Abstract
Background
Diabetes and hip fractures in geriatric patients are common, and many elderly patients have a history of diabetes. However, the influence of diabetes on surgical complications may vary based on which particular type of diabetes a patient has. To our knowledge, no prior study has stratified patients with diabetes to compare patients with noninsulin-dependent and insulin-dependent diabetes regarding rates of postoperative adverse events, length of hospitalization, and readmission rate after surgical stabilization of hip fractures in geriatric patients.
Questions/purposes
We asked whether patients with noninsulin-dependent or insulin-dependent diabetes are at increased risk (1) of sustaining an aggregated serious adverse event, aggregated minor adverse event, extended length of stay, or hospital readmission within 30 days of hip fracture surgery; (2) of experiencing any individual serious adverse event within 30 days of hip fracture surgery; and (3) of experiencing any individual minor adverse event within 30 days of hip fracture surgery.
Methods
Patients older than 65 years undergoing surgery for hip fracture between 2005 and 2012 were identified (n = 9938) from the American College of Surgeons National Surgical Quality Improvement Program® database. This database reports events within 30 days of the surgery. Demographics were compared between three groups of patients: patients with noninsulin-dependent diabetes, patients with insulin-dependent diabetes, and patients without diabetes. Patients without diabetes served as the reference group, and the relative risks for aggregated serious adverse events, aggregated minor adverse events, length of stay greater than 9 days, and readmission within 30 days were calculated for patients with noninsulin-dependent and with insulin-dependent diabetes. We then calculated relative risks for each specific serious adverse event and minor adverse event using multivariate analyses.
Results
Patients with noninsulin-dependent and insulin-dependent diabetes were at no greater risk of sustaining an aggregated serious adverse event, aggregated minor adverse event, extended postoperative length of stay, or readmission. Among individual serious adverse events, only postoperative myocardial infarction was found to be increased in the diabetic groups (relative risk [RR] = 1.9 for noninsulin-dependent diabetes, 95% CI, 1.3–2.8; RR = 1.5 for insulin-dependent diabetes, CI, 0.9–2.6; p = 0.003). Patients with noninsulin-dependent and insulin-dependent diabetes were at no greater risk of sustaining any individual minor adverse event.
Conclusions
Despite previously reported and perceived risks associated with diabetes, we found little difference in terms of perioperative risk among geriatric patients with hip fracture with noninsulin-dependent or insulin-dependent diabetes relative to patients without diabetes. Clinically, the implications of these findings will help to improve, specify, and increase the efficiency of the preoperative workup and counseling of patients with diabetes who need hip fracture surgery.
Level of Evidence
Level III, case-control study. See Instructions for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3945-7) contains supplementary material, which is available to authorized users.
Introduction
Diabetes mellitus is a widespread, chronic disease that is estimated to affect greater than 300 million people worldwide, including between 5% to 13% of the US population [4, 6, 24, 27]. The global disease burden of diabetes is expected to surpass 550 million people by 2030 [27].
By necessity, a disease of such prevalence becomes relevant to the care of all patients who may be diagnosed with it, including elderly patients undergoing operative repair of hip fractures. It has been estimated that as much as 21% of US adults older than 65 years are affected by diabetes [19]. A previous study showed that Types I and II diabetes are associated with an increase in hip fracture risk in males and females [13]. Furthermore, it also was reported that hip fracture risk is increased in patients with diabetes compared with patients without diabetes for a given age and bone mineral density or for a given WHO Fracture Risk Algorithm (FRAX) score [23].
Previous studies evaluating diabetes and operative stabilization of hip fractures have shown an increased risk of postoperative cardiac complications [10, 22], renal dysfunction [10, 17], urinary retention [1], extended length of hospital stay [22], and hospital readmission within 28 days [14]. Although all valuable contributions, many of these investigations were limited by small sample sizes, restriction to a single-hospital system, or lack of postdischarge followup. Moreover, no prior study to our knowledge has further stratified patients with diabetes to evaluate the association of noninsulin-dependent and insulin-dependent diabetes on rates of postoperative outcomes after surgical stabilization of hip fractures in elderly patients.
We therefore asked: (1) Are patients with noninsulin-dependent or insulin-dependent diabetes at increased risk of sustaining an aggregated serious adverse event, aggregated minor adverse event, extended length of stay, or hospital readmission within 30 days of hip fracture surgery? (2) Are patients with noninsulin-dependent or insulin-dependent diabetes at increased risk of experiencing any individual serious adverse event within 30 days of hip fracture surgery? (3) Are patients with noninsulin-dependent or insulin-dependent diabetes at increased risk of experiencing any individual minor adverse event within 30 days of hip fracture surgery?
Patients and Methods
Study Design and Setting
In the current retrospective case-control study, we used the American College of Surgeons National Surgical Quality Improvement Program® (ACS-NSQIP®) database to identify patients who underwent operative stabilization of a hip fracture by an orthopaedic surgeon between 2005 and 2012. The ACS-NSQIP® is a surgical database that collects patient data from greater than 350 US hospitals [2]. More than 150 distinct patient variables are extracted from the medical records, operative reports, and followup interviews of patients. These patients are prospectively identified and randomly sampled from eligible hospitals in a manner designed by the ACS-NSQIP® to minimize selection bias. Data collection occurs for each patient’s entire 30-day postoperative period, regardless of the date of discharge after surgery [2, 15].
Participants and Study Subjects
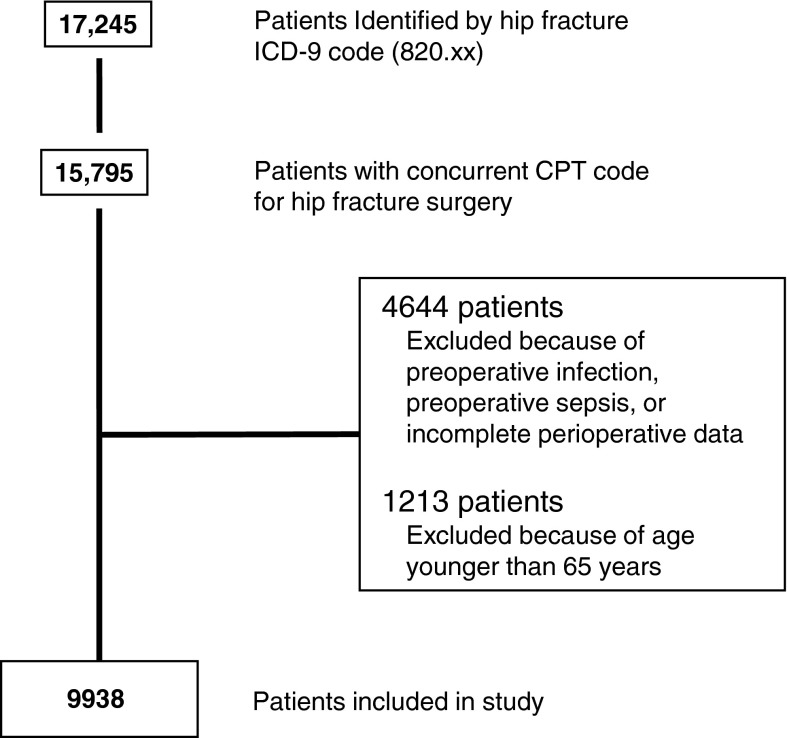
Patient data were extracted from the ACS-NSQIP® database using ICD-9 and Current Procedural Terminology (CPT) codes. All patients with hip fracture (ICD-9 code 820.xx) initially were identified (n = 17,245). From these patients, 15,795 patients (91.6%) were isolated whose records had an associated surgical procedure CPT code of 27125, 27130, 27235, 27236, 27244, or 27245 (Table 1). Four thousand six hundred forty-four patients with evidence of preoperative infection, preoperative sepsis, or who had incomplete perioperative data were excluded. Because the mechanism of sustaining a hip fracture is distinct in younger cohorts compared with elderly patients [12, 16], 1213 individuals younger than 65 years were excluded to ensure a more homogenous population of hip fractures. We therefore included 9938 patients in our study (Fig. 1).
Table 1.
CPT codes for surgical procedures associated with hip fracture
| CPT code | CPT code cescription |
|---|---|
| 27125 | Partial hip replacement with or without bipolar prosthesis |
| 27130 | Total hip replacement |
| 27235 | Percutaneous treatment of femoral fracture |
| 27236 | Open treatment of femoral fracture, proximal end, neck, internal fixation or prosthetic replacement |
| 27244 | Treatment of intertrochanteric, peritrochanteric, or subtrochanteric femoral fracture; with plate/screw type implant, with or without cerclage |
| 27245 | Treatment of intertrochanteric, peritrochanteric, or subtrochanteric femoral fracture; with intramedullary implant, with or without interlocking screws and/or cerclage |
CPT – Current Procedural Terminology.
Fig. 1.
A flow diagram shows patient selection and exclusions for the current study.
Variables, Outcome Measures, Data Sources, and Bias
Demographic variables were extracted from the ACS-NSQIP® database, and these included the age, sex, smoking status (an individual who is or was a smoker within the preceding year), and functional status of each patient. Patient functional status is a measure of the ability to complete activities of daily living (ADLs) during the 30 days before surgery. The ACS-NSQIP® definition of an independent patient is one who does not require assistance for any ADLs, whereas a partially dependent patient requires assistance for some ADLs, and a totally dependent patient requires assistance in completing all ADLs. In the current study, patients deemed either partially or totally dependent were combined to generate one designation of “dependent functional status.”
The “diabetes” variable in the ACS-NSQIP® categorizes patients into one of three groups: “Insulin” (those who use insulin to control their diabetes), “Non-Insulin” (those who use noninsulin pharmacologic methods to control their diabetes), or “None.” This final category is composed of patients who either have no history of diabetes or currently are using only diet modifications to control their diabetes. Throughout the remainder of the study, this final group is referred to as patients without diabetes. The ACS-NSQIP® does not allow for additional stratification based on level of diabetes control, such as hemoglobin A1c or admission blood glucose.
To better assess the comorbidity burden of patients in the study, the Charlson comorbidity index was used to calculate a comorbidity score for each patient [5]. The Charlson comorbidity index had to be modified to fit the data available in the ACS-NSQIP®. This sort of modification has been used before with the database [3, 9] and is similar in efficacy to the original Charlson comorbidity index [7, 26]. The methods used for establishing the modified Charlson comorbidity index are well established (Appendix 1. Supplemental material is available with the online version of CORR®).
In addition to demographics and comorbidities, the ACS-NSQIP® database also documents postoperative adverse events that occur within 30 days after surgery (Appendix 2. Supplemental material is available with the online version of CORR®). Pulmonary embolism and deep vein thrombosis were grouped together as a thromboembolic event in the current study. Similarly, superficial wound infection, deep wound infection, and organ space infection were combined as a wound-related infection. As a point of clarification, an organ space infection is defined by the ACS-NSQIP® as “any infection that appears to be related to the operation and involves any part of the anatomy (eg, organs or spaces), other than the incision, which was opened or manipulated during an operation” [1]. Adverse events with no occurrences were dropped from the analysis.
Serious and Minor Adverse Events
Adverse events were further grouped in two composite categories of serious adverse event and minor adverse event for aggregate analysis. An aggregated serious adverse event occurred if any of the following occurred: death, sepsis, septic shock, stroke or cerebrovascular accident, coma, cardiac arrest, myocardial infarction, renal failure, unplanned intubation, ventilator-assisted respiration for greater than 48 hours, thromboembolic event, wound-related infection, or return to the operating room. An aggregated minor adverse event occurred if a patient experienced a wound dehiscence, renal insufficiency, urinary tract infection, or pneumonia.
Length of Stay
The ACS-NSQIP® database documents each patient’s postoperative length of stay, recorded as the number of calendar days from the day of surgery until the day of discharge. In the current analysis, an extended length of stay was defined as any stay that was longer than the 90th percentile of all patient hospital stays, which for this population was any hospital stay longer than 9 days.
Readmission
The ACS-NSQIP® database began collecting patient readmission data in 2011 [2]. This variable was included in the current analysis for the available years of 2011 and 2012. The ACS-NSQIP® defines readmission as any admission, whether to the same or a different hospital, for any reason within 30 days after surgery.
Statistical Analyses and Study Size
Statistical Analyses
Statistical analyses were performed using Stata® Version 11.2 (StataCorp, LP, College Station, TX, USA).
First, patient demographics were evaluated. Pearson’s chi-square test was used to compare demographics between patients without diabetes mellitus and those with noninsulin-dependent diabetes, between patients without diabetes and with insulin-dependent diabetes, and finally between patients with noninsulin-dependent diabetes and with insulin-dependent diabetes.
Second, the primary hypothesis was evaluated. The risks of sustaining an aggregated serious adverse event, aggregated minor adverse event, extended length of stay, or hospital readmission after surgical stabilization of a hip fracture were tested among patients without diabetes, patients with noninsulin-dependent diabetes, and those with insulin-dependent diabetes using Poisson regression with robust error variance [28]. A statistical difference was established at a two-sided α level of 0.05 (p < 0.05).
Finally, the secondary and tertiary hypotheses were tested. The risks of sustaining each adverse event in the serious adverse event category were tested among patients without diabetes, patients with noninsulin-dependent diabetes, and those with insulin-dependent diabetes. The same testing then was performed for each adverse event in the minor adverse event category. Because these analyses involved multiple comparisons, a Bonferroni correction was used to show a more appropriate p value for detection of statistical significance [8]. A statistical difference for each test was set at a two-sided α level of 0.0042 (p < 0.0042) for adverse events in the serious adverse event category (12 comparisons) and 0.0167 (p < 0.0167) for adverse events in the minor adverse event category (three comparisons).
All mentioned comparisons were performed using multivariate analyses that controlled for the demographics and comorbidities of age (continuous), sex, modified Charlson comorbidity index score (0–4, 5, 6, ≥ 7), smoking status, functional status before surgery (independent or dependent), and procedure type (percutaneous fixation, hemiarthroplasty, total arthroplasty, plate/screw fixation, intramedullary implant) to appropriately adjust for potential confounding variables.
Poisson regression with robust error variance was used as an alternative to logistic regression. This was done so that the strengths of association could be reported as relative risks [28]. Although odds ratios often are used in cohort and cross-sectional studies, it has been established that the use of relative risk is more appropriate when the outcome being tested is not rare. When this is the case, the “rare disease assumption” that the odds ratio approximates relative risk no longer is valid [11, 20]. The use of relative risk enables a more accurate statistical comparison of risks in such cases.
Demographics, Description of Study Population
Compared with patients without diabetes, those with noninsulin-dependent diabetes were older, were less often female, and had a different distribution of modified Charlson comorbidity index (all p < 0.001; Table 2). Compared with patients without diabetes, those with insulin-dependent diabetes were older (p < 0.001), were less often female (p < 0.001), had a different distribution of modified Charlson comorbidity index (p < 0.001), and were more likely to have a dependent functional status (p = 0.033). Compared with patients with noninsulin-dependent diabetes, patients with insulin-dependent diabetes were younger (p < 0.001) but did not differ in any other demographic category.
Table 2.
Demographics of patients with hip fracture surgery
| Variable | Without diabetes | Noninsulin-dependent diabetes | Insulin-dependent diabetes | Comparisons | |||||
|---|---|---|---|---|---|---|---|---|---|
| Without diabetes with noninsulin-dependent diabetes | Without diabetes with insulin-dependent diabetes | Noninsulin-dependent with insulin-dependent diabetes | |||||||
| Number | Percent | Number | Percent | Number | Percent | p value | p value | p value | |
| 8208 | 100% | 1089 | 100% | 641 | 100% | ||||
| Age (years) | < 0.001 | < 0.001 | < 0.001 | ||||||
| 65–69 | 497 | 6% | 93 | 8% | 70 | 11% | |||
| 70–74 | 674 | 8% | 108 | 10% | 115 | 18% | |||
| 75–79 | 1090 | 13% | 194 | 18% | 103 | 16% | |||
| 80–84 | 1750 | 21% | 236 | 22% | 157 | 25% | |||
| 85–89 | 2131 | 26% | 292 | 27% | 130 | 20% | |||
| 90+ | 2066 | 25% | 166 | 15% | 66 | 10% | |||
| Gender | < 0.001 | < 0.001 | 0.117 | ||||||
| Female | 6076 | 74% | 745 | 68% | 415 | 65% | |||
| Male | 2132 | 26% | 344 | 32% | 226 | 35% | |||
| Charlson comorbidity index | < 0.001 | < 0.001 | 0.161 | ||||||
| ≤ 4 | 1812 | 22% | 306 | 28% | 183 | 28% | |||
| 5 | 3285 | 40% | 451 | 41% | 235 | 37% | |||
| 6 | 2423 | 30% | 234 | 22% | 151 | 24% | |||
| ≥ 7 | 688 | 8% | 98 | 9% | 72 | 11% | |||
| Current smoker | 0.832 | 0.217 | 0.237 | ||||||
| No | 7530 | 92% | 997 | 92% | 597 | 93% | |||
| Yes | 678 | 8% | 92 | 8% | 44 | 7% | |||
| Functional status | 0.336 | 0.033 | 0.264 | ||||||
| Independent | 5561 | 68% | 722 | 66% | 408 | 64% | |||
| Dependent | 2647 | 32% | 367 | 34% | 233 | 36% | |||
| Procedure | 0.316 | 0.220 | 0.387 | ||||||
| Percutaneous fixation | 397 | 5% | 61 | 6% | 34 | 5% | |||
| Hemiarthroplasty | 3902 | 47% | 485 | 44% | 286 | 45% | |||
| Total arthroplasty | 341 | 4% | 43 | 4% | 25 | 4% | |||
| Plate/screw fixation | 1300 | 16% | 189 | 17% | 91 | 14% | |||
| Intramedullary implant | 2268 | 28% | 311 | 29% | 205 | 32% | |||
Statistical significance was set at a two-sided α level of 0.05 (p < 0.05).
Accounting for All Patients and Study Subjects
Patient Characteristics
In total, 9938 patients older than 65 years who underwent hip fracture surgery between 2005 and 2012 were isolated from the ACS-NSQIP® database. Of these, 8208 were patients without diabetes mellitus (83%), 1089 (11%) had noninsulin-dependent diabetes, and 641 (6%) had insulin-dependent diabetes.
Results
With patients without diabetes as the reference, patients with noninsulin-dependent and with insulin-dependent diabetes were found to have no greater risk of sustaining a serious adverse event (RR = 1.1 [95% CI, 0.9–1.3], RR = 1.2 [95% CI, 1.0–1.4], p = 0.140), minor adverse event (RR = 1.2 [95% CI, 1.0–1.4], RR = 1.2 [95% CI, 0.9–1.5], p = 0.096), extended length of stay (RR = 1.1 [95% CI, 0.9–1.3], RR = 1.1 [95% CI, 0.9–1.4], p = 0.650), or hospital readmission within 30 days (RR = 1.4 [95% CI, 1.0–2.0], RR = 1.4 [95% CI, 0.9–2.2], p = 0.055) (Table 3). Taking into account the serious adverse event rate of 13.2% among patients without diabetes and 14.1% among patients with noninsulin-dependent diabetes, a level of significance of α = 0.05, and sample sizes of 8208 patients without diabetes and 1089 patients with noninsulin-dependent diabetes, a two-sided power analysis showed that the study has 99% power to detect a 5-percentage point difference in the rate of serious adverse events between patients without diabetes and patients with noninsulin-dependent diabetes (hypothetical rate of serious adverse events of 18.2% among patients without diabetes). An equivalent power analysis between patients without diabetes and patients with insulin-dependent diabetes (sample size 641 patients; serious adverse event rate of 16.2%) showed our study has 92% power to detect a 5-percentage point difference in rates of serious adverse events, again amounting to a serious adverse event rate of 18.2% among patients without diabetes. Respectively, identical power analyses were run for minor adverse events (99% power for noninsulin-dependent diabetes; 97% insulin-dependent diabetes), extended length of stay (99% power, 97% power), and readmission (99% power, 99% power).
Table 3.
Multivariate* analyses of postoperative outcomes
| Primary hypotheses | Without diabetes | Noninsulin-dependent diabetes mellitus | Insulin-dependent diabetes mellitus | p value‡ | |||
|---|---|---|---|---|---|---|---|
| Percent | Relative risk | Percent | Relative risk (95% CI) | Percent | Relative risk (95% CI) | ||
| Serious adverse event | 13% | Reference | 14% | 1.1 (0.9–1.3) | 16% | 1.2 (1.0–1.4) | 0.140 |
| Minor adverse event | 9% | Reference | 11% | 1.2 (1.0–1.4) | 10% | 1.2 (0.9–1.5) | 0.096 |
| Extended length of stay (> 9 days) | 9% | Reference | 10% | 1.1 (0.9–1.3) | 10% | 1.1 (0.9–1.4) | 0.650 |
| Readmission† | 5% | Reference | 7% | 1.4 (1.0–2.0) | 7% | 1.4 (0.9–2.2) | 0.055 |
* Final multivariate analysis controlled for all variables in Table 1; ‡statistical significance set at two-sided α level of 0.05 (p < 0.05); †readmission data available only for 2011–2012.
With multivariate analyses controlling for demographics and comorbidities, the only individual serious adverse event for which patients with noninsulin-dependent and with insulin-dependent diabetes who had hip fracture surgery were at increased risk was myocardial infarction (compared with patients without diabetes) (Table 4). Patients with noninsulin-dependent diabetes were at 1.9 times the risk (95% CI, 1.3–2.8) of patients without diabetes, whereas patients with insulin-dependent diabetes were at 1.5 times the risk (95% CI, 0.9–2.6; p = 0.003). With the numbers available, we found no differences between patients with diabetes and those without in terms of death, sepsis, septic shock, stroke or cerebrovascular accident, coma, cardiac arrest, renal failure, unplanned intubation, ventilator-assisted respiration for more than 48 hours, thromboembolic event, wound-related infection, or return to the operating room.
Table 4.
Multivariate* analyses of postoperative serious adverse events
| Secondary hypotheses | Without diabetes | Noninsulin-dependent diabetes mellitus | Insulin-dependent diabetes mellitus | p value | |||
|---|---|---|---|---|---|---|---|
| Percent | Relative risk | Percent | Relative risk (95% CI) | Percent | Relative risk (95% CI) | ||
| Serious adverse event | 13% | Reference | 14% | 1.1 (0.9–1.3) | 16% | 1.2 (1.0–1.4) | 0.140 |
| Death | 6% | Reference | 5% | 0.9 (0.7–1.2) | 6% | 1.0 (0.7–1.4) | 0.840 |
| Sepsis | 2% | Reference | 2% | 1.2 (0.8–2.0) | 2% | 1.1 (0.6–2.1) | 0.664 |
| Septic shock | 0.7% | Reference | 0.6% | 0.9 (0.4–2.0) | 0.6% | 0.8 (0.3–2.2) | 0.878 |
| Stroke/cerebrovascular accident | 0.6% | Reference | 0.9% | 2.0 (1.0–3.9) | 0.5% | 1.1 (0.3–3.6) | 0.155 |
| Cardiac arrest | 0.6% | Reference | 0.9% | 1.4 (0.7–2.8) | 2% | 2.0 (1.0–3.8) | 0.104 |
| Myocardial infarction | 2% | Reference | 3% | 1.9 (1.3–2.8) | 2% | 1.5 (0.9–2.6) | 0.003‡ |
| Renal failure | 0.4% | Reference | 0.5% | 1.2 (0.5–3.0) | 0.8% | 1.8 (0.6–4.9) | 0.572 |
| Unplanned intubation | 1% | Reference | 2% | 1.3 (0.8–2.2) | 3% | 1.9 (1.1–3.3) | 0.035 |
| On ventilator > 48 hours | 0.5% | Reference | 0.6% | 1.0 (0.4–2.2) | 1% | 1.9 (0.8–4.4) | 0.268 |
| Thromboembolic event (pulmonary embolism/deep vein thrombosis) | 2% | Reference | 0.8% | 0.5 (0.2–0.9) | 2% | 1.3 (0.8–2.1) | 0.048 |
| Wound-related infection | 1% | Reference | 2% | 1.6 (1.0–2.5) | 2% | 1.3 (0.7–2.4) | 0.156 |
| Return to operating room | 3% | Reference | 3% | 1.0 (0.7–1.5) | 3% | 1.3 (0.8–2.0) | 0.549 |
* Final multivariate analysis controlled for all variables shown in Table 1; ‡after Bonferroni correction, statistical significance was set at two-sided α level of 0.0042 (p < 0.0042).
Patients with noninsulin-dependent diabetes and insulin-dependent diabetes were found to have no greater risk of any individual minor adverse events such as wound dehiscence, renal insufficiency, urinary tract infection, or pneumonia after surgical stabilization of a hip fracture (Table 5).
Table 5.
Multivariate* analyses of postoperative minor adverse events
| Secondary hypotheses | Without diabetes | Noninsulin-dependent diabetes mellitus | Insulin-dependent diabetes mellitus | ||||
|---|---|---|---|---|---|---|---|
| Percent | Relative risk | Percent | Relative risk (95% CI) | Percent | Relative risk (95% CI) | p value‡ | |
| Minor adverse event | 9% | Reference | 11% | 1.2 (1.0–1.4) | 10% | 1.2 (0.9–1.5) | 0.096 |
| Renal insufficiency | 0.3% | Reference | 0.6% | 1.8 (0.7–4.4) | 0.8% | 2.4 (0.9–6.4) | 0.134 |
| Urinary tract infection | 6% | Reference | 7% | 1.2 (0.9–1.5) | 7% | 1.3 (0.9–1.7) | 0.203 |
| Pneumonia | 3% | Reference | 4% | 1.4 (1.0–1.9) | 3% | 0.9 (0.6–1.5) | 0.090 |
* Final multivariate analysis controlled for all variables shown in Table 1; ‡after Bonferroni correction, statistical significance was set at a two-sided α level of 0.0167 (p < 0.0167).
Discussion
Diabetes mellitus is a common chronic disease that has been identified as a risk factor for sustaining a hip fracture in elderly patients [4, 13, 23, 27]. However, to our knowledge, no previous studies have stratified patients with diabetes to evaluate the association of noninsulin-dependent and insulin-dependent diabetes on rates of postoperative complications, lengths of stay, or readmissions after surgical stabilization of elderly patients with hip fractures. Therefore, we aimed to find differences in rates of aggregated serious adverse events, aggregated minor adverse events, extended length of stay, and readmission rates between patients with noninsulin-dependent and with insulin-dependent diabetes relative to patients without diabetes mellitus.
Our study has three primary limitations. First, the classification of patients with diabetes in the ACS-NSQIP® database does not follow the more common designation of Type I versus Type II diabetes, but instead is constrained to whether a patient uses insulin or noninsulin pharmacologic methods for diabetes control. Hemoglobin A1c values or other measurements of perioperative glucose control also are not available in the database. Accordingly, the designation of noninsulin-dependent diabetes or insulin-dependent diabetes is the best available surrogate measure of the severity of a patient’s diabetes. This designation will not capture as much heterogeneity in the population with diabetes as would a hemoglobin A1c value. Although the value of hemoglobin A1c in predicting risk of postoperative events has yet to be determined, recent data indicate a correlation between elevated hemoglobin A1c and increased risk of infection and wound complications after joint arthroplasty [25]. This level of granularity is unavailable in our analysis owing to the data source and is a limitation of the study. Second, the ACS-NSQIP® database collects patient data for 30 postoperative days, so it would not capture any adverse events that occurred beyond this time. However, many national databases do not provide any followup subsequent to patient discharge, so the 30 days of followup documented by ACS-NSQIP® is a comparative benefit of the database. Even so, 30 days probably is not sufficient to identify late, deep infections, which is a complication that patients with diabetes may be more susceptible. Studies of other designs will have to resolve that important unanswered question. Finally, ACS-NSQIP® is a general surgical database and thus does not track any orthopaedic-specific outcomes that may be of interest, such as functional scores or pain improvement after surgery. Nevertheless, many important perioperative outcomes can be evaluated in orthopaedic patients with the ACS-NSQIP® database.
The results of our study are consistent with those of a previous study that found diabetes made no difference in the functional outcome and rehabilitation of patients with diabetes after hip fracture surgery [21]. An additional study determined that patients with diabetes were at increased risk of cardiac complications and pressure ulcers after hip fracture surgery, but no greater risk of thromboembolic, wound, or respiratory complications [22]. Furthermore, another study determined there was no difference in any postoperative complication between patients with diabetes and those without at 4 and 12 months followup [10]. It was not until 24 months after hip fracture surgery that an increased risk of congestive heart failure and renal failure in patients with diabetes was detected. Both studies [10, 22] are consistent with the findings of our study. The only differences were an increased risk of pressure ulcers and increased congestive heart failure and renal failure at 24 months followup, comparisons that were unavailable to us owing to specifics of the ACS-NSQIP® database. Finally, the findings of our study are in contrast to those of some studies that have associated diabetes with an increased risk of renal complications, readmission, and mortality after hip fracture surgery [1, 14, 17]. However, as an example, the study that identified an increased risk of kidney disease in patients with diabetes used an increase of 0.3 mg/dL in creatinine as criteria for postoperative kidney disease. In contrast, the ACS-NSQIP® database defined postoperative renal insufficiency as an increase of 2 mg/dL in creatinine compared with baseline and renal failure as a new need for dialysis after surgery. It is evident that the definitions of each variable are divergent among studies and may account for the differences in findings. Similarly, the study that determined an increase in readmission rate associated with patients with diabetes was complicated by dissimilar study groups for comparison [14]. The group that was readmitted had a statistically significant difference in the procedure performed and the rate of patients discharged to a skilled nursing facility. Each of these differences in study groups potentially could bias study outcomes, particularly in a group of only 55 readmitted patients.
Separate multivariate analyses for each of 12 serious adverse events showed no differences in relative risk for either noninsulin-dependent or insulin-dependent diabetes, except for myocardial infarction. As mentioned before, one study identified an increased risk of cardiac complications, of which myocardial infarction was included, in patients with diabetes after operative stabilization of hip fractures [22]. However, no other individual adverse events showed a difference in risk between patients with diabetes and those without diabetes. Some of these findings mirror those of a previous study, as is the case with no difference in risk of return to the operating room [10], whereas others are in contrast, as is the case with an increased risk of renal failure [10]. Of particular interest is the finding that there was no increased risk of any type of infection. Although it often is considered that diabetes is associated with poor wound healing and greater risk of infection, two analyses showed no increased risk of infection in patients with diabetes undergoing surgery for hip fracture [8, 9], which is consistent with our findings.
We found no differences in relative risk for patients with noninsulin-dependent or with insulin-dependent diabetes compared with patients without diabetes for minor adverse events (renal insufficiency, urinary tract infection, and pneumonia). To our knowledge, there are no published articles detailing the difference in risk of these particular events between elderly patients with diabetes and those without diabetes after operative stabilization of a hip fracture. However, diabetes has been associated with an increased risk of urinary tract infection and pneumonia in patients undergoing total joint arthroplasty [18].
In light of the high prevalence of diabetes, it is becoming increasingly important for orthopaedic surgeons to better understand the role of diabetes in the risk of postoperative outcomes. We examined postoperative complications, reoperations, and readmissions to the hospital after surgical stabilization of elderly patients with hip fractures and showed that noninsulin-dependent and insulin-dependent diabetes conferred no greater 30-day risk of sustaining an aggregated serious adverse event, aggregated minor adverse event, extended length of stay, or readmission. On analysis of each adverse event, patients with diabetes were found not to have increased risk of any individual adverse event, except for myocardial infarction, within 30 days postoperatively.
The greatest effects of these results will be in preoperative counseling, clinician decision-making, and in future directions of research. The current results confirm that cardiac clearance for surgery is an important area of focus for a clinician during preoperative workup of patients with diabetes. However, these findings also provide an indication that surgeons may be falsely advising elderly patients with diabetes who have a hip fracture about their increased risk of additional postoperative complications. Preoperative workups might be delayed owing to the misperception of this increased risk in the population with diabetes. Implementation of the conclusions of the current study could allow for a more specific and expedited evaluation of patients with diabetes who need hip fracture surgery. Finally, some studies have shown that diabetes may not play as large a role in postoperative complications in this cohort as originally thought [10, 21]. This provides a valuable and interesting foundation for future studies to further substantiate these findings. Ideally, this would be in the form of a prospective study involving a large cohort of patients with noninsulin-dependent diabetes, insulin-dependent diabetes, and without diabetes mellitus that also documented preoperative hemoglobin A1c and blood glucose for more accurate evaluation of perioperative glucose control. Proper long-term followup and documentation, not only of surgical complications, but also of clinical orthopaedic outcomes, would best achieve the goal of clarifying the association between various severities of diabetes and postoperative complications after hip fracture surgery in elderly patients.
Electronic supplementary material
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Adunsky A, Nenaydenko O, Koren-Morag N, Puritz L, Fleissig Y, Arad M. Perioperative urinary retention, short-term functional outcome and mortality rates of elderly hip fracture patients. Geriatr Gerontol Int. 2014 Jan 12 [Epub ahead of print]. [DOI] [PubMed]
- 2.American College of Surgeons. ACS-NSQIP. User Guide for the 2012 Participant Use Data File. Available at: http://site.acsnsqip.org/wp-content/uploads/2012/03/2011-User-Guide_Final.pdf. Accessed March 9, 2014.
- 3.Bohl DD, Fu MC, Gruskay JA, Basques BA, Golinvaux NS, Grauer JN. “July effect” in elective spine surgery: analysis of the American College of Surgeons National Surgical Quality Improvement Program database. Spine (Phila Pa 1976). 2013;39:603–611. [DOI] [PubMed]
- 4.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Available at: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed March 15, 2014.
- 5.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 6.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, Williams DE, Gregg EW, Bainbridge KE, Saydah SH, Geiss LS. Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32:287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49:1429–1433. doi: 10.1016/S0895-4356(96)00271-5. [DOI] [PubMed] [Google Scholar]
- 8.Dunnett CW. A multiple comparison procedure for comparing several treatments with a control. J Am Stat Assoc. 1955;50:1096–1121. doi: 10.1080/01621459.1955.10501294. [DOI] [Google Scholar]
- 9.Ehlert BA, Nelson JT, Goettler CE, Parker FM, Bogey WM, Powell CS, Stoner MC. Examining the myth of the “July Phenomenon” in surgical patients. Surgery. 2011;150:332–338. doi: 10.1016/j.surg.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Ekstrom W, Al-Ani AN, Saaf M, Cederholm T, Ponzer S, Hedstrom M. Health related quality of life, reoperation rate and function in patients with diabetes mellitus and hip fracture: a 2 year follow-up study. Injury. 2013;44:769–775. doi: 10.1016/j.injury.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 12.Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004;86:1711–1716. doi: 10.2106/00004623-200408000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol. 2007;166:495–505. doi: 10.1093/aje/kwm106. [DOI] [PubMed] [Google Scholar]
- 14.Khan MA, Hossain FS, Dashti Z, Muthukumar N. Causes and predictors of early re-admission after surgery for a fracture of the hip. J Bone Joint Surg Br. 2012;94:690–697. doi: 10.1302/0301-620X.94B5.28933. [DOI] [PubMed] [Google Scholar]
- 15.Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, Jr, Fink AS, Mentzer RM, Jr, Neumayer L, Hammermeister K, Mosca C, Healey N, Principal Investigators of the Patient Safety in Surgery Study Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Ann Surg. 2008;248:329–336. doi: 10.1097/SLA.0b013e3181823485. [DOI] [PubMed] [Google Scholar]
- 16.Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J Orthop. 2008;42:3–12. doi: 10.4103/0019-5413.38574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macheras GA, Kateros K, Koutsostathis SD, Papadakis SA, Tsiridis E. Which patients are at risk for kidney dysfunction after hip fracture surgery? Clin Orthop Relat Res. 2013;471:3795–3802. doi: 10.1007/s11999-013-3098-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marchant MH, Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am. 2009;91:1621–1629. doi: 10.2106/JBJS.H.00116. [DOI] [PubMed] [Google Scholar]
- 19.McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. 2009;64:256–263. doi: 10.1093/gerona/gln016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 21.Mizrahi EH, Fleissig Y, Arad M, Adunsky A. Functional outcome of elderly hip fracture patients: does diabetes matter? Arch Gerontol Geriatr. 2006;43:165–173. doi: 10.1016/j.archger.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Norris R, Parker M. Diabetes mellitus and hip fracture: a study of 5966 cases. Injury. 2011;42:1313–1316. doi: 10.1016/j.injury.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, Donaldson MG, Cauley JA, Harris TB, Koster A, Womack CR, Palermo L, Black DM, Study of Osteoporotic Fractures (SOF) Research Group. Osteoporotic Fractures in Men (MrOS) Research Group. Health, Aging, and Body Composition (Health ABC) Research Group Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA. 2011;305:2184–2192. doi: 10.1001/jama.2011.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Stryker LS, Abdel MP, Morrey ME, Morrow MM, Kor DJ, Morrey BF. Elevated postoperative blood glucose and preoperative hemoglobin A1C are associated with increased wound complications following total joint arthroplasty. J Bone Joint Surg Am. 2013;95(808–814):S1–S2. doi: 10.2106/JBJS.L.00494. [DOI] [PubMed] [Google Scholar]
- 26.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 27.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 28.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.