Abstract
Background and Aim:
Violence against women during pregnancy is linked to poor outcome of pregnancy, which is reported to have widespread in Iran. The aim of this study was to determine the prevalence of physical violence against women by an intimate partner during pregnancy, and to assess the impact of this physical violence on pregnancy outcomes.
Materials and Methods:
A prospective cohort study was conducted on the characteristics of pregnant women in urban areas and related violence. The modified standard World Health Organization Domestic Violence Questionnaire was used to classify pregnant women and domestic violence. A total of 1461 pregnant women were selected using cluster sampling. The association between sociodemographic with intimate partner violence (IPV) and IPV with pregnancy outcomes was determined using logistic regression.
Results:
Of these, 206 (14.1%) (confidence interval = 12.3-15.9) reported physical IPV during pregnancy. The adjusted odds ratio for IPV in illiterate women or those with primary level of education (0.001), secondary level education (0.003), and in low income households (0.0001) were significantly higher than in those women with university level education and in higher income households. After adjusting for suspected confounding factors, the women with a history of violence by partners had 1.9 fold risk of premature rupture of membranes, and a 2.9 fold risk of low birth weight compared to women who did not experience any violence from their partners.
Conclusion:
The results of this research indicated that the prevalence of IPV was high among pregnant women. Therefore, it is necessary to emphasize the screening of pregnant women at Primary Health Centers to prevent physical abuse.
Keywords: Family violence, pregnancy outcome, pregnancy social epidemiology
INTRODUCTION
Domestic violence against women is one of the most pervasive abuses of human rights in the world.[1] It is related to violence of any kind that is likely to result in physical, sexual or psychological harm or suffering of women whether it occurs in private or in public.[2] It is unlikely that pregnancy can protect the women against violence.[3] A study around the world reported a prevalence estimate between 3.8% and 8.8%.[4] Review studies indicate that approximately 1-8% of pregnant women in developed[5] and approximately 4-29% in developing countries report some type of violence by a partner.[6] The prevalence of violence during pregnancy in Iran varies from one city to the other in a range of 9-60%.[7,8]
It has been estimated that the annual health care cost resulting from intimate partner violence (IPV) is billions in the United States.[9] Physical IPV during pregnancy could affect pregnancy directly or indirectly when there is a blow to the abdomen, impact on mental health and behavioural changes and cause adverse outcomes of pregnancy such as fetal death, preterm labor, miscarriage, low birth weight (LBW), abdominal pain and hospitalization although some studies have not confirmed these associations.[10,11]
An understanding of the effect of a partner's violence against a pregnant woman could have important reproductive health implications with early identification. It could also help in shaping future intervention programs. Pregnancy provides an opportunity to screen for domestic violence since pregnant women make routine visits during this period.[12,13,14,15,16,17]
There is a dearth of literature on the effect of physical violence on pregnancy outcomes in large communities in Iran. Therefore, it is critical to explore the impact of physical violence on pregnancy outcomes in pregnant women here. In addition, this study was designed to obtain accurate information on the prevalence of physical IPV during pregnancy, and the possible associated sociodemographic factors in Mazandaran Province, Iran.
MATERIALS AND METHODS
The research design of this study was a prospective cohort study. To determine the required sample size with an expected proportion of 60%[18] α = 0.05%, and power = 80% was thus calculated to be 1500 pregnant women.
Informed written consent was obtained from all eligible singleton pregnant women, 18-45 years of age, who were routinely attending Mazandran urban primary health care centers during the first trimester. In order to determine accurately the associated sociodemographics with IPV, women with a history of mental disorders and severe pregnancy complications were excluded from the study.
The study was conducted in collaboration with the Primary Health Centers (PHCs) of Mazandaran University of Medical Sciences in the North of Iran. A total of 308 PHCs (101 PHCs in urban areas, and 207 in rural areas) were contacted for sampling. Cluster sampling was performed in each city based on the number of PHCs. Therefore, a total of 1550 pregnant women were selected randomly at the primary health care clinics in proportion to size from February to September 2010; 35 (2.3%) women were excluded based on exclusion criteria. Data was collected by face-to-face interviews, lasting approximately 20 min, conducted by trained skillful personnel in private, in the absence of the partner/or other family members. The questionnaires of 54 (3.5%) participants were not correctly filled, therefore, the final sample size was 1461, giving a participation rate of 94.3%. All the women were followed up till delivery.
The modified standard World Health Organization Domestic Violence Questionnaire was used to assess the individual's physical violence in order to classify pregnant women who experience domestic violence. It consisted of 32 questions on all dimensions of violence used in Iran-Tehran.[8] Physical, emotional, financial and sexual violence were determined. In this study, physical violence during pregnancy meant any one of these 10; the use of cold or warm weapon, a slap, a punch, being shoved, kicked, bruised, burnt, having fractures, a blow to internal organs as a result of PV. During the screening, the women were divided in two groups of pregnant women: “Exposed to physical violence” and “no physical violence”.
The socio-demographic factors included age, years married, level of education, gender of children, polygamy, consanguinity, accommodation, household members' income and occupation of the women. Information on reproductive history was collected according to the known risk factors.
The subjects were categorized into three groups by household income during the previous year: <3,500,000 Rials, 3,500,000-4,500,000 Rials, and more than 4,500,000 Rials (USD = 30,000 Rials)/month.
After the pregnancy, the outcomes such as abortion, preeclampsia, premature rupture of membranes, LBW, and preterm delivery were obtained from the medical records of the hospital where the delivery took place.[19] The alpha coefficient and internal consistency of questionnaire was tested with 50 other pregnant women and was 0.87 and 0.91, respectively.
Statistical analysis
All analyses were carried out using IBM Statistical Package for the Social Sciences (SPSS) version 20. Prevalence of domestic violence and their 95% confidence intervals (95% CIs) were computed. The association between IVP and other categorical variables was assessed using Chi-Square test or Fisher's Exact test as appropriate. To dtermine the associations between the socio-demographic factors, reproductive history with domestic violence, IPV was considered as a dependent variable for the logistic regression model. Odds ratios (ORs) were assessed using the maximum likelihood method, and associated 95% CI were computed. The final multivariate model included pregnancy outcome (LBW, Premature rapture of membrane [PROM] etc.) as the dependent and independent variables that were related to this outcome at P = 0.2 in the bivariate analyses. All P values were two-sided, and P ≤ 0.05 was considered statistically significant.
RESULTS
A total of 1461 pregnant women participated in the study. Of these, 206 women reported physical abuse with IPV prevalence rate of 14.1% (CI = 12.3-15.9). Women who reported physical abuse by intimate partner were included in group “exposed to violence”, while those who did not suffer physical abuse by intimate partner were included in the group labeled “no violence”.
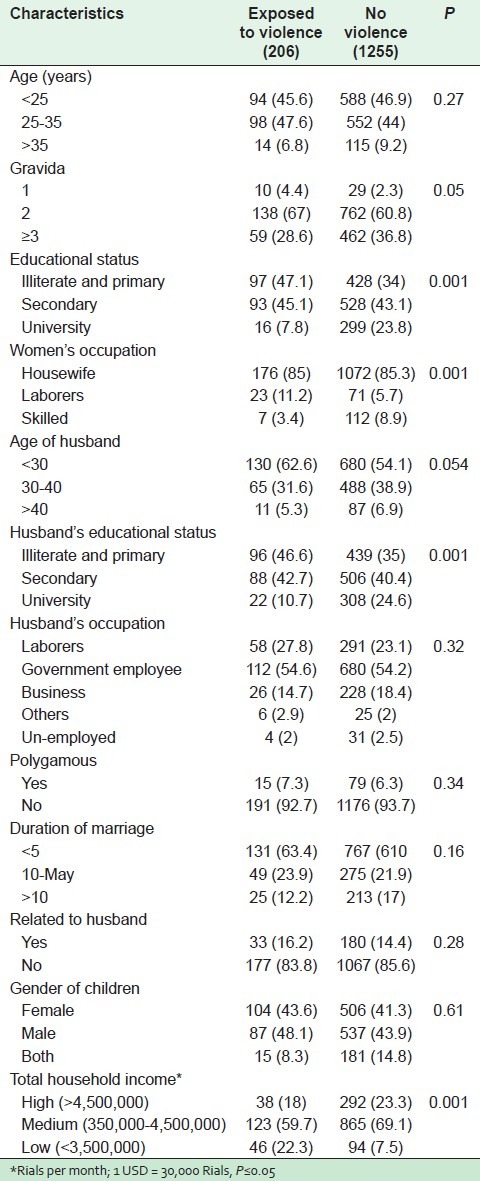
The mean value for the age of the women, husband's age, and years married was 26.8 ± 5.8, 30.8 ± 6.2 and 5.9 ± 4.7, respectively. Table 1 illustrates the prevalence of physical IPV based on the characteristics of the women. The women with a lower level of education, who were laborers, were pregnant for the first time, had low income, and were married to men with little education experienced more physical IPV during pregnancy than other women (P < 0.05).
Table 1.
Baseline characteristics of participants (n=1461)
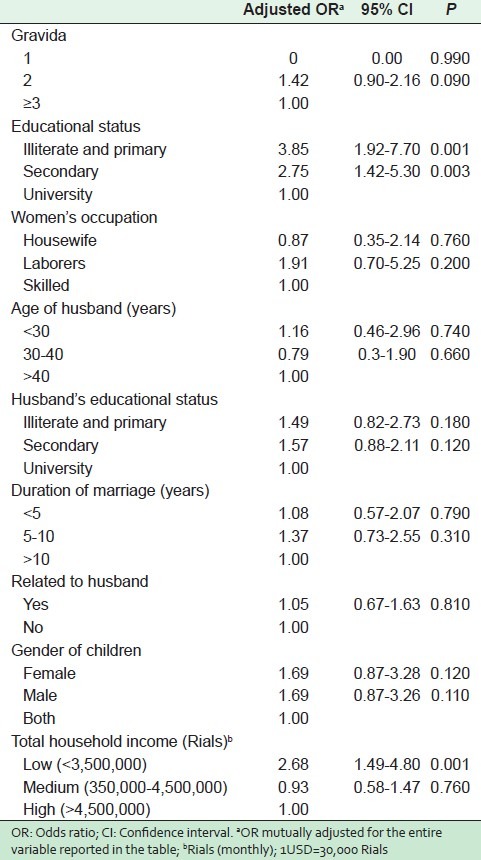
As shown in Table 2, the adjusted OR of physical IPV in illiterate women and those with primary education, secondary education, and low household income was significantly higher than those women with university education and higher household income, as evident from adjusted risk estimates (OR = 3.85; 95% CI = 1.92-7.70), (OR = 2.75; 95% CI = 1.42-5.30) and (OR = 2.68; 95% CI = 1.49-4.80), respectively.
Table 2.
Adjusted ORs from multiple logistic regression models for the association of physical violence during pregnancy by an intimate partner with sociodemographic factors, reproductive history (n=1461)
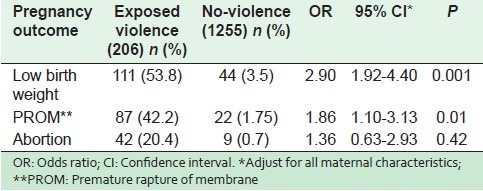
After adjustment for confounding factors (age, years married, education and occupational status of the women and their husbands, family income, state of accommodation, and parity) the risk of premature rupturing of membranes and LBW were found to be associated with the experience of physical IPV during pregnancy in multiple logistic regression [Table 3].
Table 3.
Adjusted OR from multiple logistic regression models for the association of domestic violence during pregnancy by an intimate partner with adverse pregnancy outcomes (n=1461)
DISCUSSION
Intimate partner violence is an important public health, reproductive health, and social concern of the whole world.[20] It could be a significant predictor of adverse outcomes for two individuals: The mother and her infant.[2,15] Moreover, violence during pregnancy can have long term consequences especially when it is under-recognized.[12,21]
The present study found that a high proportion of women (14.1%) were exposed to physical violence by intimate partner (IPV) during pregnancy. However, the prevalence of IPV in Pakistan and South Africa (as quoted) appears to be 2-3 times higher than what is reported in Iran.[10,22] Exposure to IPV during pregnancy takes different forms in different countries. It is difficult to arrive at definite conclusions because of the lack of a standard definition, differences in study methodology, parameters observed and the unwillingness of women to disclose physical abuse because of cultural barriers.3,[6,7] Considering the high pregnancy rate in the developing world, violence during pregnancy is a public health concern that needs special attention.[6]
In the present study, physical violence during pregnancy was associated with a lower level of education and a lower socioeconomic status of women. In her review of literature, Baily (2010) found that although no women were immune from violence in pregnancy, certain characteristics such as younger women of low socio-economic class were predisposed to increased experience of this phenomenon.[3] Similarly, a study in the USA found that income and education were the most significant predictors of violence during pregnancy.[23]
Physical IPV may have serious reproductive health consequences. Examination of violence during pregnancy in a population-based study in Iran, revealed an association between PROM and the exposure to physical IPV. Additionally, our data support the findings of previous researchers who reported that IPV during pregnancy was association with LBW[24] although this association has not been confirmed by the limited studies done.[10] A few studies have investigated the link between violence and abortion.[14,25,26] A Tanzanian survey conducted by Stöckl et al. (2012) found that women who experienced violence during pregnancy were 1.9 (95% CI: 1.30-2.89) times more likely to report an induced abortion.[27] Our study, however, did not show any significant association between violence and abortion. More detailed studies in this area are required. Many mechanisms have been postulated on how PV may impact on birth outcomes, such as direct health, mental health[28,29] physical and behavioral effects.[3,30,31] Negative health behaviour such as inadequate utilization of prenatal care and insufficient weight gain have been associated with both physical IPV and LBW.[24,32,33] Also, the link between physical IPV and a delay in prenatal care and poor nutritional intake, which are associated with poor pregnancy outcome has been explained in several reports.[7,32,34]
Numerous researches have explored the disastrous effects of mental health problems during pregnancy on adverse birth outcomes.[35] The most common mental health effect of IPV is depression.[12] Moreover, most women who experience IPV have reported experiencing posttraumatic stress disorder,[35,36] which is associated with both preterm birth and LBW.[32,37]
Physical violence during pregnancy is often directed towards the pregnant abdomen, and can lead to premature labor, rupture of membranes and placental abruption. These assaults result in preterm birth or even fetal loss.[15,16,17,15,24]
Limitations of this study are perhaps selection bias since the subjects were volunteers, and there was no detection of violence before-pregnancy. It is not known if experiencing violence prior to the pregnancy would have affected the mothers' decision to volunteer to participate in this project. However, participation rate of 94.3 is a valuable initial step in determining the relationship between IPV and pregnancy outcome, and the prevalence of IPV in pregnant women.
CONCLUSION
Our study findings revealed that physical IPV is a significant problem associated with adverse pregnancy outcomes. This gives some support to the importance of screening for IPV during pregnancy. While any pregnant women may be at risk, the most vulnerable are those of low socio-economic status with a low level of education, and those who have other medical problems.
Health care providers should be aware of the importance of violence in their practice, and try to identify women at risk. Pregnancy provides an appropriate chance to identify those at risk and provide the relevant interventions. Using a standardized instrument with cultural adaptation together with the knowledge of maternal characteristics statistically associated with violence in pregnancy can help healthcare providers to identify women at risk and assist in intervention.
Unfortunately, a number of cultural barriers in developing countries make screening for violence and intervention very difficult. Moreover, many mothers are reluctant to admit to being abused. Sometimes violence is even taken as normal or given, and a personal family issue which is accepted by the society. Exposing this matter is, therefore, often a taboo in these societies.[10] Providing relevant information by midwives about IPV, and diminishing or modifying related risk factors could be an approach to reducing the risk of adverse pregnancy outcomes.
ACKNOWLEDGMENT
Special thanks are extended to health care providers and mothers who agreed to participate in this project.
Footnotes
Source of Support: This study was supported by Mazandaran University of Medical Sciences (grant number 201074)
Conflict of Interest: None declared.
REFERENCES
- 1.Bunch C. Women's rights as human rights: Toward a re-vision of human rightsauthor(s): Charlotte bunch. Hum Rights Q. 1990;12:486–98. [Google Scholar]
- 2.García-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. WHO multi-country study on women's health and domestic violence against women. Geneva: World Health Organization; 2005. [Google Scholar]
- 3.Bailey BA. Partner violence during pregnancy: Prevalence, effects, screening, and management. Int J Womens Health. 2010;2:183–97. doi: 10.2147/ijwh.s8632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devries KM, Kishor S, Johnson H, Stöckl H, Bacchus LJ, Garcia-Moreno C, et al. Intimate partner violence during pregnancy: Analysis of prevalence data from 19 countries. Reprod Health Matters. 2010;18:158–70. doi: 10.1016/S0968-8080(10)36533-5. [DOI] [PubMed] [Google Scholar]
- 5.Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. JAMA. 1996;275:1915–20. [PubMed] [Google Scholar]
- 6.Nasir K, Hyder AA. Violence against pregnant women in developing countries: Review of evidence. Eur J Public Health. 2003;13:105–7. doi: 10.1093/eurpub/13.2.105. [DOI] [PubMed] [Google Scholar]
- 7.Faramarzi M, Esmaelzadeh S, Mosavi S. Prevalence, maternal complication and birth outcome of physical, sexual and emotional domestic violence during pregnancy. Acta Med Iran. 2005;43:115–22. [Google Scholar]
- 8.Jahanfar S, Malekzadegan Z. The prevalence of domestic violence among pregnant women who were attended in iran university of medical science hospitals. J Fam Violence. 2007;22:643–8. [Google Scholar]
- 9.Brown DS, Finkelstein EA, Mercy JA. Methods for estimating medical expenditures attributable to intimate partner violence. J Interpers Violence. 2008;23:1747–66. doi: 10.1177/0886260508314338. [DOI] [PubMed] [Google Scholar]
- 10.Zareen N, Majid N, Naqvi S, Saboohi S, Fatima H. Effect of domestic violence on pregnancy outcome. J Coll Physicians Surg Pak. 2009;19:291–6. [PubMed] [Google Scholar]
- 11.Coker AL, Sanderson M, Dong B. Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatr Perinat Epidemiol. 2004;18:260–9. doi: 10.1111/j.1365-3016.2004.00569.x. [DOI] [PubMed] [Google Scholar]
- 12.Flach C, Leese M, Heron J, Evans J, Feder G, Sharp D, et al. Antenatal domestic violence, maternal mental health and subsequent child behaviour: A cohort study. BJOG. 2011;118:1383–91. doi: 10.1111/j.1471-0528.2011.03040.x. [DOI] [PubMed] [Google Scholar]
- 13.Lipsky S, Holt VL, Easterling TR, Critchlow CW. Impact of police-reported intimate partner violence during pregnancy on birth outcomes. Obstet Gynecol. 2003;102:557–64. doi: 10.1016/s0029-7844(03)00573-8. [DOI] [PubMed] [Google Scholar]
- 14.Fanslow J, Silva M, Whitehead A, Robinson E. Pregnancy outcomes and intimate partner violence in New Zealand. Aust N Z J Obstet Gynaecol. 2008;48:391–7. doi: 10.1111/j.1479-828X.2008.00866.x. [DOI] [PubMed] [Google Scholar]
- 15.Audi CA, Segall-Corrêa AM, Santiago SM, Pérez-Escamilla R. Adverse health events associated with domestic violence during pregnancy among Brazilian women. Midwifery. 2012;28:356–61. doi: 10.1016/j.midw.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Shah PS, Shah J. Knowledge Synthesis Group on Determinants of Preterm/LBW Births. Maternal exposure to domestic violence and pregnancy and birth outcomes: A systematic review and meta-analyses. J Womens Health (Larchmt) 2010;19:2017–31. doi: 10.1089/jwh.2010.2051. [DOI] [PubMed] [Google Scholar]
- 17.Janssen PA, Holt VL, Sugg NK, Emanuel I, Critchlow CM, Henderson AD. Intimate partner violence and adverse pregnancy outcomes: A population-based study. Am J Obstet Gynecol. 2003;188:1341–7. doi: 10.1067/mob.2003.274. [DOI] [PubMed] [Google Scholar]
- 18.Faramarzi M, Esmailzadeh S, Mosavi S. Prevalence and determinants of intimate partner violence in Babol City, Islamic Republic of Iran. East Mediterr Health J. 2005;11:870–9. [PubMed] [Google Scholar]
- 19.Cunningham FG. Williams Obstetrics. New York: McGraw-Hill; 2005. [Google Scholar]
- 20.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360:1083–8. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 21.McMahon S, Huang CC, Boxer P, Postmus JL. The impact of emotional and physical violence during pregnancy on maternal and child health at one year post-partum. Child Youth Serv Rev. 2011;33:2103–11. [Google Scholar]
- 22.Hoque ME, Hoque M, Kader SB. Prevalence and experience of domestic violence among rural pregnant women in KwaZulu-Natal, South Africa. South Afr J Epidemiol Infect. 2009;24:34–7. [Google Scholar]
- 23.Bohn DK, Tebben JG, Campbell JC. Influences of income, education, age, and ethnicity on physical abuse before and during pregnancy. J Obstet Gynecol Neonatal Nurs. 2004;33:561–71. doi: 10.1177/0884217504269009. [DOI] [PubMed] [Google Scholar]
- 24.Khodakarami N, Naji H, Dashti MG, Yazdjerdi M. Woman abuse and pregnancy outcome among women in Khoram Abad, Islamic Republic of Iran. East Mediterr Health J. 2009;15:622–8. [PubMed] [Google Scholar]
- 25.Cokkinides VE, Coker AL, Sanderson M, Addy C, Bethea L. Physical violence during pregnancy: Maternal complications and birth outcomes. Obstet Gynecol. 1999;93:661–6. doi: 10.1016/s0029-7844(98)00486-4. [DOI] [PubMed] [Google Scholar]
- 26.Silverman JG, Decker MR, McCauley HL, Gupta J, Miller E, Raj A, et al. Male perpetration of intimate partner violence and involvement in abortions and abortion-related conflict. Am J Public Health. 2010;100:1415–7. doi: 10.2105/AJPH.2009.173393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stöckl H, Filippi V, Watts C, Mbwambo JK. Induced abortion, pregnancy loss and intimate partner violence in Tanzania: A population based study. BMC Pregnancy Childbirth. 2012;12:12. doi: 10.1186/1471-2393-12-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnett OW. Why battered women do not leave, part 2 external inhibiting factors social support and internal inhibiting factors. Trauma Violence Abuse. 2001;2:3–35. [Google Scholar]
- 29.Bacchus L, Mezey G, Bewley S. Domestic violence: Prevalence in pregnant women and associations with physical and psychological health. Eur J Obstet Gynecol Reprod Biol. 2004;113:6–11. doi: 10.1016/S0301-2115(03)00326-9. [DOI] [PubMed] [Google Scholar]
- 30.Kearney MH, Munro BH, Kelly U, Hawkins JW. Health behaviors as mediators for the effect of partner abuse on infant birth weight. Nurs Res. 2004;53:36–45. doi: 10.1097/00006199-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Shah AJ, Kilcline BA. Trauma in pregnancy. Emerg Med Clin North Am. 2003;21:615–29. doi: 10.1016/s0733-8627(03)00038-5. [DOI] [PubMed] [Google Scholar]
- 32.Bohn DK. Lifetime and current abuse, pregnancy risks, and outcomes among Native American women. J Health Care Poor Underserved. 2002;13:184–98. doi: 10.1353/hpu.2010.0624. [DOI] [PubMed] [Google Scholar]
- 33.Moraes CL, Amorim AR, Reichenheim ME. Gestational weight gain differentials in the presence of intimate partner violence. Int J Gynaecol Obstet. 2006;95:254–60. doi: 10.1016/j.ijgo.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 34.Nunes MA, Ferri CP, Manzolli P, Soares RM, Drehmer M, Buss C, et al. Nutrition, mental health and violence: From pregnancy to postpartum Cohort of women attending primary care units in Southern Brazil - ECCAGE study. BMC Psychiatry. 2010;10:66. doi: 10.1186/1471-244X-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mertin P, Mohr PB. Incidence and correlates of posttraumatic stress disorder in Australian victims of domestic violence. J Fam Violence. 2000;15:411–22. [Google Scholar]
- 36.Cohen H, Benjamin J, Geva AB, Matar MA, Kaplan Z, Kotler M. Autonomic dysregulation in panic disorder and in post-traumatic stress disorder: Application of power spectrum analysis of heart rate variability at rest and in response to recollection of trauma or panic attacks. Psychiatry Res. 2000;96:1–13. doi: 10.1016/s0165-1781(00)00195-5. [DOI] [PubMed] [Google Scholar]
- 37.Rosen D, Seng JS, Tolman RM, Mallinger G. Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low-income mothers. J Interpers Violence. 2007;22:1305–14. doi: 10.1177/0886260507304551. [DOI] [PubMed] [Google Scholar]


