Abstract
Background: In the Democratic Republic of Congo (DRC), few studies have focused on treatment-seeking paths selected by caretakers for the management of severe childhood malaria in an urban environment. The present study aims at describing the treatment-seeking paths according to the characteristics of households, as well as the subsequent impact on pre-hospitalisation delay and malarial fatality and on the main syndromes associated with severe childhood malaria.
Methods: This descriptive study included data collected at nine hospitals in Kinshasa between January and November 2011. A total of 1,350 children, under 15 years of age and hospitalised for severe malaria, were included in the study.
Results: Regarding the management of malaria, 31.5% of households went directly to the health centre or hospital while 68.5% opted for self-medication, church and/or traditional healing therapy. The most frequent first-line option was self-medication, adopted by more than 61.5% of households. Nevertheless, rational self-medication using antimalarial drugs recommended by the WHO (artemisinin-based combinations) was reported for only 5.5% of children. Only 12.5% of households combined 2 or 3 traditional options. The following criteria influenced the choice of a modern vs. traditional path: household socioeconomic level, residential environment, maternal education level and religious beliefs. When caretakers opted for traditional healing therapy, the pre-hospitalisation delay was longer and the occurrence of respiratory distress, severe anaemia and mortality was higher.
Conclusion: The implementation of a malaria action plan in the Democratic Republic of Congo should take into account the diversity and pluralistic character of treatment-seeking behaviours in order to promote the most appropriate options (hospital and rational self-medication) and to avoid detrimental outcomes.
Keywords: treatment-seeking path, households, severe malaria, Kinshasa (DRC)
Introduction
Malaria is the first global endemic parasitic disease and its transmission has been reported in about a hundred countries worldwide [1]. Africa is, by far, the most affected continent, and 90% of malaria cases are recorded in tropical and subtropical areas [1, 2]. In the Democratic Republic of Congo (DRC), malaria is a major public health problem, a highly endemic disease that constitutes one of the three leading causes of death. Children under 5 years of age are particularly at risk and 59% of consultations and 41.7% of deaths recorded in hospitals are related to the disease and the effects of malaria are usually more severe in that population [3]. Indeed, many patients treated at hospitals are children in an advanced stage of severe malaria, having undergone several care attempts beforehand. Treatment-seeking paths are variable, and the consultation at a reference hospital is rarely the first-line choice of caretakers [4]. Numerous studies carried out in African countries have pointed out the pluralistic character of treatment-seeking behaviours and the fact that they are often characterised by a succession of stages and a combination of several options [5, 6]. In DRC, 80% of cases are managed either at home or by traditional healers [7, 8]. Nevertheless, severe malaria remains potentially fatal in the absence of rapid and appropriate care. Few studies have focused on treatment-seeking paths selected by caretakers in case of severe childhood malaria in an urban environment. The objective of the present study is to describe the treatment-seeking paths according to household characteristics as well as and the subsequent impact on pre-hospitalisation delay and malarial fatality and on the main syndromes associated with severe childhood malaria. It is essential to consider the treatment-seeking behaviour in cases of severe malaria and to note the impact on clinical forms, on pre-hospitalisation delay, on malarial fatality, and on action plans effective in reducing morbidities and fatalities.
Methods
Context of the study
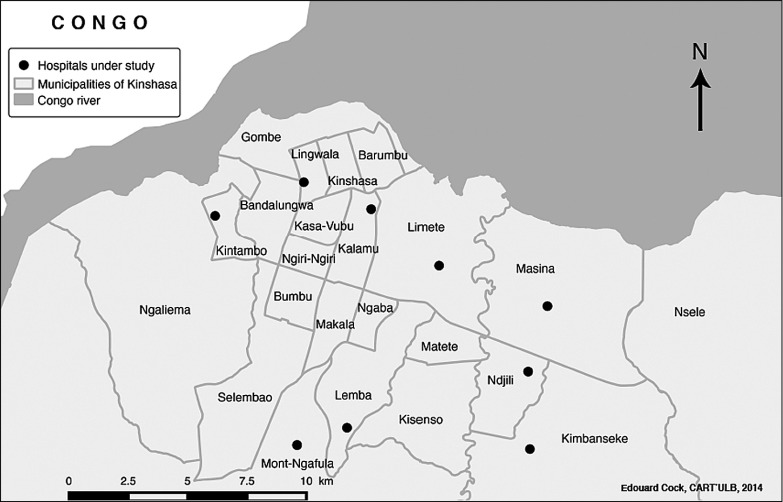
The province of Kinshasa was the framework of the study. The DRC has eleven provinces. Kinshasa is the most populated city in the country, with 9, 463, 749 inhabitants occupying a 9,965 km² area, of which more than half was strictly rural in 2012 [9]. The city is subdivided into 6 sanitary districts and 35 operational health areas. The modern health system includes public health training, private profit-seeking and private denominational sectors. Three hospitals were selected for each sector and are represented by black dots in Figure 1.
Fig. 1.
A map of Kinshasa (RDC) showing the location of the hospitals under study.
Type of study and targeted population
This descriptive study was conducted over a period of eleven months from January to November 2011. It included 1,350 hospitalised children, under 15 years of age and treated for severe malaria according to the 2000 WHO criteria [10].
Data collection
Information on affected children was extracted from medical records. Caretakers (parents/legal guardians) were questioned through a face-to-face interview which was standardised after a pre-test. Interviews were performed by previously trained students having a license in nursing sciences.
The following information was collected:
-
-Data related to the sick child: the status of the child at discharge (death or recovery), the pre-hospitalisation delay (time between the onset of first clinical signs and consultation at a health centre/hospital). The main syndromes were:
-
○Neurological clinical manifestations, characterised by a deep coma (coma with Blantyre ≤ 2 for a young child or a modified Glasgow score ≤ 9 if the child is older than 5), convulsions (≥ 2 per day) or prostration (extreme weakness).
-
○Severe anaemia, characterised by a < 15% haematocrit or a < 50 g/L haemoglobin concentration, and a >10 000/μl parasite count.
-
○Respiratory distress (acidotic breathing), characterised by a deep breathing along with an abnormal increased thorax amplitude (visualised by the degree of intercostal recession) and an increased breathing rate (tachypnoea) [11].
-
○
-
-
Household data: socioeconomic level determined by the poverty index previously developed by Foster, Greer and Thorbecke, sex of the head of household, maternal education level, paternal education level, residential environment, religious beliefs of the head of household and selected treatment-seeking path(s): (i) ‘modern’ path (health centre and hospital) and (ii) ‘traditional’ path (self-medication, traditional healing therapy and church).
Some variables were transformed for the purpose of analyses. On the basis of a previous work published within the frameworks of the “DRC demographic and health investigation” (DHI) [12], the national survey by clusters with multiple indicators (MICS-2010) [13] and the survey performed by the United Nations Development Programme (UNDP) on the profile of Kinshasa [14], the socioeconomic level was broken into three categories (low, middle and high); three groups were considered for the maternal and the paternal education level (not schooled, elementary, high school/higher education); the residential environment was divided into 2 areas (urban and peri-urban); two groups were created for religious beliefs (Catholic vs. awakening churches) and two types of treatment-seeking options were considered: “modern”, when the household directly consults the health centre or hospital, and “traditional”, when the household practices self-medication or refers to a church and/or a traditional healer.
Ethical considerations
All confidentiality and ethical rules were upheld. The study protocol and the informed consent form were approved by the Ethical Committee of the Kinshasa School of Public Health, the Medical Inspection of the City-Province of Kinshasa and the Kinshasa Provincial Ministry of Health. The study was conducted in compliance with principles set out by the International Conference on Harmonization (ICH) Good Clinical Practice (GCP) Guideline, the Declaration of Helsinki and the regulatory requirements of the DRC. Individual written informed consent was obtained from all parents or legal guardians, in the presence of an independent witness if the persons involved were illiterate (after oral explanation). Respect for anonymity was assured prior to analysis.
Statistical analyses
Descriptive statistics consisted of estimating medians, as well as 25th and 75th percentiles (P25-P75), for quantitative variables, as well as proportions for category-specific variables.
Both univariate and bivariate analyses implied performing chi-square and Mann-Whitney tests to compare household characteristics, clinical signs, pre-hospitalisation delay and malarial fatality, according to the treatment-seeking path.
In the multivariate analysis, the logistic regression allowed for the impact of therapeutic options on malarial fatality, that is, households selecting modern vs. traditional paths, as well as ≥ 1 traditional option. The maintained adjustment variables were: child age, sex, clinical aspects and household characteristics. Odds ratios and the respective confidence intervals are presented.
Data were compiled and analysed using Epi infoTM 3.5.2 and StataTM 12.0 software. A P-value below 0.05 was considered statistically significant.
Results
Description of socio-demographic characteristics, main paths and drugs used in self-medication
Table 1 provides a summary of socio-demographic characteristics, main paths, drugs used in self-medication and main syndromes associated with severe childhood malaria. Out of 1,350 children hospitalised and treated for severe malaria, 75% were under 5 years of age, and the boy/girl ratio reached 1.3. Median age (months) was statistically comparable in both groups (modern vs. traditional paths) (Me [p25–p75]: 29 [15–61], 31 [15–59] P = 0.696). More than 75% of the children hospitalized were from low and middle socioeconomic level households. Forty-five percent of mothers were not schooled vs 2.6% of fathers, and 74.9% of children were living in the peripheral area. Most children came from a male-headed household (92.9%). The main registered syndromes were: neurological form (7.9%), severe anaemia (11.4%) and respiratory distress (20.5%). The main first-line treatment options were: self-medication (61.5%), health centre/hospital (31.5%), church (6.1%) and traditional healing therapy (0.9%). In the group of children first treated by self-medication, only 5.5% received the treatment recommended by the WHO (artemisinin-based combination therapy or ACT) (Table 1).
Table 1.
Description of household socio-demographic characteristics, clinical picture, main treatment-seeking paths and drugs used for self-medication
| Parameters | n = 1,350 | % |
|---|---|---|
| Sex (boys) | 772 | 57.2 |
| Age < 5 years | 1,013 | 75.0 |
| Socioeconomic level | ||
| Low | 668 | 49.5 |
| Middle | 344 | 25.5 |
| High | 338 | 25.0 |
| Maternal education level | ||
| Not schooled | 606 | 45.0 |
| Elementary | 537 | 39.7 |
| High school and higher education | 207 | 15.3 |
| Paternal education level | ||
| Not schooled | 35 | 2.6 |
| Elementary | 321 | 23.8 |
| High school and higher education | 994 | 73.6 |
| Residential environment | ||
| Peri-urban area | 1,011 | 74.9 |
| Sex of the head of household | ||
| Male | 1,254 | 92.9 |
| Religious beliefs | ||
| Catholics | 741 | 54.9 |
| Clinical picture (n = 1,350) | ||
| Neurological (yes/no) | 107 | 7.9 |
| Severe anaemia (yes/no) | 154 | 11.4 |
| Respiratory distress (yes/no) | 277 | 20.5 |
| Main treatment-seeking paths | ||
| Self-medication | 831 | 61.5 |
| Health centre/Hospital | 425 | 31.5 |
| Churches | 82 | 6.1 |
| Traditional healing therapy | 12 | 0.9 |
| Drugs used for self-medication (n = 831) | ||
| Antypyretics | 348 | 41.9 |
| Antibiotics | 210 | 25.3 |
| Chloroquine | 3 | 0.4 |
| Artesunate-amodiaquine* | 46 | 5.5 |
| Quinine per os | 224 | 26.9 |
*Recommended by the WHO
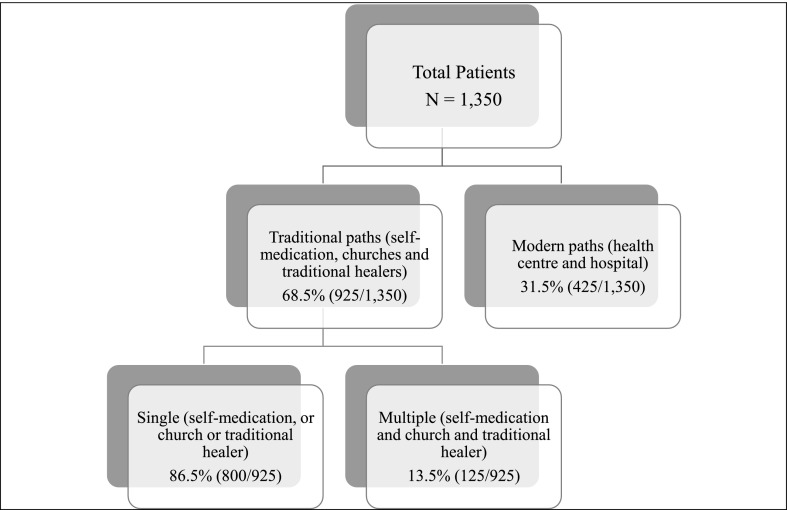
Figure 2 summarizes the treatment-seeking path for children. Out of 1,350 children hospitalised because of severe malaria, only 31.5% were directly taken to a health centre or hospital, while the rest were first treated following one or more traditional options. In the latter group, 86.5% were taken to the health centre/hospital after only one traditional option, while 13.5% arrived at the health centre/hospital after 2 or 3 traditional paths (self-medication, church and/or traditional healing therapy) (Fig. 2).
Fig. 2.
Detailed treatment-seeking paths for children.
The results presented in Table 2 show modern vs. traditional treatment-seeking paths, analysed according to household characteristics as well as the subsequent impact on pre-hospitalisation delay and malarial fatality and on the main clinical syndromes associated with severe childhood malaria. The first-line option of modern vs. traditional path was statistically different according to household socioeconomic level, maternal education level and religious beliefs. Regarding the influence of the socioeconomic level on the treatment-seeking behaviour, 51.7% of households of low socioeconomic level opted for a traditional path, compared to 23.9% and 24.4% of households of middle and high socioeconomic levels respectively. A modern path was selected by 44.7% of households with a high socioeconomic level. The difference was statistically significant (p < 0.05).
Table 2.
Modern (N = 425) vs. traditional (N = 925) treatment-seeking paths as a function of household socio-demographic characteristics, pre-hospitalisation delay, malarial fatality and the main syndromes associated with severe childhood malaria
| Parameters | Type of resort | P-values† | |
|---|---|---|---|
| Modern | Traditional | ||
| N (%) | N (%) | ||
| Socioeconomic level | 0.045 | ||
| Low | 190 (26.4) | 478 (51.7) | |
| Middle | 123 (28.9) | 221 (23.9) | |
| High | 112 (44.7) | 226 (24.4) | |
| Maternal education level | 0.012 | ||
| Not schooled | 9 (2.1) | 26 (2.8) | |
| Elementary | 92 (21.7) | 229 (24.8) | |
| High school and higher education | 324 (76.2) | 670 (72.4) | |
| Paternal education level | 0.447 | ||
| Not schooled | 213 (12.0) | 393 (42.5) | |
| Elementary | 161 (37.9) | 376 (40.7) | |
| High school and higher education | 51 (50.1) | 156 (16.8) | |
| Residential environment | 0.128 | ||
| Peri-urban area | 307 (72.2) | 704 (76.1) | |
| Urban area | 118 (27.8) | 221 (23.8) | |
| Sex of the head of household | 0.960 | ||
| Male | 395 (93.0) | 859 (92.9) | |
| Female | 30 (7.0) | 66 (7.1) | |
| Religious beliefs | 0.002 | ||
| Catholics | 259 (60.9) | 482 (47.8) | |
| Awakening churches | 166 (39.1) | 443 (52.1) | |
| Clinical picture | |||
| Neurological (yes/no) | 34 (8.0) | 73 (7.9) | 0.946 |
| Severe anaemia (yes/no) | 31 (7.3) | 123 (13.3) | 0.001 |
| Respiratory distress (yes/no) | 71 (16.7) | 206 (22.3) | 0.019 |
| Pre-hospitalisation delay (days) | |||
| Me (P25-P75) | 2.0 (1–6) | 5.0 (3–7) | < 0.001 |
| Malarial fatality | |||
| Crude OR (95% IC) | 1 | 19.5 (4.7–79.6) | < 0.001 |
| Adjusted OR (95% IC) | 1 | 20.7 (5.1–84.9) | < 0.001 |
†: Mann-Whitney test or Chi-squared test.
The mothers of 50.1% of children whose caretaker(s) opted for a modern path were educated. On the contrary, mothers of 42.5% of children whose caretaker(s) opted for a traditional path were not educated and 40.7% had reached only the elementary school level. Catholics selected modern paths (60.9%) more often than the other religions (52.1%).
The occurrence of the main clinical syndromes, pre-hospital delay and malarial fatality depended on the first-line options (Table 2). Children who first went through a traditional path presented a significantly higher occurrence of respiratory distress (22.3%) and severe anaemia (13.3%) compared to children directly treated at a health centre/hospital (16.7% of respiratory distress and 7.3% of severe anaemia, respectively). The pre-hospitalisation delay was significantly shorter for the children of the latter group (2 days vs. 5 days for the indirect treatment-seeking path, p < 0.05). Malarial fatality differed significantly for both categories of treatment-seeking behaviours (modern vs. traditional): the bivariate analysis revealed a 19.5 fold higher risk of fatality for children who first went through a traditional path. This observation was confirmed by the multiple regression, adjusted for age, socio-demographic and child’s clinical picture (aOR = 20.7 [5.1–84.9], as shown in Table 2).
Regarding traditional paths, a comparison of “single” vs. “multiple” options was performed, considering household characteristics, clinical syndromes, and their impact on the pre-hospitalisation delay and malarial fatality (Table 3). This analysis revealed a statistically significant difference between the two groups, according to the socioeconomic level, residential environment and main clinical syndromes (respiratory distress). The “multiple traditional path” was twice as frequent in the group of children from poor households (58.4%). With regard to the residential environment, multiple paths were statistically more frequent among children from the city outskirts (86.4%).
Table 3.
Number of traditional treatment-seeking paths: single (N = 800) vs. multiple (N = 125) according to household socio-demographic characteristics, pre-hospitalisation delay, malarial fatality and the main syndromes associated with severe childhood malaria
| Parameters | Number of itineraries | P-values† | |
|---|---|---|---|
| Single | Multiple | ||
| N (%) | N (%) | ||
| Socioeconomic level | 0.035 | ||
| Low | 405 (50.6) | 73 (58.4) | |
| Middle | 188 (23.5) | 33 (26.4) | |
| High | 207 (25.9) | 19 (15.2) | |
| Maternal education level | 0.447 | ||
| Not schooled | 343 (42.8) | 50 (40.0) | |
| Elementary | 327 (40.9) | 49 (39.2) | |
| High school and higher education | 130 (16.3) | 26 (20.8) | |
| Paternal education level | — | ||
| Not schooled | 20 (2.5) | 6 (4.8) | |
| Elementary | 200 (25.0) | 29 (23.2) | |
| High school and higher education | 580 (72.5) | 90 (72.0) | |
| Residential environment | 0.004 | ||
| Peri-urban area | 596 (74.5) | 108 (86.4) | |
| Urban area | 204 (25.5) | 17 (13.6) | |
| Sex of the head of household | 0.976 | ||
| Male | 743 (92.9) | 116 (92.8) | |
| Female | 57 (7.1) | 9 (7.2) | |
| Religious beliefs | 0.546 | ||
| Catholics | 420 (52.5) | 62 (49.6) | |
| Awakening churches | 380 (47.5) | 63 (50.4) | |
| Clinical picture | |||
| Neurological (yes/no) | 66 (8.3) | 7 (5.6) | 0.307 |
| Severe anaemia (yes/no) | 101 (12.6) | 22 (17.6) | 0.128 |
| Respiratory distress (yes/no) | 188 (23.5) | 18 (14.4) | 0.028 |
| Pre-hospitalisation delay (days) | |||
| Me (P25-P75) | 5.0 (3–7) | 5.0 (3–8) | 0.067 |
| Malarial fatality | |||
| Crude OR (95% IC) | 1.6(0.7–3.6) | 1 | 0.225 |
| Adjusted OR (95% IC) | 1.7(0.8–3.9) | 1 | 0.166 |
†: Mann-Whitney test or Chi-squared test.
The occurrence of respiratory distress was significantly more frequent in the group of children taking by a single path (23.5%) vs. multiple paths (14.4%). No significant difference was observed between single and multiple traditional paths for maternal education level, paternal education level, sex of the head of household, religious beliefs, development of the neurological form, observation of severe anaemia, pre-hospitalisation delay or malarial fatality (Table 3).
Discussion
The present study describes treatment-seeking paths in the management of severe malaria for children under 15 years of age, according to household characteristics, pre-hospitalisation delay, clinical syndromes and malarial fatality. Out of 1,350 children included in the study, 925 (68.5%) were treated in a health centre/hospital after several other treatment attempts (self-medication, church and/or traditional healing therapy). Only 31.5% of children went directly to a health centre/hospital (as a first-line action), which is close to the 24% estimated in Cameroon by Commeyras et al [15]. Our results highlighted the fact that traditional treatment-seeking paths are variable. Self-medication was the most frequent traditional option in our study (> 50% of children). Obvious evidence of self-medication has been observed in other African capitals over the past several years including Ivory Coast [16], Senegal (Northern District of Dakar) [17], Nigeria [18] and Southern of Ethiopia [19]. These studies showed that, in case of malarial fever, self-medication was practiced by more than 70% of families as the first-line therapeutic response to malaria before any other treatment-seeking path, findings consistent with our results. In the present study, we found that, as far as self-medication was concerned, only 5.5% of children received artesunate-amodiaquine, one of the drugs recommended by the WHO [20]. Our results confirm the estimations reported previously in other African countries: only 5% and 8% of children under 5 years of age received an Artemisinin-based Combination Treatment (ACT) for the treatment of malaria in Burkina Faso and Mali, respectively [21, 22]. A lack of parental knowledge and insufficient community awareness could be responsible for the poor choice of treatment. It is essential to alert the public to the risk of irrational self-medication, so that every child can receive the appropriate treatment recommended by the WHO.
Besides self-medication, prayer and faith in church was mentioned as another traditional option. Through the norms, values and practices it advocates, religion is liable to influence the perceptions and attitudes of individuals regarding treatment-seeking behaviour. The religious impact on treatment-seeking behaviour may depend on the group involved [23]. According to our results, 6.1% of households turned to church as a first-line treatment-seeking path. Our results are similar to the findings of other authors [4, 16, 24] asserting that households opted for church and traditional healers because they assumed exogenous causes (evil spirits, witches or fetishes) were responsible for their child’s disease.
The present study identified few caretakers turning to traditional healing therapy (treatment of malaria by herbal remedies consisting of one or multiple plants). Such a low proportion can be explained by the reluctance of parents to admit that option, because they are afraid to be “ostracized” by society. This might be seen as a declaration bias related to the environment of the study (hospital) or to the fact that students in nursing sciences led the interviews. Houéto [25] and William [26] reported the same observations. Indeed, turning to healers was rarely mentioned in their study, and the status of the investigator (health agent at the same time) could have bothered the people interviewed.
In the present study, only one child out of three was directly treated in a modern health care structure. Nevertheless, other African studies have identified the health centre as a first-line option (Far ahead of self-medication) [27–30] because mothers are well aware of the severe signs of childhood malaria. Household characteristics strongly influences the treatment-seeking path (modern vs. traditional). A clear difference was observed according to the socioeconomic level, the maternal education level and the religious affiliation of the head of household. Poor households showed a marked difference from households with a middle and high socioeconomic level in that their first-line treatment-seeking behaviour consisted of turning to traditional paths, while children of households with a high socioeconomic level were more frequently treated directly at a health centre/hospital. Our observations corroborate the conclusions of other authors [6, 15, 31] who reported that high socioeconomic level households directly select modern health structures more often. The more resources a household has, the more access it has to modern health care. The fact that low income-families were included in the present study explains the low frequency of modern treatment-seeking options and the preference for alternative solutions such as self-medication. However, another study focusing on this theme reached contradicting conclusions: Baxerres [32] suggested that the economic situation proper to each family was not the principal determinant of treatment-seeking behaviour. At first, families tend to spend a minimum amount of money and to manage their child’s health at home, whatever their level of income. Furthermore, Ishaga showed that, all other things beside, it is easier for people living in an urban area to enjoy modern health care than to turn to church or unconventional medicine [6]. Regarding clinical signs, pre-hospitalisation delay and malarial fatality, our results show a more frequent occurrence of respiratory distress, severe anaemia and malarial fatality in children first treated through traditional paths. The pre-hospitalisation delay was also longer in this group of children.
The analysis of therapeutic pluralism and household characteristics revealed a difference among children according to socioeconomic level and residential environment. Children from poor households and those living in peri-urban areas were more likely to be treated by a combination of traditional paths (2 to 3) before visiting a health centre/hospital. Our observations confirm the previous findings of Médah who reported a multiple treatment-seeking path in the poorest population in Burkina Faso [4]. Nevertheless, random treatment-seeking behaviours may be risky and this parameter should not be neglected when planning an action programme against malaria.
Limitations of the study
The present study only focused on children hospitalised for severe malaria and involved a limited number of hospitals. Mild childhood malaria was not considered. Young patients who could not treat at the hospital for some reason were not included in the study either. The memory of caretakers (parents/legal guardians) regarding the onset of clinical signs may have been faulty. The involvement of spiritual or traditional healers might have been left out as a function of the severity of the disease upon admission of the child. The plants used by traditional healers to cure severe malaria could not be identified in the present study.
Conclusion
The present study concludes that, in DRC, treatment-seeking paths are multiple in case of severe malaria. Few children are directly treated at a health centre or hospital in cases of severe malaria. Self-medication remains the main traditional treatment-seeking path. The socioeconomic level, the maternal education level and religious beliefs strongly influence the treatment-seeking behaviour. Self-medication remains the most frequent first-line option, but it rarely relies on the rational use of drugs recommended by the WHO. Multiple treatment-seeking paths are favoured, not only at low and middle socioeconomic levels, but also according to the residential environment (peri-urban area). Choosing the wrong path exerts serious consequences on clinical signs and evolving aspects of the disease in children in terms of pre-hospitalisation delay, fatality, respiratory distress and anaemia (which are less frequent when children are directly treated at modern health facilities such as a health centre or a hospital). The management of cases remains an essential component of action plans against malaria and demands an early diagnosis and a prompt initiation of treatment with effective antimalarial drugs.
Conflict of Interest
This work is the fruit of the main author’s personal efforts, without any financial support but with the help of other authors as supervisors. All authors confirm the absence of any conflict of interest.
Acknowledgements
We acknowledge the contributions of Eléonore Wolff and Eduard Cock for helping us compile the map of Kinshasa showing the location of the hospitals under study. We gratefully acknowledge the important revisions suggested by an anonymous reviewer.
References
- 1.Wold Health Organisation. Wold malaria report 2013. Available: http://www.who.int/malaria/publications/world_malaria_report_2013/report/en/ [Accessed 23 August 2014]
- 2.Rowe AK, Rowe SY, Snow RW, et al. The burden of malaria mortality among African children in the year 2000. Int J Epidemiol 2006; 35(3): 691–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.School of Public Health (ESP), National Programme of Fight against Malaria (PNLP), Global Fund. Investigation report on the assessment of the current level of basis indicators of ‘fight against malaria’ in 15 health areas of intervention of the World Funds Project in Democratic Republic of Congo. Kinshasa: University of Kinshasa; 2006. pp 80 [in french]. [Google Scholar]
- 4.Médah R. Sociological approach of health care offer and demand, the example of injections in the city of Ouagadougou (Burkina Faso). Etude Recit no 11, Ouagadougou: Laboratoire Citoyennetés; 2006. pp 22 [in French]. [Google Scholar]
- 5.Sy I, Keita M, Ould Taleb M, et al. Health care utilization in Nouakchott (Mauritania): spatial inequalities or social sluggishness? Sante 2010; 1: 51–58 [in French]. [DOI] [PubMed] [Google Scholar]
- 6.Ishaga C, Keita B, Kuepi M. Determining factors of the therapeutic resort in Mali: between sociocultural, economical and geographical accessibility factors. Population et développement en Afrique 2010; 2: 147–176 [in French]. [Google Scholar]
- 7.Wembonyama S, Mpaka S, Tshilolo L. Medicine and health in the Democratic Republic of Congo: from Independence to the Third Republic. Med Trop (Mars) 2007; 67(5): 447–457. [PubMed] [Google Scholar]
- 8.Mulumba MP. Situation of malaria in the Democratic Republic of Congo. Congo Médical Congo Médical 2002; 3: 431–435 [in French]. [Google Scholar]
- 9.Congo Democraatic Republic of the Demographics Profile. 2012. Available: http://www.axl.cefan.ulaval.ca/afrique/czaire.htm [Accessed 23 August 2014].
- 10.[No author listed] Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg 2000: S1–S90. [PubMed] [Google Scholar]
- 11.Roca-Feltrer A, Carneiro I, Armstrong Schellenberg JR. Estimates of the burden of malaria morbidity in Africa in children under the age of 5 years. Trop Med Int Health 2008; 13(6): 771–783. [DOI] [PubMed] [Google Scholar]
- 12.Ministry of Plan and Ministry of Health. Demographic and health survey; Democratic Republic of Congo. 2007. [in French]. [Google Scholar]
- 13.Ministry of Plan, National Statistics Office and United Nations International Children’s Emergency Fund. Multiple indicators Cluster survey, Democratic Republic of Congo. 2010: pp 291 [in French]. [Google Scholar]
- 14.United Nations Development Programme. Unit of fight against poverty, profile of the province of Kinshasa, RDC. 2004 [in French]. [Google Scholar]
- 15.Commeyras C, Ndo J, Merabet O, et al. Household behaviour regarding health and drug consumption in Cameroon. Sante 2006; 16: 5–12 [in French]. [PubMed] [Google Scholar]
- 16.Dossou-Yovo J, Amalaman K, Carnevale P. Antimalarial guidelines and therapy practices of the population of Bouake, Ivory Coast. Med Trop (Mars) 2001; 61(6): 495–499. [PubMed] [Google Scholar]
- 17.Ndiaye P, Tal-Dia A, Diedhiou A, et al. Self-treatment of fever in the northern district of Dakar, Senegal. Med Trop (Mars) 2006; 66(1): 74–78. [PubMed] [Google Scholar]
- 18.Omolase C, Adeleke O, Afolabi A, et al. Self-medication amongst general outpatients in a Nigerian community hospital. An Ib Postgrad Med 2007; 5: 64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deressa W, Ali A, Enqusellassie F. Self-treatment of malaria in rural communities, Butajira, southern Ethiopia. Bull World Health Organ 2003; 81(4): 261–268. [PMC free article] [PubMed] [Google Scholar]
- 20.Wold Organisation Health. Guidelines for the treatment of malaria. Geneva 2010. Available: http://www.who.int/malaria/publications/atoz/mal_treatchild_revised.pdf [Accessed 10 February 2014].
- 21.National Institute of Statistics and Demography and International ICF. Demographic and health survey and multiple indicators of Burkina Faso 2010. Calverton, Maryland, USA: INSD and ICF International; 2012. pp 525 [in French]. [Google Scholar]
- 22.National Programme of Fight against Malaria (PNLP), INFO.-STAT and ICFMacro. Prevalence survey of malarial anaemia and parasitaemia in children (EA&P) in Mali. Calverton, Maryland, USA: CPS/DNSI and ICF Macro; 2010. [in French]. [Google Scholar]
- 23.Akoto E, Kouame A, Samson B. To take care of oneself today, in Western Africa: therapeutic pluralism between tradition and modernity (Benin, Ivory Coast and Mali). les cahiers de l’Iford 2002; 27: 157–165 [in French]. [Google Scholar]
- 24.Kiniffo IR, Agbo-ola L, Issifou S, et al. Mothers of children under 5 years old and malaria in Dangbo Vally, South-East of Benin. Médecine d’Afrique Noire 2000; 47: 27–33 [in French]. [Google Scholar]
- 25.Houéto D, d’Hoore W, Ouendo EM, et al. Childhood fever in a zone of malaria prevalence in Benin: qualitative analysis of factors linked to seeking care. Sante Publique 2007; 19(5): 363–372. [DOI] [PubMed] [Google Scholar]
- 26.Williams H, Jones CO. A critical review of behavioral issues related to malaria control in sub-Saharan Africa: what contributions have social scientists made? Soc Sci Med 2004; 59(3): 501–523. [DOI] [PubMed] [Google Scholar]
- 27.Faye O, Lo M, Diop B, et al. Knowledge and treatment of malaria in rural Senegal. Med Trop (Mars) 1997; 57: 161–164. [PubMed] [Google Scholar]
- 28.Talani P, Samba G, Moyen G. Management of child fever in the battle against malaria in Brazzaville. Bull Soc Pathol Exot 2002; 95(1): 47–49. [PubMed] [Google Scholar]
- 29.Jombo G, Araoye M, Damen J. Malaria self-medications and choices of drugs for its treatment among residents of a malaria endemic community in West Africa. Asian Pacific Journal of Tropical Disease 2011: 10–16. [Google Scholar]
- 30.Tarimo DS, Lwihula GK, Minjas JN, et al. Mothers’ perceptions and knowledge on childhood malaria in the holendemic Kibaha district, Tanzania: implications for malaria control and the IMCI strategy. Trop Med Int Health 2000; 5(3): 179–184. [DOI] [PubMed] [Google Scholar]
- 31.Worrall E, Basu S, Hanson K. Is malaria a disease of poverty? A review of the literature. Trop Med Int Health 2005; 10(10): 1047–1059. [DOI] [PubMed] [Google Scholar]
- 32.Baxerres C, Le Hesran J. Resort to health care in case of child fever in Sereer country, Senegal, between economic constraint and disease perception. Sciences sociales et santé 2004; 22: 5–23 [in French]. [Google Scholar]