Abstract
The aim of the present study was to determine whether probiotics could help to improve the eradication rates and reduce the side effects associated with anti-Helicobacter pylori treatment, and to investigate the optimal time and duration of probiotic administration during the treatment, thus providing clinical practice guidelines for eradication success worldwide. By searching Pubmed, Embase, the Cochrane Central Register of Controlled Trials and the Science Citation Index, all the randomized controlled trials (RCTs) comparing probiotics as adjuvant agents of anti-H. pylori standard triple-therapy regimens with placebo or no treatment were selected. Statistical analysis was performed with the Comprehensive Meta Analysis Software. Subgroup, meta-regression and sensitivity analyses were also carried out. Twenty-one RCTs involving a total of 3,814 participants met the inclusion criteria. The pooled eradication rates of the probiotic group were 80.3% (1,709/2,128) by intention-to-treat (ITT) and 83.8% (1,709/2,039) by pro-protocol analyses; the pooled relative risk (RR) by ITT for probiotic supplementation versus treatment without probiotics was 1.12 [95% confidence interval (CI), 1.06–1.19]. A reduced risk of overall H. pylori therapy-related adverse effects was also found with probiotic supplementation (RR, 0.60; 95% CI, 0.40–0.91). The subgroup analyses showed that probiotic supplementation prior and subsequent to the treatment regimen both improved eradication rates for H. pylori infection. Furthermore, probiotic treatment lasting >2 weeks and including Lactobacillus or multiple probiotic strains significantly enhanced the efficacy. In conclusion, supplementation with probiotics for H. pylori eradication may be effective in increasing eradication rates and decreasing therapy-related side effects. Probiotic administration prior or subsequent to therapy and for a duration of >2 weeks may increase the eradication efficacy.
Keywords: probiotics, Helicobacter pylori, adjuvant treatment, meta-analysis
Introduction
Helicobacter pylori is a Gram-negative spiral bacterium that colonizes the gastric mucosa. H. pylori infection affects 70–90% the population in developing countries, and 25–50% of the population in developed countries (1). Standard triple-therapy regimens with a proton-pump inhibitor (PPI) and two of amoxicillin, clarithromycin and nitroimidazole have been used for the eradication of H. pylori; however, their efficacy has been declining with the increasing resistance of H. pylori to antibiotics, and the H. pylori eradication failure rate varies widely, from 10 to 45% (2). At present, the administration of antibiotics for 10–14 days or high-dose PPI (twice a day) has been recommended for H. pylori eradication therapy by the Maastricht IV consensus conference (3); this has resulted in the increased incidence of undesirable side effects, such as antibiotic-associated diarrhea, nausea or vomiting, during anti-H. pylori therapy, which can lead to reduced compliance (4). Among the alternative anti-H. pylori options that have been considered, probiotics have attracted substantial interest. Previous studies have shown that probiotics, predominantly including Lactobacillus, Saccharomyces boulardii and Bifidobacterium, demonstrate anti-H. pylori activity in vitro and in animal models of H. pylori infection (5–8). Probiotics have also been used as an adjuvant therapy to H. pylori infection in order to reduce the side effects of antibiotics and improve the eradication rates (9–11); however, the results have been inconsistent, with certain studies showing that adjuvant probiotics did not improve eradication rates or reduce the side effects (12–14).
Previous meta-analyses have demonstrated that probiotics, as adjuvant agents, have a positive effect on improving eradication rates and reducing adverse events (15–20); however, certain recent studies have produced results that are inconsistent with those of the previous meta-analyses (21,22). Furthermore, the appropriate timing and duration of probiotic administration are indeterminate (23,24). Miscellaneous probiotics may be used in an anti-H. pylori treatment regimen, but it is unclear whether the efficacy of different probiotics is similar. As such, an updated meta-analysis of randomized controlled trials (RCTs) comparing the eradication rates and adverse events of probiotics as an adjuvant treatment with those of a placebo (or blank control) in participants with H. pylori infection is required. The aim of the present study was to evaluate, by meta-analysis, the efficacy and safety of the administration of probiotics as adjuvant agents of standard triple-therapy regimens for H. pylori infection, and to investigate the appropriate timing and duration of the probiotic administration in order to provide evidence to support this use of probiotics in clinical practice.
Materials and methods
Study sources and search methods
The present meta-analysis was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guidelines (25). Pubmed (1966 to November 2013), Embase (1946 to November 2013), the Cochrane Central Register of Controlled Trials (Issue 11, 2013) and the Science Citation Index (SCI; 1945 to November 2013) were searched according to Medical Subject Heading and text terms: (Helicobacter pylori OR H. pylori) AND (probiotic OR probiotics OR yeast OR yeasts OR yogurt OR Lactobacillus OR Bifidobacterium OR Saccharomyces). Authors were also asked to provide unpublished randomized trial results. In addition, the ClinicalTrials.gov website (https://clinicaltrials.gov/) was searched for registered RCTs whose results had not yet been published, and relevant studies were identified from the references.
Inclusion and exclusion criteria
Articles that were eligible for inclusion in the meta-analysis met the following inclusion criteria: i) RCTs; ii) any age, endoscopic findings and symptoms at the time of enrollment; iii) confirmation of eradication outcome by urea breath test, histology or H. pylori stool antigen ≥4 weeks after therapy; iv) trials comparing at least two branches of treatment consisting of a control group (with placebo or no additional intervention) and an experimental group (the standard triple-therapy regimen plus probiotics); v) restriction of the species of probiotics to Lactobacillus, Bifidobacterium, Saccharomyces or a mixture of the three; vi) obtainable eradication rates.
The exclusion criteria for the meta-analysis were as follows: i) Undeterminable eradication rates; ii) use of agents other than probiotics as the adjuvant therapy for H. pylori infection in the experimental group; iii) articles without full-text; iv) studies in languages other than English.
Validity assessment
Two reviewers independently, but not blinded to the authors or journal, assessed the quality of the studies that met the inclusion criteria. Any disagreements between the reviewers were resolved by consulting a third reviewer. The quality of the studies was assessed by the Jadad scale (26,27). The scores, from 0 to 5, were evaluated according to three criteria: Randomization, double blinding and description of withdrawals and dropouts (26,27). To avoid the duplication of data, if trials were published repeatedly by the same authors or institutions, only the most recently published article was included.
Data extraction
Standardized data abstraction sheets were prepared. Data were extracted for study quality and type; the timing of probiotic administration; duration of eradication treatment; duration of probiotic treatment; species of probiotics; location of trials; time of publication; anti-H. pylori regimens; number and age of enrolled patients; diagnostic methods for detecting H. pylori infection prior to enrollment and subsequent to study completion; eradication rates by intention-to-treat (ITT) analysis; rates of successful and failed eradication; and total side effects (diarrhea, vomiting nausea, taste disturbance, epigastric pain and total adverse effects) from all included studies.
Statistical analysis
Statistical analysis was performed with the Comprehensive Meta-Analysis Software (version 2; Biostat, Inc., Englewood, NJ, USA). The primary outcomes for the meta-analysis were the H. pylori eradication rates and the side effects among the trials comparing probiotic and control arms, based on ITT and pro-protocol (PP) analysis. The efficacy of H. pylori eradication was measured using relative risk (RR) to compare the frequency of eradication in the probiotic arm with that in the control arm.
The RRs for all studies were pooled into a summary RR, using either a fixed- or random-effects model, based on inverse variance methods. If the heterogeneity had a statistically significant difference, the random-effects model was employed; if not, the fixed-effects model was adopted. P-values and 95% confidence intervals (CIs) were provided for the summary RRs. The heterogeneity index (I2) was additionally calculated. Other assessments of heterogeneity were accomplished using the Q-test, and a Z-test was employed to assess the pooled effects. Funnel plots, Egger’s test and Begg’s test were utilized to estimate the publication bias. Meta-regression analyses were performed to interpret the reasons for the heterogeneity.
Subgroup analysis
Subgroup analysis for the meta-analysis was performed depending on the time that the probiotics were administered [‘before’ (used prior to the eradication regimens), ‘same’ (simultaneously with the eradication regimens) and ‘after’ (beginning with the eradication regimens and continuing subsequent to the eradication regimens)], the regimens utilized, the duration of the probiotic treatment (≤2 weeks and >2 weeks), the species of probiotics, the age of the subjects, the Jadad score (>2, and ≤2), the PPIs of the experimental group and the duration of the eradication regimens.
Results
Description of the studies
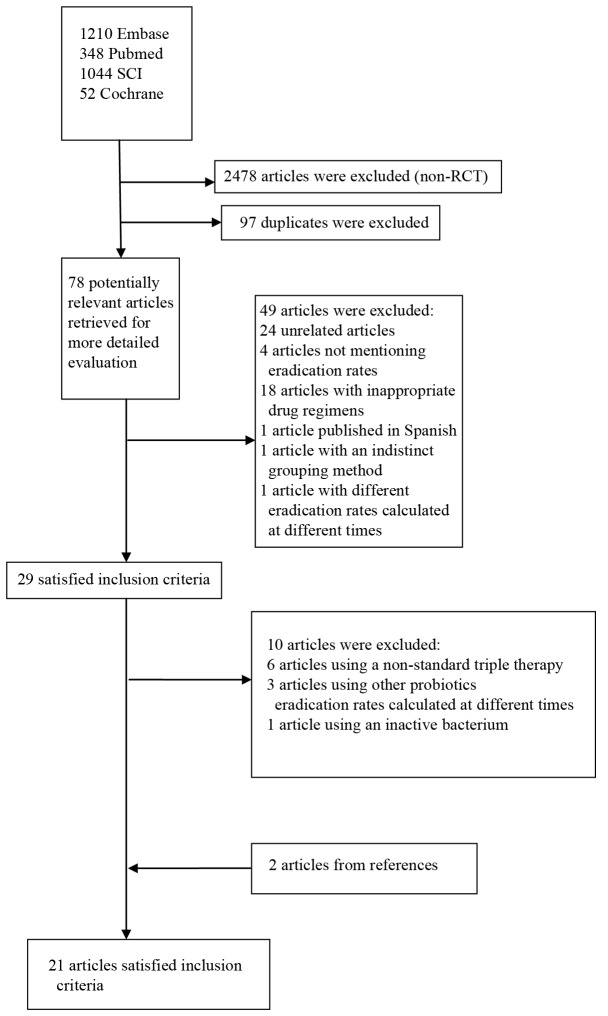
The bibliographical search yielded a total of 2,653 studies. Among the studies from Pubmed, the Cochrane Central Register of Controlled Trials, Embase and the SCI, another 2,478 articles were excluded subsequent to examining the article type. Having excluded any duplicates, 78 potentially relevant articles were retrieved for more detailed assessment. Following examinations of the title and abstract, another 24 unrelated articles, four articles that did not mention eradication rates, 18 articles with inappropriate drug regimens and one study published in Spanish (28) were excluded. The full-text articles were then reviewed and another two articles were excluded, one of which was excluded for indistinct grouping methods (29) and the other as a result of eradication rates being calculated at different times. Twenty-nine articles were further evaluated for details. Six articles were excluded due to a non-standard triple therapy regimen (9,12,30–33), three articles were excluded due to Lactobacillus, Bifidobacterium or Saccharomyces not being used in the eradication regimen (34–36) and one article due to an inactive bacterium being used (37). Two articles from the studied references were additionally included in the meta-analysis (38,39). Twenty-one RCTs ultimately met the inclusion criteria (11,38–57) (Table I) (Fig. 1).
Table I.
Characteristics of the included studies.
| First author, year (ref.) | Country, language | Total cases (treatment/control) | Patients | Eradication regimen | Regimen duration (days) | Species of probiotics | Time of probioticsa | Duration of probiotics (days) | H. pylori infection: Initial diagnosis re-checking | Jadad score |
|---|---|---|---|---|---|---|---|---|---|---|
| Armuzzia, 2001 (41) | Italy, English | 120 (60/60) | Adults | P: 40 mg b.i.d. C: 500 mg, b.i.d. T: 500 mg b.i.d. |
7 | Lactobacillus GG | 3 | 14 | 13C-UBT, H. pylori IgG antibody measurements/13C-UBT | 3 |
| Armuzzia, 2001 (40) | Italy, English | 60 (30/30) | Adults | R: 20 mg b.i.d. C: 500 mg b.i.d. T: 500 mg b.i.d. |
7 | Lactobacillus GG | 3 | 14 | 13C-UBT, H. pylori IgG antibody measurements/13C-UBT | 5 |
| Cremonini, 2002 (42) | Italy, English | 85 (64/21) | Adults | R: 20 mg b.i.d. C: 500 mg b.i.d. T: 500 mg b.i.d. |
7 | Lactobacillus GG; Saccharomyces boulardii | 3 | 14 | 13C-UBT/13C-UBT | 5 |
| Sheu, 2002 (43) | Taiwan, English | 160 (80/80) | Adults | L: 30 mg b.i.d. A: 1 g, b.i.d. C: 500 mg, b.i.d. |
7 | Lactobacillus; Bifidobacterium | 3 | 35 | Histology and RUT/13C-UBT | 2 |
| Myllyuioma, 2005 (44) | Finland, English | 47 (23/24) | Adults | L: 30 mg b.i.d. C: 500 mg b.i.d. A: 1 g b.i.d. |
7 | Lactobacillus GG (ATCC 53103); L. rhamnosus LC (DSM7061); P. freudenreichii ssp. shermanii JS (DSM7076); B. breve Bb99 (DSM 13692) | 3 | 28 | 13C-UBT, serology/13C-UBT, serology [IgG decrease by 40% (four months)] | 5 |
| Sýkora, 2005 (45) | Czech Republic, English | 86 (39/47) | Children | O: 10 mg (15–30 kg) or 20 mg (30 kg) b.i.d. A: 25 mg/kg b.i.d. C: 7.5 mg/kg b.i.d. |
7 | Lactobacillus casei (DN-114 001) | 3 | 14 | At least two of three: RUT, histology and culture/HpSAT, 13C-UBT | 5 |
| Płewinska, 2006 (46) | Poland, English | 60 (30/30) | Children | O: 0.5 mg/kg/24 h, b.i.d. A: 50 mg/kg/24 h b.i.d. C: 15 mg/kg/24 h, b.i.d. |
30 | Lactobacillus acidophilus; Lactobacillus rhamnosus | 3 | 28 | RUT, histology/RUT, histology | 1 |
| de Bortoli, 2007 (47) | Italy, English | 206 (105/101) | Adults | E: 20 mg b.i.d. C: 500 mg b.i.d. A: 1 g b.i.d. |
7 | Lactobacillus reuteri | 1 | 7 | HpSAT (99), 13C-UBT (107)/13C-UBT | 2 |
| Cindoruk, 2007 (48) | Turkey, English | 124 (62/62) | Adults | L: 30 mg b.i.d. C: 500 mg b.i.d. A: 1000 mg b.i.d. |
14 | Lactobacillus plantarum; L. reuterii; L. casei subsp. rhamnosus; Bifidobacterium infantis; B. longum; L. salivarius; L. acidophilus; Streptococcus termophilus; L. sporogenes (Lactobacillaceae) | 1 | 14 | HE or Giemsa stain/13C-UBT | 5 |
| Kim, 2008 (49) | Korea, English | 347 (168/179) | Adults | PPI b.i.d. C: 500 mg b.i.d. A: 1 g b.i.d. |
7 | L. acidophilus HY 2177; L. casei HY 2743; B. longum HY 8001; S. thermophilus B-1 | 2 | 28 | RUT, 13C-UBT, histology/13C-UBT | 3 |
| Hurduc, 2009 (50) | Romania, English | 90 (48/42) | Children | O/E: 1 mg/kg/day, b.i.d. A: 50 mg/kg/day, b.i.d. C: 15 mg/kg/day, b.i.d. |
7 or 10 | Saccharomyces boulardii | 3 | 28 | Histology, RUT/histology, RUT | 3 |
| Szajewska, 2009 (51) | Poland, English | 83 (44/39) | Children | O: 0.5 mg/kg b.i.d. A: 25 mg/kg b.i.d. C: 10 mg/kg b.i.d. |
7 | Lactobacillus GG | 1 | 7 | Two of three tests (13C-UBT, histopathology, RUT)/13C-UBT | 5 |
| Song, 2010 (52) | Korea, English | 991 (660/331) | Adults | O: 20 mg, b.i.d. A: 1 g, b.i.d. C: 500 mg, b.i.d. |
7 | S. boulardii | 3 | 28 | Histology/UBT | 3 |
| Yaşar, 2010 (53) | Turkey, English | 76 (38/38) | Adults | P: 40 mg, b.i.d. A: 1 g b.i.d., C: 500 mg b.i.d. |
14 | Bifidobacterium | 1 | 14 | HE and modified Giemsa staining/13C-UBT | 1 |
| Medeiros, 2011 (54) | Portugal, English | 62 (31/31) | Adults | E: 20 mg b.i.d. A: 1 g, b.i.d. C: 500 mg, b.i.d. |
8 | L. acidophilus | 1 | 8 | Culture/13C-UBT | 2 |
| Ozdil, 2011 (11) | Turkey, English | 285 (98/187) | Adults | Group 1: L: 30 mg b.i.d. C: 500 mg b.i.d. A: 1 g b.i.d. Group 2: E: 40 mg b.i.d. Lev: 500 mg q.d. A: 1000mg b.i.d. Group3b: E: 40 mg b.i.d. A: 1000 mg b.i.d. for 5 days E: 40 mg b.i.d. L: 500 mg q.d. T: 500 mg t.i.d. for 5 days |
14 | Saccharomyces boulardii | 1 | 14 | Giemsa-staining/monoclonal HpSAT | 1 |
| Deguchi, 2012 (55) | Japan, English | 229 (115/114) | Adults | R: 10 mg b.i.d. A: 750 mg b.i.d. C: 200 mg b.i.d. |
7 | Lactobacillus gasseri OLL2716 | 2 | 28 | Culture, RUT, histology/13C-UBT, HpSAT or culture | 2 |
| Du, 2012 (56) | China, English | 234 (155/79) | Adults | O: 20 mg b.i.d. C: 500 mg b.i.d. A: 1g b.i.d. |
7 | Lactobacillus acidophilus; S. faecalis; B. subtilis | 2 or 3 | 21 | RUT, 13C or 14C-UBT, pathology/13C or 14C-UBT | 2 |
| Tolone, 2012 (57) | Italy, English | 68 (34/34) | Children | O: 1 mg/kg (before breakfast) b.i.d. A: 50 mg/kg (after meals), b.i.d. C: 15 mg/kg (after meals) b.i.d. |
7 | Lactobacillus plantarum; L. reuterii; L. casei. subsp. rhamnosus; Bifidobacterium infantis ; B. longum; L. salivarius; L. acidophilus; Streptococcus termophilus; L. sporogenes | 1 | 7 | 13C-UBT/13C-UBT | 2 |
| Wang, 2014 (38) | China, English | 100 (49/51) | Children | PPI: 0.6–0.8 mg/kg b.i.d. C: 10–15 mg/kg b.i.d. A: 30–50 mg/kg b.i.d. |
14 | L. acidophilus; Bifidobacterium bifidum | 3 | 42 | 13C-UBT/13C-UBT | 2 |
| Dajani, 2013 (39) | Italy, English | 301 (195/106) | Children | PPI: NR C: 500 mg b.i.d. A: 1000 mg b.i.d. |
7 | Bifidobacterium infantis | 1 or 2 | 7 or 21 | 14C-UBT/14C-UBT | 2 |
1 represents ‘same’, i.e. administration simultaneously with the eradication regimens; 2 represents ‘before’, i.e. used prior to the eradication regimen/continuing until the end of the eradication treatment; 3 represents ‘after’, i.e. beginning with the eradication treatment and continuing subsequent to the end of the eradication treatment/used when the eradication regimen has ended.
Sequence therapy.
P, pantoprazole; C, clarithromycin; R, rabeprazole; T, tinidazole; L, lansoprazole; O, omeprazole; Lev, levofloxacin; E, esomeprazole; PPI, proton-pump inhibitor; b.i.d., twice a day; t.i.d., three times a day; q.d., daily; UBT, urea breath test; IgG, immunoglobulin G; RUT, rapid urease test; ATCC, American Type Culture Collection; HpSAT, H. pylori stool antigen test; HE, hematoxylin and eosin; NR, no report.
Figure 1.
Flow diagram of the trials identified and selected. SCI, Science Citation Index; RCT, randomized controlled trial.
Two institutions published two similar articles (40,41), in Italy. This triggered a concern about duplication of data; however, following a careful review of the articles in question, it was decided that the two articles were separate trials.
Efficacy of H. pylori eradication
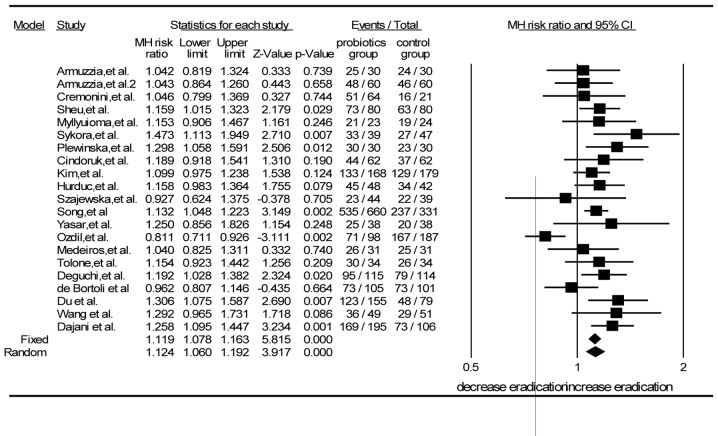
The 21 RCTs included 3,814 patients in total, of whom 21 patients were in the probiotic group and 1,529 in the control group. The pooled eradication rate of the probiotic group was 80.3% (1,709/2,128) by intention-to-treat (ITT) and 83.8% (1,709/2,039) by PP analysis; the eradication rate in the probiotic group was higher than that in the control group (80.3 vs. 72.2%) with a statistically significant difference (Z=3.917, P<0.001). Using the random-effects model, the values of I2=52.3% and P=0.003 were obtained. The RR from a pooled analysis of the selected studies was 1.12 (95% CI, 1.06–1.19) by ITT analysis (Fig. 2).
Figure 2.
Forest plot comparing the eradication rate of supplementation by intention-to-treat analysis. CI, confidence interval; RR, relative risk; MH, Mantel-Haenszel.
Subgroup analyses
Multiple subgroup analyses were carried out to explain the heterogeneity by stratifying the studies based on the timing of probiotic supplementation (‘before’, ‘same’ and ‘after’), eradication regimens, duration of probiotic supplementation, species of probiotics, age of patients (adults and children) and Jadad scores.
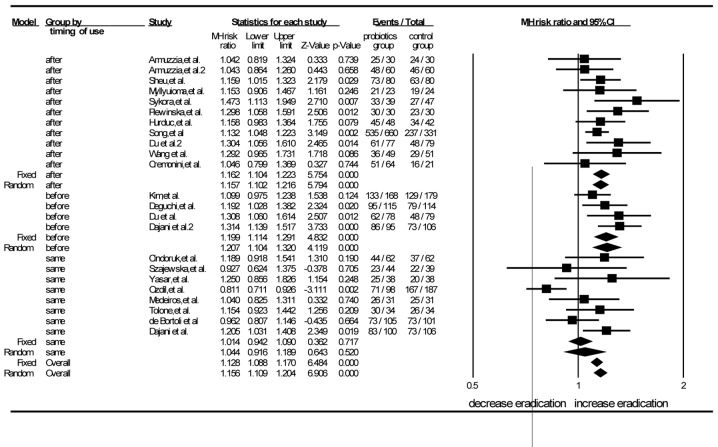
There were 11 trials in which the probiotics were administered subsequent to the eradication regimens (38,40–46,50,52,56). The pooled analysis showed that the RR was 1.15 (95% CI, 1.10–1.21) according to the random-effects model. The RR of the eight studies in which probiotics were used simultaneously with the eradication regimens was 1.04 (95% CI, 0.92–1.19) by the random-effects mode (11,51,39,47,48,53,54,57). The RR for the probiotics used prior to the eradication regimens in the four RCTs was 1.21 (95% CI, 1.10–1.32) by the random-effects model (39,49,55,56). When the probiotics were administered prior or subsequent to the standard triple therapy, the differences between the experimental and control groups were statistically significant. When probiotics were used concurrently with the eradication regimens, no significant difference was found between the experimental group and the control group. This demonstrated that the timing of probiotic supplementation, i.e. prior or subsequent to the standard triple-therapy regimen, could improve the eradication rate (Fig. 3).
Figure 3.
Forest plot of eradication rates grouped according to the timing of probiotic administration by intention-to-treat analysis. ‘Before’, probiotics were used prior to the eradication regimen and ended simultaneously the with regimen; ‘same’: probiotics were used and ended simultaneously with the eradication regimen; ‘after’, probiotics were used simultaneously with the eradication regimen and usage continued subsequent to the end of the regimen; CI, confidence interval; MH, Mantel-Haenszel.
Subgroup analyses were additionally performed according to the eradication regimens (PPI plus amoxicillin and clarithromycin, PPI plus clarithromycin and tinidazole). The RRs analyzed in the random-effects model were 1.14 (95% CI, 1.07–1.21) and 1.04 (95% CI, 0.92–1.19) for the two regimens, respectively. The combination of the standard triple-therapy regimen (PPI, amoxicillin and clarithromycin) with probiotics achieved a significantly higher eradication rate than that obtained without probiotics; however, the combination of the PPI plus clarithromycin and tinidazole triple therapy with probiotics did not significantly improve the eradication rate for H. pylori.
According to the subgroup analyses of the duration of probiotic supplementation, the RR for durations of ≤2 weeks was 1.04 (95% CI, 0.98–1.11) by random-effects model, and the RR for durations of ≤2 weeks was 1.17 (95% CI, 1.12–1.23) by random-effects model. The results showed that probiotic supplementation for >2 weeks could improve the eradication of H. pylori.
According to subgroup analyses of species, the RR for Lactobacillus was 1.14 (95% CI, 1.08–1.25), the RR of Saccharomyces boulardii was 1.06 (95% CI, 0.89–1.23) and that of Bifidobacterium was 1.25 (95% CI, 0.86–1.82) (all by random-effects model). The RR in the multiple strains subgroup was 1.15 (95% CI, 1.08–1.22). The findings demonstrated that the use of Lactobacillus and multiple probiotic strains as adjuvant agents could improve the effectiveness of the H. pylori eradication to a greater extent than the control treatment; however, the administration of Bifidobacterium or Saccharomyces boulardii did not appear to improve eradication during anti-H. pylori treatment.
In the adult and children subgroup analyses, the RRs were 1.08 (95% CI, 1.01–1.16) and 1.22 (95% CI, 1.11–1.34), respectively, by the random-effects model. The results showed the enhanced efficacy of probiotic supplementation relative to that of the control treatment (P<0.001) in both adults and children.
There were 11 trials in which the Jadad scores were ≥3, indicating that their quality was high (40–42,44,45,48–52,56). The Jadad scores were <3 in 10 studies, which indicated that their quality was low (11,30,38,39,42,44–53, 56,57). According to the pooled analysis of the high-quality trials, the summary RR was 1.13 (95% CI, 1.08–1.19) by random-effects model. The RR of the studies of low quality was 1.12 (95% CI, 1.00–1.25) by random-effects model. The high-quality studies all showed the benefit of probiotic supplementation compared with the control treatment (P<0.001), but no significant difference was found between the treatments in the low-quality studies (P=0.053).
Subgroup analyses were also performed based on the different PPIs of the trial groups and the duration of the eradication regimens. In the omeprazole and rabeprazole subgroups, the differences between the probiotic and control groups were statistically significant (P<0.001 and P=0.034, respectively). Significant differences were also found for eradication durations of seven and 10 days (P<0.001 and P=0.012, respectively).
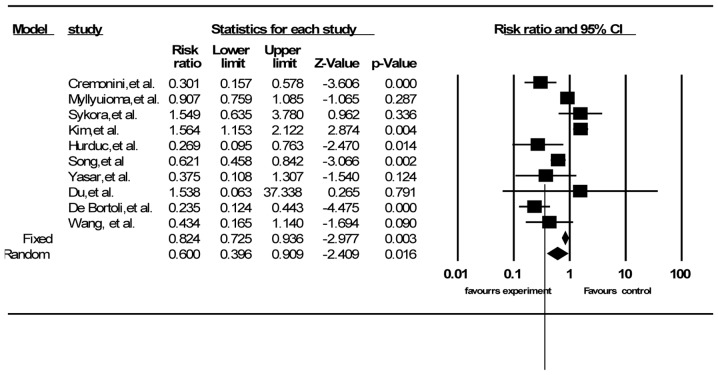
Adverse events
A total of 16 out of the 21 trials described side effects, including diarrhea, vomiting and nausea, and epigastric pain (30,38,39,42,44–53,56,57). Ten RCTs had data on total side effects (38,42,44,45,47,49,50,52,53,56). The summary RR was 0.60 (95% CI, 0.40–0.91) according to random-effects model analysis (I2=83.72%, P<0.001) (Fig. 4). Twelve RCTs reported the data for diarrhea (30,38,39,42,44,46–49,51,52,57), 10 for vomiting and nausea (30,38,42,44,46–49,52,57) and eight for epigastric pain (42,44,46–49,52,57). The pooled RRs were 0.42 for diarrhea (95% CI, 0.24–0.73) and 0.56 for vomiting and nausea (95% CI, 0.27–1.16) by random-effects model (I2=61.75%, P=0.002 and I2=60.05%, P=0.007, respectively), and 0.58 for epigastric pain (95% CI, 0.34–0.97) by the fixed-effects model (I2=34.00%, P=0.157). The majority of the studies did not provide details on how they estimated the severity of adverse events.
Figure 4.
Effect of probiotic supplementation versus control treatment without probiotics on the incidence of total side effects. CI, confidence interval.
Risk of bias in publication
Funnel plot analyses by ITT analysis revealed slight asymmetry, but Egger’s test and Begg’s test showed no significant asymmetry of the funnel plot (Fig. 5).
Figure 5.
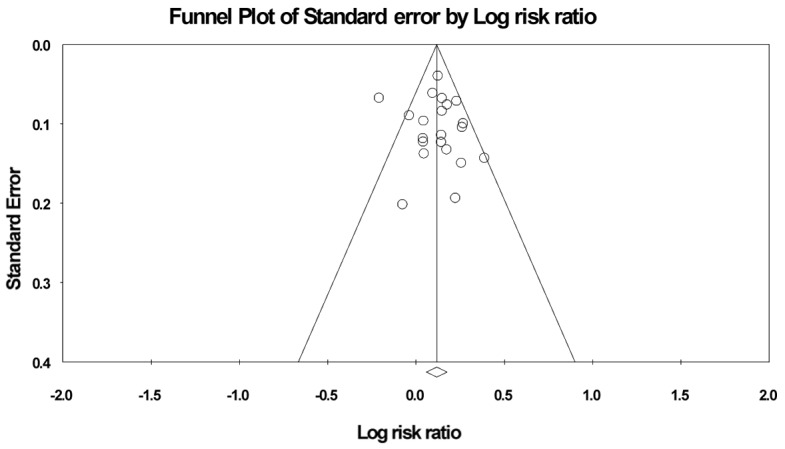
Funnel plot of included studies for eradication rates.
Sensitivity analysis
A sensitivity analysis was performed to interpret the reliability of the outcomes of the meta-analysis. Based on ITT analysis, the pooled RR values were established though the fixed- and random-effects models. The RRs were 1.12 (95% CI, 1.08–1.16) and 1.12 (95% CI, 1.06–1.19), respectively. No significant difference was found (overlapping CIs). When the largest study (52) was excluded from the sensitivity analysis, the RR did not change significantly (RR=1.12). The RRs were therefore steady.
Heterogeneity
To interpret heterogeneity in the meta-analysis, a meta-regression analysis was performed. The results showed that the timing and duration of probiotic supplementation, the duration of the eradication regimen and the quality of study were the main causes of heterogeneity.
Discussion
Probiotics, according to the World Health Organization, are defined as ‘live microorganisms, which, when administered in adequate amounts, confer a health benefit on the host’. They consist of bacteria and yeasts. It has been recognized that probiotics can exhibit an inhibitory ability against H. pylori (5). The effects of probiotics on H. pylori may be due to immunologic as well as non-immunologic mechanisms: i) Competition at the site of the stomach mucosal epithelium (6); ii) production of substances against H. pylori, such as acetic, propionic or butyric acid (58); iii) regulation of immune function and secretion of immunoglobulin A to improve mucosal defensive ability (59–61); and iv) strengthening tight junctions between epithelial cells (61,62).
The current results showed that probiotics could improve the eradication rate and decrease adverse events during anti-H. pylori treatment. The RRs were 1.12 (95% CI, 1.06–1.19) and 0.62 (95% CI, 0.40–0.91), respectively. The outcomes of the present meta-analysis were similar with several previous meta-analyses (15,17,18).
The optimal timing of probiotic administration is still unknown (23,24). It is generally believed that better efficacy occurs when probiotic supplementation occurs concurrently with or subsequent to antibiotic regimens. When probiotics are administered prior to antibiotic regimens, H. pylori is converted from a spiral to a coccoid form, which can lead to eradication failure. The timing of the addition of probiotics has been different in clinical trials (38,56,57). Whether the variability affected the eradication rate of H. pylori is not clear. The results of the current meta-analysis suggested that probiotic supplementation could improve eradication rates when provided prior or subsequent to the standard treatment regimens, but that supplementation supplied concurrently with the regimen did not significantly improve the eradication rate. The reason behind this may be that, when probiotics and antibiotics are administered simultaneously, it is inevitable that the antibiotics restrain the growth of the probiotics, resulting in a decrease in the anti-H. pylori substances produced by the probiotics (23,24).
An additional undetermined factor in studies to date is the appropriate duration of probiotic administration (23,24). In the present meta-analysis, the duration of probiotic administration varied from 7 days to months (38,45,47,51). The results suggested that a duration of >2 weeks could significantly improve the eradication rate for H. pylori infection, while a duration of ≤2 weeks could not. This indicated that the long-term administration of probiotics could be beneficial during anti-H. pylori treatment; however, further investigation is required to confirm this.
Based on the subgroup analyses of probiotic species employed, it was shown that the regimens with Lactobacillus were superior to the control group regimens (RR, 1.15; 95% CI, 1.05–1.25); however, only two RCTs used Bifidobacterium alone for adjuvant therapy during anti-H. pylori treatment. The effectiveness was slightly better than that of the control group regimens, but the difference was not statistically significant. Further investigation is therefore required to draw a definite conclusion. The use of Saccharomyces boulardii as a single supplement did not improve the eradication rate during anti-H. pylori treatment (RR, 1.05; 95% CI, 0.89–1.23). This suggests that the administration of Saccharomyces boulardii alone may not be suitable for adjuvant treatment during anti-H. pylori therapy (11,42,48,50,52).
Subgroup analyses were also performed according to different PPIs and durations of eradication regimens. It was of note that the omeprazole and rabeprazole subgroups achieved significant eradication success, while the esomeprazole, lansoprazole and pantoprazole subgroups did not, as compared with the control group. The current meta-analysis also demonstrated that the triple-therapy regimens with PPIs, amoxicillin and clarithromycin could achieve significantly higher eradication rates than the control group regimens, but the triple-therapy regimens consisting of PPIs, clarithromycin and nitroimidazole could not.
A number of studies have indicated that the administration of probiotics can ameliorate the symptoms and reduce the adverse effects associated with eradication therapy for H. pylori, such as diarrhea, vomiting, nausea and epigastric pain (14,35,47); however, certain investigations have suggested that probiotic supplementation does not reduce the incidence of side effects (21,49). The side effects experienced during anti-H. pylori regimens were therefore examined in the current meta-analysis, which showed that the supplementation of probiotics had a substantial effect on reducing H. pylori therapy-related adverse reactions, particularly diarrhea and epigastric pain. The results were consistent with those of previous meta-analyses (15,17,18). We believe that the application of probiotics has a beneficial effect and diminishes the discomfort during anti-H. pylori therapy.
To decrease bias in the present meta-analysis, the study selection, data extraction and assessment of study quality were performed by two reviewers. Another strength of the current meta-analysis was that it identified the majority of the RCTs published in English that used different species of probiotics as adjuvant agents for H. pylori treatment. The efficacy and safety of probiotics in anti-H. pylori treatment were comprehensively analyzed. The meta-regression analysis made the outcomes of the present meta-analysis reliable.
There were several limitations to the meta-analysis. Firstly, some evident heterogeneity was noted in the meta-analysis, although sub-analysis and meta-regression analysis were conducted to decrease the effects. Secondly, the language restriction could have influenced the results. There could have been a bias in the published languages, so it is likely that the present meta-analysis does not reflect all the outcomes of probiotics used for anti-H. pylori treatment. Finally, certain authors were asked for unpublished data, so the introduction of bias on that basis is possible. The Egger’s and Begg’s tests suggested that there could have been publication biases, and these could have affected the results of the meta-analysis.
In conclusion, the present meta-analysis showed that probiotic supplementation can improve eradication rates and reduce the adverse effects experienced during eradication therapy. In addition, probiotics appear to have enhanced effects on eradication rates when administered prior or subsequent to the standard regimens. Long-term probiotic treatment may have a superior effect to short-term probiotic administration. Lactobacillus and probiotic supplementation with multiple species appear to improve the eradication rate for H. pylori infection.
Acknowledgements
This study was supported by a grant from the National Science and Technology Major Projects for ‘Major New Drug Innovation and Development’ of China (no. 2011ZX09302-007-03). The original manuscript was edited and proofread by Medjaden Bioscience Limited. The abstract of the present study has previously been published in the proceedings for the XXVIIth International Workshop on Helicobacter and Microbiota in Chronic Digestive Inflammation and Gastric Cancer (11–13 September 2014), and in the Journal of Gastroenterology and Hepatology (vol 29, supplement S3, 2014).
References
- 1.Go MF. Review article: natural history and epidemiology of Helicobacter pylori infection. Aliment Pharmacol Ther. 2002;16(Suppl 1):3–15. doi: 10.1046/j.1365-2036.2002.0160s1003.x. [DOI] [PubMed] [Google Scholar]
- 2.Chey WD, Wong BC Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808–1825. doi: 10.1111/j.1572-0241.2007.01393.x. [DOI] [PubMed] [Google Scholar]
- 3.Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection - the Maastricht IV/Florence consensus report. Gut. 2012;61:646–664. doi: 10.1136/gutjnl-2012-302084. [DOI] [PubMed] [Google Scholar]
- 4.Bell GD, Powell K, Burridge SM, et al. Experience with ‘triple’ anti-Helicobacter pylori eradication therapy: side effects and the importance of testing the pre-treatment bacterial isolate for metronidazole resistance. Aliment Pharmacol Ther. 1992;6:427–435. doi: 10.1111/j.1365-2036.1992.tb00556.x. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia SJ, Kochar N, Abraham P, Nair NG, Mehta AP. Lactobacillus acidophilus inhibits growth of Campylobacter pylori in vitro. J Clin Microbiol. 1989;27:2328–2330. doi: 10.1128/jcm.27.10.2328-2330.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mukai T, Asasaka T, Sato E, et al. Inhibition of binding of Helicobacter pylori to the glycolipid receptors by probiotic Lactobacillus reuteri. FEMS Immunol Med Microbiol. 2002;32:105–110. doi: 10.1111/j.1574-695X.2002.tb00541.x. [DOI] [PubMed] [Google Scholar]
- 7.Johnson-Henry KC, Mitchell DJ, Avitzur Y, et al. Probiotics reduce bacterial colonization and gastric inflammation in H. pylori-infected mice. Dig Dis Sci. 2004;49:1095–1102. doi: 10.1023/B:DDAS.0000037794.02040.c2. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh PS, Tsai YC, Chen YC, et al. Eradication of Helicobacter pylori infection by the probiotic strains Lactobacillus johnsonii MH-68 and L. salivarius ssp salicinius AP-32. Helicobacter. 2012;17:466–477. doi: 10.1111/j.1523-5378.2012.00992.x. [DOI] [PubMed] [Google Scholar]
- 9.Tursi A, Brandimarte G, Giorgetti GM, Modeo ME. Effect of Lactobacillus casei supplementation on the effectiveness and tolerability of a new second-line 10-day quadruple therapy after failure of a first attempt to cure Helicobacter pylori infection. Med Sci Monit. 2004;10:CR662–CR666. [PubMed] [Google Scholar]
- 10.Lionetti E, Indrio F, Pavone L, et al. Role of probiotics in pediatric patients with Helicobacter pylori infection: a comprehensive review of the literature. Helicobacter. 2010;15:79–87. doi: 10.1111/j.1523-5378.2009.00743.x. [DOI] [PubMed] [Google Scholar]
- 11.Ozdil K, Calhan T, Sahin A, et al. Levofloxacin based sequential and triple therapy compared with standard plus probiotic combination for Helicobacter pylori eradication. Hepatogastroenterology. 2011;58:1148–1152. doi: 10.5754/hge11075. [DOI] [PubMed] [Google Scholar]
- 12.Yoon H, Kim N, Kim JY, et al. Effects of multistrain probiotic-containing yogurt on second-line triple therapy for Helicobacter pylori infection. J Gastroenterol Hepatol. 2011;26:44–48. doi: 10.1111/j.1440-1746.2010.06477.x. [DOI] [PubMed] [Google Scholar]
- 13.Scaccianoce G, Zullo A, Hassan C, et al. Triple therapies plus different probiotics for Helicobacter pylori eradication. Eur Rev Med Pharmacol Sci. 2008;12:251–256. [PubMed] [Google Scholar]
- 14.Ahmad K, Fatemeh F, Mehri N, Maryam S. Probiotics for the treatment of pediatric Helicobacter pylori infection: a randomized double blind clinical trial. Iran J Pediatr. 2013;23:79–84. [PMC free article] [PubMed] [Google Scholar]
- 15.Tong JL, Ran ZH, Shen J, Zhang CX, Xiao SD. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther. 2007;25:155–168. doi: 10.1111/j.1365-2036.2006.03179.x. [DOI] [PubMed] [Google Scholar]
- 16.Szajewska H, Horvath A, Piwowarczyk A. Meta-analysis: the effects of Saccharomyces boulardii supplementation on Helicobacter pylori eradication rates and side effects during treatment. Aliment Pharmacol Ther. 2010;32:1069–1079. doi: 10.1111/j.1365-2036.2010.04457.x. [DOI] [PubMed] [Google Scholar]
- 17.Zou J, Dong J, Yu X. Meta-analysis: Lactobacillus containing quadruple therapy versus standard triple first-line therapy for Helicobacter pylori eradication. Helicobacter. 2009;14:97–107. doi: 10.1111/j.1523-5378.2009.00716.x. [DOI] [PubMed] [Google Scholar]
- 18.Wang ZH, Gao QY, Fang JY. Meta-analysis of the efficacy and safety of Lactobacillus-containing and Bifidobacterium-containing probiotic compound preparation in Helicobacter pylori eradication therapy. J Clin Gastroenterol. 2013;47:25–32. doi: 10.1097/MCG.0b013e318266f6cf. [DOI] [PubMed] [Google Scholar]
- 19.Sachdeva A, Nagpal J. Effect of fermented milk-based probiotic preparations on Helicobacter pylori eradication: a systematic review and meta-analysis of randomized-controlled trials. Eur J Gastroenterol Hepatol. 2009;21:45–53. doi: 10.1097/MEG.0b013e32830d0eff. [DOI] [PubMed] [Google Scholar]
- 20.Zheng X, Lyu L, Mei Z. Lactobacillus-containing probiotic supplementation increases Helicobacter pylori eradication rate: evidence from a meta-analysis. Rev Esp Enferm Dig. 2013;105:445–453. doi: 10.4321/S1130-01082013000800002. [DOI] [PubMed] [Google Scholar]
- 21.Shavakhi A, Tabesh E, Yaghoutkar A, et al. The effects of multistrain probiotic compound on bismuth-containing quadruple therapy for Helicobacter pylori infection: a randomized placebo-controlled triple-blind study. Helicobacter. 2013;18:280–284. doi: 10.1111/hel.12047. [DOI] [PubMed] [Google Scholar]
- 22.Navarro-Rodriguez T, Silva FM, Barbuti RC, et al. Association of a probiotic to a Helicobacter pylori eradication regimen does not increase efficacy or decreases the adverse effects of the treatment: a prospective, randomized, double-blind, placebo-controlled study. BMC Gastroenterol. 2013;13:56. doi: 10.1186/1471-230X-13-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsushima M, Takagi A. ‘Is it effective?’ to ‘How to use it?’: the era has changed in probiotics and functional food products against Helicobacter pylori infection. J Gastroenterol Hepatol. 2012;27:851–853. doi: 10.1111/j.1440-1746.2012.07094.x. [DOI] [PubMed] [Google Scholar]
- 24.Boyanova L, Mitov I. Coadministration of probiotics with antibiotics: why, when and for how long? Expert Rev Anti Infect Ther. 2012;10:407–409. doi: 10.1586/eri.12.24. [DOI] [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 27.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sahagún-Flores JE, López-Peña LS, de la Cruz-Ramírez Jaimes J, et al. Eradication of Helicobacter pylori: triple treatment scheme plus Lactobacillus vs. triple treatment alone. Cir Cir. 2007;75:333–336. (In Spanish) [PubMed] [Google Scholar]
- 29.Ziemniak W. Efficacy of Helicobacter pylori eradication taking into account its resistance to antibiotics. J Physiol Pharmacol. 2006;57(Suppl 3):123–141. [PubMed] [Google Scholar]
- 30.Sheu BS, Cheng HC, Kao AW, et al. Pretreatment with Lactobacillus- and Bifidobacterium-containing yogurt can improve the efficacy of quadruple therapy in eradicating residual Helicobacter pylori infection after failed triple therapy. Am J Clin Nutr. 2006;83:864–869. doi: 10.1093/ajcn/83.4.864. [DOI] [PubMed] [Google Scholar]
- 31.Lionetti E, Miniello VL, Castellaneta SP, et al. Lactobacillus reuteri therapy to reduce side-effects during anti-Helicobacter pylori treatment in children: a randomized placebo controlled trial. Aliment Pharmacol Ther. 2006;24:1461–1468. doi: 10.1111/j.1365-2036.2006.03145.x. [DOI] [PubMed] [Google Scholar]
- 32.Manfredi M, Bizzarri B, Sacchero RI, et al. Helicobacter pylori infection in clinical practice: probiotics and a combination of probiotics + lactoferrin improve compliance, but not eradication, in sequential therapy. Helicobacter. 2012;17:254–263. doi: 10.1111/j.1523-5378.2012.00944.x. [DOI] [PubMed] [Google Scholar]
- 33.Xu C, Xiao L, Zou H. Effect of birid triple viable on peptic ulcer patients with Helicobacter pylori infection. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2010;35:1000–1004. doi: 10.3969/j.issn.1672-7347.2010.09.017. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 34.Park SK, Park DI, Choi JS, et al. The effect of probiotics on Helicobacter pylori eradication. Hepatogastroenterology. 2007;54:2032–2036. [PubMed] [Google Scholar]
- 35.Bekar O, Yilmaz Y, Gulten M. Kefir improves the efficacy and tolerability of triple therapy in eradicating Helicobacter pylori. J Med Food. 2011;14:344–347. doi: 10.1089/jmf.2010.0099. [DOI] [PubMed] [Google Scholar]
- 36.Nista EC, Candelli M, Cremonini F, et al. Bacillus clausii therapy to reduce side-effects of anti-Helicobacter pylori treatment: randomized, double-blind, placebo controlled trial. Aliment Pharmacol Ther. 2004;20:1181–1188. doi: 10.1111/j.1365-2036.2004.02274.x. [DOI] [PubMed] [Google Scholar]
- 37.Canducci F, Armuzzi A, Cremonini F, et al. A lyophilized and inactivated culture of Lactobacillus acidophilus increases Helicobacter pylori eradication rates. Aliment Pharmacol Ther. 2000;14:1625–1629. doi: 10.1046/j.1365-2036.2000.00885.x. [DOI] [PubMed] [Google Scholar]
- 38.Wang YH, Huang Y. Effect of Lactobacillus acidophilus and Bifidobacterium bifidum supplementation to standard triple therapy on Helicobacter pylori eradication and dynamic changes in intestinal flora. World J Microbiol Biotechnol. 2014;30:847–853. doi: 10.1007/s11274-013-1490-2. [DOI] [PubMed] [Google Scholar]
- 39.Dajani AI, Abu Hammour AM, Yang DH, et al. Do probiotics improve eradication response to Helicobacter pylori on standard triple or sequential therapy? Saudi J Gastroenterol. 2013;19:113–120. doi: 10.4103/1319-3767.111953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Armuzzi A, Cremonini F, Bartolozzi F, et al. The effect of oral administration of Lactobacillus GG on antibiotic-associated gastrointestinal side-effects during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther. 2001;15:163–169. doi: 10.1046/j.1365-2036.2001.00923.x. [DOI] [PubMed] [Google Scholar]
- 41.Armuzzi A, Cremonini F, Ojetti V, et al. Effect of Lactobacillus GG supplementation on antibiotic-associated gastrointestinal side effects during Helicobacter pylori eradication therapy: a pilot study. Digestion. 2001;63:1–7. doi: 10.1159/000051865. [DOI] [PubMed] [Google Scholar]
- 42.Cremonini F, Di Caro S, Covino M, et al. Effect of different probiotic preparations on anti-Helicobacter pylori therapy-related side effects: a parallel group, triple blind, placebo-controlled study. Am J Gastroenterol. 2002;97:2744–2749. doi: 10.1111/j.1572-0241.2002.07063.x. [DOI] [PubMed] [Google Scholar]
- 43.Sheu BS, Wu JJ, Lo CY, et al. Impact of supplement with Lactobacillus- and Bifidobacterium-containing yogurt on triple therapy for Helicobacter pylori eradication. Aliment Pharmacol Ther. 2002;16:1669–1675. doi: 10.1046/j.1365-2036.2002.01335.x. [DOI] [PubMed] [Google Scholar]
- 44.Myllyluoma E, Veijola L, Ahlroos T, et al. Probiotic supplementation improves tolerance to Helicobacter pylori eradication therapy - a placebo-controlled, double-blind randomized pilot study. Aliment Pharmacol Ther. 2005;21:1263–1272. doi: 10.1111/j.1365-2036.2005.02448.x. [DOI] [PubMed] [Google Scholar]
- 45.Sýkora J, Valecková K, Amlerová J, et al. Effects of a specially designed fermented milk product containing probiotic Lactobacillus casei DN-114 001 and the eradication of H. pylori in children: a prospective randomized double-blind study. J Clin Gastroenterol. 2005;39:692–698. doi: 10.1097/01.mcg.0000173855.77191.44. [DOI] [PubMed] [Google Scholar]
- 46.Plewińska EM, Płaneta-Małecka I, Bąk-Romaniszyn L, Czkwianianc E, Małecka-Panas E. Probiotics in the treatment of Helicobacter pylori infection in children. Gastroenterologia Polska. 2006;13:315–319. [Google Scholar]
- 47.de Bortoli N, Leonardi G, Ciancia E, et al. Helicobacter pylori eradication: a randomized prospective study of triple therapy versus triple therapy plus lactoferrin and probiotics. Am J Gastroenterol. 2007;102:951–956. doi: 10.1111/j.1572-0241.2007.01085.x. [DOI] [PubMed] [Google Scholar]
- 48.Cindoruk M, Erkan G, Karakan T, Dursun A, Unal S. Efficacy and safety of Saccharomyces boulardii in the 14-day triple anti-Helicobacter pylori therapy: a prospective randomized placebo-controlled double-blind study. Helicobacter. 2007;12:309–316. doi: 10.1111/j.1523-5378.2007.00516.x. [DOI] [PubMed] [Google Scholar]
- 49.Kim MN, Kim N, Lee SH, et al. The effects of probiotics on PPI-triple therapy for Helicobacter pylori eradication. Helicobacter. 2008;13:261–268. doi: 10.1111/j.1523-5378.2008.00601.x. [DOI] [PubMed] [Google Scholar]
- 50.Hurduc V, Plesca D, Dragomir D, Sajin M, Vandenplas Y. A randomized, open trial evaluating the effect of Saccharomyces boulardii on the eradication rate of Helicobacter pylori infection in children. Acta Paediatr. 2009;98:127–131. doi: 10.1111/j.1651-2227.2008.00977.x. [DOI] [PubMed] [Google Scholar]
- 51.Szajewska H, Albrecht P, Topczewska-Cabanek A. Randomized, double-blind, placebo-controlled trial: effect of Lactobacillus GG supplementation on Helicobacter pylori eradication rates and side effects during treatment in children. J Pediatr Gastroenterol Nutr. 2009;48:431–436. doi: 10.1097/MPG.0b013e318182e716. [DOI] [PubMed] [Google Scholar]
- 52.Song MJ, Park DI, Park JH, et al. The effect of probiotics and mucoprotective agents on PPI-based triple therapy for eradication of Helicobacter pylori. Helicobacter. 2010;15:206–213. doi: 10.1111/j.1523-5378.2010.00751.x. [DOI] [PubMed] [Google Scholar]
- 53.Yaşar B, Abut E, Kayadıbı H, et al. Efficacy of probiotics in Helicobacter pylori eradication therapy. Turk J Gastroenterol. 2010;21:212–217. doi: 10.4318/tjg.2010.0090. [DOI] [PubMed] [Google Scholar]
- 54.Medeiros JA, Gonçalves TM, Boyanova L, et al. Evaluation of Helicobacter pylori eradication by triple therapy plus Lactobacillus acidophilus compared to triple therapy alone. Eur J Clin Microbiol Infect Dis. 2011;30:555–559. doi: 10.1007/s10096-010-1119-4. [DOI] [PubMed] [Google Scholar]
- 55.Deguchi R, Nakaminami H, Rimbara E, et al. Effect of pretreatment with Lactobacillus gasseri OLL2716 on first-line Helicobacter pylori eradication therapy. J Gastroenterol Hepatol. 2012;27:888–892. doi: 10.1111/j.1440-1746.2011.06985.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Du YQ, Su T, Fan JG, et al. Adjuvant probiotics improve the eradication effect of triple therapy for Helicobacter pylori infection. World J Gastroenterol. 2012;18:6302–6307. doi: 10.3748/wjg.v18.i43.6302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tolone S, Pellino V, Vitaliti G, Lanzafame A, Tolone C. Evaluation of Helicobacter pylori eradication in pediatric patients by triple therapy plus lactoferrin and probiotics compared to triple therapy alone. Ital J Pediatr. 2012;38:63. doi: 10.1186/1824-7288-38-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gotteland M, Brunser O, Cruchet S. Systematic review: are probiotics useful in controlling gastric colonization by Helicobacter pylori? Aliment Pharmacol Ther. 2006;23:1077–1086. doi: 10.1111/j.1365-2036.2006.02868.x. [DOI] [PubMed] [Google Scholar]
- 59.Yang YJ, Sheu BS. Probiotics-containing yogurts suppress Helicobacter pylori load and modify immune response and intestinal microbiota in the Helicobacter pylori-infected children. Helicobacter. 2012;17:297–304. doi: 10.1111/j.1523-5378.2012.00941.x. [DOI] [PubMed] [Google Scholar]
- 60.Kwon HK, Kim GC, Kim Y, et al. Amelioration of experimental autoimmune encephalomyelitis by probiotic mixture is mediated by a shift in T helper cell immune response. Clin Immunol. 2013;146:217–227. doi: 10.1016/j.clim.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 61.Sultana R, McBain AJ, O’Neill CA. Strain-dependent augmentation of tight-junction barrier function in human primary epidermal keratinocytes by Lactobacillus and Bifidobacterium lysates. Appl Environ Microbiol. 2013;79:4887–4894. doi: 10.1128/AEM.00982-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yeung CY, Chiang Chiau JS, Chan WT, et al. In vitro prevention of Salmonella lipopolysaccharide-induced damages in epithelial barrier function by various Lactobacillus strains. Gastroenterol Res Pract. 2013;2013:973209. doi: 10.1155/2013/973209. [DOI] [PMC free article] [PubMed] [Google Scholar]