in contrast with the Canadian study that showed that around one-third of the households had a staircase. A previous study carried out in Pakistan also showed a low percentage of barriers for the stairs.17 The high percentage reported in our study may be because no standard definition of stair barrier was followed. Any type of barrier used by the family of the child to block the stairs was accounted in our study, thus giving a higher percentage. In our study, the access to a baby walker was twice that compared with a hospital-based study from Canada that showed that in 7.1% households children had access to baby walkers.24 However, a study carried out in Pakistan showed that about half the study population had a baby walker.17
The association between lower levels of parental education with risk of injury in a child is well established.20,25–27 By contrast, despite the relatively high level of education of the caretakers in our study, there were several risks noted in the households enrolled in our study. Previous work shows that parents may perceive fewer risks for their children and may believe that their own child is invulnerable to risks, and follows safety rules better than other children.28 Parents may welcome passive strategies that rely on changing environment to reduce injury, whereas active strategies depend on individual behaviour to promote safety.29
Most HICs have noted a dramatic decrease in the prevalence of home injuries with the implementation of passive prevention strategies, such as smoke alarms30 and child-proof medicine bottle caps.31 In lower-income settings, most of the passive safety strategies are either not present or not implemented by the government, for example, construction codes for houses are not a prerequisite, child-resistant packaging for medicines is not mandatory, and older models of baby walkers with wheels are still being used. Furthermore, the practice of home modification does not exist with the addition of a child in the family. Particularly, lower-income families feel that they are not in a position to make risk reduction modifications to their homes because of financial cost.29
The 64th World Health Assembly placed emphasis on member states to involve all relevant stakeholders to implement child injury prevention strategies at the national level. This means the involvement of government along with other stakeholders, like communities, non-governmental organisations and civil society.32 The multilevel collaboration can facilitate the implementation of both active and passive preventive strategies and enables better resource allocation for child injury prevention programmes in the country.32
The role of supervision by caregivers is important, and lapses in attention have been reported as a risk factor for injuries.33 The phenomenon, common in many LMICs, of young children being supervised by their elder siblings was also demonstrated in this study. Previous studies showed that injuries often occur when children were either alone or attended by their siblings.29,34 However, further research is needed to identify parents’ perceptions about supervision and to identify strategies for improving supervision in these lower-income communities.
While the main goal of this study was focused on assessing the feasibility of the tool, several lessons were learnt during the process, and some of these were limitations which would need to be addressed in the main study in the future. First, the level of agreement between the three study teams quantifying injury risks in this study was not assessed; despite rigorous training, there could have been differences in perception of injury risks between observers. We aim to develop a protocol for such inter-rater reliability in the main study. Second, there was no standard measurement given for the definition of ‘within reach of the child’; it was up to the data collectors to assess accessibility for children less than 5 years of age. While this is challenging to standardise, we feel that guidelines would need to be developed to help assessments. Finally, we could not explore our pilot results by socioeconomic status within the selected lower-income settings as we specifically chose households with certain socioeconomic characteristics. For example, we selected those in which the parents could read in Urdu. In the future, we hope to apply the tool over several communities and a larger sample to allow for such analysis.
In HICs, the prevention of home injuries has been attempted through counselling and education by home visitation and provision of safety equipment. Systematic reviews and individual studies have shown the effectiveness of these home visitations in terms of safety practices,35–37 but there is inconclusive evidence regarding the actual reduction in injuries at homes.20,35,38 Unfortunately, the dissemination of injury prevention information is neglected in lower-income countries and, likewise, a subset of our sample reported having received no injury prevention information despite having had an injury event in a child in their home in the previous 3 months.
CONCLUSION
These findings point out the need for the implementation of safety and injury prevention measures that may involve legal changes and application of passive safety strategies. There is also an opportunity for important strategies that parents may employ on their own, such as storing chemicals/matches out of the reach of the child and covering open vats/buckets of water, thus making homes safer for their children.
What is already knownon this topic
A substantial proportion of unintentional injuries in young children are home-related.
These injuries at home are due to the many sources of potential hazards in the environment.
There is a lack of studies with comprehensive home injury hazard identification for children under 5 years of age in urban lower-income communities.
What this study adds
Risks for childhood falls, drowning, burns and poisoning are present in lower-income housing communities.
The Child Home Hazard Assessment Tool is for an assessment of childhood home injury risks tailored to a lower-income country context.
Acknowledgments
We would also like to thank Mr Faheem, Ms Rubaba Naeem, Ms Sana Siddiqui and Ms Jasmine for data collection in Karachi, Pakistan.
Funding Support for this study was provided by the WHO’s Division of Violence and Injury Prevention and the Johns Hopkins Center for Global Health (Grant number 1605010085). This study was a collaborative work of the Department of Emergency Medicine, Aga Khan University, Pakistan and International Injury Research Unit, Johns Hopkins Bloomberg School of Public Health, USA (WHO GCUIS Grant number 107148-96006080).
Footnotes
Contributors URK was involved in the basic conception of this study, data analysis and paper writing. AC was involved in the conception of the study and paper writing while NZ was involved in data analysis and paper writing. C-MH was involved in conception of the study and critical revision of the paper. SSDR was involved in conception of the study and critical revision of the paper, AF was involved in data analysis. AAH was involved in conception of the study and critical revision of the paper. JAR was involved in conception of the study and critical revision of the paper.
Patient consent Obtained.
Ethics approval Ethical Review Committee of Aga Khan University, Pakistan, and the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health, USA.
Provenance and peer review Not commissioned; externally peer reviewed.
Competing interests AAH, AC, URK and JAR were also partially supported by the Fogarty International Center, Grant Number D43-TW007-292 from the Fogarty International Center of the USA National Institutes of Health.
References
- 1.Peden M, Oyegbite K, Ozanne-Smith J, et al. World Report on Child Injury Prevention. World Health Organization; 2008. [PubMed] [Google Scholar]
- 2.Sengoelge M, Hasselberg M, Laflamme L. Child home injury mortality in Europe: a 16-country analysis. Eur J Public Health. 2011;21:166–70. doi: 10.1093/eurpub/ckq047. [DOI] [PubMed] [Google Scholar]
- 3.Snodgrass AM, Ang A. Unintentional injuries in infants in Singapore. Singapore Med J. 2006;47:376–82. [PubMed] [Google Scholar]
- 4.Rahman F, Andersson R, Svanström L. Health Impact of Injuries: A Population-Based Epidemiological Investigation in a Local Community of Bangladesh. J Safety Res. 1998;24:213–22. [Google Scholar]
- 5.Mohammadi R, Ekman R, Svanstrom L, et al. Rationales for home safety promotion in the Iranian primary healthcare system: results from a pilot study. Public Health. 2006;120:58–64. doi: 10.1016/j.puhe.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Fatmi Z, Kazi A, Hadden WC, et al. Incidence and pattern of unintentional injuries and resulting disability among children under 5 years of age: results of the National Health Survey of Pakistan. Paediatr Perinat Epidemiol. 2009;23:229–38. doi: 10.1111/j.1365-3016.2009.01024.x. [DOI] [PubMed] [Google Scholar]
- 7.Hyder AA, Sugerman DE, Puvanachandra P, et al. Global childhood unintentional injury surveillance in four cities in developing countries: a pilot study. Bull World Health Organ. 2009;87:345–52. doi: 10.2471/BLT.08.055798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrongiello BA, Ondejko L, Littlejohn A. Understanding toddlers’ in-home injuries: I. Context, correlates, and determinants. J Pediatr Psychol. 2004;29:415–31. doi: 10.1093/jpepsy/jsh046. [DOI] [PubMed] [Google Scholar]
- 9.Thein MM, Lee BW, Bun PY. Childhood injuries in Singapore: a community nationwide study. Singapore Med J. 2005;46:116–21. [PubMed] [Google Scholar]
- 10.LeBlanc JC, Pless IB, King WJ, et al. Home safety measures and the risk of unintentional injury among young children: a multicentre case-control study. CMAJ. 2006;175:883–7. doi: 10.1503/cmaj.050592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phelan KJ, Khoury J, Xu Y, et al. Validation of a HOME Injury Survey. Inj Prev. 2009;15:300–6. doi: 10.1136/ip.2008.020958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forjuoh SN. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–37. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Desapriya E, Scime G, Subzwari S, et al. Prevention of baby-walker-related injury. Lancet. 2009;373:545. doi: 10.1016/S0140-6736(09)60201-4. [DOI] [PubMed] [Google Scholar]
- 14.Jordaan ER, Atkins S, van Niekerk A, et al. The development of an instrument measuring unintentional injuries in young children in low-income settings to serve as an evaluation tool for a childhood home injury prevention program. J Safety Res. 2005;36:269–80. doi: 10.1016/j.jsr.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhari VP, Srivastava RK, Moitra M, et al. Risk of domestic accidents among under five children. Internet J Fam Pract. 2009;7:1. [Google Scholar]
- 16.Arshi S, Bazargani HS, Mohammadi R. Burn injury-specific home safety assessment: a cross-sectional study in iran. PLoS One. 7:e49412. doi: 10.1371/journal.pone.0049412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rehmani R, Leblanc JC. Home visits reduce the number of hazards for childhood home injuries in Karachi, Pakistan: a randomized controlled trial. Int J Emerg Med. 2010;3:333–9. doi: 10.1007/s12245-010-0238-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyder AA, Chandran A, Khan UR, et al. Childhood unintentional injuries: need for a community-based home injury risk assessments in Pakistan. Int J Pediatr. 2012;2012:203204. doi: 10.1155/2012/203204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Offical Web Portal of City District Government Karachi. 2011 Aug 30; http://www.karachicity.gov.pk/
- 20.Gielen AC, McDonald EM, Wilson ME, et al. Effects of improved access to safety counseling, products, and home visits on parents’ safety practices: results of a randomized trial. Arch Pediatr Adolesc Med. 2002;156:33–40. doi: 10.1001/archpedi.156.1.33. [DOI] [PubMed] [Google Scholar]
- 21.Marshall SW, Runyan CW, Yang J, et al. Prevalence of selected risk and protective factors for falls in the home. Am J Prev Med. 2005;28:95–101. doi: 10.1016/j.amepre.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 22.Sawalha AF. Storage and utilization patterns of cleaning products in the home: toxicity implications. Accid Anal Prev. 2007;39:1186–91. doi: 10.1016/j.aap.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Rhodes KV, Iwashyna TJ. Child injury risks are close to home: parent psychosocial factors associated with child safety. Matern Child Health J. 2007;11:269–75. doi: 10.1007/s10995-006-0171-2. [DOI] [PubMed] [Google Scholar]
- 24.King WJ, Klassen TP, LeBlanc J, et al. The effectiveness of a home visit to prevent childhood injury. Pediatrics. 2001;108:382–8. doi: 10.1542/peds.108.2.382. [DOI] [PubMed] [Google Scholar]
- 25.Richardson N, Higgins DJ, Bromfield LM, et al. The relationship between childhood injuries and family type. Family Matters. 2005;7:44–9. [Google Scholar]
- 26.Kristensen P, Kristiansen T, Rehn M, et al. Social inequalities in road traffic deaths at age 16–20 years among all 611,654 Norwegians born between 1967 and 1976: a multilevel analysis. Inj Prev. 2012;18:3–9. doi: 10.1136/ip.2011.031682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thein MM, Lee BW, Bun PY. Knowledge, attitude and practices of childhood injuries and their prevention by primary caregivers in Singapore. Singapore Med J. 2005;46:122–6. [PubMed] [Google Scholar]
- 28.Gaines J, Schwebel DC. Recognition of home injury risks by novice parents of toddlers. Accid Anal Prev. 2009;41:1070–4. doi: 10.1016/j.aap.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Munro SA, van Niekerk A, Seedat M. Childhood unintentional injuries: the perceived impact of the environment, lack of supervision and child characteristics. Child Care Health Dev. 2006;32:269–79. doi: 10.1111/j.1365-2214.2006.00593.x. [DOI] [PubMed] [Google Scholar]
- 30.Haddix AC, Mallonee S, Waxweiler R, et al. Cost effectiveness analysis of a smoke alarm giveaway program in Oklahoma City, Oklahoma. Inj Prev. 2001;7:276–81. doi: 10.1136/ip.7.4.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodgers GB. The safety effects of child-resistant packaging for oral prescription drugs. Two decades of experience. JAMA. 1996;275:1661–5. [PubMed] [Google Scholar]
- 32.Child Injury Prevention. World Health Organization; 2011. Contract No.: Document Number. [PubMed] [Google Scholar]
- 33.Morrongiello BA, Dayler L. A community-based study of parents’ knowledge, attitudes and beliefs related to childhood injuries. Can J Public Health. 1996;87:383–8. [PubMed] [Google Scholar]
- 34.Morrongiello B, Schmidt S, Schell SL. Sibling supervision and young children’s risk of injury: a comparison of mothers’ and older siblings’ reactions to risk taking by a younger child in the family. Soc Sci Med. 2010;71:958–65. doi: 10.1016/j.socscimed.2010.05.047. [DOI] [PubMed] [Google Scholar]
- 35.Kendrick D, Coupland C, Mulvaney C, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev. 2007;(1):CD005014. doi: 10.1002/14651858.CD005014.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Sznajder M, Leduc S, Janvrin MP, et al. Home delivery of an injury prevention kit for children in four French cities: a controlled randomized trial. Inj Prev. 2003;9:261–5. doi: 10.1136/ip.9.3.261. discussion 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Turner S, Arthur G, Lyons RA, et al. Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev. 2011;(2):CD003600. doi: 10.1002/14651858.CD003600.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts I, Kramer MS, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. BMJ. 1996;312:29–33. doi: 10.1136/bmj.312.7022.29. [DOI] [PMC free article] [PubMed] [Google Scholar]