Abstract
Background
Massive bone allografts have been used for limb salvage of bone tumor resections as an alternative to endoprostheses, although they have different outcomes and risks. There is no general consensus about when to use these alternatives, but when it is possible to save the native joints after the resection of a long bone tumor, intercalary allografts offer some advantages despite complications, such as fracture. The management and outcomes of this complication deserve more study.
Questions/purposes
The purposes of this study were to (1) analyze the fracture frequency in a group of patients treated with massive intercalary bone allografts of the femur and tibia; (2) compare the results of allografts treated with open reduction and internal fixation (ORIF) with those treated with resection and repeat allograft reconstruction; and (3) determine the likelihood that treatment of a fracture resulted in a healed intercalary reconstruction.
Methods
We reviewed patients treated with intercalary bone allografts between 1991 and 2011. During this period, patients were generally treated with intercalary allografts when after tumor resection at least 1 cm of residual epiphysis remained to allow fixation of the osteotomy junction. To obtain a homogeneous group of patients, we excluded allograft-prosthesis composites and osteoarticular and hemicylindrical intercalary allografts from this study. We analyzed the fracture rate of 135 patients reconstructed with segmental intercalary bone allografts of the lower extremities (98 femurs and 37 tibias). In patients whose grafts fractured were treated either by internal fixation or a second allograft, ORIF generally was attempted but after early failures in femur fractures, these fractures were treated with a second allograft. Using a chart review, we ascertained the frequency of osseous union, complications, and reoperations after the treatment of fractured intercalary allografts. Followup was at a mean of 101 months (range, 24–260 months); of the original 135 patients, no patient was lost to followup.
Results
At latest followup, 19 patients (14%) had an allograft fracture (16 femurs [16%] and three tibias [8%]). Six patients were treated with internal fixation and addition of autologous graft (three femurs and three tibias) and 13 patients were treated with a second intercalary allograft (13 femurs). The three patients with femoral allograft fractures treated with internal fixation and autologous grafts failed and were treated with a second allograft, whereas those patients with tibia allograft fractures treated by the same procedure healed without secondary complications. When we analyzed the 16 patients with a second intercalary allograft (13 as primary treatment of the fracture and three as secondary treatment of the fracture), five failed (31%) and were treated with resection of the allograft and reconstructed with an endoprosthesis (four patients) or an osteoarticular allograft (one patient).
Conclusions
Fractures of intercalary allografts of the tibia could successfully be treated with internal fixation and autologous iliac crest bone graft; however, this treatment failed when used for femur allograft fractures. Femoral fractures could be treated with resection and repeat allograft reconstruction, however, with a higher refracture frequency. The addition of a vascularized fibular graft in the second attempt should be considered.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Intercalary allografts of the lower extremities may be used to restore bone continuity after tumor resections or traumatic bone loss of the shaft of a long bone. Intercalary allografts are frequently used because they avoid the need to harvest large amounts of autograft and are associated with acceptable functional results when healing occurs [1, 4, 5, 10]. They have the advantage of preserving the native joints and avoiding complications associated with osteoarticular allografts such as degenerative joint disease or instability and have a lower reported infection rate (6%) [4, 5, 10].
Fracture is a major cause of failure in this type of reconstruction; however, there is no general consensus regarding the management of this complication and little information exists regarding the results of fracture treatment [4, 5]. Although most papers that analyzed allograft reconstructions described the rate of fracture [1, 6–8, 10], only few papers analyzed the management of this complication [2, 11, 12]. Those reports that have analyzed the incidence and treatment of bone allograft fractures [2, 11, 12] included not only intercalary reconstruction, but also osteoarticular and allograft-prosthetic composites, which have dissimilar biomechanical forces and implantation techniques compared with intercalary allografts. For that reason, we sought to analyze exclusively the fracture rate and outcomes of treatment of fracture in a group of intercalary allografts of the lower extremities.
The purposes of this study were to (1) analyze the fracture frequency in a group of patients treated with massive intercalary bone allografts of the femur and tibia; (2) compare the results of allografts treated with open reduction and internal fixation (ORIF) with those treated with resection and repeat allograft reconstruction; and (3) determine the likelihood that treatment of a fracture resulted in a healed intercalary reconstruction.
Patients and Methods
We retrospectively reviewed patients treated with massive bone allografts between 1991 and 2011. During this period, patients generally treated with intercalary allografts when the bone tumors were localized in the metadiaphyseal area with no or partial compromise of both epiphysis and a residual epiphysis of 1 cm or more remained after resection to allow fixation of the osteotomy junction and safe oncologic margins. During that time, we performed a total of 545 massive bone allografts in the lower extremities. To obtain a homogeneous group of patients, we excluded allograft-prosthesis composites and osteoarticular and hemicylindrical intercalary allografts from this study. This resulted in a group of 143 allografts, but eight patients died of disease before 2 years of followup, so 135 had followup available at a mean of 101 months (range, 24–260 months). No patient was lost to followup. We analyzed the fracture rate of 135 patients reconstructed with segmental intercalary bone allografts of the femoral and tibial shafts. Mean patient age at time of diagnosis was 26 years (range, 1–80 years). There were 57 females and 78 males. Ninety-eight tumors were localized in the femur and 37 in the tibia. The mean age of the donor was 36 years (range, 13–59 years); 47 donors were females and 88 males. The original diagnoses included osteosarcoma (n = 62), Ewing’s sarcoma (n = 21), chondrosarcoma (n = 11), bone metastasis (n = 8), malignant fibrohistiocytoma (n = 6), giant cell tumors (n = 5), fibrosarcoma (n = 3), aneurismal bone cyst (n = 3), fibrous dysplasia (n = 2), adamantinoma (n = 2), chondromyxoid fibroma (n = 2), liposarcoma (n = 1), osteofibrous dysplasia (n = 1), osteoblastoma (n = 1), and revision of another intercalary reconstruction (n = 7). Eighty-six patients received chemotherapy, whereas 49 did not.
The surgical procedure began with resection of the lesion, including biopsy scars with appropriate bone and soft tissue margins. After being thawed in a warm solution, a fresh deep-frozen nonirradiated allograft segment, sized to fit the bone defect, was cut to the proper length. All allograft-host junctions are made with a transverse osteotomy. Both osteotomies were fixed with internal fixation. From a total of 270 host-donor junctions, 154 were located in the diaphyseal bone and 116 in the metaphyseal bone. We used plates and screws for internal fixation in 123 junctions located at the diaphysis and in 67 for the metaphysis. We used intramedullary locked nails in 31 diaphyseal and 10 metaphyseal osteotomies. In 39 host-donor junctions, where a thin epiphyseal segment was saved, only cancellous screws were used for fixation. In the first decade of this study (1991–2001), we used dynamic compression plates (DCP), whereas in the second decade (2002–2011), we used locking compression plates (LCP) and we added a second plate to each osteotomy. However, in all cases (DCP and LCP) we performed compression of the osteotomies with the plates.
Antibiotics were administered postoperatively for a minimum of 24 hours or until the deep drains were discontinued. Patients were restricted from weightbearing for 3 to 6 months after reconstruction based on radiographic evidence of allograft healing. Followup was performed 2 weeks, 6 weeks, and 3 months after surgery, then every 3 months until 2 years, and then every 6 months. Plain radiographs and physical examination were performed at each followup.
Patients who fractured their allografts were treated one of two ways, either with ORIF or with resection of the fractured graft and repeat allograft reconstruction. During the beginning of the period in question, ORIF generally was attempted but after early failures in femur fractures, these fractures were treated with resection of the fractured graft and repeat reconstruction with a second intercalary allograft. However, ORIF was always indicated for tibia allograft fractures. When we performed ORIF, we removed the loose or broken internal fixation, we put a new plate with screws, and we added autologous iliac crest graft in the fracture site. When we opted to do a resection and repeat allografting, the technique was to remove the fractured graft and the previous internal fixation and we put a second intercalary allograft fixed in both osteotomies with plates and screws. As a result of bone host growing in the osteotomy site of the fractured allograft, the second allograft was shorter than the previous one. In those cases when originally there was only a small segment from the articular surface, the segment was longer so it facilitates the revision situation.
Using a chart review, we ascertained the frequency of osseous union, complications, and reoperations after the treatment of fractured intercalary allografts. After approval by our institution’s institutional review board, preoperative data (demographic information, including patient age, sex, affected bone, diagnosis, and age and sex of the donor) and postoperative data (local recurrence, infection, nonunion and fracture complications) were recorded.
Results
At latest followup, we identified 59 patients with complications requiring a second operation, including nine local recurrences, four deep infections, 19 fractures, and 23 nonunions. Of the 19 patients (14%) who had a fracture of the allograft, 16 fractures were located in the femur (16%) (Figs. 1, 2) and three in the tibia (8%) (Fig. 3). The mean time to fracture was 53 months after surgery (range, 15–110 months). We analyzed the fracture frequency by each decade of age of the patient, and there was no difference in fracture rate by decade of life (Table 1). When we analyzed the fracture frequency regarding the allograft donor age, we found no difference either (Table 2). When we analyzed fracture rates regarding patients’ sex, we found similar rates. There were 11 fractures in 78 males (14%) and eight fractures in 57 females (14%). When we compared the sex of the donor, there were 14 fractures in 88 male donor bones (16%) and five fractures in 47 female donor bones (10%).
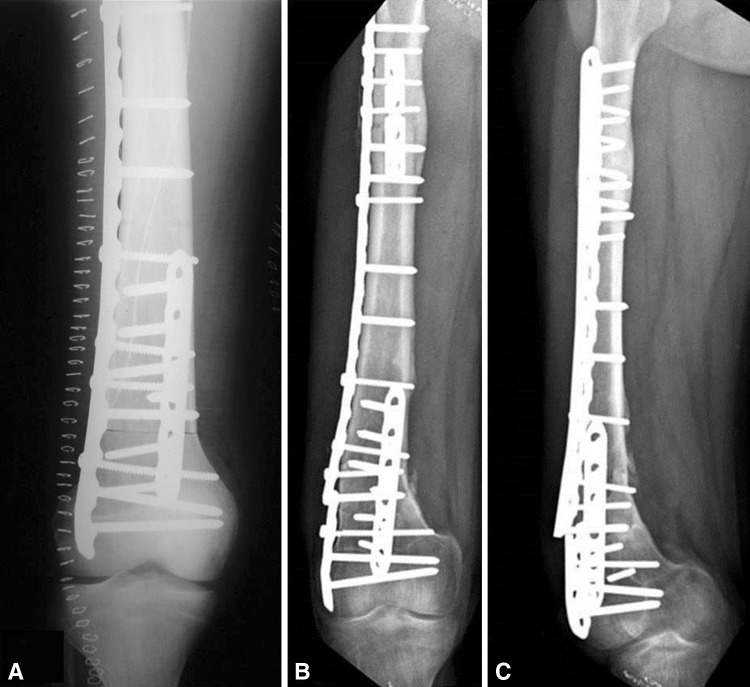
Fig. 1A–C.
Figure shows postoperative radiographs of the right femur after resection of diaphyseal osteosarcoma and reconstruction with an intercalary allograft. Fixation of the allograft to the host was performed with two short anterior plates and one long lateral plate. (A) AP radiograph of the right distal femur immediately after surgery that shows the distal osteotomy line. (B) AP radiograph of the right femur that shows breakage of the lateral plate in the distal part with fracture of the intercalary allograft 5 years after the initial operation. (C) Lateral radiograph of the right femur showing the fracture of the allograft and the hardware failure.
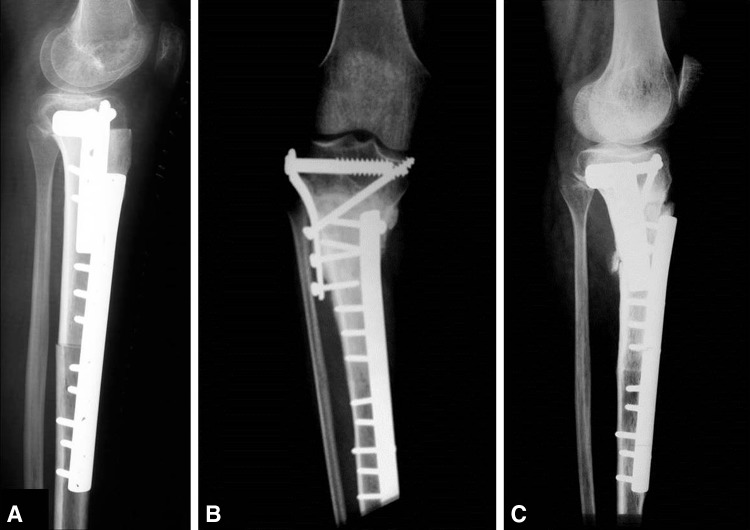
Fig. 2A–B.
AP and lateral 2-year postoperative radiographs are shown of the right femur after resection of the fractured allograft and reconstruction with a second intercalary allograft. (A) AP radiograph of the right femur showing healing of both osteotomies; a distal femur locking plate was used in the lateral side that covers both osteotomies and the addition of a short anterior plate in the proximal osteotomy. (B) Lateral radiograph of the right femur showing adequate fixation of both osteotomies.
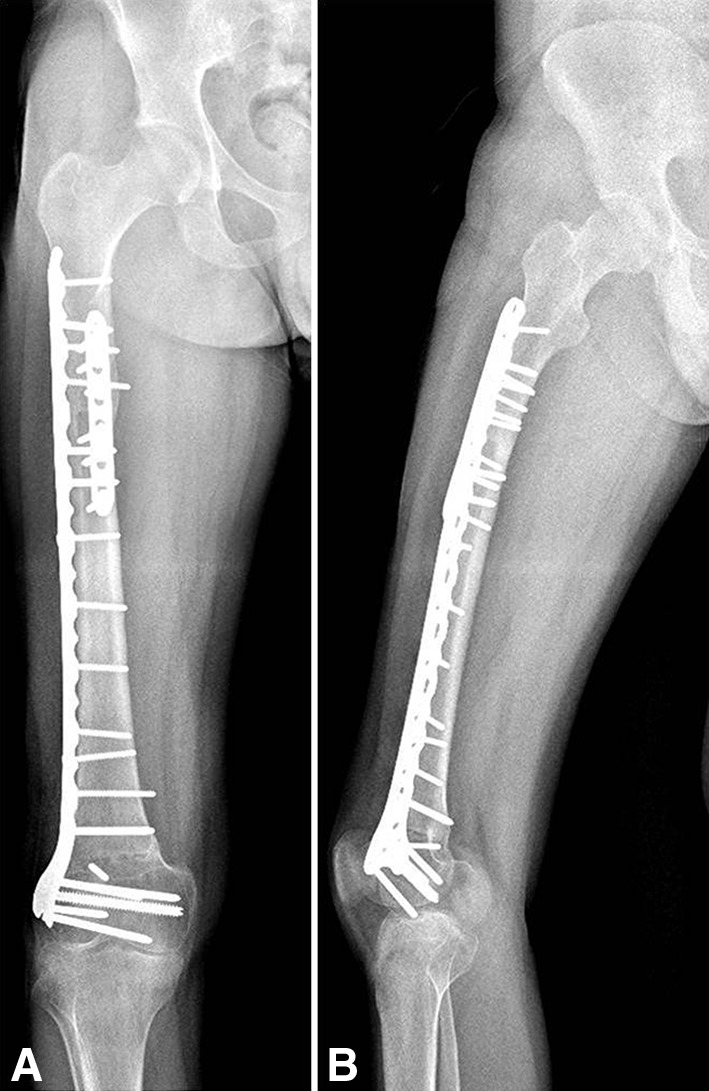
Fig. 3A–C.
Postoperative radiographs show right proximal tibia after resection of metadiaphyseal osteosarcoma and reconstruction with an intercalary tibia allograft. Fixation of the allograft to the host was performed with a lateral buttress proximal plate and a medial dynamic compression plate. (A) Lateral radiograph of the right proximal tibia immediately after surgery that shows both osteotomy lines. (B) AP radiograph of the right proximal tibia 7 years after surgery that shows fracture of the intercalary allograft with loosening of the screws of the buttress plate. (C) Lateral radiograph of the right proximal tibia showing the fracture of the tibia intercalary allograft.
Table 1.
Fracture frequency by each decade of age of the patient
| Decade of age | Number of patients | Number of fractures |
|---|---|---|
| First (1–9 years old) | 17 | 2 (12%) |
| Second (10–19 years old) | 49 | 9 (18%) |
| Third (20–29 years old) | 22 | 2 (9%) |
| Fourth (30–39 years old) | 13 | 2 (15%) |
| Fifth (40–49 years old) | 18 | 1 (5%) |
| Older (> 50 years old) | 16 | 3 (19%) |
Table 2.
Fracture frequency by each decade of age of the allograft donor
| Decade of age | Number of donors | Number of fractures |
|---|---|---|
| First (1–9 years old) | No donors | – |
| Second (10–19 years old) | 16 | 2 (12%) |
| Third (20–29 years old) | 35 | 4 (11%) |
| Fourth (30–39 years old) | 19 | 3 (15%) |
| Fifth (40–49 years old) | 34 | 4 (11%) |
| Older (> 50 years old) | 31 | 6 (19%) |
After sustaining the fracture, patients were treated by two different approaches. Six patients were treated with internal fixation and autologous iliac crest bone graft (three femurs and three tibias) maintaining the original allograft; and 13 patients were treated with resection of the allograft and reconstructed with a second intercalary allograft (13 femurs) (Fig. 2). Three of the patients with femoral allograft fractures treated with internal fixation and autologous grafts failed and were treated with resection of the allograft and reconstructed with a second intercalary allograft. The patients with a tibia allograft fracture treated with internal fixation and autogenous bone graft healed without secondary complications (Fig. 4).
Fig. 4A–B.
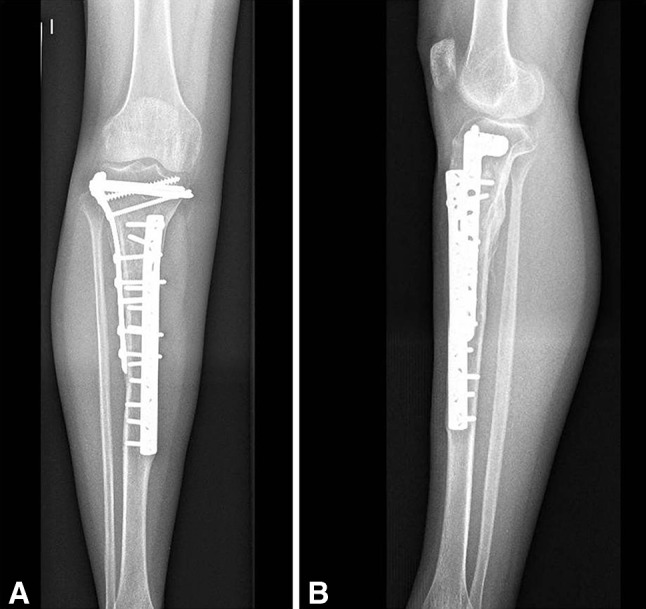
Five-year postoperative AP and lateral radiographs show the right tibia after treatment of the allograft fracture with a new lateral long plate (proximal tibia locking compression plate) and autologous graft, maintaining the original allograft and the medial plate. (A) AP radiograph of the right tibia that shows adequate healing of the allograft fracture with the new lateral long plate that covers both osteotomies. (B) Lateral radiograph of the right tibia showing healing of the allograft fracture with bone formation in the posterior cortical of the tibia.
When we analyzed the 16 patients with a second intercalary allograft (13 as primary treatment of the fracture and three as secondary treatment of the fracture), five failed (31%) and were treated with resection of the allograft and reconstructed in four cases with an endoprosthesis and in the remaining case with an osteoarticular allograft.
Discussion
Intercalary bone allografts have been shown previously to have better functional results compared with osteoarticular allografts or allograft-prosthetic composites because they preserve native joints [4, 5, 10]. Fracture is the main cause of failure with this type of reconstruction. However, there is no general consensus on how to manage this complication nor is there much data on the results of treatment once a fracture occurs. We therefore studied a group of intercalary segmental massive bone allografts of the lower extremities, analyzing the fracture rate, two approaches to the management of this specific complication (ORIF and resection and repeat reconstruction with another allograft), and the union rate after this complication.
Our study has certain limitations. First, we did not analyze fractures in all type of allografts, only in segmental intercalary, so we cannot apply the findings of this study to osteoarticular or allograft-prosthesis composites. However, in this specific group of allografts, fractures were the main cause of failure as has been reported in the literature. Second, the group has some inherent heterogeneity in terms of diagnosis, chemotherapy, the amount of soft tissue resection, extension of internal fixation, amount of compression at the host-donor junction, and anatomic allograft fitting, which could affect the incidence of fracture and complications. Finally, we do not exclude intercalary allograft that failed for other reasons (such as local recurrence and infection); this suggests that our estimate of the frequency of fracture of allografts may be a low estimate.
The fracture frequency in this series was 14% and is similar to previous reports [5, 10]. Although Thompson et al [12] reported that the use of plates and screws influences the likelihood of fracture, in other reports, the use of nails had even higher fracture rates [5]. Currently, the use of rigid fixation with plates and screws is recommended in most of the publications for allograft reconstructions [4, 5, 10]. The addition of vascularized fibular graft has been recommended by some for intercalary allograft reconstruction [3, 5]. However, in a recent study, there was little difference in the fracture rate comparing allograft with and without this vascularized graft [5]. In the same study [5], protecting the allograft with intramedullary cement was not found to be significant in decreasing the allograft fracture rate. Thompson et al [12] reported an increase in the fracture rate in patients who received chemotherapy, whereas Sorger et al [11] in a larger series did not find a correlation between chemotherapy and allograft fracture. The use of massive bone allografts has a risk for infection, fracture, and nonunion [6–8]. Fracture and infection usually lead to allograft removal and a high failure rate. Infection is the main cause of failure in most series with a reported incidence of 7.9% in a large series of 945 patients [9]. In the same series, fracture rate (18%) was higher than the infection rate. These results are similar to other reports [5, 10].
The use of massive bone allografts implies the risk for fractures; however, only few papers analyze the management of this complication [2, 11, 12]. Berrey et al [2] reported in their series 22 fractures of the shaft including allograft-prosthesis composites and osteoarticular and intercalary allografts. In their series two healed without operation after a period of immobilization. Four were treated with resection of the fractured allograft and reconstructed with a secondary allograft in three and autologous iliac crest in one. The remaining 16 were treated with ORIF and autogenous bone from the iliac crest, but healing and restoration of function resulted only in six of the 16. Sorger et al [11] treated only 41 of the 185 fractures with ORIF and only half of them required only one operation. We found in our series that tibial intercalary allograft could be successfully treated with ORIF and autologous iliac crest graft. Previous series [2, 11], although they report successful in some case results with ORIF, they do not clearly state in which kind or type of fractures. However, Sorger et al [11] found a significantly worse outcome with time in patients with femoral allograft fractures than those with tibial or humeral allograft fractures.
In the present series, all femoral fractures were ultimately treated with resection of the original allograft and reconstructed with a second intercalary allograft. However, the fracture frequency for this second intercalary allograft (31%) is similar to if not higher than the primary surgery group (16%). Although Frisoni et al [5] found little difference in the fracture rate comparing allograft with and without a vascularized fibular graft, this option could be considered in those patients who should revised for fracture to avoid this complication again. In their series [5], nine femoral fractured allografts were left in place and augmented with a vascularized fibular graft and in 11, the allograft was replaced with a fresh one coupled with a vascularized fibular graft with no subsequent failure. Meanwhile, in 14 reconstructions in which the allograft was substituted with another allograft without a supplementary vascularized reconstruction, three patients had a second failure (21%). Fractures of intercalary allografts of the tibia were successfully treated with internal fixation and autologous graft; however, this treatment failed when it was used in femur allograft fractures. The lower rate for tibia fractures is also supported by previous reports [4]. This may be explained by the presence of the fibula that may diminish the loads in the allograft.
In conclusion, fractures of intercalary allografts of the tibia could successfully be treated with internal fixation and autologous iliac crest bone graft; however, this treatment failed when used for femur allograft fractures. Femoral fractures could be treated with resection and repeat allograft reconstruction, however, with a similar if not higher refracture frequency that ended in endoprosthesis or osteoarticular allograft. Based on these findings, in femoral fractures of pediatric and young adults, a second attempt at salvage of an intercalary allograft is performed, whereas in older patients, it might be preferable to proceed to endoprosthesis or osteoarticular allograft. The addition of a vascularized fibular graft in the second attempt should be considered.
Footnotes
One of the authors certifies that he (LAA-T) or she, or a member of his or her inmediate family, has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Stryker Americas (Miami, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution has approved the reporting of this case report and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aponte-Tinao L, Farfalli GL, Ritacco LE, Ayerza MA, Muscolo DL. Intercalary femur allografts are an acceptable alternative after tumor resection. Clin Orthop Relat Res. 2012;470:728–734. doi: 10.1007/s11999-011-1952-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berrey BH, Jr, Lord CF, Gebhardt MC, Mankin HJ. Fractures of allografts. Frequency, treatment, and end-results. J Bone Joint Surg Am. 1990;72:825–833. [PubMed] [Google Scholar]
- 3.Campanacci DA, Puccini S, Caff G, Beltrami G, Piccioli A, Innocenti M, Capanna R. Vascularised fibular grafts as a salvage procedure in failed intercalary reconstructions after bone tumour resection of the femur. Injury. 2013 Oct 18 [Epub ahead of print]. [DOI] [PubMed]
- 4.Farfalli GL, Aponte-Tinao L, Lopez-Millán L, Ayerza MA, Muscolo DL. Clinical and functional outcomes of tibial intercalary allografts after tumor resection. Orthopedics. 2012;35:e391–e396. doi: 10.3928/01477447-20120327-21. [DOI] [PubMed] [Google Scholar]
- 5.Frisoni T, Cevolani L, Giorgini A, Dozza B, Donati DM. Factors affecting outcome of massive intercalary bone allografts in the treatment of tumours of the femur. J Bone Joint Surg Br. 2012;94:836–841. doi: 10.1302/0301-620X.94B6.28680. [DOI] [PubMed] [Google Scholar]
- 6.Gebhardt MC, Flugstad DI, Springfield DS, Mankin HJ. The use of bone allografts for limb salvage in high-grade extremity osteosarcoma. Clin Orthop Relat Res. 1991;270:181–196. [PubMed] [Google Scholar]
- 7.Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW. Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res. 1996;324:86–97. doi: 10.1097/00003086-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Mankin HJ, Gebhardt MC, Tomford WW. The use of frozen cadaveric allografts in the management of patients with bone tumors of the extremities. Orthop Clin North Am. 1987;18:275–289. [PubMed] [Google Scholar]
- 9.Mankin HJ, Hornicek FJ, Raskin KA. Infection in massive bone allografts. Clin Orthop Relat Res. 2005;432:210–216. doi: 10.1097/01.blo.0000150371.77314.52. [DOI] [PubMed] [Google Scholar]
- 10.Muscolo DL, Ayerza MA, Aponte-Tinao L, Ranalletta M, Abalo E. Intercalary femur and tibia segmental allografts provide an acceptable alternative in reconstructing tumor resections. Clin Orthop Relat Res. 2004;426:97–102. doi: 10.1097/01.blo.0000141652.93178.10. [DOI] [PubMed] [Google Scholar]
- 11.Sorger JI, Hornicek FJ, Zavatta M, Menzner JP, Gebhardt MC, Tomford WW, Mankin HJ. Allograft fractures revisited. Clin Orthop Relat Res. 2001;382:66–74. doi: 10.1097/00003086-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Thompson RC, Jr, Garg A, Clohisy DR, Cheng EY. Fractures in large-segment allografts. Clin Orthop Relat Res. 2000;370:227–235. doi: 10.1097/00003086-200001000-00023. [DOI] [PubMed] [Google Scholar]