Abstract
Aim:
To compare air nicotine levels in public places in Ahmedabad, India, before (June 2008) and after (January, 2010) the implementation of a comprehensive smoking ban which was introduced in October 2008.
Materials and Methods:
Air nicotine concentrations were measured by sampling of vapor-phase nicotine using passive monitors. In 2008 (baseline), monitors were placed for 5-7 working days in 5 hospitals, 10 restaurants, 5 schools, 5 government buildings, and 10 entertainment venues, of which 6 were hookah bars. In 2010 (follow-up), monitors were placed in 35 similar venues for the same duration.
Results:
Comparison of the overall median nicotine concentration at baseline (2008) (0.06 μg/m3 Interquartile range (IQR): 0.02-0.22) to that of follow-up (2010) (0.03 μg/m3 IQR: 0.00-0.13), reflects a significant decline (% decline = 39.7, P = 0.012) in exposure to second-hand smoke (SHS). The percent change in exposure varied by venue-type. The most significant decrease occurred in hospitals, from 0.04 μg/m3 at baseline to concentrations under the limit of detection at follow-up (%decline = 100, P < 0.001). In entertainment venues, government offices, and restaurants, decreases in SHS exposure also appeared evident. However, in hookah bars, air nicotine levels appeared to increase (P = 0.160).
Conclusion:
Overall, SHS exposure was significantly reduced in public places after the smoke-free legislation came into force. However, nicotine concentrations were still detected in most of the venues indicating imperfect compliance with the comprehensive ban.
Keywords: Air nicotine monitoring, second-hand smoke, smoke-free law, smoking ban
Introduction
Tobacco products are the leading preventable cause of death, killing around 6 million people in 2011;(1) with the majority of the burden in low- and middle-income countries.(1,2) Women and children in south Asian countries are often the victims of morbidity and mortality caused by second-hand smoke (SHS) exposure due to high male smoking prevalence.(3) SHS contains more than 7,000 chemicals and around 70 carcinogens;(4) and the relationship between SHS exposure and increased morbidity and mortality is clear.(5,6,7,8,9,10,11,12,13) There is no safe level of exposure to SHS.(4) The World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC), Article 8, mandates countries “to protect citizens from exposure to tobacco smoke in workplaces, public transport, and indoor public places.”(14) Comprehensive smoke-free laws have been shown to be effective at reducing SHS exposure, smoking prevalence, cardiovascular disease, and lung cancer incidence in many high-income countries.(15,16,17)
SHS is a major public health challenge in India with 275 million adults using a range of tobacco products.(18,19) According to the 2009-2010 Global Adult Tobacco Survey, 35% of adults over the age of 15 years in India currently use tobacco, with the prevalence of tobacco use among males being 48% and among females 20%.(20,21) Bidis(22) are the most popular form of smoked tobacco used in India, accounting for 73% of all smoking forms.(23) Bidi smoking produces more nicotine, tar, and carbon monoxide than manufactured cigarettes.(24)
India was among the first few countries to sign and ratify the WHO FCTC.(25) The Government of India enacted the comprehensive “Cigarette and Other Tobacco Products Act, 2003” (COTPA 2003) that came in enforcement from May 2004.(26) Section 4 of COTPA 2003 prohibited smoking in most public places and work places, but provided an optional separate provision for smoking areas or spaces in hotels having 30 or more rooms, in restaurants having a seating capacity of 30 or more, and in airports.(26) Despite the comprehensive law, violations appear to be extensive due to limited awareness and lack of clarity regarding enforcement mechanisms among stakeholders.(27) The Government of India revised the national smoke-free law, “prohibition of smoking in public places rules, 2008” that came in effect from 2nd October 2008 by making additional provisions to improve enforcement.(28)
The objective of this study was to compare the exposure to SHS at most commonly visited public places and work places (government offices, hospitals, education institutes, restaurants, and entertainment venues, including hookah bars) through air nicotine concentration monitoring, and to compare the smoke-free law implementation status through observational findings before (2008) and after (2010) the implementation of the revised national smoke-free law in Gujarat, India.
Materials and Methods
Study type
Cross-sectional surveys were conducted at baseline (July 2008) and after (January 2010) the implementation of revised national smoke-free law to compare the air nicotine concentrations and smoke-free law implementation status.
Study location and sampling
The study was conducted in Ahmedabad (the fifth largest city in India and former capital of the state of Gujarat situated in western India). Ahmedabad has a population of more than 5.8 million and an extended urban area population of 6.3 million.(29) To represent most commonly visited public places and work places, government offices (n = 5), hospitals (n = 5), educational institutes (n = 5), restaurants (n = 10), entertainment venues (n = 4), and hookah bars (n = 6) were identified by convenience sampling representing all six zones of the city. Most venues were the same for both surveys except for three restaurants and two hookah bars that closed following the 2008 survey. These were replaced by the selection of other similar venues in the 2010 survey. Air nicotine levels were measured and comprehensive observational sheets were completed at all venues by trained field workers.
Study protocol and nicotine measurement
SHS was estimated by passive sampling of vapor-phase nicotine using sodium bisulfate-coated filters.(30) The placement of the monitors in the room adhered to the following guidelines: Monitors should hang in the air (1-2 meters from the floor); monitors should be at least 1 meter away from an open window or a ventilation system; monitors should be at least 1 meter away from a potential regular smoker; monitors should not be placed in an area where air does not circulate; and monitors should not be too visible or accessible to avoid tampering. Blank and duplicate monitors were maintained and placed to ensure quality control. The sampling areas in the buildings were pre-specified following a consistent systematic approach aimed at minimizing bias since levels of air pollutants vary within a building. Sampler locations included common areas of the building where people congregate and spend time, along with additional areas of scientific or public interest (e.g., restrooms and cafeterias). The placement of the monitors within a building was documented using a simple diagram that also indicated the location of windows and doors. For each monitor, location and the date and time of placement and collection was recorded on a sampling sheet. All buildings were visited once during the monitoring period, and field workers verified whether the placement of the monitor was correct and noted the condition of the windows and doors, the location of the air nicotine monitor, the estimated occupancy of the building, the number of smokers observed during a 15-minute period, and the distance from the filter to the nearest smoker. At the end of the sampling period, all monitor labels were checked by the fieldwork coordinator and the monitors were then stored in a smoke-free place at room temperature before they were transported to the laboratory. Laboratory analysis was performed using gas chromatography in the laboratory at the Johns Hopkins Bloomberg School of Public Health, USA.
Other recorded information included the presence of “No Smoking” signage, the presence of the smell of smoke, the presence of cigarette/bidi butts, and any other observations that might reasonably be expected to affect SHS assessment.
In 2008, of the 132 air nicotine monitors received from 35 buildings, results from 105 monitors were reported after excluding blanks, duplicates, erroneous, and ripped monitors. Similarly in 2010, of the 123 air nicotine monitors received from 35 buildings representing the same types of venues, results from 117 monitors were reported after excluding blanks, duplicates, erroneous, and ripped monitors.
Data analysis
Given the skewed distribution of air nicotine levels, medians and interquartile ranges (IQRs) were used to describe the data. The Wilcoxon-Mann-Whitney test was used for bivariate analyses. Fisher's exact chi-square test was used for the comparison of categorical variables. Some data are presented with a further stratification of venue type. For nicotine values below the detection level (0.0073 μg/mL), half of this set value was used for analysis purposes. All the analyses were performed in Stata 12.0.
Results
At baseline (July 2008), the overall median nicotine concentration was 0.06 μg/m3 (IQR: 0.02-0.22). At follow-up (January 2010), the overall median concentration was 0.03 μg/m3 (IQR: 0.00-0.13) reflecting a significant decline (% decline = 39.7, P = 0.012) of exposure to SHS [Table 1].
Table 1.
Air nicotine concentrations (μg/m3) in public places before/baseline (July 2008) and after/follow-up (January 2010) the smoking ban (October 2008)
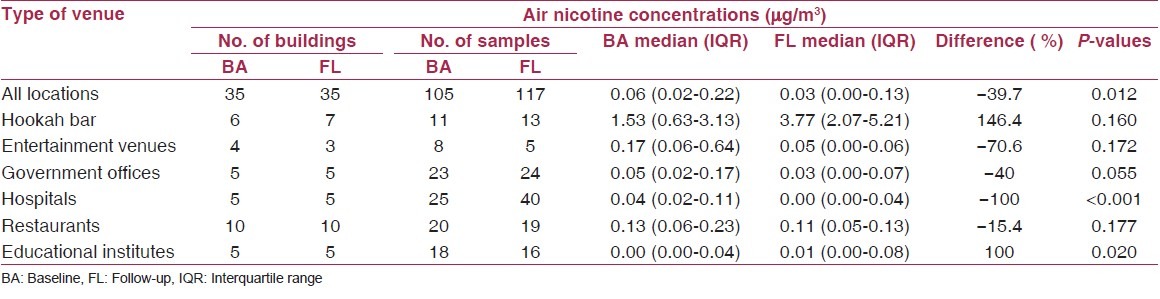
In 2008, median air nicotine concentrations were highest in hookah bars (1.53 μg/m3, IQR: 0.63-3.13), followed by entertainment venues (0.17 μg/m3, IQR: 0.06-0.64), and lowest in educational institutes (0.00 μg/m3, IQR: 0.00-0.04) which was under the detectable level [Table 1]. The percentage change from 2008 to 2010 varied by venue-type. The largest decrease of SHS occurred in hospitals, from 0.04 μg/m3 at baseline to concentrations under the limit of detection at follow-up in 2010 (% decline = 100, P < 0.001). Educational institutes, which were under the limit of detection at baseline, had detectable concentrations of air nicotine at follow-up (P = 0.020) [Table 1 and Figure 1]. In entertainment venues, government offices, and restaurants, decreases in SHS exposure also appeared evident. Air nicotine levels declined in entertainment venues, from 0.17 μg/m3 at baseline to 0.05 μg/m3 at follow-up (% decline = 70.6, P = 0.172); in government offices, from 0.05 μg/m3 at baseline to 0.03 μg/m3 at follow-up (% decline = 40, P = 0.055); and in restaurants, from 0.13 μg/m3) at baseline to 0.11 μg/m3 at follow-up (% decline = 15.4, P = 0.177). However, in hookah bars, an increase in exposure to SHS was observed, as the air nicotine levels went from 1.53 μg/m3 at baseline to 3.77 μg/m3 at follow-up (P = 0.160).
Figure 1.
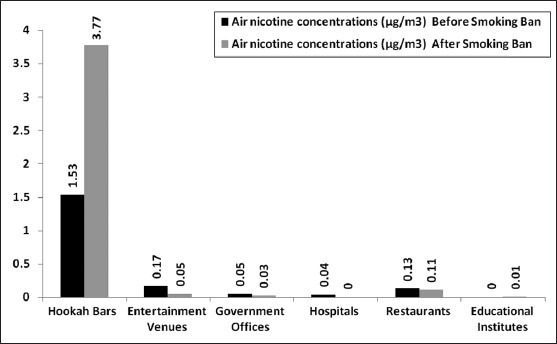
Air nicotine concentrations (μg/m3) in public places before and after the smoking ban
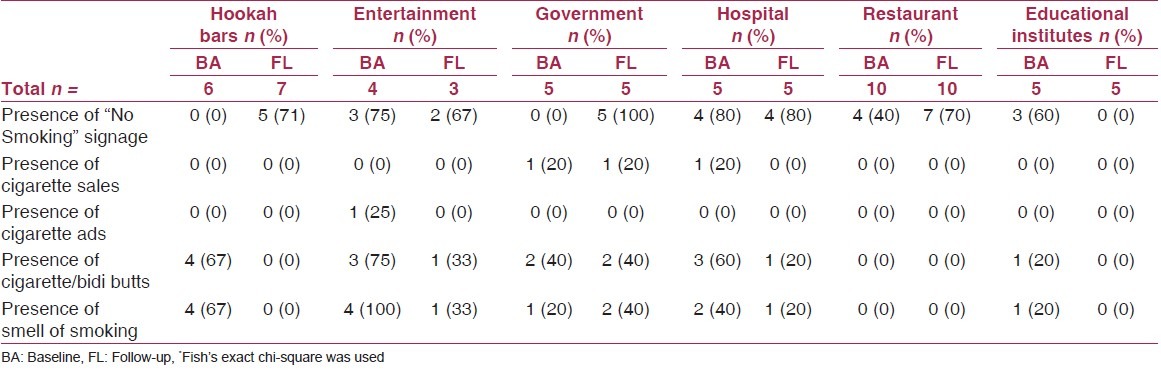
Overall, almost all the locations showed improved compliance with the law [Table 2]. For example, a significant improvement in the presence of “No Smoking” signage was observed at the smoking restricted areas of hookah bars (from no signage at baseline to 70% presence of signage at follow-up) and government offices (from no signage at baseline to 100% presence of signage at follow-up). However, “No Smoking” signage was not present in any of the educational institutes at follow-up. The presence of cigarette sales was only observed at one government office both at baseline and follow-up. The presence of cigarette advertisements was not observed anywhere after the smoking ban. In hookah bars, after the smoking ban, neither the presence of cigarette or bidi butts nor the smell of smoking was observed in designated non-smoking areas- a significant improvement in compliance from baseline. In hospitals, entertainment venues and government offices, however, both the presence of cigarette and bidi butts and the smell of smoke, while reduced after the smoking ban, were still observed.
Table 2.
Observational informationin public places before/baseline (July 2008) and after/follow-up (January 2010) the smoking ban (October 2008)
Well-regulated smoke-free venues included government offices, hospitals, and educational institutes, though they did not meet the criteria of a 100% smoke-free environment. However, relatively high air nicotine levels were observed in entertainment venues, restaurants, and hookah bars despite improved compliance with the national smoke-free law.
Discussion
Main findings
Overall air nicotine concentrations significantly declined and compliance with the national smoke-free law visibly improved after the smoking ban although air nicotine was detected in most places even after the smoking ban.
Section 4 of the Indian national smoke-free law (COTPA 2003), prohibited smoking in most public places and provided an optional separate provision for smoking areas or spaces in hotels having 30 or more rooms, restaurants having a seating capacity of 30 or more, and in airports.(27) The revised smoke-free law, “The prohibition of smoking in public places rules, 2008” gave more clarity to the law and defined hotels (including boarding house, guest house), restaurants (including refreshment rooms, banquet halls, discotheques, coffee house, pub, bar, airport lounge, and the like), additional public places (including work places, shopping malls, and cinema halls), and open public space (including open auditoriums, stadiums, railway stations, busstops/stands, and other such places) where smoking is banned.(29) To represent the most commonly visited closed public places, hospitals; government offices; educational institutes; restaurants; entertainment venues (shopping malls, cinema halls); and hookah bars were selected as sampling venues in the present study.
Well-implemented smoke-free laws not only protect common people and workers from exposure to second-hand smoke, but also increase public awareness of the adverse health effects of smoking. Previous studies have highlighted the challenges and barriers to implementing 100% smoke-free laws and policies. A study done in Cairo, Egypt, showed that smoke-free policies were poorly enforced in large teaching hospitals.(31) Reddy et al., reported poor compliance regarding active smoking (36%) and the improper display of “No smoking” signage at the entrance of public places in India (89%).(32) The present study not only found observational improvement in compliance with the Indian smoke-free law, but also found below detectable levels of air nicotine concentration in hospitals of Ahmedabad, India.
High airborne nicotine levels have been observed in venues where there is only a partial smoking ban in place. In South Korea, for example, where smoking is partially prohibited in computer rooms, Kim et al., have pointed out that a complete smoke-free law is needed to reduce SHS in such venues because high air nicotine levels are still detected in nearby non-smoking areas.(33) In Spain, a study looking at the influence of the Spanish no-smoking law on exposure to SHS reached a similar conclusion, as, before the law was implemented, SHS levels were high in non-smoking areas in venues that allowed smoking.(34) In Finland, a partial smoking ban was introduced in July 2003, but the air nicotine levels reported after the ban in 20 bars, restaurants, and discos were similar to those observed before the ban.(35) An analysis of hospitality workers' exposure to SHS indicates that a smoking ban in hospitality venues works best when the venues are 100% tobacco smoke-free; noting that in such cases there is about a 90% reduction in air nicotine and PM2.5 levels.(36) The present study found similar results as high air nicotine concentration were found at restaurants and hookah bars before and after the smoking ban. This was probably due to the fact that the national smoke-free law allows for a designated smoking area at these venues, which clearly demonstrates the need for a 100% smoke-free policy for such venues. Also, the presence of very high air nicotine concentrations at hookah bars at both study intervals may be due to nicotine used as part of the mixture burned for hookah smoking.
Complementary efforts are needed in India to enhance compliance with and enforcement of smoke-free laws with the aim of reducing exposure to SHS in public places. A compliance survey done by Sonu G et al., in Punjab, India, revealed an overall high compliance rate with the smoke-free policies defined under COTPA. The authors suggest that this is probably because of education and communication activities regularly conducted by the state tobacco control cell and the district tobacco control office; and because of the creation of a District Task Force set up to help ensure effective implementation of the legislation.(37) Although the “Smoke-free Ahmedabad and Gandhinagar” project was started by the state tobacco control cell of Gujarat government towards the end of 2009 with support of the Bloomberg Initiative to Reduce Tobacco Use, no activities were started on the ground when the follow-up study was conducted (January 2010). The variability in results after implementing smoking bans may also be due to differences across study jurisdictions (e.g., the makeup of the study population, literacy rates, socio-economic conditions, socio-religious factors, awareness levels, and enforcement mechanisms).
This current study of changes in air nicotine levels in public places in Ahmedabad from 2008 to 2010, the results of similar studies in other parts of India and the related experience of other countries, all support the notion that comprehensive, 100% smoke-free legislation covering all public places is required to adequately protect people from the adverse health effects of exposure to SHS. There is an urgent need to review and strengthen the existing smoke-free law by withdrawing the optional smoking areas allowed at hospitality venues. In addition to awareness campaigns for improving implementation of the national smoke-free law, there is a need to develop effective enforcement and regular compliance monitoring mechanisms at the local level.
Strengths and limitations
The major strength of this study is that nicotine is considered a sensitive and specific marker of SHS and has been used and validated in previous studies.(38,39) This is the first study comparing air nicotine concentrations before and after the enactment of a comprehensive smoke-free law at similar venues in Ahmedabad, India. It provides insight into the effectiveness and level of compliance with the law across different public venues and suggests which venues require additional enforcement and awareness-raising attention.
There are few limitations of the current study. The before-and-after study design was not carried out during the same months, so despite the fact that air nicotine monitoring was carried out in closed public places, there may be potential seasonal differences or other unknown factors that could explain some of the differences in air nicotine levels.(40) Also, the stratified convenience sampling was done to select the most commonly visited public venues with small sample size due to the availability of a limited number of air nicotine monitors. Because the study was conducted in only one city, the ability to generalize our results is limited. However, Ahmedabad is comparable to other large cities in India,(29) so we hypothesize that the findings in other Indian cities would be similar.
In summary, SHS exposure was significantly reduced overall in public places after enactment of the smoke-free legislation in Ahmedabad, India. However, nicotine concentrations were still detected in most of the venues, indicating that compliance with the ban still needs to be improved, especially in those venues where smoking is not completely prohibited.
Acknowledgement
The authors gratefully acknowledge the collaboration and support of Lisa Hepp from Institute for Gobal Tobacco Control, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA for her technical inputs, staff of the State Tobacco Control Cell, Government of Gujarat for execution of this study and Managers of public places of Ahmedabad city for permission and cooperation to conduct this study.
Footnotes
Source of Support: This work was supported by an award from the Bloomberg Initiative to Reduce Tobacco Use and from the Flight Attendant Medical Research Institute to the Institute for Global Tobacco Control at the Johns Hopkins Bloomberg School of Public Health
Conflict of Interest: None declared.
References
- 1.Eriksen M, Mackay J, Ross H. Ch. 1. 4th ed. Atlanta: American Cancer Society and World Lung Foundation; 2012. The Tobacco Atlas. [Google Scholar]
- 2.Jha P. Avoidable global cancer deaths and total deaths from smoking. Nat Rev Cancer. 2009;9:655–64. doi: 10.1038/nrc2703. [DOI] [PubMed] [Google Scholar]
- 3.Mackay J, Eriksen M, Shafey O. The Tobacco Atlas. 2nd ed. Brighton: American Cancer Society; 2006. [Google Scholar]
- 4.The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2006. Office on Smoking and Health (US) [PubMed] [Google Scholar]
- 5.Wang JB, Jiang Y, Wei WQ, Yang GH, Qiao YL, Boffetta P. Estimation of cancer incidence and mortality attributable to smoking in China. Cancer Causes Control. 2010;21:959–65. doi: 10.1007/s10552-010-9523-8. [DOI] [PubMed] [Google Scholar]
- 6.Jemal A, Thun MJ, Ries LA, Howe HL, Weir HK, Center MM, et al. Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst. 2008;100:1672–94. doi: 10.1093/jnci/djn389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Mohandes AA, Kiely M, Blake SM, Gantz MG, El-Khorazaty MN. An intervention to reduce environmental tobacco smoke exposure improves pregnancy outcomes. Pediatrics. 2010;125:721–8. doi: 10.1542/peds.2009-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eisner MD, Wang Y, Haight TJ, Balmes J, Hammond SK, Tager IB. Secondhand smoke exposure, pulmonary function, and cardiovascular mortality. Ann Epidemiol. 2007;17:364–73. doi: 10.1016/j.annepidem.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Schroeder SA. New evidence that cigarette smoking remains the most important health hazard. N Engl J Med. 2013;368:389–90. doi: 10.1056/NEJMe1213751. [DOI] [PubMed] [Google Scholar]
- 10.Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–64. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandey D, Pandey R. Case-control study of smoking and death in India. N Engl J Med. 2008;358:2844. [PubMed] [Google Scholar]
- 12.Maritz GS, Mutemwa M. Tobacco smoking: Patterns, health consequences for adults, and the long-term health of the offspring. Glob J Health Sci. 2012;4:62–75. doi: 10.5539/gjhs.v4n4p62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanski SE, Wilson KM. Children and secondhand smoke: Clear evidence for action. Pediatrics. 2012;129:170–1. doi: 10.1542/peds.2011-3190. [DOI] [PubMed] [Google Scholar]
- 14.Conference of the Parties to the WHO Framework Convention on Tobacco Control. Geneva: World Health Organization; 2003. [Google Scholar]
- 15.Barnoya J, Glantz S. Association of the California tobacco control program with declines in lung cancer incidence. Cancer Causes Control. 2004;15:689–95. doi: 10.1023/B:CACO.0000036187.13805.30. [DOI] [PubMed] [Google Scholar]
- 16.Jemal A, Cokkinides VE, Shafey O, Thun MJ. Lung cancer trends in young adults: An early indicator of progress in tobacco control (United States) Cancer Causes Control. 2003;14:579–85. doi: 10.1023/a:1024891201329. [DOI] [PubMed] [Google Scholar]
- 17.Callinan JE, Clarke A, Doherty K, Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010:CD005992. doi: 10.1002/14651858.CD005992.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Kaur J, Jain DC. Tobacco control policies in India: Implementation and challenges. Indian J Public Health. 2011;55:220–7. doi: 10.4103/0019-557X.89941. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization (WHO) Geneva, Switzerland. MPOWER. WHO Report on the Global tobacco epidemic, World Health Organization. 2008 [Google Scholar]
- 20.Ministry of Health and Family Welfare, Government of India. New Delhi: 2010. International Institute for Population Sciences. Global Adult Tobacco Survey India (GATS India) 2009-2010. [Google Scholar]
- 21.Srivastava S, Malhotra S, Harries AD, Lal P, Arora M. Correlates of tobacco quit attempts and cessation in the adult population of India: Secondary analysis of the Global Adult Tobacco Survey, 2009-10. BMC Public Health. 2013;12:263. doi: 10.1186/1471-2458-13-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prasad R, Ahuja RC, Singhal S, Srivastava AN, James P, Kesarwani V, et al. A case-control study of bidi smoking and bronchogenic carcinoma. Ann Thorac Med. 2010;5:238–41. doi: 10.4103/1817-1737.69116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaudhry K, Rath GK. Multisectoral and intersectoral approach to national tobacco control. Paper commissioned by the World Health Organization on the occasion of the WHO International Conference on Global Tobacco Control Law: Towards a WHO Framework Convention on Tobacco Control; New Delhi. 2000. [Google Scholar]
- 24.Ahamad T, Alshehri SM. TG-FTIR-MS (Evolved Gas Analysis) of bidi tobacco powder during combustion and pyrolysis. J Hazard Mater. 2012;199-200:200–8. doi: 10.1016/j.jhazmat.2011.10.090. [DOI] [PubMed] [Google Scholar]
- 25.Sinha DN, Narain JP, Kyaing NN, Rinchen S. WHO framework convention on tobacco control and its implementation in South-East Asia region. Indian J Public Health. 2011;55:184–91. doi: 10.4103/0019-557X.89949. [DOI] [PubMed] [Google Scholar]
- 26.Government of India, Ministry of Health and Family Welfare. The cigarettes and other tobacco products (Prohibition of Advertisement and Regulation of Trade and Commerce, Production, Supply and Distribution) Act, 2003 and related rules & regulations; New Delhi. 2003. [Google Scholar]
- 27.Jhanjee S. Tobacco Control in India — Where are we now. Review article? Delhi Psychiatr J. 2011;14:26–32. [Google Scholar]
- 28.Government of India, Ministry of Health and Family Welfare. The prohibition of smoking in public places rules, 2008; New Delhi. 2008. [Google Scholar]
- 29.Census of India 2011. New Delhi: Government of India; 2011. Office of the Registrar General & Census Commissioner, Ministry of Home Affairs, Government of India. [Google Scholar]
- 30.Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol. 1987;21:494–7. doi: 10.1021/es00159a012. [DOI] [PubMed] [Google Scholar]
- 31.Radwan GN, Loffredo CA, Aziz R, Abdel-Aziz N, Labib N. Implementation, barriers and challenges of smoke-free policies in hospitals in Egypt. BMC Res Notes. 2012;5:568. doi: 10.1186/1756-0500-5-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reddy KS, Arora M, Shrivastav R. Implementation of the Framework Convention on Tobacco Control (FCTC) in Indiaa shadowreport-2010. New Delhi, India: HRIDAY and Framework Convention Alliance; 2010. [Google Scholar]
- 33.Kim S, Sohn J, Lee K. Exposure to particulate matters (PM2.5) and airborne nicotine in computer game rooms after implementation of smoke-free legislation in South Korea. Nicotine Tob Res. 2010;12:1246–53. doi: 10.1093/ntr/ntq189. [DOI] [PubMed] [Google Scholar]
- 34.Lopez MJ, Nebot M, Schiaffino A, Pérez-Ríos M, Fu M, Ariza C, et al. Spanish Smoking Law Evaluation Group. Two-year impact of the Spanish smoking law on exposure to secondhand smoke: Evidence of the failure of the ‘Spanish model’. Tob Control. 2012;21:407–11. doi: 10.1136/tc.2010.042275. [DOI] [PubMed] [Google Scholar]
- 35.Johnsson T, Tuomi T, Riuttala H, Hyvärinen M, Rothberg M, Reijula K. Environmental tobacco smoke in Finnish restaurants and bars before and after smoking restrictions were introduced. Ann Occup Hyg. 2006;50:331–41. doi: 10.1093/annhyg/mel011. [DOI] [PubMed] [Google Scholar]
- 36.Polanska K, Hanke W, Konieczko K. Hospitality workers' exposure to environmental tobacco smoke before and after implementation of smoking ban in public places: A review of epidemiological studies. Med Pr. 2011;62:211–24. [PubMed] [Google Scholar]
- 37.Goel S, Ravindra K, Singh RJ, Sharma D. Effective smoke-free policies in achieving a high level of compliance with smoke-free law: Experiences from a district of North India. Tob Control. 2014;23:291–4. doi: 10.1136/tobaccocontrol-2012-050673. [DOI] [PubMed] [Google Scholar]
- 38.Hammond SK, Sorensen G, Youngstrom R, Ockene JK. Occupational exposure to environmental tobacco smoke. JAMA. 1995;274:956–60. [PubMed] [Google Scholar]
- 39.Mulcahy M, Evans DS, Hammond SK, Repace JL, Byrne M. Secondhand smoke exposure and risk following the Irish smoking ban: An assessment of salivary cotinine concentrations in hotel workers and air nicotine levels in bars. Tob Control. 2005;14:384–8. doi: 10.1136/tc.2005.011635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phillips K, Bentley MC. Seasonal assessment of environmental tobacco smoke and respirable suspended particle exposures for nonsmokers in Bremen using personal monitoring. Environ Int. 2001;27:69–85. doi: 10.1016/s0160-4120(01)00057-5. [DOI] [PubMed] [Google Scholar]


