Abstract
Background:
Vitiligo is one of the disorder that has social impact. Both skin and mucous membrane show depigmentation in vitiligo. Depigmentation in oral cavity can be more easily observed and the patient can be given awareness regarding the condition if they are unaware of vitiligo elsewhere in their body and can be guided for treatment.
Aim and objectives:
The aim of this study is to determine the frequency of occurrence of oral mucosal vitiligo in vitiligo patients and to determine the most commonly involved oral mucosal site.
Materials and methods:
The study sample included 100 vitiligo patients. The patients of all age groups and both genders were included. Vitiligo patients associated with systemic conditions such as thyroid disorders, juvenile diabetes mellitus, pernicious anemia, Addison's disease were excluded in this study.
Results:
Out of 100 vitiligo patients 44 % male and 56% were female. The oral presentation of vitiligo in this study showed depigmentation of buccal mucosa in 5% of patients, labial mucosa in 5% of patients, palate in 8% of patients, gingiva in 2% of patients and alveolar mucosa 1%. Depigmentation of lip was seen in 42% of patients. Lip involvement refers to depigmentation of both the lips or either lip. Also vermilion border involvement was noted in majority of cases. In some cases, the depigmentation of lip extended to the facial skin also.
Conclusion:
In this study 55 patients out of 100 patients showed depigmentation in the oral cavity. Lip involvement was most common in this study showing about 42% of patients. Intraoral mucosal involvement was found in 21% of patients. Among intraoral mucosal site palate was common followed by buccal and labial mucosa, gingiva. Two patients had lip pigmentation as the only manifestation without any depigmentation in the skin.
Keywords: Depigmentation, leukoderma, leukopathia, vitiligo
What was known?
In patients with vitiligo oral manifestations have been reported in the lips, palate and gingiva.
Introduction
Vitiligo is a non-contagious acquired pigmentation disorder characterized by defined white patches of variable shape and dimensions, increasing in size and number with time.[1] It is also called leukopathia or leukoderma.[2] Vitiligo occurs worldwide with an overall prevalence of 1%.[2,3,4,5,6,7,8,9] In India, the incidence of vitiligo is found to be 0.25-2.5%.[8] The prevalence range in India found to be 0.46-8.8%[10] with Gujarat and Rajasthan states have highest prevalence of approximately 8.8%.[8] International studies showed an incidence range of vitiligo to be 0.1-8.8%.[11] Approximately 30% acquire the disease before the age of 20 years and 14% before the age of 10 years, with decreasing incidence in later life, and fewer than 10% develop vitiligo by the age of 42 years. Infants 4-6 months of age may develop typical vitiligo mainly in the genital or perianal area.
Etiology of vitiligo is not known but the loss of melanocytes in epidermis is explained by certain pathogenetic hypothesis such as genetic hypothesis, autoimmune hypothesis, neural hypothesis, autocytotoxic hypothesis, novel microenvironment-related hypothesis and convergence theory.[1]
As a depigmenting disease vitiligo also has a greater impact on patients’ psychosocial aspects. Persons affected with vitiligo especially children and females have greater difficulty in their social relationships due to psychological depression.
Materials and Methods
Our study group consists of 100 vitiligo patients. The demographic features including age and genders were included in this study. Patients with vitiligo skin lesions were only included in this study. Vitiligo associated with systemic conditions such as thyroid disorders, juvenile diabetes mellitus, pernicious anemia, Addison's disease was not included.
The frequency of the occurrence of oral mucosal vitiligo and most commonly involved mucosal site were observed in this study.
Results
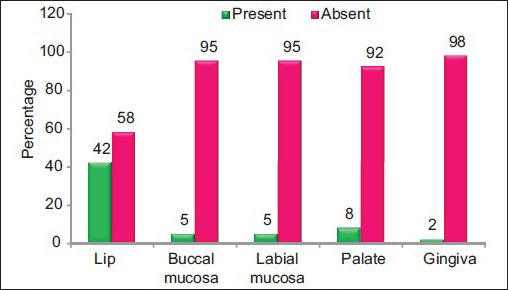
Among the 100 vitiligo patients in our study 44% were males and 56% females. The minimum age of 4 years and the maximum age of 76 years were observed in this study. Among the 100 vitiligo patients 18% were up to 25 years, 14% within 25 to 35 years, 30% within 35 to 45 years, 19% within 45 to 55 years and 19% more than 55 years (Graph 1). In the present study of 100 vitiligo patients, 55 patients showed depigmentation in the oral cavity. Oral mucosal depigmentation were presented in lip (42%), palate (8%), buccal mucosa (5%), labial mucosa (5%) and gingiva (2%) [Table 1 and Graph 2]. The association of oral vitiligo with respect to age was 10% within 25 years, 6% among age group of 26-35 years, 14% among age group of 36-45 years, 6% within 46-55 years and 9% of patients above 55 years [Table 2 and Graph 3]. Regarding the gender, the association of oral presentation among our study group showed to be 18% in males and 27% in females [Table 3 and Graph 4].
Graph 1.
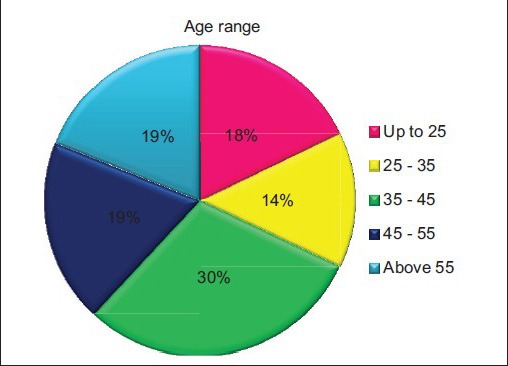
Pie chart showing the age distribution among the 100 vitiligo patients
Table 1.
Presence of depigmentation in various sites of oral cavity
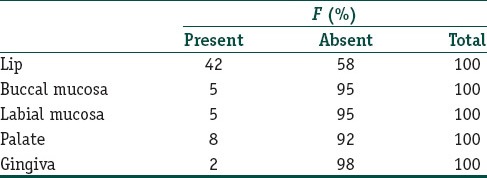
Graph 2.
Percentage of presence and absence of oral depigmentation in lips, buccal mucosa, labial mucosa, palate and gingiva among the study group
Table 2.
Presence of oral findings with respect to age
Graph 3.
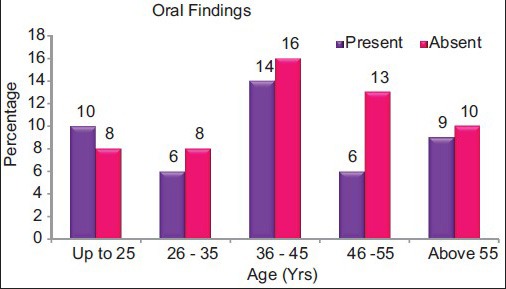
Presence of oral findings with respect to age
Table 3.
Presence of oral findings with respect to gender
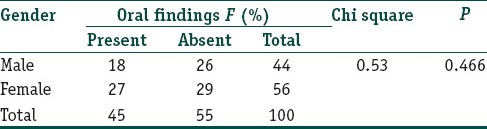
Graph 4.
Presence of oral findings with respect to gender
Discussion
Vitiligo is a common non-infectious dermatological disorder characterized by acquired, idiopathic, progressive, circumscribed hypomelanosis of the skin and hair, with the total absence of melanocytes microscopically.[12,13]
Age distribution
Out of 100 patients in this study, 44 patients were males and 56 patients were females showing higher incidence. This finding was consistent with studies conducted by Shajil et al.,[8] Nigam et al.,[14] Pandya et al.,[15] Chanda et al.[12] The study conducted by Shameer et al.[13] showed male predilection. The mean age of incidence in our study was 41.5 years. Other studies by Shameer et al.,[13] Shajil et al.,[8] Pandya et al.[15] showed 33.8 years, 25.59 years and 21 to 30 years, respectively.
Age range
Our study of vitiligo patients showed a minimum age of 4 years and a maximum age of 76 years. Another study by Gonul et al.[16] showed minimum and maximum age as 8 years to 72 years respectively which is closely correlating with our study.
Oral presentation
The oral presentation of vitiligo in the present study showed depigmentation of lip in 42 patients, buccal mucosa in 5 patients, labial mucosa in 5 patients, palate in 8 patients, gingiva in 2 patients. In our study out of 100 vitiligo patients, 21 patients showed intra oral mucosal depigmentation. Among the intraoral mucosal sites palate was found to be the common followed by labial and buccal mucosa, gingiva and alveolar mucosa.
The number of vitiligo patients in our study showing oral depigmentation was about 9 up to 25 years, 8 in the age range of 25 to 35 years, 19 among the age of 35 to 45 years, 15 in the age range of 45 to 55 years and 11 above 55 years. Thus, higher incidence of oral mucosal vitiligo was noted in patients of age 35 to 45 years of age in the present study. Also, females showed higher oral presentation of about 33 patients and 29 patients were males.
In a report of three vitiligo cases by Dummett et al.,[17] one patient had complete clinical depigmentation of all the oral tissues and another patient with history of heavy gingival pigmentation showed pink edentulous ridges at the time of examination.
Mucosal involvement occurring frequently in lips, genitals, gingival, areolar and nipples have been reported in the literature.[2] Solitary presentation of palatal depigmentation in a vitiligo patient was reported by Lawoyin et al.[2]
Site of oral vitiligo in relation to gender and age
Lip
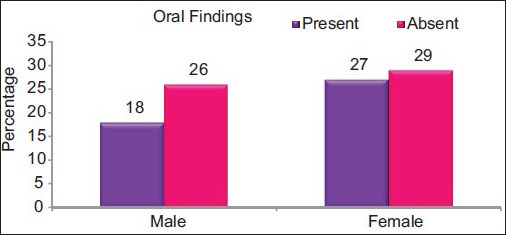
In our study 42 patients presented lip depigmentation out of which 20 were males and 22 females. Age range up to 25 years with lip involvement was noted in 7 patients, 25-35 years of age range showed 6 patients, 10 patients with lip involvement were within 35-45 years, 45-55 years of age showing lip depigmentation in 11 patients and above 55 years 8 patients presented lip depigmentation [Figure 1].
Figure 1.

Depigmentation in lip
Buccal mucosa
Among 100 patients in our study depigmentation of buccal mucosa was present in five patients in which three were males and two females. With age of range up to 25 years none, within 25-35 years of age two patients, among patients of age 35-45 years two patients, within age range of 45-55 years one patient and above 55 years of age none of the patients showed depigmentation in buccal mucosa [Figure 2].
Figure 2.

Depigmentation in palate
Labial mucosa
In the present study labial mucosa showed depigmentation in a male patient and four female patients. The following age ranges of up to 25 years, 25-35 years, 35-45 years, 45-55 years, above 55 years presented depigmentation of labial mucosa in one patient, none, three patients, one patient and none, respectively [Figure 3].
Figure 3.

Depigmentation in buccal mucosa
Palate
In our study palatal depigmentation was found in eight patients out of them five patients were males and three were females. Up to age range of 25 years one patient had palatal depigmentation, 25-35 years of range showed none, within age of 35-45 years three patients, 45-55 years of age range two patients and above 55 years of age two patients showed depigmentation in palate [Figure 4].
Figure 4.
Depigmentation in labial mucosa
Gingiva
Our study showed two patients with gingival depigmentation. With respect to age of up to 25 years, 25-35 years, 45-55 years age none showed gingival depigmentation. Patients within the age range of 35-45 years and above 55 years showed one patient each with depigmentation of gingiva [Figure 5].
Figure 5.

Depigmentation in gingiva
Oral manifestation as only finding
Among the 100 patients in our study 2 patients showed oral depigmentation as the only manifestation of vitiligo both manifestating in the lip. In relation to age up to 25 years one patient and 35-45 years one patient showed oral depigmentation.
Depigmentation of oral mucosa can be noted as an early feature in oral submucous fibrosis. In reverse smoking the palatal changes can show areas of depigmentation.[18,19] These depigmentations are excluded based on the clinical history.
In our study no relation of previous dental procedures to the depigmentation was noted. As far as our knowledge no literature states about the koebner phenomenon as a cause for oral vitiligo.
Conclusion
Vitiligo lesions presenting as skin depigmentation may also show oral mucosal depigmentation with lip and palate being the most common sites. Sometimes oral depigmentation may be the first indicator of vitiligo which may manifest in unnoticeable areas. In such case, dental surgeons can create awareness about vitiligo. So educating patients regarding oral depigmentation and possibility of occurrence in other parts of body will help in the earlier commencement of treatment, thereby battling against a socially distressing disorder could be possible.
What is new?
Very few articles have been published regarding oral manifestations of vitiligo. These articles report depigmentation of lip, palate and gingiva. In our study we have identified the presence of depigmentation of labial mucosa and buccal mucosa as well.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Moretti S. Giannotti B, editor. Vitiligo. [Last accessed on 2014 Dec 11]. Available from: http://www.orpha.net/data/patho/GB/uk-.vitiligo.pdf .
- 2.Lawoyin D, Brown R, Reid E, Sam F, Obayomi T. Concurrent presentation of cutaneous and oral soft tissue vitiligo: A case report and literature review. The Int J of Dent Sci. 2007;5:56–60. [Google Scholar]
- 3.Kavuossi H. Induction of depigmentation in a universal vitiligo patient with combination of cryotherapy and phenol. J Pak Assoc Dermatol. 2009;19:112–4. [Google Scholar]
- 4.Herane MI. Vitiligo and leukoderma in children. Clin Dermatol. 2003;21:283–95. doi: 10.1016/s0738-081x(03)00048-8. [DOI] [PubMed] [Google Scholar]
- 5.Oyarbide-Valencia K, van den Boorn JG, Denman CJ, Li M, Carlson JM, Hernandez C, et al. Therapeutic implications of autoimmune vitiligo T cells. Autoimmun Rev. 2006;5:486–92. doi: 10.1016/j.autrev.2006.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta R. 1st ed. Delhi, India: Atlantic Publishers and Distributors (P) Ltd; 2007. Leucoderma( Vitiligo) Book review; p. 1. [Google Scholar]
- 7.Dawber RP. Clinical associations of vitiligo. Postgrad Med J. 1970;46:276–7. doi: 10.1136/pgmj.46.535.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shajil EM, Agarwal D, Vagadia K, Marfatia YS, Begum R. Vitiligo: Clinical profiles in Vadodara, Gujarat. Indian J Dermatol. 2006;51:100–4. [Google Scholar]
- 9.Sehgal VN, Srivastava G. Vitiligo: Compendium of clinico-epidemiological features. Indian J Dermatol Venereol Leprol. 2007;73:149–56. doi: 10.4103/0378-6323.32708. [DOI] [PubMed] [Google Scholar]
- 10.Misri R, Khopkar U, Shankarkumar U, Ghosh K. Comparative case control study of clinical features and human leukocyte antigen susceptibility between familial and nonfamilialvitiligo. Indian J Dermatol Venereol Leprol. 2009;75:583–7. doi: 10.4103/0378-6323.57719. [DOI] [PubMed] [Google Scholar]
- 11.Alzolibani AA, Al Robaee A, Zedan K. Park KK, Murase JE, editors. “Vitiligo: Management and treatment” and Chapter “ Genetic epidemiology and heritability of Vitiligo”. InTech. 2011:17. [Google Scholar]
- 12.Chanda M, Dey SK, Gangopadhyay DN, Choudhuri SC, Roy A. Thyroid function in vitiligo. Indian J Dermatol. 1996;41:125–8. [Google Scholar]
- 13.Shameer P, Prasad VS, Kaviarasan PK. Serum zinc level in vitiligo: A case control study. Indian J Dermatol Venereol Leprol. 2005;71:206–7. doi: 10.4103/0378-6323.16243. [DOI] [PubMed] [Google Scholar]
- 14.Nigam PK, Patra PK, Khodiar PK, Gual J. A study of blood CD3+, CD4+ and CD8+ T cell levels and CD4+: CD8+ ratio in vitiligo patients. Indian J DermatolVenereolLeprol. 2011;77:111. doi: 10.4103/0378-6323.74993. [DOI] [PubMed] [Google Scholar]
- 15.Pandya V, Parmar KS, Shah BJ, Bilimoria FE. A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393–7. doi: 10.4103/0378-6323.18942. [DOI] [PubMed] [Google Scholar]
- 16.Gonul M, Cakmak SK, Soylu S, Kilic A, Gul U. Serum vitamin B12, folate, ferritin and iron levels in Turkish patients with vitiligo. Indian J DermatolVenereolLeprol. 2010;76:448. doi: 10.4103/0378-6323.66611. [DOI] [PubMed] [Google Scholar]
- 17.Dummett CO. The oral tissues in vitiligo. Oral Surg Oral Med Oral Patho l. 1959;12:1073–9. doi: 10.1016/0030-4220(59)90315-9. [DOI] [PubMed] [Google Scholar]
- 18.Sitheeque M, Ariyawardana A, Jayasinghe R, Tilakaratne W. Depigmentation oforal mucosa as the earliest possible manifestation of oral submucous fibrosis in SriLankan preschool children. J InvestigClin Dent. 2010;1:156–9. doi: 10.1111/j.2041-1626.2010.00021.x. [DOI] [PubMed] [Google Scholar]
- 19.Shafer, Hine, Levy . Shafer's Textbook of Oral Pathology. In: Rajendran R, Sivapathasundaram B, editors. Noida India: Reed Elsevier India Private Limited; 2006. p. 134. [Google Scholar]


