Abstract
Kaposi's sarcoma (KS) is a malignant proliferation of the endothelial cells. It typically presents with several vascular nodules on the skin and other organs. The penile localization of KS, particularly on the shaft area, is exceptional. We report an HIV-positive 34-year-old man who had multiple purplish-black plaques on his extremities and several small violaceous macules on the glans and shaft of the penis. Kaposi's sarcoma was diagnosed by histopathology.
Keywords: HIV, Kaposi's sarcoma, penile lesion
What was known?
Kaposi's sarcoma is a cancer that develops from the cells that line lymph or blood vessels.
KS can cause serious problems or even become life threatening when the lesions are in the liver lungs, or digestive tract.
AIDS-related KS, HAART has been shown to prevent or induce regression of this tumor.
Introduction
Kaposi's sarcoma (KS) is the most common malignancy among patients with acquired immune deficiency syndrome. The precise origin of this pathology is still unclear, but the current investigation is the narrow link between the appearance of the Kaposi's sarcoma and the infection by human herpes virus 8. The initial lesion of AIDS-associated KS generally develops on the trunk, face, or oral mucosa. The presentation of this tumor on the penis is extremely rare.[1]
Case Report
A 34-year-old heterosexual man with co-infection of HIV and HCV for 5 years was referred to our center due to fever, dyspnea, weight loss, and icterus. He had been taking highly active anti-retroviral therapy (HAART) (Zidovudine 300 mg/bid, Lamivudine 300 mg/bid, Efavirenz 600 mg/d) regularly since a year prior to his admission. He had a history of intravenous drug abuse with a Norgesic substance (Buprenorphine plus Dexamethansone), which stopped 5 years ago. In addition, he was hospitalized 1 year ago because of the pulmonary tuberculosis with continuation of anti-tuberculosis drugs for 6 months.
On admission to our hospital, he was toxic, dyspneic and febrile with oral temperature 40°C, respiratory rate 24 per/min, pulse rate 134 per/min, and blood pressure 110/60 mg/Hg. Peripheral blood leukocyte count was 4000/uL, hemoglobin 6 g/dl, platelet count 34000/uL, total bilirubin 15 mg/dl and direct 10 mg/dl, alanine aminotransferase 31 IU/L, aspartate aminotransferase 22 IU/L, and lactate dehydrogenase 512 IU/L. The patient was severely immunosuppressed with CD4 lymphocyte counts 79/mm3, plasma HIV viral load 395722 IU/ml, and HCV viral load was 21900 IU/ml. On physical examination, there were multiple purplish-black plaques on his arms and feet. Also, several small violaceous macules ranged from 2 mm to 1 cm were observed on the glans and shaft of the penis, which had started gradually over the last year [Figure 1].
Figure 1.

Violaceous macules localized on the glans and shaft of the penis
Sonography study demonstrated hepatosplenomegaly, and spiral computed tomography scan of the thorax was shown bilateral pleural effusion with consolidation in the upper lobe of the right lung. Finally, sputum mycobacteriological examination was positive for Mycobacterium tuberculosis; therefore, a relapse of pulmonary tuberculosis was diagnosed. A modified anti-tuberculosis medication (Ethambutol 800 mg/d, Amikacin 500 mg/d, and Ofloxacin 600 mg/d) was started in this patient due to abnormal liver function.
Ultimately, skin biopsy of the lesions of foot and penis was performed for histopathologic examination. Hematoxylin and eosin-stained sections revealed a marked dermal neovascularization with spindle cells proliferation and also nuclear atypia compatible with Kaposi's sarcoma [Figure 2]. Moreover, nested polymerase chain reaction (PCR) for human herpes virus-8 (HHV8) was also positive in the penile tissue [Figure 3].
Figure 2.
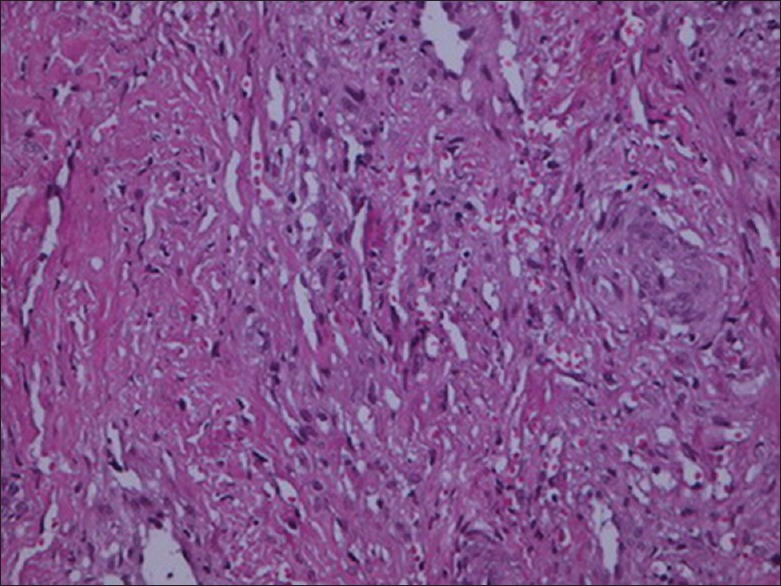
Penile lesion; Irregular vascular spaces, and spindle-shaped cells with extravasated RBCs (H and E, ×40)
Figure 3.
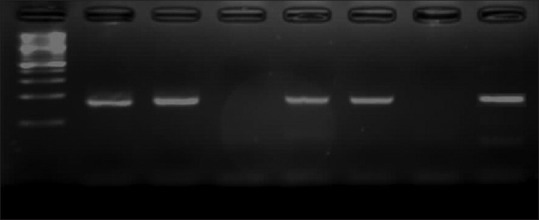
Electrophoresis of the Nested PCR products for detection of HHV-8. Line 1: 100 bp ladder marker, Line 2: Whole blood sample of studies case, Line 3: Plasma sample of studied case, Line 4: Negative control (human DNA), Line 5 and 6: Penile biopsy tissue of studies case, Line 7: Non-template control (double distilled water), Line 8: Positive control
Our patient was referred for chemotherapy treatment with Vinblastine, but he deferred it and discharged himself from hospital.
Discussion
Kaposi's sarcoma can be categorized into 4 distinct forms: Endemic, classic, iatrogenic, and AIDS- associated.[2] Penile KS is uncommon; majority of reports are from HIV-negative patients, especially who were homosexual and appears to have an aggressive behavior.[3] The areas more often involved on the penis are glans, foreskin, coronal sulcus, frenulum, and urethral meatus.[4] However, involvement of the shaft of penis is extremely unusual, and it is typically associated with lesions located on the glans or coronal sulcus.[5] The majority of the previous reported penile KS have been located on the glans, especially in HIV-negative patients and are also limited to the genitalia area.[3,4,6] Our patient was notable due to the involvement of the shaft of the penis in addition to the glans. Also, it was not limited to the genitalia and simultaneously involved to the upper and lower extremities.
The differential clinical diagnosis includes balanitis, Bowen's disease, molluscum contagiosum, and condiloma acuminate.[6] The decisive diagnosis is established by biopsy that the histological pattern is similar to that of Kaposi's sarcoma seen in other sites of the body.[3] The exact pathogenesis of KS is uncertain. Recent data showed a correlation between all types of KS and infection with HHV-8, known as KS-associated herpes virus (KSHV).[4] It assumes that the route of HHV-8 transmission might be both sexual and non-sexual. The detection of HHV-8 antibodies in children and nuns without sexual activity proposes the non-sexual route; on the other hand, high HHV-8 seroprevalence in individuals with high-risk sexual activity represents the sexual route. Additionally, it was reported that saliva could be a potential source of spread of HHV-8 in the general population.[7]
There have been several studies documented complete remission of KS with HAART medication and support its efficacy as a first step of therapy in the management of this malignancy in HIV patients.[8] Alternatively, for the advanced disease, additional therapy is needed, for instance, chemotherapy with the liposomal forms of doxorubicin and daunorubicin.[9] HIV suppression with anti-retroviral therapy is believed to be crucial and is considered the best factor of response. This might be related to the consequent suppression of HHV-8 replication and a reduction in the HIV-associated Tat protein, which is angiogenic and anti-apoptotic.[10]
Conclusion
Report of this case highlights the importance of cutaneous lesions in patients with HIV infection. Although the penile Kaposi's sarcoma is relatively uncommon among HIV-positive men, clinicians should consider its possibility. Usually, histopathologic evaluation is necessary to establish the diagnosis.
What is new?
In patients with HIV infection, Kaposi's sarcoma may involve shaft and glans of penis and concurrent lesions may be found in extremities.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Franceschi S, Maso LD, Rickenbach M, Polesel J, Hirschel B, Cavassini M, et al. Kaposi sarcoma incidence in the Swiss HIV Cohort Study before and after highly active antiretroviral therapy. Br J Cancer. 2008;99:800–4. doi: 10.1038/sj.bjc.6604520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morelli L, Pusiol T, Piscioli F, Hofler H, Weirich G, Werner M, et al. Herpesvirus 8-associated penile Kaposi's sarcoma in an HIV-negative patient: First report of a solitary lesion. Am J Dermatopathol. 2003;25:28–31. doi: 10.1097/00000372-200302000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Chitale SV, Peat D, Meaden JD, Johnson HB, Burgess NA. Kaposi's sarcoma of the glans penis in an HIV negative patient. Int Urol Nephrol. 2002;34:251–3. doi: 10.1023/a:1023239018160. [DOI] [PubMed] [Google Scholar]
- 4.Gonen M, Cenker A, Kiyici H, Kalkan M. Penile Kaposi's sarcomas in a circumcised and HIV-seronegative patient. Int J Urol. 2006;13:318–20. doi: 10.1111/j.1442-2042.2006.01282.x. [DOI] [PubMed] [Google Scholar]
- 5.Micali G, Nasca MR, De Pasquale R, Innocenzi D. Primary classic Kaposi's sarcoma of the penis: Report of a case and review. J Eur Acad Dermatol Venereol. 2003;17:320–3. doi: 10.1046/j.1468-3083.2003.00747.x. [DOI] [PubMed] [Google Scholar]
- 6.Pacifico A, Piccolo D, Fargnoli MC, Peris K. Kaposi's sarcoma of the glans penis in an immunocompetent patient. Eur J Dermatol. 2003;13:582–3. [PubMed] [Google Scholar]
- 7.Zargari O. Exclusive penile Kaposi's sarcoma: Report of an HIV-negative man successfully treated with radiotherapy. J Eur Acad Dermatol Venereol. 2006;20:318–20. doi: 10.1111/j.1468-3083.2006.01423.x. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen HQ, Magaret AS, Kitahata MM, Van Rompaey SE, Wald A, Casper C. Persistent Kaposi sarcoma in the era of highly active antiretroviral therapy: Characterizing the predictors of clinical response. AIDS. 2008;22:937–45. doi: 10.1097/QAD.0b013e3282ff6275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Northfelt DW, Dezube BJ, Thommes JA, Miller BJ, Fischl MA, Friedman-Kien A, et al. Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi's sarcoma: Results of a randomized phase III clinical trial. J Clin Oncol. 1998;16:2445–51. doi: 10.1200/JCO.1998.16.7.2445. [DOI] [PubMed] [Google Scholar]
- 10.Martinez V, Caumes E, Gambotti L, Ittah H, Morini JP, Deleuze J, et al. Remission from Kaposi's sarcoma on HAART is associated with suppression of HIV replication and is independent of protease inhibitor therapy. Br J Cancer. 2006;94:1000–6. doi: 10.1038/sj.bjc.6603056. [DOI] [PMC free article] [PubMed] [Google Scholar]


