Abstract
Background
Over the years, en bloc spondylectomy has proven its efficacy in controlling spinal tumors and improving survival rates. However, there are few reports of large series that critically evaluate the results of multilevel en bloc spondylectomies for spinal neoplasms.
Questions/purposes
Using data from a large spine tumor center, we answered the following questions: (1) Does multilevel total en bloc spondylectomy result in acceptable function, survival rates, and local control in spinal neoplasms? (2) Is reconstruction after this procedure feasible? (3) What complications are associated with this procedure? (4) is it possible to achieve adequate surgical margins with this procedure?
Methods
We retrospectively investigated 38 patients undergoing multilevel total en bloc spondylectomy by a single surgeon (AL) from 1994 to 2011. Indications for this procedure were primary spinal sarcomas, solitary metastases, and aggressive primary benign tumors involving multiple segments of the thoracic or lumbar spine. Patients had to be medically fit and have no visceral metastases. Analysis was by chart and radiographic review. Margin quality was classified into intralesional, marginal, and wide. Radiographs, MR images, and CT scans were studied for local recurrence. Graft healing and instrumentation failures at subsequent followup were assessed. Complications were divided into major or minor and further classified as intraoperative and early and late postoperative. We evaluated the oncologic status using cumulative disease-specific and metastases-free survival analysis. Minimum followup was 24 months (mean, 39 months; range, 24–124 months).
Results
Of the 38 patients, 34 (89%) were alive and walking without support at final followup. Thirty-one (81%) had no evidence of disease. Two patients died postoperatively and another two died of systemic disease (without local recurrence). Only three patients (8%) had a local recurrence. There were 14 major complications and 22 minor complications in 25 patients (65%). Only one patient required revision of implants secondary to mechanical failure. Two cases of cage subsidence were noted but had no clinical significance. Wide margins were achieved in nine patients (23%), marginal in 25 (66%), and intralesional in four (11%).
Conclusions
In patients with multisegmental spinal tumors, oncologic resections were achieved by multilevel en bloc spondylectomy and led to an acceptable survival rate with reasonable local control. Multilevel en bloc surgery was associated with a high complication rate; however, most patients recovered from their complications. Although the surgical procedure is challenging, our encouraging mid-term results clearly favor and validate this technique.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3578-x) contains supplementary material, which is available to authorized users.
Introduction
Over the years, total en bloc spondylectomy has proved its efficacy in local disease control and improved survival rates in patients with tumors of the spine [2, 4, 7, 11–13, 15, 17, 19, 21, 23]. This technique was developed to resect the tumor en bloc, thus achieving safe tumor-free margins and reducing recurrences. Multilevel en bloc resections are technically demanding and are associated with considerable morbidity, owing to the proximity of neurovascular structures, visceral organs, need for a combined anterior and posterior approach, and increased blood loss, surgical time, and risk of complications.
Total en bloc spondylectomy is a difficult procedure even in experienced hands. It becomes further challenging when the tumor involves multiple levels and visceral structures. There are a few reports in the literature on multilevel en bloc procedures, although most are case reports and small series [1, 3, 5, 6, 8, 9, 13, 14, 20].
We therefore evaluated a larger group of patients who underwent multilevel en bloc spondylectomy in the treatment of spinal tumors affecting the thoracic and lumbar spine. Using data from a large spine tumor center, we answered the following questions: (1) Does multilevel en bloc spondylectomy result in acceptable function, survival rates, and local control in spinal neoplasms? (2) Is reconstruction after multisegmental spinal tumor surgery feasible? (3) What are the complications associated with this procedure? (4) is it possible to achieve adequate surgical margins with this procedure?
Patients and Methods
Study Patients
We performed a retrospective study of patients treated with multilevel total en bloc spondylectomy by the same surgeon (AL) between January 1994 and January 2011. During the study period, 130 patients underwent total en bloc spondylectomies. For this study, we assessed only patients treated with multilevel thoracic and lumbar total en bloc spondylectomy for primary spinal sarcomas, solitary metastases, and aggressive primary benign tumors with a minimum 2-year followup. All patients with single-level total en bloc spondylectomy were excluded. Patients with cervical and cervicothoracic tumors were also excluded. Patients were diagnosed based on histopathology reports of a core needle biopsy. Whole-body CT, MRI of the whole spine, bone scintigraphy, and positron emission tomography were performed on all patients. In patients with an established diagnosis from previous surgeries, a new biopsy was not performed.
Thirty-eight patients were included in the study. There were 20 females and 18 males, with a mean age of 48 years (range, 8–74 years). Total en bloc spondylectomy involved two levels in 19 patients (Figs. 1, 2), three levels in 15 patients (Suppl Figs. 1, 2; supplemental materials are available with the online version of CORR®), four levels in three patients (Figs. 3–5), and five levels in one patient (Suppl Fig. 3; supplemental materials are available with the online version of CORR®). The majority of patients were diagnosed with spinal sarcomas (Table 1). No patients were lost to followup. The mean followup was 39 months (range, 24–124 months).
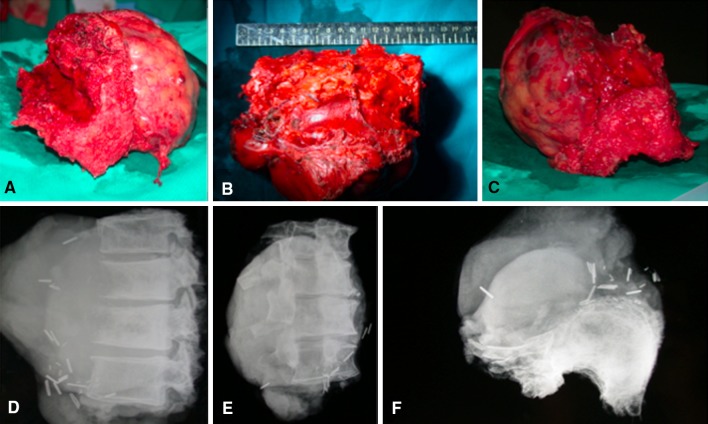
Fig. 4A–F.
Postoperative images are shown for the patient in Figure 3. (A–C) A 15- × 10- × 8-cm tumor was resected. (D) Lateral, (E) coronal, and (F) axial CT scans show the specimen. Histopathology reported marginal margins.
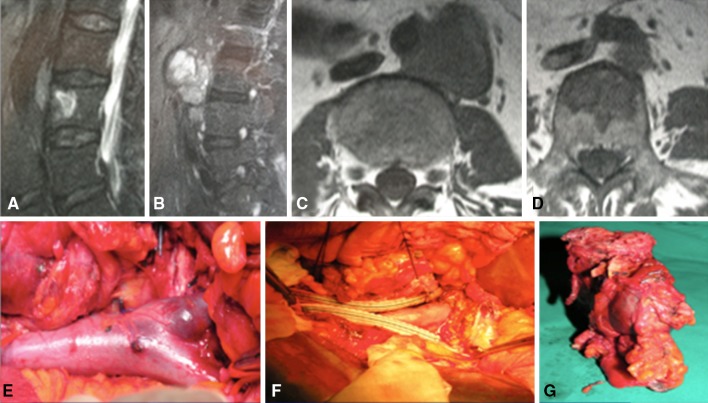
Fig. 1A–G.
Images illustrate the case of a 63-year-old woman, diagnosed with a two-level (L3–L4) synovial sarcoma with involvement of bifurcation of the aorta. (A–D) MR images show a tumor spanning across L3–L4, involving the aorta. (E) Through an anterior approach, the bifurcation of the aorta was exposed. (F) The aorta was ligated above and below the involved area and a bypass graft was created with the aid of a vascular surgeon. The bifurcation was left in situ with the tumor and was resected en bloc through a posterior approach. (G) The tumor was removed en bloc along with the L3 and L4 bodies and bifurcation of the aorta.
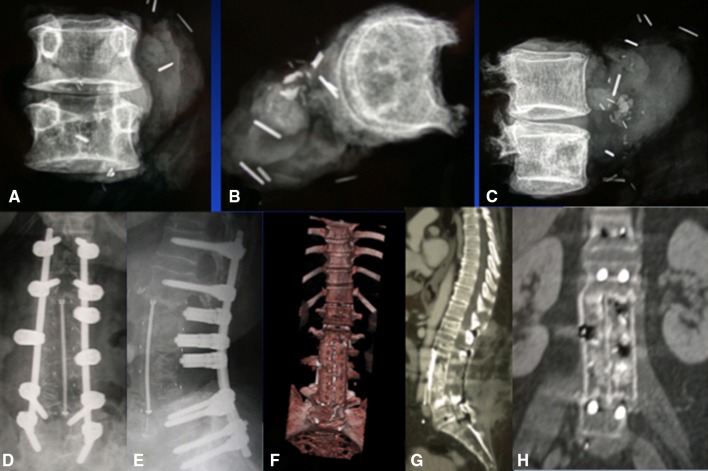
Fig. 2A–H.
Postoperative images are shown for the patient in Fig. 1. (A–C) CT scan shows the tumor immediately after en bloc removal to assess margins and histopathology, which reported wide margins. (D, E) Postoperative radiographs show the reconstruction of the defect. (F) Three-dimensional, (E) sagittal and (H) coronal CT scans taken at 18 months show no cage subsidence and good fusion. The patient was alive with no evidence of disease at 8 years.
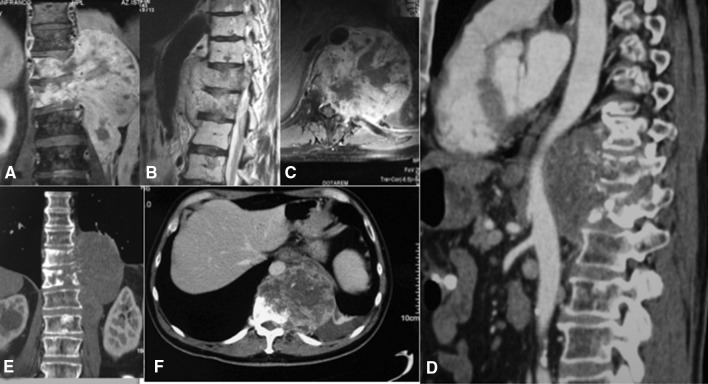
Fig. 3A–F.
Images illustrate the case of a 64-year-old man diagnosed with four-level (T10–L1) chordoma, with involvement of the adventitia of the aorta. (A) Coronal, (B) sagittal, and (C) axial MR images show a tumor spanning from T10 to L1. (D) A CT angiogram shows the tumor in close proximity to the aorta, involving its adventitia. (E) Coronal and (F) axial CT scans show the extent of the tumor. We undertook resection using an anterior–posterior approach. The adventitia of the aorta was adherent to the tumor. It was separated and the tumor was removed en bloc along with the adventitia via the posterior approach.
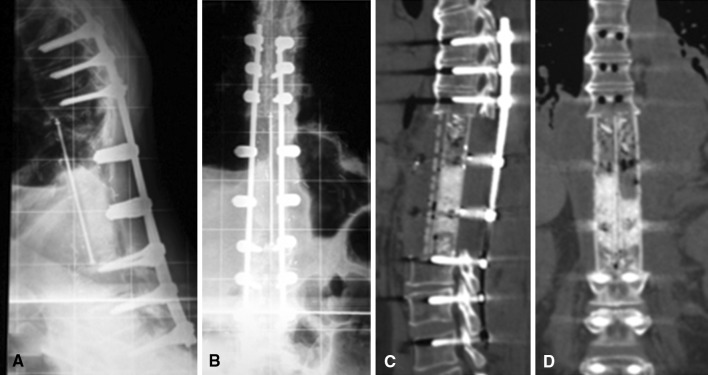
Fig. 5A–D.
Followup images are shown for the patient in Figures 3 and 4. Postoperative (A) lateral and (B) AP radiographs show stable reconstruction of the defect. The patient developed neurologic deterioration (Grade 2) postoperatively, which recovered to Grade 4. (C) Sagittal and (D) coronal CT scan at 18 months show no implant failure. The patient was alive with systemic disease but no local recurrence at 9 years.
Table 1.
Types of tumors affecting patients
| Type of tumor | Number of patients |
|---|---|
| Chondrosarcoma | 6 |
| Chordoma | 6 |
| Osteosarcoma | 6 |
| Lung adenocarcinoma | 5 |
| Single metastasis | 4 (2 kidney, 2 breast) |
| Synovial sarcoma | 3 |
| Malignant hemangioendothelioma | 3 |
| Malignant high-grade schwannoma | 2 |
| Aggressive giant cell tumor | 2 |
| Leiomyosarcoma | 1 |
Surgical Decision Making
Surgical decision making was achieved by a multispecialty team that included the primary spine surgeon, approach-related surgeon, oncologist, radiotherapist, and anesthesiologist. Only after thorough discussion were patients offered a multilevel en bloc procedure. Patients who had a chance of increased survival and disease-free life were offered surgery. The indications for surgery were similar to those suggested by Tomita et al. [23, 24]: patients having solitary metastases or primary malignant tumors, who were medically fit, and had no visceral metastases. Tumor involvement was classified as Stage 6 (involving two or more levels).according to the classification of Tomita et al. [24].
The surgical approach and technique were chosen based on the location and size of the tumor and involvement of surrounding neurovascular structures, as evident on radiographic studies. Guidance from approach-related surgeons was used in decision making and surgery. After the surgical plan was confirmed, the patients were thoroughly briefed regarding the procedure and the morbidity associated with it. If preoperative radiotherapy would be required, depending on tumor histology, the patients underwent surgery after 30 days but no later than 40 days after radiotherapy. Preoperative spinal angiography was performed in all patients to study the anatomy of Adamkiewicz’ artery. Preoperative embolization was performed only in the two patients with kidney metastases.
Surgical Procedure
Multilevel en bloc spondylectomy requires release of surrounding neurovascular structures from the tumor, en bloc resection of the tumor, posterior instrumentation, and reconstruction of the anterior defect. In patients with three or more levels of involvement, we released the neurovascular structures using primarily an anterior approach followed by posterior en bloc removal, pedicle screw instrumentation, and reconstruction of the anterior defect. If any surrounding structures were involved in the tumor, a partial or full resection was undertaken with the aid of another specialist surgeon. For the majority of two-level tumors, an all-posterior approach was sufficient. In a few patients, we also went posterior–anterior–posterior. The decision concerning the type and number of approaches depended on the relationship of the tumor with the surrounding vital structures.
In anterior–posterior surgeries, once release was completed, a gauze sponge was placed anterior to the tumor, protecting the neurovascular structures and surrounding organs, which would later be accessible and removed from the second posterior approach. After completing the anterior release, the patient was positioned prone for the posterior en bloc resection. We generally prefer a same-day anterior–posterior procedure unless the patient is hemodynamically unstable after the first procedure. The posterior procedure included insertion of pedicle screws, removal of the laminae, bilateral costotranversectomy (in the thoracic spine, usually for a four-level resection, five to six ribs were removed bilaterally), resection of the nerve roots, and release of the dura from the tumor. The pedicles were then removed using a high-speed burr, a curette, or an ultrasonic scalpel. In case of pedicle involvement, the pedicles were left in situ and removed en bloc with the tumor. A temporary rod was then fixed on one side. Malleable retractors were placed anterior to the vertebral bodies, protecting the surrounding neurovascular structures. The caudad and cephalad discs were then removed and the tumor, along with the vertebral bodies and other structures involved (lung, aorta, nerve roots, etc), was removed en bloc from posteriorly. Using large towel clips to hold the vertebrae and applying a rotating maneuver aided in posterior en bloc removal of the tumor. Once the tumor was resected, it was sent for CT scan and MRI to confirm the margins achieved. The caudad and cephalad end plates were then curetted to prepare a vascular bed for fusion. In patients who had only ½ of the vertebral bodies removed, the posterior vertebral osteotomy was done using an ultrasonic scalpel and osteotomes while maintaining anterior control and protection of the major surrounding organs with malleable retractors. The gauze piece that was placed during the anterior procedure was then removed and a thorough wash using normal saline was given.
In patients requiring a two-level en bloc spondylectomy, an all-posterior approach was advocated if the anterior visceral and vascular structures were not involved. The surgery required removal of all posterior structures, bilateral costotransversectomy in the thoracic spine, and thorough release of the spinal cord or cauda equina. Lumbar roots were also sacrificed if need be; however, every attempt was made to save the lumbar roots. A plane was created between the anterior vascular structures and the anterior wall of vertebral body. Malleable retractors were placed to protect the anterior structures and then an en bloc spondylectomy was carried out.
Anterior reconstruction in the thoracic and lumbar spine was then performed using stackable carbon cages (coLigne AG, Zurich, Switzerland) filled with iliac crest and rib autograft or with autologous bone grafts only or autografts and allografts. Rods (coLigne) were then applied and compressed. We also used false pedicles (implants that replace resected pedicles) (coLigne) connecting the cage anteriorly and rod posteriorly. This was mainly done to prevent the lung falling onto the dura. Drains were placed and skin closed in layers.
Aftercare
Postoperatively, patients were transferred to the intensive care unit. Drains were removed once collection was less than 100 mL. Patients were started on deep vein thrombosis prophylaxis (low-molecular-weight heparin) the next morning and calf pumps for 1 week. Mobilization was started once patients were shifted from the intensive care unit. Depending on the oncologist, patients were started on adjuvant chemotherapy postoperatively.
Perioperative Data
Mean operative time was 9 hours (range, 7–16 hours). Mean total blood loss was 4000 mL (range, 2500–16,000 mL). Mean stay in the intensive care unit was 3.8 days (range, 2–14 days). Mean stay in the hospital was 18 days (range, 12–40 days). The operative time, blood loss, and total hospital stay were higher with higher numbers of levels resected due to increased risk of complications.
Data Collection and Outcome Measures
Patient and surgical data (age, type of tumor, previous surgeries, surgical time, approach, blood loss, total blood transfused, type of instrumentation, type of bone graft and interbody cage) were recorded. Preoperatively, tumor involvement was classified according to the surgical strategy classification of Tomita et al. [24]. We evaluated metastatic lesions using the revised prognostic score of Tokuhashi et al. [22] and the score of Tomita et al. [23]. Treatment with radiotherapy and chemotherapy was assessed.
Patients were evaluated every 3 months for the first 2 years and then every 6 months thereafter. Radiographs, MRI, and CT scans were studied for local recurrences, cage subsidence, and instrumentation failures at followups. At final followup, patients were classified as alive or dead with or without evidence of disease. Complications were divided into major (altering the expected course of recovery) or minor. Function (walking status) was recorded. Resected tumor data were studied with respect to histopathology margins. All resected specimens were subjected to CT scan and/or MRI to confirm radiographic margins. Type of excision was classified into intralesional, marginal, and wide margins.
Results
Of the 38 patients, 34 (89%) were walking without support at final followup. Thirty-one patients (81%) were alive without any evidence of disease at final followup. Three patients had local recurrences (8%) and were alive with evidence of disease. These three patients had intralesional margins reported on histopathology. Two patients (5%) died of systemic disease at 10 and 27 months postoperatively. Two patients (5%) died of complications during the first postoperative month.
Anterior reconstruction of the defect after en bloc spondylectomy was achieved using stackable carbon cages filled with iliac crest and rib autograft in 30 patients, autologous bone graft only in four patients, and autografts and allografts in four patients. Only autografts and allografts were used mainly in two-level en bloc spondylectomy and during the initial years of the surgery. Carbon cages were used in most of the patients during the last decade. Posterior instrumentation was achieved using pedicle screws in all patients. False pedicles connecting the cage anteriorly and rod posteriorly were also used in patients with thoracic involvement or involvement of more than four levels. Only one patient required revision of instrumentation due to mechanical failure. Cage subsidence was found in two patients but was of no clinical or radiographic significance with respect to the outcome. The combined anterior–posterior approach was undertaken in 27 patients and the all-posterior approach in 11 patients. Bifurcation of the aorta was involved in the tumor in one patient. It was resected en bloc along with the tumor and replaced (Figs. 1, 2). The patient is alive without evidence of disease at 8 years postoperatively. Similarly, inferior lobe of the lung was resected en bloc in one patient, adventitia of the aorta in one patient, and unilateral kidney in one patient.
There were 14 major complications and 22 minor complications in 25 patients. Major complications included massive intraoperative bleeding (16,000 and 10,000 mL) in two patients, leading to death in one patient secondary to intraoperative vascular injury. The vessel injury could be attributed to a previously irradiated aorta. The site was packed and closed. The patient died 5 days postoperatively in the intensive care unit. Another patient died postoperatively due to cardiac arrest 8 days after surgery. One patient receiving four-level en bloc spondylectomy had major neurologic deterioration postoperatively (Grade 2 power in bilateral lower limbs) that recovered to Grade 4 at final followup (Figs. 3–5). There were five major infections requiring débridement and antibiotics for 6 weeks. Four patients had minor infections treated with antibiotics only. Eight patients had iatrogenic thoracic duct lesions that did not require any revision. Thoracic duct injury is difficult to avoid in multilevel thoracic spondylectomy due to the anatomy of the duct, which lies very close to the vertebral bodies. Thirteen patients had intraoperative cerebrospinal fluid leakage. Three of these patients required revision of the leak. One patient required revision of instrumentation secondary to mechanical failure. All of the living patients recovered from their complications at last followup.
Histopathologic surgical margins achieved were wide in nine patients (23%), marginal in 25 patients (65%), and intralesional in four patients (12%). Three patients with intralesional margins had recurrences.
Discussion
The aim of total en bloc spondylectomy is to achieve safe margins which leads to increased survival rates and reduce local recurrences. For obvious reasons, there are no studies comparing en bloc resections such as these to other treatments. Radical resections are frequently carried out for malignant tumors involving long bones with good success rates [18]. In the spine, radical resection is rarely possible; hence, wide or marginal resection is often the goal to achieve safe margins. When spinal tumors (not responding to medical treatment and requiring resection) involve multiple segments with adjoining structures, the only surgical option left is to carry out a multilevel total en bloc spondylectomy. Hence, we investigated the results of multilevel total en bloc spondylectomy in the management of complex spinal tumors by answering the following questions: (1) Does multilevel total en bloc spondylectomy result in acceptable function, survival rates, and local control in spine neoplasms? (2) Is reconstruction after multisegmental spinal tumor surgery feasible? (3) What are the complications associated with this procedure? (4) is it possible to achieve adequate surgical margins with this procedure?
One limitation of this study is the small sample size (38 patients). However, other studies [1, 5] reporting on en bloc spondylectomy have included even fewer numbers of patients. The indications for this surgery are limited, hence the small sample size. This study is a retrospective study; larger studies with a comparison group are required to establish a definitive role of multilevel total en bloc spondylectomy in the treatment of spinal tumors, but such data will be difficult if not impossible to obtain. Also, this is a heterogeneous group of patients with a broad range of ages and diagnoses ranging from benign aggressive tumors to sarcomas and metastatic carcinoma.
In our study, at final followup, 34 patients (89%) were walking without support with local control. Thirty-one patients (81%) were alive without any evidence of disease. Other case series and case reports in the literature have also shown total en bloc spondylectomy to be effective in increasing patient survival and preventing local recurrences [1, 3, 5, 6, 8, 9, 13, 14, 20] (Table 2). Boriani et al. [1], in their study of 33 patients undergoing multilevel en bloc spondylectomy, had a disease-free survival rate of more than 50%. Disch et al. [5] found 13 of 20 patients surviving without any evidence of disease and 17 walking without support. Kato et al. [10] studied patient and family satisfaction with en bloc total resection as a treatment for solitary spinal metastasis. Forty-five of 47 patients were satisfied with their outcome and were willing to have surgeries again if required. Thirteen patients indicated that they felt like patients without cancer.
Table 2.
Comparison of different articles published in the literature on multilevel en bloc spondylectomy
| Study | Number of resected levels | Total number of patients | Recurrence (number of patients) | Margin quality | Survival (number of patients) | Complications (number of patients) | Anterior reconstruction |
|---|---|---|---|---|---|---|---|
| Boriani et al. [1] | 2 (n = 24) 3 (n = 5) 4 (n =1) 5 (n = 2) 6 (n = 1) |
33 | 21/134 (all resections) (15.7%); no comparison given of recurrences between single and multilevel resections | Not mentioned | > 50% of patients alive without evidence of disease | Multilevel resections not significant predictors of minor complications; combined approach and multilevel resections independent predictors of major complications | Carbon cages; no failure of anterior reconstruction |
| Liljenqvist et al. [13] | 2 (n = 3) 3 (n = 1) 4 (n = 1) |
5 | 1 | 1 wide 3 marginal 1 intralesional | 2 alive with disease 2 alive without disease 1 died of disease | 1 complete paraplegia postoperatively | Expandable titanium ring cages; no cage subsidence or mechanical failures |
| Kawahara et al. [11] | 3 (n = 3) | 3 | None | Wide at all areas except intralesional at the pedicle | 1 died without evidence of disease 2 alive without evidence of disease | Transient weakness in knee extension | Moss cages with autograft; no failures |
| Disch et al. [5] | 2 (n = 7) 3 (n = 9) 4 (n = 3) 5 (n = 1) |
20 | 1 | 13 marginal 7 wide | 13 with no evidence of disease 5 alive with disease 2 alive without evidence of disease | 7 minor and 6 major; 17 patients alive and walking without any support | Carbon cages; no implant-related complications or cage subsidence |
| Our study | 2 (n = 19) 3 (n = 15) 4 (n = 3) 5 (n = 1) |
38 | 3 | 9 wide (23%) 25 marginal (65%) 4 intralesional (12%) | 31 (81%) alive without evidence of disease 3 alive with evidence of disease 2 died of disease 2 died from complications | 14 major and 22 minor in 25 patients; all living patients recovered from their complications at final followup | Carbon cages in 30; autograft and allograft only in 8; no cage-related complications |
In one study of multilevel total en bloc spondylectomy reconstructed with a carbon composite vertebral body replacement system, the authors reported no implant breakage or loosening [5]. The interconnected carbon cages showed no dislocation. There was no stress shielding or sintering at the endplate interfaces. The advantage of carbon cages is in elastic vibration to prevent stress shielding and provide radiolucency for artifact-free restaging with local MRI/CT. In our series, we had no cage-related complications. Cage subsidence was observed in two patients without any clinical significance. Only one patient required revision of pedicle screws and rods secondary to mechanical failure. Other authors have also reported no complications associated with the use of cages for anterior reconstruction [1, 2, 11, 13] (Table 2). We also used false pedicles connecting the cage anteriorly and rod posteriorly. This was mainly done to prevent the lung falling onto the dura and not for added stability.
Boriani et al. [1], in their study on morbidity of en bloc resections, noted that the combined approach and the number of resected spine segments were independent predictors of major complications, but they also noted that complications were much higher in patients with local recurrences and revision surgeries and advocated a primary, safe-margin surgery for local control (Table 2). Multilevel resections were not significant predictors of minor complications in their series. Liljenqvist et al. [13] had one patient with complete paraplegia postoperatively. Similarly, we had one patient with postoperative paraplegia. However, his lower limb power recovered to Grade 4 at final followup. Murakami et al. [16] retrospectively studied neurologic status in 79 patients after spondylectomy. None of the patients had neurologic deterioration after surgery. Disch et al. [5], in their study of 20 patients, had seven minor complications and six major complications. In our series, we had 14 major and 22 minor complications. All living patients recovered from their complications at final followup. In the literature, the majority of patients treated with multilevel en bloc spondylectomy recover from their complications [3, 6, 8, 9, 14, 20]. Multilevel en bloc resections are technically more demanding and morbid, owing to the proximity of neurovascular structures, visceral organs, need for an anterior and posterior approach, and increased blood loss and surgical time, thus increasing the risk of complications. With a multispecialty team approach (general surgeons, thoracic surgeons, vascular surgeons, plastic surgeons) and judicious preoperative assessment, complication rates could be minimized.
The sole purpose of attempting such a challenging procedure is to make the patient disease free. Achieving success is dependent on the surgical margins achieved intraoperatively. To gain wide or marginal tumor-free margins, the primary spine surgeon must have expertise and experience with these approaches. A thorough study of the MR images and CT scans to gain knowledge of tumor anatomy and surrounding structures should be carried out preoperatively to decide the approach. A total en bloc spondylectomy involving three levels or more usually requires a combined anterior–posterior approach. However, an all-posterior approach can be used in two-level resections if it does not compromise the margins achieved to reduce the morbidity. If required, the involved visceral and vascular structures should be resected en bloc with the tumor to achieve good margins. The margins we achieved were wide in nine patients (23%), marginal in 25 patients (65%), and intralesional in four patients (12%). Three of the four patients with intralesional margins had recurrence of the tumor. Disch et al. [5] achieved 13 marginal margins and seven wide margins. They had only one local recurrence. Other authors have also had minimal to no recurrences when the margins achieved were wide or marginal [1, 3, 6, 8, 9, 13, 14, 20].
In conclusion, in patients with multisegmental spinal tumors, safe oncologic resections can be achieved by multilevel total en bloc spondylectomy, with reasonable mid-term survival rates and local control. The morbidity associated with this procedure and high complication rate should not prevent an experienced surgeon from offering this surgery when indicated, as the majority of patients recover from their complications. Reconstruction of the spine is feasible with minimal implant failures if the biomechanics of the spine are respected. Although the surgical procedure is challenging, our encouraging results favor and validate this technique.
Electronic supplementary material
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at IRCCS Istituto Ortopedico Galeazzi, Milan, Italy.
References
- 1.Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F, Gasbarrini A. Morbidity of en bloc resections in the spine. Eur Spine J. 2009;19:231–241. doi: 10.1007/s00586-009-1137-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boriani S, Biagini R, De Iure F, Bertoni F, Malaguti M, Di Fiore M, Zanoni A. En bloc resections of bone tumors of the thoracolumbar spine: a preliminary report on 29 patients. Spine (Phila Pa 1976). 1996;21:1927–1931. [DOI] [PubMed]
- 3.Chanplakorn P, Chanplakorn N, Pongtippan A, Jaovisidha S, Laohacharoensombat W. Recurrent epithelioid sarcoma in the thoracic spine successfully treated with multilevel total en bloc spondylectomy. Eur Spine J. 2011;20:S302–S308. doi: 10.1007/s00586-011-1723-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chi JH, Sciubba DM, Rhines LD, Gokaslan ZL. Surgery for primary vertebral tumors: en bloc versus intralesional resection. Neurosurg Clin N Am. 2008;19:111–117. doi: 10.1016/j.nec.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Disch AC, Schaser KD, Melcher I, Feraboli F, Schmoelz W, Druschel C, Luzzati A. Oncosurgical results of multilevel thoracolumbar en-bloc spondylectomy and reconstruction with a carbon composite vertebral body replacement system. Spine (Phila Pa 1976). 2011;36:E647–E655. [DOI] [PubMed]
- 6.Druschel C, Disch AC, Melcher I, Engelhardt T, Luzzati A, Haas NP, Schaser KD. Surgical management of recurrent thoracolumbar spinal sarcoma with 4-level total en bloc spondylectomy: description of technique and report of two cases. Eur Spine J. 2012;21:1–9. doi: 10.1007/s00586-011-1859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. 1980. Clin Orthop Relat Res. 2003;415:4–18. doi: 10.1097/01.blo.0000093891.12372.0f. [DOI] [PubMed] [Google Scholar]
- 8.Hardes J, Gosheger G, Halm H, Winkelmann W, Liljenqvist U. Three-level en bloc spondylectomy for desmoplastic fibroma of the thoracic spine. Spine (Phila Pa 1976). 2003;28:E169–E172. [DOI] [PubMed]
- 9.Kato S, Kawahara N, Murakami H, Demura S, Shirai T, Tsuchiya H, Tomita K. Multi-level total en bloc spondylectomy for solitary lumbar metastasis of myxoid liposarcoma. Orthopedics. 2010;33:446. doi: 10.3928/01477447-20100429-33. [DOI] [PubMed] [Google Scholar]
- 10.Kato S, Murakami H, Demura S, Yoshioka K, Ota T, Shinmura K, Yokogawa N, Kawahara N, Tomita K, Tsuchiya H. Patient and family satisfaction with en bloc total resection as a treatment for solitary spinal metastasis. Orthopedics. 2013;36:e1424–e1430. doi: 10.3928/01477447-20131021-27. [DOI] [PubMed] [Google Scholar]
- 11.Kawahara N, Tomita K, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors: surgical techniques and related basic background. Orthop Clin N Am. 2009;40:47–63. doi: 10.1016/j.ocl.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Krepler P, Windhager R, Bretschneider W, Toma CD, Kotz R. Total vertebrectomy for primary malignant tumours of the spine. J Bone Joint Surg Br. 2002;84:712–715. doi: 10.1302/0301-620X.84B5.12684. [DOI] [PubMed] [Google Scholar]
- 13.Liljenqvist U, Lerner T, Halm H, Buerger H, Gosheger G, Winkelmann W. En bloc spondylectomy in malignant tumors of the spine. Eur Spine J. 2008;17:600–609. doi: 10.1007/s00586-008-0599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsumoto M, Ishii K, Takaishi H, Nakamura M, Morioka H, Chiba K, Takahata T, Toyama Y. Extensive total spondylectomy for recurrent giant cell tumor in the thoracic spine. J Neurosurg Spine. 2007;6:600–605. doi: 10.3171/spi.2007.6.6.15. [DOI] [PubMed] [Google Scholar]
- 15.Melcher I, Disch AC, Khodadadyan-Klostermann C, Tohtz S, Smolny M, Stöckle U, Haas NP, Schaser KD. Primary malignant bone tumors and solitary metastases of the thoracolumbar spine: results by management with total en bloc spondylectomy. Eur Spine J. 2007;16:1193–1202. doi: 10.1007/s00586-006-0295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Tomita K. Neurological function after total en bloc spondylectomy for thoracic spinal tumors. J Neurosurg Spine. 2010;12:253–256. doi: 10.3171/2009.9.SPINE09506. [DOI] [PubMed] [Google Scholar]
- 17.Roy-Camille R, Saillant G, Bisserie M, Judet T, Hautefort E, Mamoudy P. Total excision of thoracic vertebrae (author’s transl) [in French] Rev Chir Orthop Reparatrice Appar Mot. 1981;67:421–430. [PubMed] [Google Scholar]
- 18.Ruggieri P, Bosco G, Pala E, Errani C, Mercuri M. Local recurrence, survival and function after total femur resection and megaprosthetic reconstruction for bone sarcomas. Clin Orthop Relat Res. 2010;468:2860–2866. doi: 10.1007/s11999-010-1476-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakaura H, Hosono N, Mukai Y, Ishii T, Yonenobu K, Yoshikawa H. Outcome of total en bloc spondylectomy for solitary metastasis of the thoracolumbar spine. J Spinal Disord Tech. 2004;17:297–300. doi: 10.1097/01.bsd.0000096269.75373.9b. [DOI] [PubMed] [Google Scholar]
- 20.Samartzis D, Marco RA, Benjamin R, Vaporciyan A, Rhines LD. Multilevel en bloc spondylectomy and chest wall excision via simultaneous anterior and posterior approach for Ewing sarcoma. Spine (Phila Pa 1976). 2005;30:831–837. [DOI] [PubMed]
- 21.Stener B. Total spondylectomy in chondrosarcoma arising from the seventh thoracic vertebra. J Bone Joint Surg Br. 1971;53:288–295. [PubMed] [Google Scholar]
- 22.Tokuhashi Y, Matsuzaki H, Toriyama S, Kawano H, Ohsaka S. Scoring system for the preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 1990;15:1110–1113. [DOI] [PubMed]
- 23.Tomita K, Kawahara N, Baba H, Tsuchiya H, Nagata S, Toribatake Y. Total en bloc spondylectomy for solitary spinal metastases. Int Orthop. 1994;18:291–298. doi: 10.1007/BF00180229. [DOI] [PubMed] [Google Scholar]
- 24.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26:298–306. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.