Abstract
Systemic Lupus Erythematosus (SLE) is a multisystem disorder characterized by production of numerous autoantibodies, some of which have pathogenic consequences and result in considerable morbidity. Herein, we present a case of 48-year-old female with SLE having autoimmune hemolytic anemia, autoimmune thrombocytopenia, renal involvement, and recurrent flares of skin manifestations. She did not respond to the conventional therapy and was controlled and treated with Rituximab, a chimeric, monoclonal antiCD20 antibody, which specifically depletes B lymphocytes.
Keywords: Rituximab, systemic lupus erythematous, thrombocytopenia
What was known?
Systemic steroids are used to treat autoimmune thrombocytopenia in SLE
Introduction
SLE is a multisystem disorder, characterized by production of numerous autoantibodies, some of which have pathogenic consequences and result in considerable morbidity. Autoimmune thrombocytopenia is a common manifestation of SLE.[1] Medications for treatment include steroids as the first line therapy. But, many patients require immunosuppressive or other therapies to control the disease and prevent relapses.[2] Rituximab is a chimeric, monoclonal antiCD20 antibody, which specifically depletes B cells. It has demonstrated effectiveness in various autoimmune hematological disorders.[3]
Case Report
A 48-year-old lady, known case of SLE from last 2 years, was admitted with fever, malaise, weakness, rash on the face, and swelling of the right knee joint since 1 month.
General examination revealed pallor and fever with temperature of 37.6°C.
Cardiovascular, respiratory, abdominal, and central nervous system examination were normal.
Dermatological examination revealed erythematous malar rash and ulcers over the buccal mucosa. Right knee joint was swollen with painful movements. There was no effusion of the knee joint.
Her investigations were as followed: Hb 9 gm%, white cell count 17200/mm3 polymorphs 92%, platelet count1, 31,000/mm3, ESR 75 mm/hour, LDH 219 U/L, serum creatinine 1.53 mg/dl and 24 hour urinary protein 1.94 gm/dl. Anti-nuclear antibody, Anti-double stranded DNA, Rheumatoid factor, and direct Coomb's test was positive.
She was diagnosed as a case of SLE with autoimmune hemolytic anemia with renal involvement.
She was treated with 40 mg dexamethasone IV for 4 days followed by oral prednisolone 1 mg/kg/day along with azathioprine 50 mg daily and hydroxychloroquine 200 mg daily and sunscreen lotion. Her condition improved, and she was discharged from the hospital.
After 4 weeks, the patient was re-admitted with high-grade fever and hematuria. Her hemoglobin was 7 gm%, white cell count 6880/mm3, platelet count 30,000/mm3, serum creatinine 2.21 mg/dl, urine examination showed albumin 3+ with plenty of pus cells. Her urine culture grew E. coli, which was sensitive to ceftriaxone and amikacin. Blood sugar level was above 400 mg%. No purpura or cutaneous bleed were seen.
The clinical and laboratory features indicated active lupus with thrombocytopenia in spite of immunosuppressive therapy. Hence, we considered the use of Rituximab. After informed written consent, she was administered 1st dose of Rituximab 1 gm IV with cardiac monitoring in the ICU. She was also given antibiotics and insulin.
She showed no adverse effects and clinically improved within 3-4 days. On discharge, her platelet count was 64,000/mm3 and serum creatinine 1.69 mg/dl. The dose of oral prednisolone was tapered to 20 mg/day rapidly within 15 days. Tablet azathioprine and hydroxychloroquine were continued.
She received 2nd dose of rituximab exactly after 15 days without any adverse events.
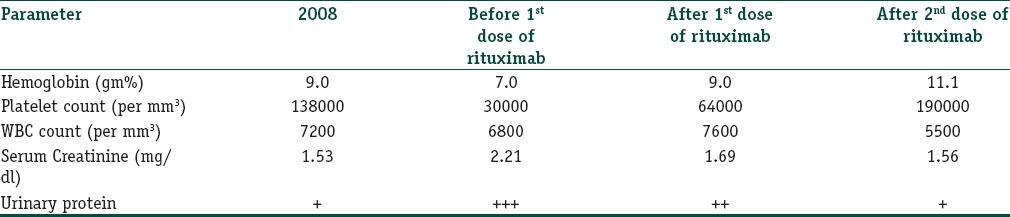
Within 1 week, she showed dramatic improvement. Her platelet count was 1,90,000/mm3, serum creatinine 1.56 mg/dl, and urine examination showed only trace albumin [Table 1].
Table 1.
The various parameters during course of hospitalization
After 2 doses of Rituximab, her dose of oral prednisolone was further tapered to 2.5 mg alternate day. Azathioprine was completely stopped. She is on regular follow-up for last 4 yrs without any recurrence.
Discussion
SLE is a multisystem disorder, characterized by production of numerous autoantibodies, some of which have pathogenic consequences and result in considerable morbidity. The American College of Rheumatology (ACR) criteria summarizes features necessary to diagnose SLE.[1] The presence of 4 of the 11 criteria yields a sensitivity of 85% and a specificity of 95% for SLE. In the present study, more than 4 criteria were present.
Thrombocytopenia is a common manifestation in SLE, its prevalence ranging from 7% to 30% of patients, with the American College of Rheumatology (ACR)[1] defining it as a platelet count less of than 100,000/mm.[3] Steroids are still the first line of treatment, but many patients require immunosuppressive or other therapies to control the disease and prevent relapses.[4,5] Refractory thrombocytopenia occurs when conventional treatment with steroids fails and a platelet count is less than 30,000/mm3 or clinical bleeding is seen, constituting a poor prognostic factor associated with elevated mortality.[6,7]
Rituximab is a chimeric mouse-human monoclonal antibody against a transmembrane protein, the CD20 antigen; present on B lymphocytes. CD20 antigen is present on all stages of B cell development except plasma cells, immunoglobulin production is not affected, and the risk of infections is not increased. Rituximab results in inhibition of B cell proliferation, apoptosis, and lysis through complement-dependent and complement- independent mechanisms.[8] Preliminary results of treatment with rituximab confirmed its efficacy and safety in subjects with SLE.[9]
The present patient had severe and recurrent flares of lupus, which was difficult to manage with standard medications including corticosteroids, hydroxychloroquine, and azathioprine. Intense immunosuppression resulted in infections, requiring multiple hospital admissions. Rituximab administration helped in steroid sparing with satisfactory improvement in skin rash, fever, thrombocytopenia, and renal symptoms. The response in our case was similar to that seen by Hua et al.[10]
Thus, we conclude that Rituximab therapy is promising and an effective alternative in the treatment of thrombocytopenia secondary to SLE.
What is new?
Steroid resistant thrombocytopenia in SLE can be successfully treated with Rituximab
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Tan EM, Cohen AS, Fries JF, Masi AT, Mc Shane DJ, Rothfield NF, et al. The Revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 2.Calverley D, Jones G, Kelton J. Splenic radiation for corticosteroid-resistant immune thrombocytopenia. Ann Intern Med. 1992;116:977–81. doi: 10.7326/0003-4819-116-12-977. [DOI] [PubMed] [Google Scholar]
- 3.Franchini M, Veneri D, Lippi G, Stenner R. The efficacy of rituximab in the treatment of inhibitor-associated hemostatic disorders. Thromb Haemost. 2006;96:119–25. [PubMed] [Google Scholar]
- 4.Roach B, Hutchinson G. Treatment of refractory systemic lupus erythematosus associated thrombocytopenia with intermittent low-dose intravenous cyclophosphamide. Arthritis Rheum. 1993;36:682–4. doi: 10.1002/art.1780360516. [DOI] [PubMed] [Google Scholar]
- 5.Godeau B, Oksenhendler E, Bierling P. Dapsone for autoimmune thrombocytopenic purpura. Am J Hematol. 1993;44:70–2. doi: 10.1002/ajh.2830440117. [DOI] [PubMed] [Google Scholar]
- 6.Moss K, Ioannou Y, Sultan SM, Haq I, Isenberg DA. Outcome of a cohort of 300 patients with systemic lupus erythematosus attending a dedicated clinic for over two decades. Ann Rheum Dis. 2002;61:409–13. doi: 10.1136/ard.61.5.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ward MM, Pyun E, Studenski S. Mortality risks associated with specific clinical manifestations of systemic lupus erythematosus. Arch Intern Med. 1996;156:1337–44. [PubMed] [Google Scholar]
- 8.Salama AD, Pusey CD. Drug insight: Rituximab in renal disease and transplantation. Nature Clin Pract Nephrol. 2006;2:221–30. doi: 10.1038/ncpneph0133. [DOI] [PubMed] [Google Scholar]
- 9.Looney RJ, Anolik JH, Campbell D, Felgar RE, Young F, Arend LJ, et al. B cell depletion as a novel treatment for systemic lupus erythematosus: A phase I/II dose-escalation trial of rituximab. Arthritis Rheum. 2004;50:2580–9. doi: 10.1002/art.20430. [DOI] [PubMed] [Google Scholar]
- 10.Chen H, Zheng W, Su J, Xu D, Wang Q, Leng X, et al. Low-dose rituximab therapy for refractory thrombocytopenia in patients with systemic lupus erythematosus-a prospective pilot study. Rheumatology (Oxford) 2011;50:1640–7. doi: 10.1093/rheumatology/ker176. [DOI] [PubMed] [Google Scholar]


