Abstract
The ongoing Ebola outbreak poses an alarming risk to the countries of West Africa and beyond. To assess the effectiveness of containment strategies, we developed a stochastic model of Ebola transmission between and within the general community, hospitals, and funerals, calibrated to incidence data from Liberia. We find that a combined approach of case isolation, contact-tracing with quarantine, and sanitary funeral practices must be implemented with utmost urgency in order to reverse the growth of the outbreak. As of 19 September, under status quo, our model predicts that the epidemic will continue to spread, generating a predicted 224 (134 to 358) daily cases by 1 December, 280 (184 to 441) by 15 December, and 348 (249 to 545) by 30 December.
A multinational Ebola outbreak of unprecedented magnitude was declared a Public Health Emergency of International Concern by the World Health Organization (WHO) on 8 August 2014 (1). From Guinea, the outbreak has spread to the neighboring nations of Liberia and Sierra Leone, subsequently expanding into Nigeria and Senegal (2). Imported Ebola cases have recently led to transmission in the United States and Spain (2). As of 15 October, more than 9000 cases and 4000 fatalities have been reported, with the majority of both occurring in Liberia (2).
Initial Ebola symptoms include fever, malaise, myalgia, and headache, followed by pharyngitis, vomiting, diarrhea, and maculopapular rash (3). Severe and fatal stages are accompanied by hemorrhagic diathesis and multiple-organ dysfunction (3). Human-to-human transmission occurs primarily via contact with body fluids (3). Inadequate and improper use of personal protective equipment (PPE), compounded by staff shortages in isolation wards, poses major infection risks for health care workers (4, 5), leading to nosocomial transmission that can cripple health services (5). Ebola transmission is further exacerbated by traditional West African funeral practices that may involve washing, touching, and kissing the body (5–7). Given the current lack of licensed therapeutic treatments and vaccines (8), near-term measures to curb transmission must rely on nonpharmaceutical interventions, including quarantine, case isolation, contact precautions, and sanitary burial practices that consist of disinfecting the cadaver before inclosure in a body bag that is further disinfected.
To evaluate the effectiveness of nonpharmaceutical interventions for curtailing the epidemic in Liberia, we developed a stochastic model of Ebola disease transmission that takes into account Ebola transmission within and between the community, hospitals, and funerals (fig. S1 and supplementary materials, materials and methods, section S1). We parameterized our model using epidemiological data on disease progression and on delay from symptom onset to hospital admission obtained from the current outbreak in Liberia (table S1) (9), as well as using demographic data from the 2008 National Housing Census of Liberia (10). In the absence of data on the number of infections due to funeral transmission for the current outbreak, we parameterized the elevated risk posed by funeral attendance using odds ratios calculated from data collected during a previous Ebola outbreak in the Democratic Republic of the Congo (11). We tracked the density of individuals in the following epidemiological classes: susceptible (S), latently infected (E), infected and infectious (I), deceased (F), recovered with sterilizing immunity (R), and buried (D). To account for heterogeneity in contact and transmission between individuals in different locations, we further stratified each epidemiological class into compartments that correspond to foci of Ebola transmission: the general community, hospitals, and funerals. Hospitals were further stratified into patients and hospital workers. We parameterized hospital visitors per patient and rate of funeral attendance per death based on the number of family members in a Liberian household (10).
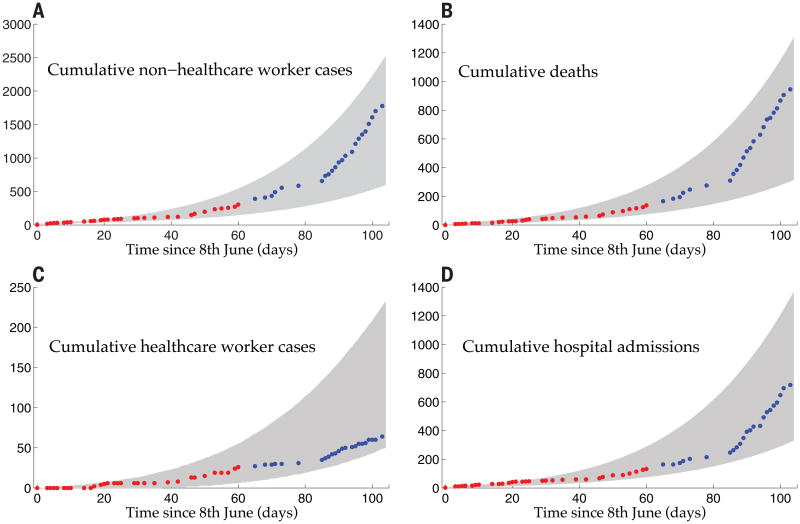
To calibrate our model, we obtained data from Situation Reports provided by the Liberian Ministry of Health and Social Welfare (table S1) (12). Outbreak control measures were not coordinated on a national scale in Liberia until 8 August 2014, when the Armed Forces of Liberia established checkpoints to restrict the movement from affected regions (13). To avoid potential confounding of behavior change as a result of interventions, we used Ebola cases, deaths, health care worker infections, and hospitalizations from Liberia reported between 8 June and 7 August 2014 to calibrate our model (Fig. 1 and supplementary materials). Given intervention assistance from the international community deployed on 20 September (14), we validated our model by comparing data between 8 August and 19 September to our model projection over that time period (Fig. 1).
Fig. 1. Model fit to data.
(A) Cumulative non–health care worker cases. (B) Cumulative deaths. (C) Cumulative health care worker cases. (D) Cumulative hospital admissions. Cumulative Ebola cases and fatalities were obtained from the Liberian Ministry of Health and Social Welfare Situation Reports nos. 10 to 89 (red circles), to which the model was fit. A 95% prediction interval was generated by 10,000 runs of the model, with parameters randomly sampled from within their confidence intervals (gray fill) (supplementary materials). Validation of the model predictions was provided by comparison with data of the cumulative Ebola cases and fatalities from Situation Reports nos. 89 to 127 (blue circles), representing 12 August 2014 to 19 September 2014, which were not used for model fitting.
In our study, we evaluated whether four WHO-recommended nonpharmaceutical interventions can efficiently control the current Ebola epidemic: (i) transmission precautions for health care workers, (ii) sanitary burial, (iii) isolation of infectious Ebola patients, and (iv) contact-tracing with follow-up and quarantine. Under no intervention strategies, our model assumes a status quo that reflects the control measures in place before 20 September. In addition, we also assessed a fifth intervention, enforcement of a cordon sanitaire, implemented by Liberian authorities. We calculated the basic reproductive number (R0)—the average number of secondary cases generated by an average primary case in an entirely susceptible population (15)—and quantified the contribution of transmission arising from each of the community, hospital, and funeral settings.
We calculated R0 for Ebola in Liberia to be 1.63 [95% confidence interval (CI), 1.59 to 1.66] before widespread interventions, which is consistent with other R0 estimates for the current outbreak (16–18) but somewhat lower than those calculated for the previous outbreaks, which ranged between 1.8 and 2.7 (19–21). Our model structure allowed us to partition the contribution of different transmission routes in sustaining the epidemic. We calculated that in the absence of nosocomial transmission, R0 = 1.48 (1.44 to 1.51); without community transmission, R0 = 1.39 (1.35 to 1.42); if only funeral transmission were present and both nosocomial and community transmission were eliminated, R0 = 1.16 (1.13 to 1.18); and if funeral transmission were absent but community and hospital transmission were present, R0 = 0.93 (0.87 to 0.99). These results for R0 imply that reducing transmission in hospitals and the community is insufficient to stem the exponentially growing epidemic. To stem Ebola transmission in Liberia, it is imperative to simultaneously restrict traditional burials, which are effectively serving as super-spreader events (22, 23).
The close agreement between the epidemiological data and the temporal trajectory of our model between 8 August and 19 September suggests that the cordon sanitaire and curfews implemented in that period (13) have had little impact on the exponential increase of Ebola before 19 September (Fig. 1) and may have even been detrimental considering the civil unrest that was fueled by these measures (24). This result is underscored by our R0 analysis that shows removal of community-based transmission only has a marginal impact on R0 value.
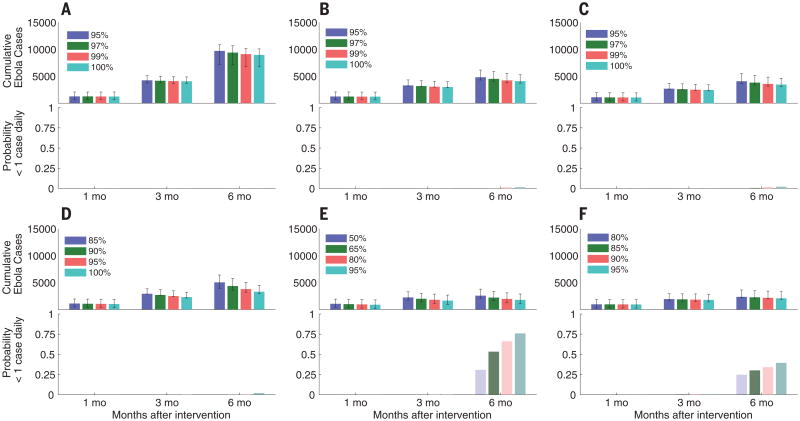
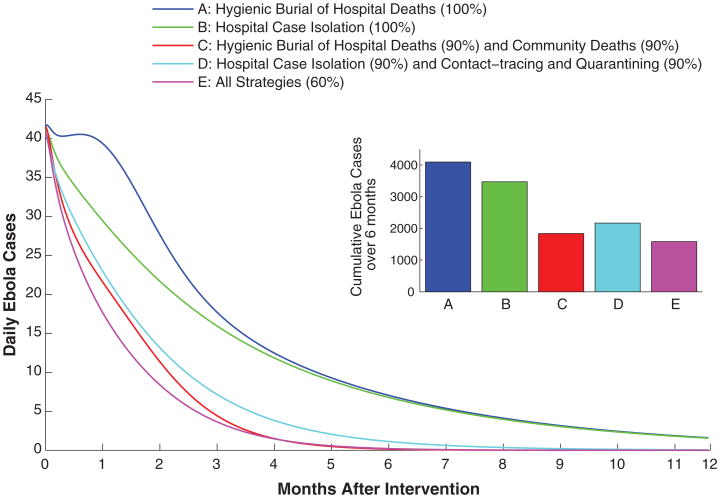
Under the status quo scenario of no change in control measures from 20 September onward, our model predicts that the epidemic will continue to spread, generating a predicted 224 (134 to 358) daily cases by 1 December, 280 cases (184 to 441) by 15 December, and 348 cases (249 to 545) by 30 December. Reducing nosocomial transmission with the use of PPE is unquestionably fundamental to maintain medical infrastructure and to implement case isolation. Nevertheless, hospital-based measures alone, like community-based efforts alone, are insufficient to stem the Ebola outbreak in Liberia (Fig. 2, A to D). Instead, these efforts must be combined with sanitary burial practices (Fig. 2E) and ideally with contact-tracing (Fig. 2F) in order to achieve a reasonable likelihood of epidemic control over the next 6 months. The potential for rapid control depends on the efficacies that can be achieved for each intervention. For example, the combination of case isolation, sanitary burials of hospital deaths, and reduction in nosocomial transmission, each applied with an efficacy of 95%, would reduce the number of daily cases in Liberia to a projected 24 (15 to 41) by 1 December, whereas combining case isolation with contact-tracing and quarantine, each with an efficacy of 90%, is predicted to reduce the number of daily cases in Liberia to 9 (5 to 23) by 1 December. A strategy that achieves efficacies of 60% for sanitary burial, case isolation, and contact-tracing combined could reduce the number of daily Ebola cases to 7 (2 to 13) by 1 December and to 0 (0 to 3) by 15 March in Liberia (Fig. 3). Achieving efficacies in the region of 90% for any one intervention in Liberia would be challenging, if not unrealistic. Thus, combining all of the nonpharmaceutical approaches considered here offers the greatest promise for curtailing the epidemic.
Fig. 2. Nonpharmaceutical intervention effectiveness.
(A to F) Model predictions of the cumulative number of new cases after 1, 3, and 6 months after 20 September 2014, as well as the probability of fewer than one case daily after these months for (A) 80% reduction in transmission to health care workers combined with different reductions in community transmission, (B) increasing proportions of sanitary burial of hospital deaths, (C) increasing proportions of hospital case isolation, (D) 90% reduction in transmission to health care workers and increasing sanitary burial of hospital deaths, (E) 80% sanitary burial of hospitalized deaths with increasing sanitary burial of community deaths, and (F) 80% case isolation of hospitalized patients with concurrent contact-tracing and quarantine of infected contacts. One thousand simulations of the stochastic model were used to generate the cumulative case count error bars (95% prediction interval) and to estimate the probability of less than one new case per day.
Fig. 3. Effectiveness comparison of individual and combined intervention strategies.
Model predictions of the daily number of new and cumulative cases after 6 months for sanitary burial and hospital deaths, sanitary burial of community deaths, case isolation of hospitalized patients, contact-tracing in the community, and quarantine of infected contacts.
To investigate the applicability of our national-scale results to a more local scale, we fit our model to data from Montserrado County (12). Here, too, our results show that swift control of the epidemic on a local level is only achievable through a combination of control strategies, which is consistent with our results on the national level (fig. S3).
Recent reports by WHO have suggested that cases in Liberia are underreported, although it is difficult to know by how much (25). To evaluate the impact of underreporting on our results, we refit our model to account for a range of plausible underreporting. In addition, we considered the possibility that underreporting differs between community and hospital settings. When we recalculated intervention effectiveness using these new model fits (fig. S2), we found that underreporting would reduce our estimates of intervention effectiveness. For example, an underreporting rate of 20% predicts an average of 37 daily cases by 15 March compared with 8 daily cases for perfect reporting for the strategy of 80% case isolation as well as 50% contact-tracing and quarantining. Moreover, our results show that when only community cases are underreported (fig. S2, D to F), the effectiveness of nosocomial interventions is reduced (fig. S2D) because there is proportionally greater transmission within the community than observed. This possibility for lower effectiveness that arises when accounting for underreporting further argues for rapid application of diverse control interventions.
Underreporting might also manifest via asymptomatic infections, which have been observed in previous outbreaks (26). Although there is considerable empirical uncertainty regarding the proportion of infections that are asymptomatic, our sensitivity analysis indicates that the larger the proportion of asymptomatic infections, the greater the impact of intervention effectiveness (Fig. 4 and supplementary materials).
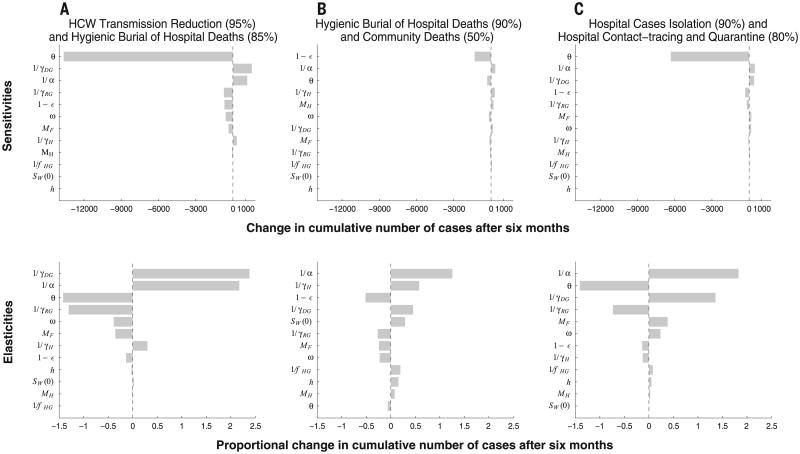
Fig. 4. Sensitivities and elasticities with respect to epidemiological parameters.
(A to C) Sensitivities and elasticities of cumulative cases under (A) 85% successful sanitary burial of hospital deaths with 95% reduction in transmissibility to health care workers for 6 months (Fig. 2D, blue line); (B) successful sanitary funeral of 90% hospital deaths and 50% community deaths, respectively; and (C) 90% successful hospital case isolation with concurrent contact-tracing and quarantine of 80% infected contacts. We varied the number of pre-outbreak health care workers [SW(0)], the incubation period (1/α), the duration from symptom onset to death if not hospitalized (1/γDG), the duration from symptom onset to recovery if not hospitalized (1/γRG), the duration between symptom onset and hospitalization (1/γH), the hospitalization rate per person for reasons other than Ebola (h), the duration of hospitalization for reasons other than Ebola (1/fHG), the number of funeral attendees with close contact to the body (MF), the number of hospital visitors per patient (MH), the transmission rate at funerals relative to general community (ω), the fraction of asymptomatic infections (1 – ε), and the hospital admission rate (θ). For each parameter varied, we recalibrated and reran the model.
To evaluate the impact of uncertainty around epidemiological parameters on predicted outcomes, we analyzed the sensitivity and elasticity of intervention effectiveness to variation in epidemiological parameters (Fig. 4). Unsurprisingly, we find that lower transmissibility at funerals (ω) reduces the effectiveness of the funeral-based interventions (Fig. 4 and supplementary materials). More generally, the effectiveness of an intervention that reduces transmission to health care workers and increases sanitary burial of hospital cases is most sensitive and elastic to the incubation period (1/α), the durations from symptom onset to death (1/γDG), and recovery (1/γRG) (Fig. 4A). In contrast, when the intervention scenario focuses on community transmission alone, there is less sensitivity to these parameters (Fig. 4, B and C).
Also to be considered is the impact of feasibility, human behavior, and likely adherence to recommendations (27) on the effectiveness of intervention strategies when making policy recommendations. As the epidemic unfolds, funeral attendance and traditional burial practices may decline with increased awareness of the disease, facilitating the enforcement of sanitary burial practices. In contrast, other behavior changes may hinder intervention efforts. For example, contact-tracing has recently become more challenging because of relocation of contacts from urban to rural communities (28). Additionally, case isolation outside of Monrovia is hampered by the scarcity of ambulances for prompt referral to Ebola-specific treatment centers (29). Similarly, the implementation of hospital-based interventions will depend on treatment center capacity and admission rates, in that an insufficient number of beds and low admission rates reduce the effectiveness of hospital-based interventions (Fig. 4, A and C). Because our model does not explicitly account for hospital capacity, our predicted outcomes regarding hospital-based interventions may be optimistic, further under-scoring the importance of combining hospital-based interventions with contact-tracing and quarantine. Additionally, we stress the protection of health care workers as an essential component for maintaining the medical infrastructure and for implementing any response strategy. Although recent cumulative case data over October 2014 from Liberia suggest that the exponential growth that has characterized the epidemic for both communities and health care workers may be slowing down (30), it is too early to tell whether this apparent reduction in the effective reproductive number is a result of control measures initiated toward the end of September.
Although our predictions concur with an analysis of the 1995 Democratic Republic of Congo and 2000 Uganda outbreaks, suggesting that funeral transmission is an important driver of Ebola transmission (20), our study also reveals that at this point in the current Liberian outbreak, sanitary burial alone is insufficient to swiftly contain disease spread, unlike for past Ebola outbreaks. Other models assess countrywide intervention effectiveness (16, 31) but do not explicitly parse the specific intervention strategies that are effective in particular settings. In contrast, our model has the complexity to demonstrate that a combination of case isolation in the hospital settings, contact-tracing in the community, and sanitary burials must be implemented to achieve a pronounced likelihood of controlling the outbreak over the next 6 months.
Until very recently, Ebola has been extremely neglected. Consequently, scarcity of data on both previous outbreaks and on the current outbreak limits the complexity of models that can be reasonably parameterized. In particular, there are no epidemiological data available with which to parameterize a spatially explicit model of Ebola transmission. Such data would be useful for predicting not only the scale of interventions required but also the geographical areas on which to focus control efforts and preparedness strategies.
Ebola poses an urgent threat not only to West Africa but also to the international community. The most effective approach to both limiting international spread of Ebola and minimizing local death toll is to control the disease at its source. We find that only a concerted suite of targeted nonpharmaceutical interventions has the potential to curtail the outbreak over the next few months. In the absence of immediate and effective multifaceted action, our predictions suggest that hundreds of new infections will be arising daily by early December in Liberia alone. The implementation of effective interventions needed to reverse the growth of the Ebola outbreak in impoverished West African countries will be logistically challenging even with substantial international aid, but impossible without it.
Supplementary Material
Acknowledgments
The research was supported by the National Institutes of Health (NIH 2 U01 GM087719 and 5 U01 GM105627) and the Notsew Orm Sands Foundation. We thank S. G. Gaffney, A. Hofmann, and M. Traina for helpful feedback on the manuscript. All model code and data are available via https://github.com/abhiganit/EbolaCodes/tree/master/Science_Code.
Footnotes
Supplementary Materials: www.sciencemag.org/content/346/6212/991/suppl/DC1
Materials and Methods
References (32–42)
The data reported in this paper are tabulated in the supplementary materials.
References and Notes
- 1.World Health Organization. WHO Statement on the Meeting of the International Health Regulations Emergency Committee Regarding the 2014 Ebola Outbreak in West Africa. World Health Organization; 2014. available at www.who.int/mediacentre/news/statements/2014/ebola-20140808/en. [Google Scholar]
- 2.World Health Organization. WHO: Ebola Response Roadmap Update—15 October 2014. World Health Organization; 2014. pp. 1–11. available at http://apps.who.int/iris/bitstream/10665/136508/1/roadmapsitrep15Oct2014.pdf?ua=1. [Google Scholar]
- 3.Heymann D, editor. American Public Health Association. Control Commun Dis Man. American Public Health Association; Washington, DC: 2008. pp. 204–206. [Google Scholar]
- 4.Ksiazek TG, et al. J Infect Dis. 1999;179(suppl. 1):S177–S187. doi: 10.1086/514321. [DOI] [PubMed] [Google Scholar]
- 5.Khan AS, et al. J Infect Dis. 1999;179(suppl. 1):S76–S86. doi: 10.1086/514306. [DOI] [PubMed] [Google Scholar]
- 6.Hewlett BS, Amola RP. Emerg Infect Dis. 2003;9:1242–1248. doi: 10.3201/eid0910.020493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leroy EM, et al. Science. 2004;303:387–390. doi: 10.1126/science.1092528. [DOI] [PubMed] [Google Scholar]
- 8.Galvani AP, Ndeffo-Mbah ML, Wenzel N, Childs JE. Ann Intern Med. 2014 doi: 10.7326/M14-1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO Ebola Response Team. N Engl J Med. 2014;371:1481–1495. doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liberia Institute of Statistics and Geo-Information Services. 2008 National Population and Housing Census: Preliminary Results. Government for the Republic of Liberia; Monrovia, Liberia: 2008. [Google Scholar]
- 11.Roels TH, et al. J Infect Dis. 1999;179(suppl. 1):S92–S97. doi: 10.1086/514286. [DOI] [PubMed] [Google Scholar]
- 12.Ministry of Health & Social Welfare. Liberia Ebola SitRep no 10-130. 2014 available at www.mohsw.gov.lr/content_display.php?sub=report2.
- 13.The Bureau of Public Affairs. Daily Media Summary, 08-08-2014. Minist Foreign Aff Repub Lib. 2014 available at www.mofa.gov.lr/public2/2press.php?news_id=1226&related=7&pg=sp.
- 14.S. O. S. International, International SOS–Liberia. Int SOS. 2014 available at www.internationalsos.com/ebola/index.cfm?content_id=396&language_id=ENG.
- 15.Anderson RM, May RM. Infectious Diseases of Humans: Dynamics and Control. Oxford University Press; 1991. [Google Scholar]
- 16.Althaus CL. PLOS Curr. 2014 doi: 10.1371/currents.outbreaks.91afb5e0f279e7f29e7056095255b288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomes MFC, et al. PLOS Curr. 2014 doi: 10.1371/currents.outbreaks.cd818f63d40e24aef769dda7df9e0da5. [DOI] [Google Scholar]
- 18.Fisman D, Khoo E, Tuite A. PLOS Curr. 2014 doi: 10.1371/currents.outbreaks.89c0d3783f36958d96ebbae97348d571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White LF, Pagano M. Stat Med. 2008;27:2999–3016. doi: 10.1002/sim.3136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Legrand J, Grais RF, Boelle PY, Valleron AJ, Flahault A. Epidemiol Infect. 2007;135:610–621. doi: 10.1017/S0950268806007217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chowell G, Hengartner NW, Castillo-Chavez C, Fenimore PW, Hyman JM. J Theor Biol. 2004;229:119–126. doi: 10.1016/j.jtbi.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd-Smith JO, Schreiber SJ, Kopp PE, Getz WM. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galvani AP, May RM. Nature. 2005;438:293–295. doi: 10.1038/438293a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daily Media Summary, 08-18-2014. Minist Foreign Aff Repub Lib. 2014 available at www.mofa.gov.lr/public2/2press.php?news_id=1246&related=7&pg=sp.
- 25.World Health Organization. Why the Ebola outbreak has been underestimated. World Health Organization; 2014. available at www.who.int/mediacentre/news/ebola/22-august-2014/en. [Google Scholar]
- 26.Leroy EM, et al. Lancet. 2000;355:2210–2215. doi: 10.1016/s0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- 27.Bauch CT, Galvani AP. Science. 2013;342:47–49. doi: 10.1126/science.1244492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ministry of Health & Social Welfare. Liberia Ebola SitRep no 136. 2014 available at www.mohsw.gov.lr/documents/Liberia%20Ebola%20Sit%20Rep%20136%20Sept%2028,%202014.pptx%20New.pdf.
- 29.Ministry of Health & Social Welfare. Liberia Ebola SitRep no 135. 2014 available at www.mohsw.gov.lr/documents/Liberia%20Ebola%20Sit%20Rep%20135%20Sept%2027,%202014.pptx%20New.pdf.
- 30.Nishiura H, Chowell G. Euro Surveill. 2014;19:20894. doi: 10.2807/1560-7917.es2014.19.36.20894. [DOI] [PubMed] [Google Scholar]
- 31.Ministry of Health & Social Welfare. Liberia Ebola SitRep no 149. 2014 available at www.mohsw.gov.lr/documents/SITRep%20149%20Oct%2011th,%202014.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.