Abstract
Originally described in the 1970s, vascularized bone grafting has become a critical component in the treatment of bony defects and non-unions. Although well established in the lower extremity, recent years have seen many novel techniques described to treat a variety of challenging upper extremity pathologies. Here the authors review the use of different techniques of vascularized bone grafts for the upper extremity bone pathologies. The vascularized fibula remains the gold standard for the treatment of large bone defects of the humerus and forearm, while also playing a role in carpal reconstruction; however, two other important options for larger defects include the vascularized scapula graft and the Capanna technique. Smaller upper extremity bone defects and non-unions can be treated with the medial femoral condyle (MFC) free flap or a vascularized rib transfer. In carpal non-unions, both pedicled distal radius flaps and free MFC flaps are viable options. Finally, in skeletally immature patients, vascularized fibular head epiphyseal transfer can provide growth potential in addition to skeletal reconstruction.
Keywords: vascularized bone graft, vascularized fibula, medial femoral condylar flap, bone graft, vascularized epiphyseal transfer
Historically, vascularized bone grafting is reserved for segmental bone loss > 5 to 6 cm associated with a poorly vascularized local soft tissue environment.1 2 3 4 5 6 7 8 In the lower extremity, this is typically seen following open fractures, oncological resection, and during the treatment of osteomyelitis or non-unions.1 2 3 4 5 6 7 8 These same situations are encountered in the upper extremity; however, there is also a need to treat much smaller defects, such as cases of avascular necrosis or recalcitrant non-union of the carpal bones or metacarpals. In recent years, many vascularized strategies have been developed to treat small bony defects recalcitrant to nonvascularized autograft or allograft. Newer options such as the free medial femoral condyle graft and pedicled distal radius grafts can be used to treat carpal bone avascular necrosis and carpal non-unions, whereas vascularized epiphyseal transfer can be used to restore forearm growth in pediatric patients.9 10 11 12 13 14 15
For bone defects < 6 cm, nonvascularized grafts have been demonstrated to be successful, providing that the graft is covered by well-vascularized tissue and the wound is free of infection.16 Nonvascularized bone grafts are incorporated into defects through the process of creeping substitution and vascular ingrowth. By contrast, vascularized bone grafts allow for the maintenance of bones microenvironment, allowing for primary bony healing into the recipient site, instead of depending on the remodeling process of the recipient bone (which may be compromised due to radiation, infection, or avascular necrosis).3 17 18 Vascularized bone grafts have been shown to provide more rapid healing, reduce the risk of subsequent fracture, and have the ability to remodel under physiologic load allowing for early weight bearing.8 19 Our purpose here is to review the use of vascularized bone grafts for upper extremity reconstruction.
Vascularized Fibula
The free vascularized fibulas has been the gold standard of long bone reconstruction because its inception in 1975.5 Numerous reports have demonstrated the success of these grafts, with union rates up to 80% on first time grafting, and up to 97% following supplemental grafting.7 8 20 21 22 In adults, it can provide up to 25 cm of straight, cortical bone along with a reliable vascular pedicle with low donor site morbidity.20 23 In upper extremity, the tubular shape of the bones and easy access to recipient vessels renders it one of the most promising locations for free fibular transfer.24
The fibula's size and shape is very similar to the diaphysis of radius and ulna, making it an ideal donor for reconstruction of significant forearm bone loss.25 These similarities often enable vascularized fibula reconstruction to produce a stable forearm and wrist. Furthermore, the rapid maturation of the graft enables early load bearing and resumption of activities.25 Forearm free fibula reconstruction has achieved excellent results by most reports, with 85 to 89% of patients attaining union of the graft.8 22 26 27 In a large series by Han and colleagues, there was a 15% rate of non-union; however, none of the grafts developed a symptomatic non-union, yielding limb salvage in all patients with forearm reconstruction.8 The most common bony complication following free fibular transfer to the forearm is stress fractures, seen in up to 17% of patients.8 22 28
Humeral diaphyseal bone defects are also often treated with a vascularized free fibula graft, enabling the restoration of a functional shoulder and elbow. However, the success rate is not as predictable as the forearm, with late fracture rates of up to 40%.8 21 24 28 29 30 31 32 The high rate of fracture is thought to be due to a combination of failed bony union, size mismatch, osteosynthesis, and the local soft tissue environment.29 31 33 Rashid and colleagues noted a graft fracture rate of only 8% and union rate of 95%, attributing this to the use of rigid compression plating and augmentation with the use of an additional flap for soft tissue coverage.31 Interestingly, in the cases of graft fracture it was noted that none of the patients had any additional soft tissue coverage.29 This highlights the role of a well-vascularized local soft tissue environment in treating large bone defects (Fig. 1).
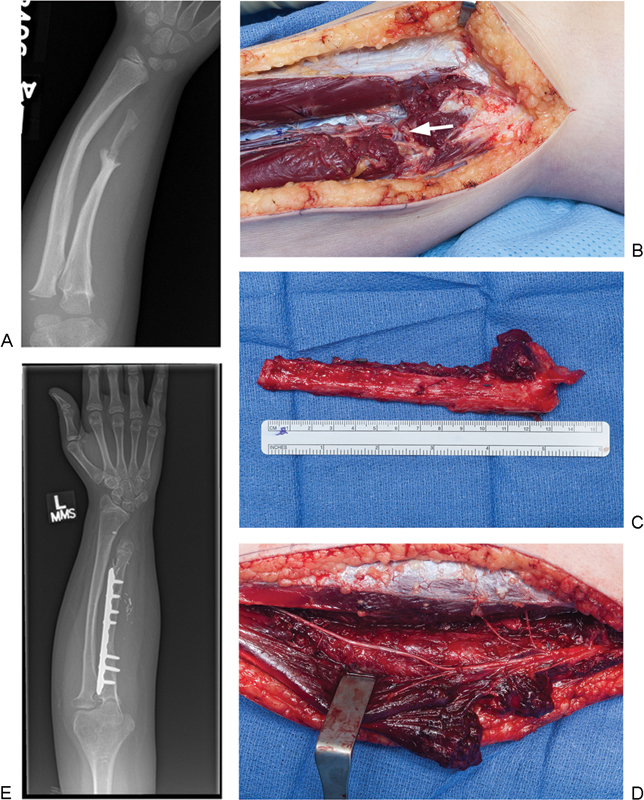
Fig. 1.
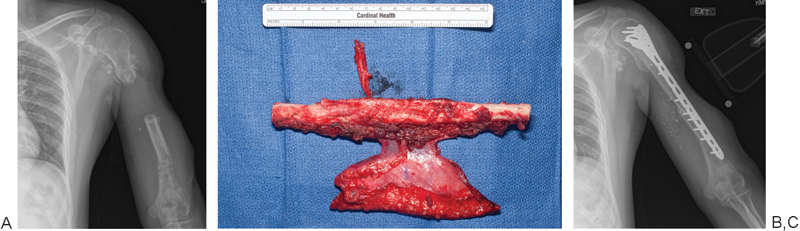
A 26-year-old soldier involved in a land mine accident with segmental humeral loss. (A) Anteroposterior (AP) radiograph of arm showing segmental bone loss in humerus. (B) A vascularized fibula with skin paddle was used as an intercalary graft to reconstruct the humerus. (C) Final AP radiograph showing solid incorporation of the fibular graft.
Glenohumeral arthrodesis can be supplemented by the use of a free fibula, particularly in a salvage operation in the setting of proximal humeral bone loss.34 35 36 37 The goal of this procedure is to provide a stable shoulder and allow for elbow, wrist, and hand function.34 35 36 37 Although the vascularized fibula helps patients to recover some upper extremity function, there still remains a high reoperation rate up to 43%.34 35 36 37
For metacarpal defects, although local flaps are frequently the first option, those injuries associated with significant soft tissue or bone loss can be treated successfully with free fibular flaps.31 38 39 40 In this setting, the free fibula can be divided into segments to bridge multiple bone defects.31 38 39 40 Typically, when the defect involves the joint surface, the joint is fused to the fibula.31 38 39 40 Alternatively, the fibula and proximal phalangeal articular surface can mimic a pseudarthrosis, preserving limited motion of the hand and wrist.38 40 Wrist preservation can also be achieved utilizing a silicone arthroplasty with the free fibula flap.41
Although the vascularized fibula bone grafts provide a reliable option to restore bony anatomy in the upper extremity, the functional recovery remains very difficult. This is due to the complex articulation of the forearm, hand, and wrist.42 Functional ratings following free fibula reconstruction vary drastically, with some patients reporting good overall function, while others have very poor function.21 22 30 31 35 One study suggested that patients with more distal reconstructions had better outcomes due to the amount of “normal” proximal tissue.31 However, there remains a lack of consensus about the specific indications that will lead to improved functional recoveries.
Capanna Technique
Although free vascularized fibular grafts have many advantages in upper extremity reconstruction, the vascular pedicle often prevents the use of dual plate or intramedullary fixation and they lack the structural support of large cortical allografts.5 Large cortical allografts have historically been used following tumor resection when diaphyseal and metaphyseal reconstruction is needed. Large structural allografts allow for strong fixation, but are prone to infection and fracture due to their avascular nature. Capanna described the combination of a large structural allograft with an intramedullary vascularized fibula in 1980. When these two graft types are combined, the osteogenic properties of the free fibula can be supplemented by the structural support of the bulk allograft, providing a durable biological reconstruction option.43 Although this technique is usually used to reconstruct lower extremity defects, it has been successfully utilized in the humerus.44 45 In a study by Li and colleagues, the authors showed excellent results using the Capanna technique following oncologic resection of the humeral diaphysis.45 Union was noted in all patients, with all able to return to physical activities using their upper extremity without weight-bearing restrictions.45
Vascularized Scapula
The scapular flap first described in 1982, is based off the subscapular artery.46 47 48 This flap has been used in the reconstruction of defects in the extremities following trauma and oncological extirpation.46 47 48 49 50 A bipedicled flap can be achieved by incorporating the angular branch of the thoracodorsal artery.51 Benefits of this flap are its large size, ability to be harvested with overlying muscle and skin, linear shape, ability to hypertrophy under physiological stress, and reliable vascular pedicle.46 47 48 49 50 52 53 54 Typically the scapular flap can be successfully used for reconstruction of upper extremity defects with minimal donor site morbidity.50 54 55
In recent years, the use of this flap has increased due to the rise in blast injuries in military settings.50 With a majority of blast injuries occurring to soldiers who are dismounted, there has been an increased rate of traumatic extremity amputations, resulting in a lack of the leg as a donor site for flap reconstruction of the upper extremity.50 Sabino and colleagues showed that in the setting of severe multiextremity trauma, the scapula flap was used successfully to reconstruct 10 upper extremity injuries (nine forearm/elbow and one hand). The limb salvage rate in this series was 100%.50 In another large study looking at the use of scapular flaps for upper extremity reconstruction, Datiashvili and colleagues successfully used this flap in 9 of 11 upper extremity defects (Fig. 2).54
Fig. 2.
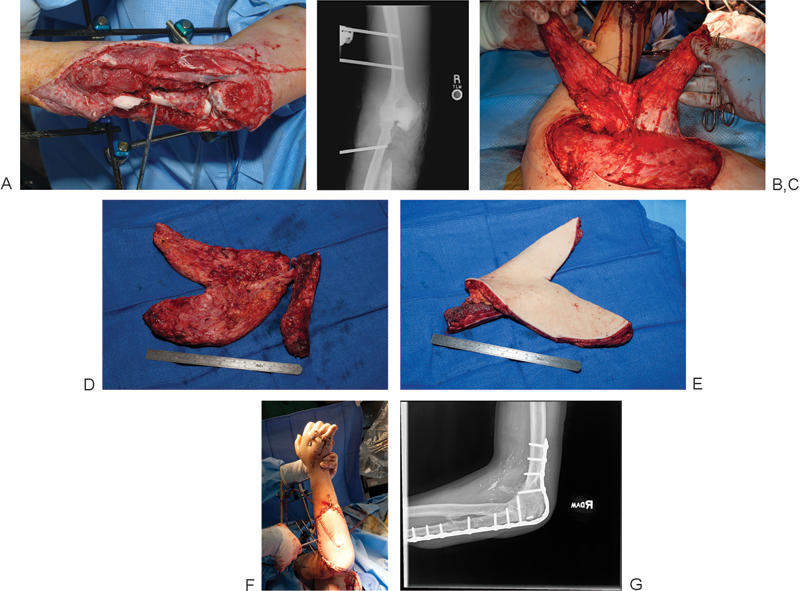
(A) A 19-year-old man who suffered open comminuted fracture of elbow with loss of proximal ulna and concomitant soft tissue loss following an explosion. (B) Anteroposterior (AP) radiograph showing proximal ulnar loss. Both legs were also lost in the injury, making donor sites for vascularized bone limited. (C,D) A composite flap based on the scapular system was designed to incorporate both the parascapular and scapular skin paddles, as well as the bone from the scapular spine. (E) Image of flap prior to inset. (F) Image at time of insetting. (G) Lateral radiograph showing radiographic union.
Vascularized Rib
Free rib flaps were first described in 1977 for reconstruction of lower extremity injuries.56 The rib is composed of membranous bone that possesses a dual blood supply, from the posterior intercostal artery and an abundant periosteal blood supply from the serratus anterior muscle.57 58 59 The periosteal blood supply is derived from the thoracodorsal artery providing a long reliable pedicle to be used in vascularized bone grafting. Typically this graft is used to reconstruct lower extremity or maxillofacial defects; however, there are a few reports of its use in the humerus and clavicle.60 61 62 63
In its use to reconstruct clavicular or humeral defects, the rib can either be transported as either a pedicled graft or as a free flap.60 61 62 63 One advantage of this flap is the combination of a large serratus muscle soft tissue envelope with or without the latissimus.57 58 59 The use of free rib graft for the treatment of humeral bone defects has been associated with union rates up to 100%.61 63 For the treatment of clavicular non-unions, Werner and colleagues showed that a double rib transfer was anatomically feasible and biomechanically superior to a single rib transfer to treat clavicular non-unions (Fig. 3).62
Fig. 3.
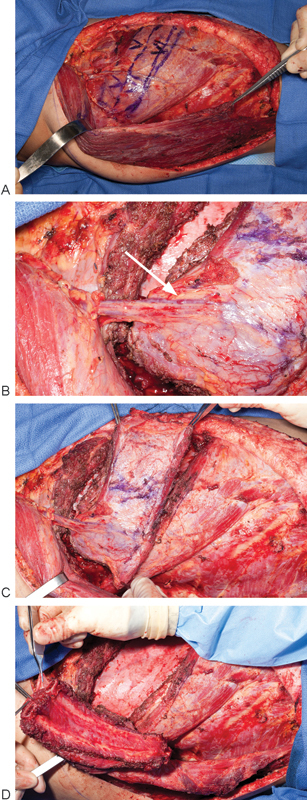
Single- and double-vascularized rib transfers have been found to be successful for clavicle, humerus, and forearm reconstruction. The addition of the serratus muscle provides excellent soft tissue coverage in cases of concomitant soft tissue loss. (A) The technique for elevation involves dissection of the lateral border of the latissimus to expose the serratus. (B) The serratus branch of the thoracodorsal artery is carefully isolated running on the superficial aspect of the serratus (arrow). (C) Two to three slips of the serratus muscle along with two underlying ribs are then dissected. (D) The intercostal muscle is included in the harvest to protect the periosteal blood supply. The chest wall defect is covered with dermal allograft or mesh prior to chest closure.
Vascularized Bone from the Distal Radius
First described in 1978, the radial forearm flap is now considered a “workhorse” flap for soft tissue reconstruction.64 Although it is typically used as a soft tissue flap, the radial forearm flap can also incorporate the lateral third of the distal radius to create an osteocutaneous forearm flap.64 65 This flap is commonly used for head and neck reconstruction; however, in cases of upper extremity reconstruction, this flap can either be a free or pedicled flap based off the radial artery.64 65 Niazi and colleagues noted a 100% graft survival when using this flap for upper extremity reconstruction.64
The downsides to using the radial forearm flap in cases of ipsilateral limb injury are multiple. First, the flap utilizes the radial artery and can potentially compromise blood flow to the hand. Additionally, the use of the radius bone with the radial artery is associated with a high incidence of iatrogenic fracture, thus limiting the use of this flap. A more applicable use of radius bone is to base the grafts on either the dorsal or palmar carpal arcade of vessels as described by Sheetz and colleagues; these grafts while small in size can be used to aid in carpal fusion or for the management of non-unions within the carpus.
Pedicled vascularized bone grafts from the dorsoradial aspect of the distal radius were first described by Zaidemberg in 1991.66 This flap is based off the ascending irrigating branch of the radial artery, specifically the 1,2 intercompartmental supraretinacular artery (ICSRA).12 66 In some studies, this pedicled bone graft has achieved a union rate as high as 90 to 100% when used in the treatment of scaphoid AVN or non-unions.66 67 68 69 Alternatively, a study by Boyer and colleagues reported union rates were only 60%.70 Of note, all the patients who failed in this study had failed a previous bone grafting procedure. Straw and colleagues also reported discouraging results, with union in only 27% of proximal pole scaphoid non-unions treated with pedicled distal radius flaps.71 Possible explanations for these findings could involve poor fracture fixation and removal of fixation components prior to the confirmation of healing.71 Additional studies have shown higher rates of failure in females and smokers, as well as the presence of humpback deformity of the scaphoid with these grafts.72 73 When union is achieved, the use of the 1,2 ICSRA flap can be expected to result in improved clinical outcomes, with decreases in Disabilities of the Arm, Shoulder and Hand (DASH) scoring and also improvements in SF-36 scores.73
Vascularized Medial Femoral Condyle
The medial femoral condyle (MFC) vascularized graft is based off either the articular descending genicular or superomedial genicular artery, creating either an osteoperiosteal or corticoperiosteal flap (Fig. 4).74 75 Along with the extraosseous blood supply, the MFC also possesses a robust intraosseous blood supply, with an average of 30 intraosseous perforators.76 These perforators are typically concentrated in the inferior distal quadrant of the MFC, making it the preferred location for graft elevation.77 Due to the consistent and robust vascular supply in the medial femoral condyle, this flap can be raised as a composite flap, including overlying skin and muscle.78 79 80
Fig. 4.
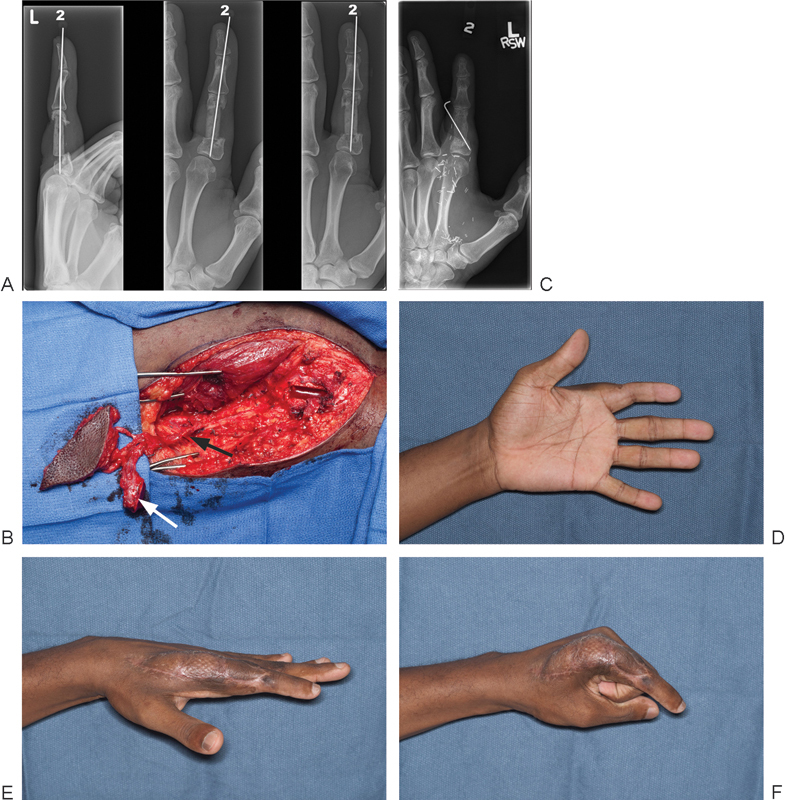
A 35-year-old man suffers a gunshot wound to the index finger resulting in loss of the majority of the proximal phalanx, but maintains finger viability and sensation. (A) Radiographs of finger showing antibiotic impregnated cement spacer placed within proximal phalanx to maintain length. (B) A flap is harvested based on the descending geniculate artery (black arrow) to include bone (white arrow) and skin. Bony healing is obtained in 9 weeks as seen in this (C) anteroposterior (AP) radiograph (D–F) and final function is acceptable.
In the upper extremity, the MFC graft has been most commonly described to reconstruct scaphoid non-unions.77 Initially, the MFC was used to treat non-unions of the scaphoid with associated AVN as an alternative to distal radius flaps.81 Secondary to the pliability and abundant vascularity of the graft, a high union rate is able to be achieved, leading to good to excellent recovery of wrist motion and pain relief in the majority of patients.81 When comparing pedicled distal radius flaps (1,2 ISCRA) to the MFC, it was found that the MFC was superior, especially in the setting of carpal collapse and AVN of the scaphoid.82 In the review by Jones and colleagues comparing MFC to 1,2 ISCRA flap in the setting of carpal collapse and scaphoid AVN, union was achieved in 100% of MFC flaps, compared with only 40% of the 1,2 ISCRA flaps.82 Likewise it has been shown that in the setting of scaphoid nonunion with associated carpal collapse, humpback deformity, or AVN, the MFC not only achieves healing of the nonunion site, but also contributes to an improvement in the carpal alignment and architecture.10
Additional uses for the MFC in the upper extremity include the humerus, clavicle, metacarpals, and forearm.75 77 83 84 85 86 In these cases the pliable flap is typically wrapped around the tubular bone to “patch” the non-union site, having subsequent union rates up to 100%.75 77 83 84 85 86 This graft deserves particular consideration in the clavicle in the setting of failed open reduction, internal fixation (ORIF) or fractures associated with prior radiation treatments.9 84 In these cases, the MFC is wrapped around the site of the non-union and held in place with heavy sutures.84 Because the MFC provides little structural stability, it is critical to supplement it with rigid internal fixation.84 This technique has also been successfully used to treat non-unions of the radius and ulna by resecting the nonunion and augmenting a rigid internal fixation with MFC graft.85 87 For atrophic non-unions of the humerus, the MFC flap is typically used at the time of revision fixation with reports of union ranging from 90 to 100%.9 55 83 88
In addition to being a corticocancellous flap, the MFC can also be an osteocartilaginous flap by including the medial femoral trochlea for the treatment of proximal pole of the scaphoid AVN.89 90 91 The size of the medial trochlea in relation to the arc of curvature of scaphoid allows for anatomical reconstruction of the scaphoid.90 In a series by Bürger et al, this flap was used in 16 patients, with healing of the nonunion noted in 15 patients.89 The patients in this study had a reduction in the pain, with a majority reporting no pain, and also an improvement in their wrist motion.89 Likewise there was preservation of the scapholunate relationship in patients undergoing this transfer through the preservation of the distal portion of the scapholunate ligament.89
Donor-site complications following this procedure are minimal. In a report by Jones et al, all patients noted knee pain following the procedure; however, at 6 weeks follow-up the pain had completely resolved and no long-term complications were noted.82 There have been no reports of deep infection, knee motion complications, or fracture reported.77 In a radiographic assessment of the knee in patients who have undergone MFC grafting, it was found that there was no increase in osteoarthritis compared with the contralateral side.92 Biomechanical studies have also shown that the stress of ambulation is not sufficient to cause a fracture, even in the setting of a large graft harvest.93
The Foot as a Donor Site for Vascularized Bone
Vascularized portions of the metatarsals have been used to reconstruct portions of the distal radius and ulna.94 95 For malunions of the distal radius, Del Pinal and colleagues have shown that the base of the third metatarsal can be used to reconstruct the articular surface.95 The authors showed significant improvement in wrist motion, grip strength, and also improvements in pain and DASH scores.95 Radiographs also showed preservation of the articular surface without any signs of osteoarthritis.95 Likewise, there were minimal donor-site complications, with a mean American Orthopedic Foot and Ankle score of 96/100 reported at follow-up.95
Similarly, a case report using the metatarsal head to reconstruct the distal radio-ulna joint (DRUJ) has been reported.94 In this patient, the soft tissue attachments of the sigmoid notch and triangular fibrocartilage complex (TFCC) were intact; however, the ulnar head suffered avascular necrosis following a fracture leading to pain and decreased function.94 The metatarsal head was transferred and used to successfully recreate the ulnar head, providing the patient with improvements in grip strength and symmetrical carpal motion.94
Vascularized Epiphyseal Transfer
Skeletally immature patients with large bone defects represent a challenging problem secondary to the need to match their healthy bone's growth in the upper extremity. One solution involves the transfer of the proximal fibular epiphysis enabling both bony reconstruction and growth potential. The use of the proximal fibular physis was first used to reconstruct the distal radius.96 The physis of the fibula is supplied by the anterior tibial artery. It is critical to maintain the proximal physeal blood supply to preserve the graft growth potential. The epiphyseal arterial pedicle arises from the main tibial artery just prior to entering the anterior compartment of the tibia, along with the musculoperiosteal branches to the diaphysis.97
Innocenti and colleagues showed the use of the proximal fibular physis can be successfully used to reconstruct the distal radius in children.98 The transplanted physes demonstrated reliable healing with continued growth at a rate similar to the contralateral side and ipsilateral ulna.98 Likewise, radiographs of the transplanted physis showed remodeling of the articular surface, providing a stable, functional wrist, with 70% of wrist motion compared with the contralateral side.98 Similar successful results have been demonstrated by other authors using proximal fibular physis transfer to the distal radius (Fig. 5).99 100
Fig. 5.
(A) A 9-year-old girl who presents with distal ulnar hypoplasia and non-union. Proximal fibular physeal transfer was used for reconstruction of the involved ulna. (B) Image of perforating branch to physis originating from the anterior tibial artery (arrowhead). (C) Image of graft prior to insetting. (D) Image of donor site showing carefully preserved branches of deep peroneal nerve, which must be preserved during dissection to avoid a postoperative foot drop. (E) Anteroposterior (AP) radiograph of forearm showing proximal bony union and re-establishment of forearm length.
The proximal fibular physis has also been used to reconstruct the proximal humerus in children.100 101 However, these results are not as promising as seen in the distal radius. In the largest series by Innocenti and colleagues, despite the high rate of graft fracture, all patients achieved a painless, functional extremity.101 The authors of this study feel the worse outcomes are related to the difference in size between the fibula and humerus, while also dependent on the amount of rotator cuff removed during the oncologic resection.101
Conclusion
Although the fibular graft still remains the gold standard for most upper extremity reconstruction, newer options such as the scapula osteocutaneous flap and extended medial femoral condyle flap have significant potential for reconstructing composite defects involving both bone and soft tissue. The possibility of articular reconstruction is now possible with vascularized grafts from the knee and foot. Long-term outcomes of these articular reconstructions still remain unknown; additional studies will be required to determine the long-term success and potential donor-site complications.
References
- 1.Wood M B, Cooney W P III, Irons G B Jr. Skeletal reconstruction by vascularized bone transfer: indications and results. Mayo Clin Proc. 1985;60(11):729–734. doi: 10.1016/s0025-6196(12)60414-5. [DOI] [PubMed] [Google Scholar]
- 2.Wood M B. Free vascularized bone transfers for nonunions, segmental gaps, and following tumor resection. Orthopedics. 1986;9(6):810–816. doi: 10.3928/0147-7447-19860601-07. [DOI] [PubMed] [Google Scholar]
- 3.de Boer H H, Wood M B. Bone changes in the vascularised fibular graft. J Bone Joint Surg Br. 1989;71(3):374–378. doi: 10.1302/0301-620X.71B3.2722923. [DOI] [PubMed] [Google Scholar]
- 4.Dell P C, Sheppard J E. Vascularized bone grafts in the treatment of infected forearm nonunions. J Hand Surg Am. 1984;9(5):653–658. doi: 10.1016/s0363-5023(84)80006-4. [DOI] [PubMed] [Google Scholar]
- 5.Taylor G I, Miller G D, Ham F J. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55(5):533–544. doi: 10.1097/00006534-197505000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Malizos K N, Zalavras C G, Soucacos P N, Beris A E, Urbaniak J R. Free vascularized fibular grafts for reconstruction of skeletal defects. J Am Acad Orthop Surg. 2004;12(5):360–369. doi: 10.5435/00124635-200409000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Wood M B. Femoral reconstruction by vascularized bone transfer. Microsurgery. 1990;11(1):74–79. doi: 10.1002/micr.1920110114. [DOI] [PubMed] [Google Scholar]
- 8.Han C S, Wood M B, Bishop A T, Cooney W P III. Vascularized bone transfer. J Bone Joint Surg Am. 1992;74(10):1441–1449. [PubMed] [Google Scholar]
- 9.Choudry U H, Bakri K, Moran S L, Karacor Z, Shin A Y. The vascularized medial femoral condyle periosteal bone flap for the treatment of recalcitrant bony nonunions. Ann Plast Surg. 2008;60(2):174–180. doi: 10.1097/SAP.0b013e318056d6b5. [DOI] [PubMed] [Google Scholar]
- 10.Jones D B Jr, Moran S L, Bishop A T, Shin A Y. Free-vascularized medial femoral condyle bone transfer in the treatment of scaphoid nonunions. Plast Reconstr Surg. 2010;125(4):1176–1184. doi: 10.1097/PRS.0b013e3181d1808c. [DOI] [PubMed] [Google Scholar]
- 11.Rizzo M, Moran S L. Vascularized bone grafts and their applications in the treatment of carpal pathology. Semin Plast Surg. 2008;22(3):213–227. doi: 10.1055/s-2008-1081404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheetz K K, Bishop A T, Berger R A. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg Am. 1995;20(6):902–914. doi: 10.1016/S0363-5023(05)80136-4. [DOI] [PubMed] [Google Scholar]
- 13.Shin A Y, Bishop A T, Berger R A. Vascularized pedicled bone grafts for disorders of the carpus. Tech Hand Up Extrem Surg. 1998;2(2):94–109. doi: 10.1097/00130911-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Innocenti M, Delcroix L, Balatri A. Vascularized growth plate transfer for distal radius reconstruction. Semin Plast Surg. 2008;22(3):186–194. doi: 10.1055/s-2008-1081402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Innocenti M Delcroix L Manfrini M Ceruso M Capanna R Vascularized proximal fibular epiphyseal transfer for distal radial reconstruction J Bone Joint Surg Am 200587(Pt 2, Suppl 1):237–246. [DOI] [PubMed] [Google Scholar]
- 16.Bieber E J, Wood M B. Bone reconstruction. Clin Plast Surg. 1986;13(4):645–655. [PubMed] [Google Scholar]
- 17.Arata M A, Wood M B, Cooney W P III. Revascularized segmental diaphyseal bone transfers in the canine. An analysis of viability. J Reconstr Microsurg. 1984;1(1):11–19. doi: 10.1055/s-2007-1007048. [DOI] [PubMed] [Google Scholar]
- 18.Berggren A, Weiland A J, Dorfman H. The effect of prolonged ischemia time on osteocyte and osteoblast survival in composite bone grafts revascularized by microvascular anastomoses. Plast Reconstr Surg. 1982;69(2):290–298. doi: 10.1097/00006534-198202000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Fujimaki A, Suda H. Experimental study and clinical observations on hypertrophy of vascularized bone grafts. Microsurgery. 1994;15(10):726–732. doi: 10.1002/micr.1920151012. [DOI] [PubMed] [Google Scholar]
- 20.Lin C H, Wei F C, Chen H C, Chuang D C. Outcome comparison in traumatic lower-extremity reconstruction by using various composite vascularized bone transplantation. Plast Reconstr Surg. 1999;104(4):984–992. doi: 10.1097/00006534-199909040-00013. [DOI] [PubMed] [Google Scholar]
- 21.Heitmann C, Erdmann D, Levin L S. Treatment of segmental defects of the humerus with an osteoseptocutaneous fibular transplant. J Bone Joint Surg Am. 2002;84-A(12):2216–2223. doi: 10.2106/00004623-200212000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Jupiter J B, Gerhard H J, Guerrero J, Nunley J A, Levin L S. Treatment of segmental defects of the radius with use of the vascularized osteoseptocutaneous fibular autogenous graft. J Bone Joint Surg Am. 1997;79(4):542–550. doi: 10.2106/00004623-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Wei F C, Chen H C, Chuang C C, Noordhoff M S. Fibular osteoseptocutaneous flap: anatomic study and clinical application. Plast Reconstr Surg. 1986;78(2):191–200. doi: 10.1097/00006534-198608000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Wood M B, Bishop A T. Massive bone defects of the upper limb: reconstruction by vascularized bone transfer. Hand Clin. 2007;23(1):49–56. doi: 10.1016/j.hcl.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Stevanovic M, Gutow A P, Sharpe F. The management of bone defects of the forearm after trauma. Hand Clin. 1999;15(2):299–318. [PubMed] [Google Scholar]
- 26.Soucacos P N, Korompilias A V, Vekris M D, Zoubos A, Beris A E. The free vascularized fibular graft for bridging large skeletal defects of the upper extremity. Microsurgery. 2011;31(3):190–197. doi: 10.1002/micr.20862. [DOI] [PubMed] [Google Scholar]
- 27.Kremer T Bickert B Germann G Heitmann C Sauerbier M Outcome assessment after reconstruction of complex defects of the forearm and hand with osteocutaneous free flaps Plast Reconstr Surg 20061182443–454., discussion 455–456 [DOI] [PubMed] [Google Scholar]
- 28.Minami A, Kasashima T, Iwasaki N, Kato H, Kaneda K. Vascularised fibular grafts. An experience of 102 patients. J Bone Joint Surg Br. 2000;82(7):1022–1025. doi: 10.1302/0301-620x.82b7.10332. [DOI] [PubMed] [Google Scholar]
- 29.Rose P S, Shin A Y, Bishop A T, Moran S L, Sim F H. Vascularized free fibula transfer for oncologic reconstruction of the humerus. Clin Orthop Relat Res. 2005;438(438):80–84. doi: 10.1097/01.blo.0000179586.34727.5b. [DOI] [PubMed] [Google Scholar]
- 30.Gebert C, Hillmann A, Schwappach A. et al. Free vascularized fibular grafting for reconstruction after tumor resection in the upper extremity. J Surg Oncol. 2006;94(2):114–127. doi: 10.1002/jso.20326. [DOI] [PubMed] [Google Scholar]
- 31.Rashid M, Hafeez S, Zia ul Islam M. et al. Limb salvage in malignant tumours of the upper limb using vascularised fibula. J Plast Reconstr Aesthet Surg. 2008;61(6):648–661. doi: 10.1016/j.bjps.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 32.Friedrich J B, Moran S L, Bishop A T, Wood C M, Shin A Y. Free vascularized fibular graft salvage of complications of long-bone allograft after tumor reconstruction. J Bone Joint Surg Am. 2008;90(1):93–100. doi: 10.2106/JBJS.G.00551. [DOI] [PubMed] [Google Scholar]
- 33.Wood M B. Upper extremity reconstruction by vascularized bone transfers: results and complications. J Hand Surg Am. 1987;12(3):422–427. doi: 10.1016/s0363-5023(87)80017-5. [DOI] [PubMed] [Google Scholar]
- 34.Bilgin S S. Reconstruction of proximal humeral defects with shoulder arthrodesis using free vascularized fibular graft. J Bone Joint Surg Am. 2012;94(13):e94. doi: 10.2106/JBJS.J.01823. [DOI] [PubMed] [Google Scholar]
- 35.Fuchs B, O'Connor M I, Padgett D J, Kaufman K R, Sim F H. Arthrodesis of the shoulder after tumor resection. Clin Orthop Relat Res. 2005;(436):202–207. doi: 10.1097/01.blo.0000162997.31976.15. [DOI] [PubMed] [Google Scholar]
- 36.Scalise J J, Iannotti J P. Glenohumeral arthrodesis after failed prosthetic shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(1):70–77. doi: 10.2106/JBJS.G.00203. [DOI] [PubMed] [Google Scholar]
- 37.Viehweger E, Gonzalez J F, Launay F. et al. [Shoulder arthrodesis with vascularized fibular graft after tumor resection of the proximal humerus] Rev Chir Orthop Repar Appar Mot. 2005;91(6):523–529. doi: 10.1016/s0035-1040(05)84442-3. [DOI] [PubMed] [Google Scholar]
- 38.Simsek T, Engin M S, Demir A, Tayfur V, Eroglu L. Reconstruction of hand injuries with multiple metacarpal defects using free fibular osteoseptocutaneous flap. Microsurgery. 2012;32(7):520–526. doi: 10.1002/micr.21977. [DOI] [PubMed] [Google Scholar]
- 39.Lee H B, Tark K C, Kang S Y, Kim S W, Chung Y K. Reconstruction of composite metacarpal defects using a fibula free flap. Plast Reconstr Surg. 2000;105(4):1448–1452. doi: 10.1097/00006534-200004040-00029. [DOI] [PubMed] [Google Scholar]
- 40.Lin C H, Wei F C, Rodriguez E D, Lin Y T, Chen C T. Functional reconstruction of traumatic composite metacarpal defects with fibular osteoseptocutaneous free flap. Plast Reconstr Surg. 2005;116(2):605–612. doi: 10.1097/01.prs.0000173554.46455.5a. [DOI] [PubMed] [Google Scholar]
- 41.Jones N F, Dickinson B P, Hansen S L. Reconstruction of an entire metacarpal and metacarpophalangeal joint using a fibular osteocutaneous free flap and silicone arthroplasty. J Hand Surg Am. 2012;37(2):310–315. doi: 10.1016/j.jhsa.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 42.Hollenbeck S T, Komatsu I, Woo S. et al. The current role of the vascularized-fibular osteocutaneous graft in the treatment of segmental defects of the upper extremity. Microsurgery. 2011;31(3):183–189. doi: 10.1002/micr.20703. [DOI] [PubMed] [Google Scholar]
- 43.Capanna R Campanacci D A Belot N et al. A new reconstructive technique for intercalary defects of long bones: the association of massive allograft with vascularized fibular autograft. Long-term results and comparison with alternative techniques Orthop Clin North Am 200738151–60., vi vi [DOI] [PubMed] [Google Scholar]
- 44.Chang D W, Weber K L. Use of a vascularized fibula bone flap and intercalary allograft for diaphyseal reconstruction after resection of primary extremity bone sarcomas. Plast Reconstr Surg. 2005;116(7):1918–1925. doi: 10.1097/01.prs.0000189203.38204.d5. [DOI] [PubMed] [Google Scholar]
- 45.Li J, Wang Z, Pei G X, Guo Z. Biological reconstruction using massive bone allograft with intramedullary vascularized fibular flap after intercalary resection of humeral malignancy. J Surg Oncol. 2011;104(3):244–249. doi: 10.1002/jso.21922. [DOI] [PubMed] [Google Scholar]
- 46.Gilbert A, Teot L. The free scapular flap. Plast Reconstr Surg. 1982;69(4):601–604. doi: 10.1097/00006534-198204000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Barwick W J, Goodkind D J, Serafin D. The free scapular flap. Plast Reconstr Surg. 1982;69(5):779–787. doi: 10.1097/00006534-198205000-00007. [DOI] [PubMed] [Google Scholar]
- 48.Hamilton S G, Morrison W A. The scapular free flap. Br J Plast Surg. 1982;35(1):2–7. doi: 10.1016/0007-1226(82)90075-3. [DOI] [PubMed] [Google Scholar]
- 49.Izadi D, Paget J T, Haj-Basheer M, Khan U M. Fasciocutaneous flaps of the subscapular artery axis to reconstruct large extremity defects. J Plast Reconstr Aesthet Surg. 2012;65(10):1357–1362. doi: 10.1016/j.bjps.2012.04.032. [DOI] [PubMed] [Google Scholar]
- 50.Sabino J, Franklin B, Patel K, Bonawitz S, Valerio I L. Revisiting the scapular flap: applications in extremity coverage for our U.S. combat casualties. Plast Reconstr Surg. 2013;132(4):577e–585e. doi: 10.1097/PRS.0b013e31829f4a08. [DOI] [PubMed] [Google Scholar]
- 51.Coleman J J III, Sultan M R. The bipedicled osteocutaneous scapula flap: a new subscapular system free flap. Plast Reconstr Surg. 1991;87(4):682–692. doi: 10.1097/00006534-199104000-00013. [DOI] [PubMed] [Google Scholar]
- 52.Allen R J, Dupin C L, Dreschnack P A, Glass C A, Mahon-Deri B. The latissimus dorsi/scapular bone flap (the “latissimus/bone flap”) Plast Reconstr Surg. 1994;94(7):988–996. doi: 10.1097/00006534-199412000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Guerra A B Metzinger S E Lund K M Cooper M M Allen R J Dupin C L The thoracodorsal artery perforator flap: clinical experience and anatomic study with emphasis on harvest techniques Plast Reconstr Surg 2004114132–41., discussion 42–43 [DOI] [PubMed] [Google Scholar]
- 54.Datiashvili R O, Yueh J H. Management of complicated wounds of the extremities with scapular fascial free flaps. J Reconstr Microsurg. 2012;28(8):521–528. doi: 10.1055/s-0032-1315772. [DOI] [PubMed] [Google Scholar]
- 55.Muramatsu K, Doi K, Ihara K, Shigetomi M, Kawai S. Recalcitrant posttraumatic nonunion of the humerus: 23 patients reconstructed with vascularized bone graft. Acta Orthop Scand. 2003;74(1):95–97. doi: 10.1080/00016470310013734. [DOI] [PubMed] [Google Scholar]
- 56.Buncke H J, Furnas D W, Gordon L, Achauer B M. Free osteocutaneous flap from a rib to the tibia. Plast Reconstr Surg. 1977;59(6):799–804. doi: 10.1097/00006534-197706000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Lin C H, Wei F C, Levin L S. et al. Free composite serratus anterior and rib flaps for tibial composite bone and soft-tissue defect. Plast Reconstr Surg. 1997;99(6):1656–1665. [PubMed] [Google Scholar]
- 58.Bruck J C, Bier J, Kistler D. The serratus anterior osteocutaneous free flap. J Reconstr Microsurg. 1990;6(3):209–213. doi: 10.1055/s-2007-1006820. [DOI] [PubMed] [Google Scholar]
- 59.Ueng W N, Chuang C C, Shih C H. Double-rib composite free transfer to reconstruct a single-spared lower extremity defect. J Trauma. 1995;38(2):210–212. doi: 10.1097/00005373-199502000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Onishi K, Maruyama Y. Compound rib-latissimus dorsi osteomusculocutaneous flap in reconstruction of the upper arm. Ann Plast Surg. 1996;37(2):191–194. doi: 10.1097/00000637-199608000-00014. [DOI] [PubMed] [Google Scholar]
- 61.Sundaresh D C, Gopalakrishnan D, Shetty N. Vascularised rib graft defects of the diaphysis of the humerus in children. A report of two cases. J Bone Joint Surg Br. 2000;82(1):28–32. doi: 10.1302/0301-620x.82b1.9678. [DOI] [PubMed] [Google Scholar]
- 62.Werner C M, Favre P, van Lenthe H G, Dumont C E. Pedicled vascularized rib transfer for reconstruction of clavicle nonunions with bony defects: anatomical and biomechanical considerations. Plast Reconstr Surg. 2007;120(1):173–180. doi: 10.1097/01.prs.0000263537.57701.8b. [DOI] [PubMed] [Google Scholar]
- 63.Unlü R E, Kargi A E, Celebioğlu S, Erdoğan B, Sensöz O. Reconstruction of the upper extremity with a compound rib-latissimus dorsi osteomusculocutaneous flap. Scand J Plast Reconstr Surg Hand Surg. 2002;36(1):34–38. doi: 10.1080/028443102753478354. [DOI] [PubMed] [Google Scholar]
- 64.Niazi Z B, McLean N R, Black M J. The radial forearm flap: a reconstructive chameleon. J Reconstr Microsurg. 1994;10(5):299–304. doi: 10.1055/s-2007-1006598. [DOI] [PubMed] [Google Scholar]
- 65.Cormack G C, Duncan M J, Lamberty B G. The blood supply of the bone component of the compound osteo-cutaneous radial artery forearm flap—an anatomical study. Br J Plast Surg. 1986;39(2):173–175. doi: 10.1016/0007-1226(86)90077-9. [DOI] [PubMed] [Google Scholar]
- 66.Zaidemberg C, Siebert J W, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg Am. 1991;16(3):474–478. doi: 10.1016/0363-5023(91)90017-6. [DOI] [PubMed] [Google Scholar]
- 67.Steinmann S P, Bishop A T, Berger R A. Use of the 1,2 intercompartmental supraretinacular artery as a vascularized pedicle bone graft for difficult scaphoid nonunion. J Hand Surg Am. 2002;27(3):391–401. doi: 10.1053/jhsu.2002.32077. [DOI] [PubMed] [Google Scholar]
- 68.Malizos K N, Dailiana Z H, Kirou M, Vragalas V, Xenakis T A, Soucacos P N. Longstanding nonunions of scaphoid fractures with bone loss: successful reconstruction with vascularized bone grafts. J Hand Surg [Br] 2001;26(4):330–334. doi: 10.1054/jhsb.2001.0570. [DOI] [PubMed] [Google Scholar]
- 69.Tsai T T, Chao E K, Tu Y K, Chen A C, Lee M S, Ueng S W. Management of scaphoid nonunion with avascular necrosis using 1, 2 intercompartmental supraretinacular arterial bone grafts. Chang Gung Med J. 2002;25(5):321–328. [PubMed] [Google Scholar]
- 70.Boyer M I, von Schroeder H P, Axelrod T S. Scaphoid nonunion with avascular necrosis of the proximal pole. Treatment with a vascularized bone graft from the dorsum of the distal radius. J Hand Surg [Br] 1998;23(5):686–690. doi: 10.1016/s0266-7681(98)80029-6. [DOI] [PubMed] [Google Scholar]
- 71.Straw R G, Davis T R, Dias J J. Scaphoid nonunion: treatment with a pedicled vascularized bone graft based on the 1,2 intercompartmental supraretinacular branch of the radial artery. J Hand Surg [Br] 2002;27(5):413. doi: 10.1054/jhsb.2002.0808. [DOI] [PubMed] [Google Scholar]
- 72.Chang M A, Bishop A T, Moran S L, Shin A Y. The outcomes and complications of 1,2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. J Hand Surg Am. 2006;31(3):387–396. doi: 10.1016/j.jhsa.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 73.Hirche C, Heffinger C, Xiong L. et al. The 1,2-intercompartmental supraretinacular artery vascularized bone graft for scaphoid nonunion: management and clinical outcome. J Hand Surg Am. 2014;39(3):423–429. doi: 10.1016/j.jhsa.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 74.Hertel R, Masquelet A C. The reverse flow medial knee osteoperiosteal flap for skeletal reconstruction of the leg. Description and anatomical basis. Surg Radiol Anat. 1989;11(4):257–262. doi: 10.1007/BF02098691. [DOI] [PubMed] [Google Scholar]
- 75.Sakai K, Doi K, Kawai S. Free vascularized thin corticoperiosteal graft. Plast Reconstr Surg. 1991;87(2):290–298. doi: 10.1097/00006534-199102000-00011. [DOI] [PubMed] [Google Scholar]
- 76.Yamamoto H, Jones D B Jr, Moran S L, Bishop A T, Shin A Y. The arterial anatomy of the medial femoral condyle and its clinical implications. J Hand Surg Eur Vol. 2010;35(7):569–574. doi: 10.1177/1753193410364484. [DOI] [PubMed] [Google Scholar]
- 77.Friedrich J B, Pederson W C, Bishop A T, Galaviz P, Chang J. New workhorse flaps in hand reconstruction. Hand (NY) 2012;7(1):45–54. doi: 10.1007/s11552-011-9385-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rahmanian-Schwarz A, Spetzler V, Amr A, Pfau M, Schaller H E, Hirt B. A composite osteomusculocutaneous free flap from the medial femoral condyle for reconstruction of complex defects. J Reconstr Microsurg. 2011;27(4):251–260. doi: 10.1055/s-0031-1275489. [DOI] [PubMed] [Google Scholar]
- 79.Pelzer M, Reichenberger M, Germann G. Osteo-periosteal-cutaneous flaps of the medial femoral condyle: a valuable modification for selected clinical situations. J Reconstr Microsurg. 2010;26(5):291–294. doi: 10.1055/s-0030-1248239. [DOI] [PubMed] [Google Scholar]
- 80.Iorio M L, Masden D L, Higgins J P. Cutaneous angiosome territory of the medial femoral condyle osteocutaneous flap. J Hand Surg Am. 2012;37(5):1033–1041. doi: 10.1016/j.jhsa.2012.02.033. [DOI] [PubMed] [Google Scholar]
- 81.Doi K, Sakai K. Vascularized periosteal bone graft from the supracondylar region of the femur. Microsurgery. 1994;15(5):305–315. doi: 10.1002/micr.1920150505. [DOI] [PubMed] [Google Scholar]
- 82.Jones D B Jr, Bürger H, Bishop A T, Shin A Y. Treatment of scaphoid waist nonunions with an avascular proximal pole and carpal collapse. A comparison of two vascularized bone grafts. J Bone Joint Surg Am. 2008;90(12):2616–2625. doi: 10.2106/JBJS.G.01503. [DOI] [PubMed] [Google Scholar]
- 83.Kakar S, Duymaz A, Steinmann S, Shin A Y, Moran S L. Vascularized medial femoral condyle corticoperiosteal flaps for the treatment of recalcitrant humeral nonunions. Microsurgery. 2011;31(2):85–92. doi: 10.1002/micr.20843. [DOI] [PubMed] [Google Scholar]
- 84.Fuchs B, Steinmann S P, Bishop A T. Free vascularized corticoperiosteal bone graft for the treatment of persistent nonunion of the clavicle. J Shoulder Elbow Surg. 2005;14(3):264–268. doi: 10.1016/j.jse.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 85.De Smet L. Treatment of non-union of forearm bones with a free vascularised corticoperiosteal flap from the medial femoral condyle. Acta Orthop Belg. 2009;75(5):611–615. [PubMed] [Google Scholar]
- 86.Jones D B Jr, Rhee P C, Bishop A T, Shin A Y. Free vascularized medial femoral condyle autograft for challenging upper extremity nonunions. Hand Clin. 2012;28(4):493–501. doi: 10.1016/j.hcl.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 87.Del Piñal F, García-Bernal F J, Regalado J, Ayala H, Cagigal L, Studer A. Vascularised corticoperiosteal grafts from the medial femoral condyle for difficult non-unions of the upper limb. J Hand Surg Eur Vol. 2007;32(2):135–142. doi: 10.1016/J.JHSB.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 88.Yajima H, Maegawa N, Ota H, Kisanuki O, Kawate K, Takakura Y. Treatment of persistent non-union of the humerus using a vascularized bone graft from the supracondylar region of the femur. J Reconstr Microsurg. 2007;23(2):107–113. doi: 10.1055/s-2007-970182. [DOI] [PubMed] [Google Scholar]
- 89.Bürger H K, Windhofer C, Gaggl A J, Higgins J P. Vascularized medial femoral trochlea osteocartilaginous flap reconstruction of proximal pole scaphoid nonunions. J Hand Surg Am. 2013;38(4):690–700. doi: 10.1016/j.jhsa.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 90.Hugon S, Koninckx A, Barbier O. Vascularized osteochondral graft from the medial femoral trochlea: anatomical study and clinical perspectives. Surg Radiol Anat. 2010;32(9):817–825. doi: 10.1007/s00276-010-0629-1. [DOI] [PubMed] [Google Scholar]
- 91.Kälicke T, Bürger H, Müller E J. [A new vascularized cartilague-bone-graft for scaphoid nonunion with avascular necrosis of the proximal pole. Description of a new type of surgical procedure] Unfallchirurg. 2008;111(3):201–205. doi: 10.1007/s00113-007-1308-5. [DOI] [PubMed] [Google Scholar]
- 92.Rao S S, Sexton C C, Higgins J P. Medial femoral condyle flap donor-site morbidity: a radiographic assessment. Plast Reconstr Surg. 2013;131(3):357e–362e. doi: 10.1097/PRS.0b013e31827c6f38. [DOI] [PubMed] [Google Scholar]
- 93.Katz R D, Parks B G, Higgins J P. The axial stability of the femur after harvest of the medial femoral condyle corticocancellous flap: a biomechanical study of composite femur models. Microsurgery. 2012;32(3):213–218. doi: 10.1002/micr.20986. [DOI] [PubMed] [Google Scholar]
- 94.del Piñal F, Guerrero-Navarro M L, Studer A, Thams C, Moraleda E. Reconstruction of the ulnar head with a vascularized second metatarsal head: case report. J Hand Surg Am. 2012;37(8):1568–1573. doi: 10.1016/j.jhsa.2012.04.039. [DOI] [PubMed] [Google Scholar]
- 95.del Piñal F, Klausmeyer M, Moraleda E. et al. Vascularized graft from the metatarsal base for reconstructing major osteochondral distal radius defects. J Hand Surg Am. 2013;38(10):1883–1895. doi: 10.1016/j.jhsa.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 96.Pho R W. Malignant giant-cell tumor of the distal end of the radius treated by a free vascularized fibular transplant. J Bone Joint Surg Am. 1981;63(6):877–884. [PubMed] [Google Scholar]
- 97.Taylor G I, Wilson K R, Rees M D, Corlett R J, Cole W G. The anterior tibial vessels and their role in epiphyseal and diaphyseal transfer of the fibula: experimental study and clinical applications. Br J Plast Surg. 1988;41(5):451–469. doi: 10.1016/0007-1226(88)90001-x. [DOI] [PubMed] [Google Scholar]
- 98.Innocenti M, Delcroix L, Manfrini M, Ceruso M, Capanna R. Vascularized proximal fibular epiphyseal transfer for distal radial reconstruction. J Bone Joint Surg Am. 2004;86-A(7):1504–1511. doi: 10.2106/00004623-200407000-00021. [DOI] [PubMed] [Google Scholar]
- 99.Akinbo O, Strauch R. Physeal transfers for skeletal reconstruction. J Hand Surg Am. 2008;33(4):584–590. doi: 10.1016/j.jhsa.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 100.Medrykowski F, Barbary S, Gibert N, Lascombes P, Dautel G. Vascularized proximal fibular epiphyseal transfer: two cases. Orthop Traumatol Surg Res. 2012;98(6):728–732. doi: 10.1016/j.otsr.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 101.Innocenti M Delcroix L Romano G F Capanna R Vascularized epiphyseal transplant Orthop Clin North Am 200738195–101., vii [DOI] [PubMed] [Google Scholar]


