Abstract
We examine progress towards the 1994 International Conference on Population and Development (ICPD) commitment to provide universal access to sexual and reproductive health (SRH) services by 2014, with an emphasis on changes for those living in poor and emerging economies. Accomplishments include a 45% decline in the maternal mortality ratio (MMR) between 1990 and 2013; 11.5% decline in global unmet need for modern contraception; ~21% increase in skilled birth attendance; and declines in both the case fatality rate and rate of abortion. Yet aggregate gains mask stark inequalities, with low coverage of services for the poorest women. Demographic and Health Surveys and Multiple Indicator Cluster Surveys from 80 developing countries highlight persistent disparities in skilled birth attendance by household wealth: in 70 of 80 countries (88%), ≥80% of women in the highest quintile were attended by a skilled provider at last birth; in only 23 of the same countries (29%) was this the case for women in the lowest wealth quintile. While there have been notable declines in HIV incidence and prevalence, women affected by HIV are too often bereft of other SRH services, including family planning. Achieving universal access to SRH will require substantially greater investment in comprehensive and integrated services that reach the poor.
Keywords: sexual and reproductive health, maternal health, ICPD
Background
A hallmark of the 1994 International Conference on Population and Development (ICPD) Programme of Action (POA) (United Nations Population Fund [UNFPA], 1995) was the consensus that increasing access to sexual and reproductive health (SRH), and protecting human rights especially of women and adolescents, would ultimately secure a better future for all. To achieve these objectives, ICPD affirmed the commitment by member states to make comprehensive SRH services accessible to all persons through the primary health care system by 2014. States reaffirmed that commitment in the 1999 Key Actions (UNFPA, 1999), specifying the need to strengthen ‘basic health care systems, from which people living in poverty in particular can benefit’, and Millennium Development Goal (MDG) 5B reaffirmed that universal access to reproductive health is a global priority. This paper examines progress towards those goals through a review of trends in key SRH outcomes, and the use of related services over the past two decades.
Improvements in SRH outcomes have been considerable since ICPD, reflecting growing public and government support for gender equality, widespread gains in primary education, breakthroughs in communications technology, a decline in the number of persons living in extreme poverty and improvements in health systems themselves. Yet aggregate gains in SRH outcomes mask substantial inequalities, and people's ability to exercise their reproductive rights is neither universal nor equitable. While the number of maternal deaths per 100,000 live births (the maternal mortality ratio, MMR) fell by 45% over the past two decades, 800 women a day still die from causes related to pregnancy and childbirth; and while use of modern contraceptives has increased by 10% since ICPD, an estimated 25% of reproductive age women in Africa still have an unmet need for contraception (United Nations Department of Economic and Social Affairs [UNDESA], Population Division, 2014b; UNFPA, 2012a). As anti-retroviral (ARV) drugs have averted an estimated 5.2 million deaths in low- and middle-income countries (LMICs), new treatment guidelines (World Health Organization [WHO], 2013b) suggest more than 65% of treatment-eligible persons need care (UNAIDS, 2013). Further, the celebrated decline in new HIV infections coincides with vastly unequal progress between countries (UNAIDS, 2013), and rising HIV incidence in parts of Eastern Europe, Central Asia, the Middle East and North Africa (UNAIDS, 2013).
The current paper examines inequalities in SRH outcomes and services both between and within regions and countries, highlighting wealth differentials in access to both skilled attendance at birth, and the use of modern contraception. National and state briefs published in this same series describe policy conditions that have enhanced or obstructed progress towards universal SRH since ICPD in diverse settings, emphasising the essential and persistent need for greater state investments, cooperation between governments and civil society, more accountability, and greater recognition that comprehensive health system investments will be needed to achieve progress in SRH at significant scale. Regional and national distinctions in SRH coverage are notable, but the overall findings underscore the persistent unmet need to increase access to services for the world's poorest women.
Methods
This review draws on multiple sources, including analyses undertaken for the Framework of Actions for the follow up to the Programme of Action of the ICPD Beyond 2014 (United Nations Economic and Social Council [UN-ECOSOC], 2014a, 2014b) and the corresponding summary by the same title (UN-ECOSOC, 2014a); publicly available data on service utilisation (e.g. skilled birth attendance, antenatal care [ANC], emergency obstetric and newborn care [EmONC]), and contraceptive prevalence collected through the Demographic and Health Surveys (DHS) (ICF International, 2014) and the Multiple Indicator Cluster Surveys (MICS) (select indicators are displayed by household wealth quintiles for the survey years noted) (UNICEF, 2014). Annual estimates of maternal mortality and incident cases of sexually transmitted infections (STIs) are based on values collected and published by the WHO; estimates of HIV prevalence, coverage of ARV therapy and incident infections are all based on data available from UNAIDS, including their national online reports. Estimates of urban versus rural access to the management of post-partum haemorrhage (PPH) were generated using publicly available data from the Maternal and Neonatal Effort Index (MNPI) project (MEASURE Evaluation PRH, 2014). All data sources are provided within the text.
Aggregate progress masks severe inequalities by wealth
Maternal mortality
Of all SRH outcomes, the greatest gains in the past two decades have been in reducing maternal death. In absolute numbers, more than half a million women died each year from largely preventable causes related to pregnancy and childbirth in 1994, a number estimated at 289,000 deaths in 2013 (WHO, 2014b). The MMR decreased from 380 in 1990 to 210 in 2013 (WHO, 2014b), a decrease of 45%.
Declines in MMR over the past 20 years reflect advances in both clinical and social determinants, including increased use of ANC, skilled attendance at delivery and EmONC; gains in female education, delays in the age of marriage and first birth; and a decrease in mortality related to abortion (WHO, 2013d, 2014b). A decomposition of the progress in reducing maternal death in South Asia (SA) since 1994, for example, suggests that approximately 32% of the reduction in the absolute number of maternal deaths was attributable to declining fertility enabled by greater use of contraception (Jain, 2011), a resulting lower number of pregnancies and better pregnancy spacing (Jain, 2011; WHO, 2014b). Vaidyanathan (2014) attributes a dramatic decline in MMR in the Indian state of Tamil Nadu from the mid-1980s to 2007–2009 to a combination of innovative financing that strengthened primary health care, and social reforms that enhanced women's empowerment (Acharya, Vaidyanathan, Muraleedharan, Dheenadayalan, & Dash, 2011; Gupta, Desikachari, Somanathan, & Padmanaban, 2009; International Institute for Population Science [IIPS] & Macro International, 2007; Muraleedharan, Dash, & Gilson, 2009; Padmanaban, Raman, & Mavalankar, 2009; Ramasundaram et al., 2001; State Health Society, 2012; Visaria, 2000; WHO, 2009b).
Differences in the risk of maternal death between developed and developing countries continue to be extreme. Women living in industrialised countries have a 1 in 4000 lifetime risk of dying of maternal causes, while the comparable risk of women in the least developed countries is 1 in 51, and in sub-Saharan Africa (SSA), the risk is 1 in 38 (WHO, 2014b).
Among the 50 countries with MMR ≥ 500 in 1990, eight have already achieved MDG 5, target A, i.e. to reduce the MMR by three quarters between 1990 and 2015 (WHO, 2014b); these countries include Bhutan, Cambodia, Equatorial Guinea, Eritrea, Lao People's Democratic Republic, Nepal, Rwanda and Timor-Leste. Another 17 have reduced MMR by ≥ 50% but less than 75%, while 25 countries have not yet reduced their 1990 MMR by 50%. All but one of these latter 25 countries are located in Africa (the exception being Haiti), where there continues to be inadequate coverage of skilled providers and SRH services, especially in rural or remote areas and slums (Ahman & Shah, 2011).
Antenatal care
The percentage of pregnant women who had at least one ANC visit increased globally from 63% in 1990 to 80% in 2010, an overall improvement of approximately 30%. Similar to maternal mortality, accomplishments mask regional disparities: in southern Africa 94% of women had one ANC visit in 2010, compared to only 67% in West Africa. In Latin America, nearly all women now have at least one ANC visit (96%) and 88% have at least four (ICF International, 2014; UNICEF, 2014).
Skilled attendance at birth
The proportion of deliveries attended by skilled health personnel is highly correlated with MMR (AbouZahr & Wardlaw, 2001; Ronsmans et al., 2003), and is among the strongest indicators of where health systems are able to reach women in reproductive emergencies. It is a better predictor of MMR than ANC coverage (Lancet Maternal Survival Series Steering Group, Campbell, & Graham, 2006), and is a valuable indicator of health system access, indicating the extent to which acute skilled care is available to pregnant women and to newborns in a given country. The worldwide proportion of skilled attendance rose from 57% in 1990 to 66% in 2010, a gain of approximately 15% (Figure 1), and by 2012 had reached 69% (United Nations, 2013). Despite this positive trend, access to skilled attendance remains highly inequitable between regions, countries and between women in the lowest and highest wealth quintiles within the same country. Recent DHS and MICS surveys (2004 or later), from 80 developing countries, highlight stark differentials in such access by household wealth in the last decade (Table 1).
Figure 1. The percentage of women who had a skilled attendant (doctor, nurse or mid-wife) at birth increased approximately 15% globally from 1990 to 2010, but with notable distinctions in progress between regions.
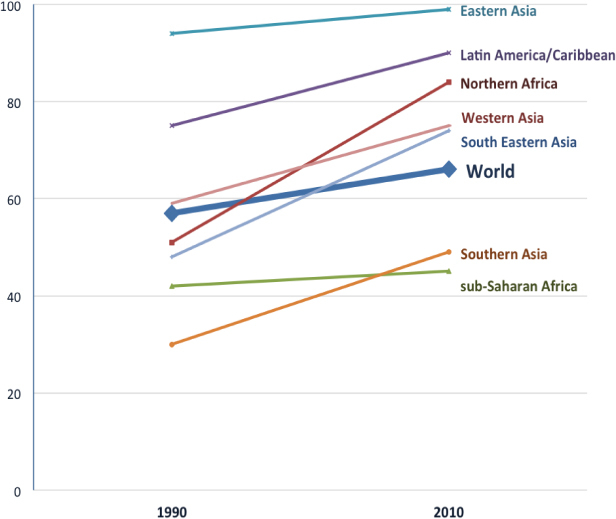
Source: DHS and MICS data, as reported in UN-ECOSOC (2014b).
Table 1. Coverage of skilled birth attendance at last birth (%), and modern contraceptive prevalence (%), by household wealth quintiles in 80 developing countries, 2004 or later.
| Skilled attendance at birth (%) |
Modern CPR (%) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Year | Source | Poorest 20% | Second 20% | Middle 20% | Fourth 20% | Richest 20% | Δ–highest to lowest | Poorest 20% | Second 20% | Middle 20% | Fourth 20% | Richest 20% | Δ–highest to lowest |
| Albania | 2008–2009 | DHS | 100 | 99 | 99 | 100 | 100 | 1 | 11 | 9 | 11 | 9 | 14 | 4 |
| Angola | 2006–2007 | MICS | 16 | 35 | 61 | 86 | 94 | 78 | – | – | – | – | – | – |
| Armenia | 2010 | DHS | 100 | 100 | 100 | 99 | 100 | 0 | 21 | 17 | 27 | 34 | 38 | 16 |
| Azerbaijan | 2006 | DHS | 76 | 88 | 91 | 99 | 100 | 24 | 11 | 11 | 10 | 18 | 21 | 10 |
| Bangladesh | 2011 | DHS | 12 | 19 | 28 | 43 | 64 | 52 | 53 | 54 | 52 | 51 | 51 | −2 |
| Belarus | 2005 | MICS | 100 | 100 | 100 | 100 | 100 | 0 | 49 | 53 | 59 | 60 | 59 | 9 |
| Belize | 2006 | MICS | 84 | 100 | 100 | 100 | 98 | 14 | – | – | – | – | – | – |
| Benin | 2006 | DHS | 59 | 72 | 82 | 93 | 98 | 39 | 2 | 4 | 5 | 7 | 13 | 11 |
| Bhutan | 2010 | MICS | 34 | 43 | 67 | 81 | 95 | 61 | 69 | 66 | 65 | 66 | 62 | −7 |
| Bolivia (Plurinational State of) | 2008 | DHS | 39 | 69 | 83 | 94 | 99 | 59 | 23 | 27 | 34 | 41 | 47 | 24 |
| Bosnia and Herzegovina | 2006 | MICS | 99 | 100 | 100 | 99 | 100 | 0 | 4 | 10 | 7 | 13 | 20 | 15 |
| Burkina Faso | 2010 | DHS | 51 | 64 | 74 | 83 | 96 | 45 | 7 | 9 | 10 | 16 | 34 | 26 |
| Burundi | 2010 | DHS | 55 | 59 | 64 | 66 | 83 | 28 | 15 | 14 | 17 | 17 | 26 | 12 |
| Cote d'Ivoire | 2006 | MICS | 29 | 40 | 59 | 79 | 95 | 66 | 3 | 5 | 6 | 10 | 18 | 15 |
| Cambodia | 2010 | DHS | 49 | 64 | 75 | 87 | 97 | 48 | 35 | 37 | 37 | 34 | 31 | −4 |
| Cameroon | 2011 | DHS | 19 | 56 | 78 | 91 | 98 | 79 | 2 | 8 | 14 | 22 | 26 | 23 |
| Chad | 2004 | DHS | 2 | 7 | 9 | 14 | 52 | 50 | 0 | 0 | 1 | 0 | 7 | 7 |
| Colombia | 2010 | DHS | 86 | 98 | 99 | 100 | 99 | 14 | 69 | 73 | 73 | 75 | 75 | 6 |
| Congo | 2005 | DHS | 69 | 78 | 92 | 98 | 99 | 30 | 9 | 7 | 12 | 16 | 18 | 9 |
| Democratic Republic of the Congo | 2010 | MICS | 60 | 68 | 69 | 85 | 96 | 36 | 1 | 2 | 3 | 7 | 14 | 13 |
| Dominican Republic | 2007 | DHS | 90 | 96 | 96 | 98 | 98 | 8 | 67 | 71 | 72 | 71 | 69 | 3 |
| Egypt | 2008 | DHS | 58 | 73 | 85 | 91 | 97 | 39 | 52 | 55 | 59 | 59 | 62 | 10 |
| Ethiopia | 2011 | DHS | 3 | 4 | 4 | 9 | 50 | 48 | 13 | 22 | 24 | 30 | 48 | 35 |
| Gambia | 2006 | MICS | 28 | 46 | 59 | 73 | 89 | 60 | – | – | – | – | – | – |
| Georgia | 2005 | MICS | 95 | 99 | 99 | 99 | 99 | 3 | 12 | 16 | 18 | 23 | 28 | 16 |
| Ghana | 2008 | DHS | 23 | 52 | 66 | 82 | 96 | 73 | 12 | 14 | 16 | 20 | 21 | 9 |
| Guinea | 2005 | DHS | 15 | 20 | 35 | 58 | 87 | 72 | 3 | 3 | 4 | 7 | 13 | 10 |
| Guinea-Bissau | 2006 | MICS | 19 | 26 | 31 | 54 | 79 | 59 | 1 | 2 | 3 | 9 | 19 | 18 |
| Guyana | 2009 | DHS | 82 | 96 | 96 | 98 | 97 | 15 | 31 | 39 | 43 | 41 | 45 | 14 |
| Haiti | 2012 | DHS | 10 | 21 | 38 | 55 | 78 | 68 | 30 | 30 | 35 | 34 | 28 | −7 |
| Honduras | 2005–2006 | DHS | 38 | 56 | 81 | 91 | 98 | 61 | 41 | 52 | 59 | 62 | 65 | 24 |
| India | 2005–2006 | DHS | 21 | 34 | 52 | 70 | 90 | 69 | 35 | 44 | 50 | 55 | 58 | 23 |
| Indonesia | 2007 | DHS | 47 | 69 | 80 | 89 | 96 | 50 | 50 | 60 | 59 | 59 | 58 | 8 |
| Jordan | 2007 | DHS | 99 | 99 | 100 | 100 | 100 | 2 | 35 | 38 | 41 | 49 | 47 | 12 |
| Kazakhstan | 2006 | MICS | 100 | 100 | 100 | 99 | 100 | 0 | 40 | 45 | 49 | 51 | 57 | 17 |
| Kenya | 2008–2009 | DHS | 23 | 32 | 42 | 56 | 82 | 59 | 17 | 33 | 43 | 50 | 48 | 31 |
| Kyrgyzstan | 2006 | MICS | 93 | 99 | 97 | 98 | 100 | 7 | 47 | 40 | 43 | 48 | 49 | 1 |
| Lao People's Democratic Republic | 2011–2012 | DHS/MICS | 11 | 24 | 45 | 64 | 91 | 80 | 33 | 41 | 47 | 49 | 40 | 7 |
| Lesotho | 2009 | DHS | 52 | 65 | 70 | 84 | 95 | 42 | 29 | 37 | 45 | 48 | 61 | 32 |
| Liberia | 2007 | DHS | 30 | 32 | 46 | 74 | 82 | 52 | 3 | 6 | 13 | 14 | 17 | 14 |
| Madagascar | 2008–2009 | DHS | 22 | 28 | 42 | 58 | 90 | 68 | 18 | 24 | 29 | 36 | 36 | 19 |
| Malawi | 2010 | DHS | 68 | 70 | 72 | 80 | 91 | 23 | 35 | 40 | 41 | 45 | 48 | 14 |
| Maldives | 2009 | DHS | 93 | 96 | 97 | 100 | 100 | 7 | 29 | 27 | 27 | 26 | 26 | −3 |
| Mali | 2012–2013 | DHS | 35 | 46 | 50 | 75 | 94 | 59 | 3 | 5 | 6 | 13 | 23 | 18 |
| Mauritania | 2007 | MICS | 21 | 41 | 71 | 90 | 95 | 75 | – | – | – | – | – | – |
| Mongolia | 2005 | MICS | 98 | 99 | 100 | 99 | 100 | 2 | 65 | 63 | 63 | 59 | 53 | −12 |
| Montenegro | 2006 | MICS | 98 | 99 | 100 | 98 | 100 | 3 | 8 | 18 | 17 | 19 | 23 | 15 |
| Morocco | 2003–2004 | DHS | 32 | 52 | 74 | 88 | 96 | 64 | 51 | 55 | 55 | 55 | 57 | 5 |
| Mozambique | 2008 | MICS | 37 | 45 | 53 | 66 | 89 | 52 | 5 | 5 | 9 | 15 | 30 | 25 |
| Namibia | 2006–2007 | DHS | 61 | 75 | 85 | 95 | 98 | 37 | 30 | 46 | 47 | 66 | 68 | 39 |
| Nepal | 2011 | DHS | 21 | 39 | 54 | 67 | 90 | 70 | 36 | 41 | 43 | 45 | 49 | 13 |
| Niger | 2012 | DHS | 12 | 18 | 21 | 29 | 71 | 59 | 9 | 8 | 8 | 13 | 24 | 15 |
| Nigeria | 2013 | DHS | 6 | 17 | 40 | 62 | 85 | 79 | 1 | 4 | 9 | 14 | 23 | 22 |
| Pakistan | 2006–2007 | DHS | 18 | 28 | 40 | 56 | 79 | 62 | 12 | 16 | 22 | 26 | 32 | 19 |
| Peru | 2007–2008 | DHS | 44 | 67 | 90 | 98 | 99 | 55 | 36 | 41 | 49 | 54 | 54 | 18 |
| Philippines | 2008 | DHS | 26 | 56 | 76 | 86 | 94 | 69 | 26 | 36 | 37 | 39 | 33 | 7 |
| Republic of Moldova | 2005 | DHS | 99 | 99 | 100 | 100 | 100 | 1 | 37 | 39 | 43 | 46 | 51 | 15 |
| Rwanda | 2010 | DHS | 70 | 72 | 76 | 82 | 91 | 21 | 39 | 41 | 47 | 49 | 50 | 11 |
| Sao Tome and Principe | 2008–2009 | DHS | 76 | 75 | 85 | 89 | 92 | 16 | 31 | 32 | 31 | 37 | 37 | 6 |
| Senegal | 2010–2011 | DHS | 30 | 52 | 74 | 87 | 95 | 65 | 4 | 7 | 12 | 15 | 23 | 18 |
| Serbia | 2010 | MICS | 99 | 100 | 100 | 100 | 100 | 0 | 11 | 17 | 20 | 25 | 31 | 21 |
| Sierra Leone | 2010 | MICS | 44 | 56 | 64 | 72 | 85 | 41 | 5 | 5 | 9 | 12 | 21 | 16 |
| Somalia | 2006 | MICS | 11 | 14 | 20 | 45 | 77 | 66 | 0 | 0 | 0 | 2 | 4 | 4 |
| Suriname | 2006 | MICS | 81 | 91 | 98 | 93 | 96 | 15 | 29 | 44 | 49 | 48 | 51 | 22 |
| Swaziland | 2010 | MICS | 65 | 76 | 87 | 89 | 94 | 29 | 55 | 60 | 62 | 66 | 68 | 13 |
| Syrian Arab Republic | 2006 | MICS | 78 | 95 | 98 | 97 | 99 | 21 | 29 | 37 | 44 | 48 | 53 | 23 |
| Tajikistan | 2005 | MICS | 70 | 81 | 87 | 90 | 91 | 21 | 26 | 32 | 32 | 36 | 39 | 13 |
| Thailand | 2006 | MICS | 93 | 98 | 98 | 99 | 100 | 7 | 79 | 79 | 75 | 74 | 70 | −8 |
| The Former Yugoslav Republic of Macedonia | 2005 | MICS | 95 | 99 | 98 | 100 | 100 | 5 | 8 | 10 | 6 | 8 | 17 | 9 |
| Timor-Leste | 2009–2010 | DHS | 12 | 16 | 24 | 41 | 71 | 59 | 15 | 16 | 17 | 24 | 32 | 17 |
| Trinidad and Tobago | 2006 | MICS | 98 | 99 | 94 | 99 | 100 | 2 | 37 | 34 | 35 | 39 | 45 | 8 |
| Uganda | 2011 | DHS | 45 | 53 | 58 | 63 | 91 | 46 | 13 | 21 | 25 | 31 | 39 | 26 |
| Ukraine | 2007 | DHS | 99 | 98 | 100 | 99 | 100 | 1 | 36 | 45 | 47 | 51 | 53 | 17 |
| United Republic of Tanzania | 2010 | DHS | 31 | 35 | 44 | 62 | 88 | 57 | 19 | 22 | 23 | 35 | 38 | 19 |
| Uzbekistan | 2006 | MICS | 100 | 100 | 100 | 100 | 100 | 0 | 61 | 60 | 61 | 58 | 57 | −4 |
| Vanuatu | 2008 | MICS | 55 | 78 | 73 | 87 | 90 | 35 | 28 | 40 | 34 | 39 | 44 | 16 |
| Viet Nam | 2011 | MICS | 72 | 96 | 100 | 100 | 99 | 27 | 65 | 62 | 60 | 55 | 58 | −7 |
| Yemen | 2006 | MICS | 17 | 20 | 32 | 50 | 74 | 56 | 5 | 9 | 19 | 29 | 35 | 30 |
| Zambia | 2007 | DHS | 26 | 27 | 36 | 72 | 92 | 65 | 31 | 24 | 23 | 39 | 48 | 18 |
| Zimbabwe | 2010–2011 | DHS | 46 | 55 | 62 | 79 | 90 | 44 | 52 | 53 | 56 | 60 | 64 | 11 |
Source: Demographic and Health and Multiple Indicator Cluster Surveys.
In 70 of 80 countries surveyed (88%), more than 80% of women in the highest wealth quintile were attended by a skilled provider at last birth, suggesting that most developing countries are able to provide skilled care at least for women in the wealthiest households. Of the 10 countries unable to provide skilled care even for pregnant women in the highest wealth quintile, five are in Africa (e.g. Chad, Ethiopia, Guinea-Bissau, Niger and Somalia); two in SA (Bangladesh, Pakistan); plus Haiti, Timor-Leste and Yemen. In contrast, in only 23 of the 80 countries surveyed (29%), were more than 80% of pregnant women in the lowest wealth quintile attended by a skilled provider at last birth, illustrating the present shortfall in achieving universal access to skilled delivery care. Coverage for pregnant women in the lowest wealth quintile ranged from 2% in Chad to 100% in Albania, Armenia, Belarus, Kazakhstan and Uzbekistan; no country in Africa or SA achieved 80% coverage of skilled attendance at birth for pregnant women in the poorest wealth quintile. Other regional disparities are notable: skilled attendance was nearly universal in 13 of the 15 European and Central Asian countries surveyed, with coverage between 93% and 100% across all quintiles except in Tajikistan and Azerbaijan, where differences in coverage between the highest and lowest quintiles were 21 and 24 percentage points, respectively (Table 1).
Among the six countries surveyed in SA, differentials in the coverage of skilled birth attendance between the lowest and highest wealth quintiles were far greater, e.g. more than 50 percentage points in Bangladesh, Bhutan, India, Nepal and Pakistan. Coverage for the wealthiest pregnant women reached 90% or greater in Bhutan, India, Nepal; while coverage for pregnant women from the lowest wealth quintiles of these countries was 34%, 21% and 21%, respectively, and reached only 12% and 18%, respectively, of the poorest women in Bangladesh and Pakistan (Table 1).
Among the 35 countries surveyed in SSA, the mean disparity between rich and poor (52 percentage points) was similar to that observed in SA, with skilled coverage for the wealthiest pregnant women above 90% in 20 of 35 countries, while the lack of coverage among the poorest quintile was particularly extreme. In 13 countries, fewer than 25% of the pregnant women in the lowest wealth quintile had skilled coverage, including only 6% in Nigeria (2013), 2% in Ethiopia (2011) and 2% in Chad (2004, with the 2014 DHS pending).
Changes in skilled care by wealth in a selection of countries since 1990 (Figure 2), illustrate the diversity in trends, with widening disparities in some countries (e.g. Bangladesh, Cameroon, Haiti, Nigeria and Peru), declining inequalities in others (e.g. Bolivia and Vietnam) and no change in a number of others (e.g. Philippines, Tanzania).
Figure 2. Trends from select countries display the changing inequalities by household wealth in the percentage of women who had a skilled attendant (doctor, nurse or mid-wife) at last birth between 1990 and 2010.
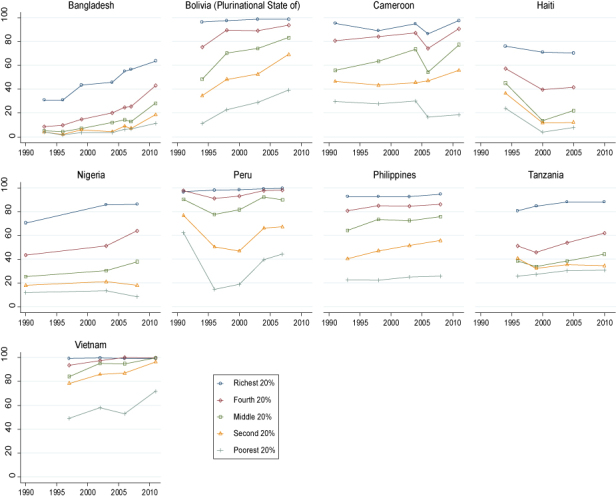
Source: DHS and MICS data, as reported in UN-ECOSOC (2014b).
Emergency obstetric and newborn care
Even with ANC and skilled attendance at birth, delivery complications arise in approximately 15% of all pregnancies, a majority of which can be managed if quality EmONC is accessible (UNICEF, WHO, & UNFPA, 1997). Yet, EmONC coverage remains seriously inadequate in developing countries (UNFPA, 2012b), and unmanaged pregnancy complications contribute to the estimated 289,000 maternal deaths each year (WHO, 2014b) with millions more suffering from chronic morbidities. Access to EmONC, expressed as the density of EmONC facilities per annual number of births, is correlated with lower MMR (Gabrysch, Zanger, & Campbell, 2012).
A majority of facilities that offer maternity care still fail to provide all functions required for classification as an EmONC facility (basic or comprehensive), and geographic and financial barriers persist (Gabrysch et al., 2012). Management of basic obstetric and neonatal emergencies includes the administration of oxytocics, antibiotics, anticonvulsants, manual extraction of the placenta, removal of retained products and neonatal resuscitation, while management of comprehensive EmONC includes capacity to perform C-section surgery in cases of obstructed labour, and blood transfusions. The rural versus urban differential in key components of EmONC (e.g. management of PPH) (Figure 3), reflect the continuing challenges of delivering services to women with structural obstacles to care (e.g. few or no transport options and poor or seasonal roads) (Gabrysch et al., 2012). The recommended minimum density of basic and comprehensive EmONC facilities differs depending on the metrics used (e.g. facilities per births or per population), but given the unpredictable nature of complications, the need for skilled care that can either manage all complications, or provide timely referral to comprehensive emergency care if complications arise, is not disputed (Campbell & Graham, 2006), only underscoring the continuing need to address the structural inadequacies in health systems (UN-ECOSOC, 2014a, 2014b).
Figure 3. Proportion of women in select Asian countries with access to management of post-partum haemorrhage in 2005, with specific focus on urban versus rural access.
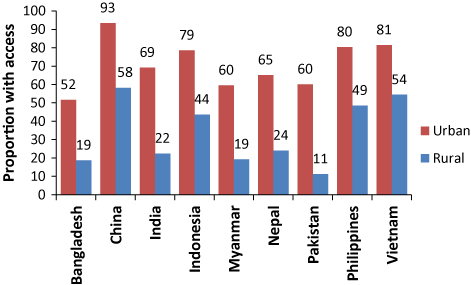
Source: UN-ECOSOC (2014b); Analysis based on data from the Maternal and Neonatal Program Effort Index (MNPI): http://www.policyproject.com/pubs/mnpi/getmnpi.cfm.
Fertility decline and increasing contraceptive use obscure unmet needs
Globally, the total fertility rate (TFR) fell by 23% between 1990 and 2010 (UNDESA, Population Division, 2013a). Aspirations for smaller families correspond to other changes in development, including increasing child survival and expanding opportunities for women, especially education. In Africa as a whole, and SSA in particular, fertility decline has been slower than in other regions, and despite large increases in the proportion of women using any method of contraception in the past two decades, contraceptive prevalence rates (CPR) remains low (especially CPR for modern methods), and TFRs are almost twice those in other regions (UNDESA, Population Division, 2014a, 2014b).
Global CPR increased from a median estimate of 58.7 in 1994 to 63.7% in 2014, an increase of approximately 8.5%. CPR in the least developed countries increased by 87% over the same period, admittedly from a lower starting point (20.7%), but reaching 38.8% in 2014. Despite these changes, overall contraceptive use remains rare in a number of extremely poor countries of Africa (e.g. in Chad, Guinea and South Sudan), where CPR is less than 10%. It should be noted that CPRs reflect the use among women age 15–49 who are married or in union, providing no data on use among single women; the importance of this limitation will increase in the near future, given that the age of first marriage, the proportion of women who never marry, and rates of divorce are all rising. Global use of modern methods of contraception (i.e. CPR for any modern method), increased from 51.9% in 1994 to 57.4% in 2012, a rise of approximately 11%; both overall CPR and CPR of modern methods increased more during the decade of the 1990s than it has since then (UNDESA, Population Division, 2014b; Alkema, Kantorova, Menozzi, & Biddlecom, 2013).
Global unmet need for modern contraception declined by 11.5% from 1994 to 2014; this masked dramatic declines in unmet need for modern methods in Eastern Europe (from 36.9% to 25.1%, a decrease of 32%), and Southern Europe (from 37.6% to 27.1%), a smaller decline in the least developed countries (from 33.3% to 29.2%, a change of 12.3%), and a mere 6.5% decline in SSA, from 32.3% to 30.2% (UNDESA, Population Division, 2014b; Cleland & Shah, 2013). In 2014, the unmet need for modern methods of contraception affects more than 30% of women in Africa, 34.2% in Western Asia and 41.8% in Polynesia; within Africa, the highest unmet need for modern methods is in Middle Africa (38%).
Differentials in modern CPR by household wealth (Table 1) were high in several countries (e.g. Yemen, Bolivia, Honduras), but generally more equitable than skilled attendance at birth, and a number of countries from all regions have both high and equitable modern CPR (e.g. with no wealth quintile at less than 50% CPR), e.g. Columbia, Dominican Republic, Bangladesh, Belarus, Bhutan, Egypt, Indonesia, Mongolia, Morocco, Swaziland, Thailand, Uzbekistan, Vietnam and Zimbabwe. In some countries from both East Asia and the Pacific (EAP) and SA, modern CPR is actually highest among women from poorer households. For example, in Bangladesh, Bhutan, Cambodia, Indonesia, the Maldives, Mongolia, Thailand and Vietnam, women in the poorest or second poorest households had the highest CPR.
Contraceptive method mix
The diversification of modern contraceptive methods over the past 20 years has been modest compared to the expansion of new methods that took place in the two decades preceding ICPD (Brache & Faundes, 2010; fhi360, 2013; Nelson, 2010; Power, French, & Cowan, 2007). Because clients differ in their method preferences and clinical needs (including, e.g. contraindications) over the life-course, a range of distinct contraceptive method types needs to be available to allow trial and error or periodic switching, and expanded choice increases contraceptive use (Ross, Hardee, Mumford, & Eid, 2002; Seiber, Bertrand, & Sullivan, 2007; Stover & Ross, 2010; Sullivan, Bertrand, Rice, & Shelton, 2006; UN-ECOSOC, 2014a, 2014b).
In 1994, global contraceptive method mix was dominated by widespread use of the intrauterine contraceptive device (IUD) in China, early and almost universal use of female sterilisation in India, and the use of pills, barrier methods and sterilisation in Europe and the Americas (UNDESA, Population Division, 1996). Twenty years later, these patterns have shifted within given countries, but the overall mix of contraceptive methods used has diversified only slightly, mostly by increased use of injectable methods, and to a lesser extent, contraceptive implants.
Without a choice of contraceptive methods, and quality provision of counselling, information and care, use of contraception is interrupted and unplanned pregnancies lead to an increase in the demand for abortion. Contraceptive services in Brazil are characterised by poor quality of counselling and limited choice, and the country has high rates of unplanned and unwanted pregnancies (see Diniz & Araujo, 2014; Curtis, 2012; Diniz & Medeiros, 2012; Diniz, d'Oliveira, & Lansky, 2012; do Carmo Leal et al., 2012; Ministerio de Saude, 2009; Silva & Surita, 2012; Victora et al., 2011; Vieira, 2012).
In the world's two largest countries, China and India, a majority of contraceptive users still rely on one or two methods, suggesting limited choice of commodities and/or limited knowledge and counselling capacity within family planning services. Since the outset of its family planning programme, China's family planning programme has relied heavily on the IUD (40.6% of all methods used in 2013) (UNDESA, Population Division, 2014a), using domestically manufactured IUDs that have increased in quality over time (Bilian, 2007; Kaufman, 1993). In 2013, approximately 28.7% women relied on female sterilisation, 4.5% relied on male sterilisation, and from 1988 to 2013, reliance on male condoms rose from 3.9% to 8.5% of all methods (UNDESA, Population Division, 2014b; Zheng et al., 2012). Despite the rise in condom use, sterilisation (both female and male) and the IUD still account for 73.8% of all contraceptive use, and only a minority of women use other reversible modern methods, e.g. pills, implants.
The high reliance on female sterilisation in India – 74% of modern method use in 2007–2008 – has been virtually unchanged since 1992–1993 (International Institute for Population Science [IIPS], 2010; UN-ECOSOC, 2014b), reflecting an under-resourced public health sector, as well as a legacy of widespread public distrust of state or private sector contraceptive promotion, among other factors (see Vaidyanathan, 2014), (Berer, 1993; Singh, Pallikadavath, Ram, Ogollah, & Noor, 2012). India faces a major challenge to strengthen health system capacity and accountability to improve promotion and quality provision of modern reversible methods (Oliveira, Dias, Padmadas, & Leone, 2014; Koenig, Foo, & Joshi, 2000).
Men's use of contraception
Europe is the region with the highest reliance on male condoms (25.2% of all methods used) (UNDESA, Population Division, 2014a), but use has increased among young people ages 15–24 years in many countries since 1994 (UN-ECOSOC, 2014b) and may not be captured in CPR estimates based on married women. Beyond condoms, male sterilisation offers the only modern means for men to assume responsibility for contraception, an explicit objective of the ICPD POA. Of 92 countries with more than two data points on the proportion of contraceptive prevalence attributable to male sterilisation (UNDESA, Population Division, 2013b), and with at least one data point during or since 2005, 38 countries (41.3%) report no use of male sterilisation, and in only 4 countries does male sterilisation contribute to more than 10% of contraceptive prevalence: the UK (21%), the Republic of Korea (16.8%), the USA (12.7%) and Bhutan (12.6%). Twenty-seven countries (29.3%) have actually seen declines in the relative use of male sterilisation since 1994, including Sri Lanka (−3.7%), India (−2.4%), Thailand (−1.9%), Myanmar (−1.4%) and the USA (−0.5%), suggesting either absolute declines in use of male sterilisation or increased reliance on other methods (UN-ECOSOC, 2014b; Darroch, 2008; UNDESA, Population Division, 2013a; 2013b).
Abortion continues to be widely used
Reliable, and especially comparative, abortion statistics are not easy to collect, but recent estimates suggest that the risk of death due to unsafe abortion has decreased from an estimated 69,000 deaths in 1990 to 47,000 in 2008 (Sedgh et al., 2012; UN-ECOSOC, 2014b). This is widely attributed to growing use of medical abortion, increasing legal provision for abortion, safer technologies and better standards for post-abortion care (Baggaley, Burgin, Campbell, & Gravenor, 2010; Dzuba, Winikoff, & Peña, 2013; Harper, Blanchard, Grossman, Henderson, & Darney, 2007; Ngo, Park, Shakur, & Free, 2011; Prata, Sreenivas, Vahidnia, & Potts, 2009).
The absolute number of abortions declined from 45·6 million in 1995 to 43.8 million in 2008, of which an estimated 22 million are unsafe (WHO, 2012b). The overall rate of abortions declined globally from 35 per 1000 women (ages 15–44 years) in 1995, to 28 per 1000 in 2003, but remained stable at 29 per 1000 in 2008 (Sedgh et al., 2012) the latest year of available estimates. The global decline was largely driven by a declining rate of abortion in Eastern Europe, the sub-region that still has the highest rate of abortions (43 per 1000), despite CPRs that are increasingly comparable to those in Western Europe (UN-ECOSOC, 2014b). The persistence of relatively high rates of abortion in Eastern Europe despite rising contraceptive use suggests that method use may be intermittent, technologies inadequate or long-standing reliance on abortion has not been amenable to rapid change. The lowest sub-regional rate is in Western Europe (12 per 1000), and an estimated 86% of all abortions in 2008 took place in the developing world (Sedgh et al., 2012).
Nearly all abortions in Africa (outside of Southern Africa) and in Central and South America remain unsafe (97%) (Sedgh et al., 2012), with the risk of death due to abortion being 15 times higher in Africa than in Latin America and the Caribbean (WHO, 2007b; 2011). It is also in Africa where the number of deaths due to unsafe abortion has declined the least since 1990; in Latin America, deaths declined from 80 to 30 per 100,000 abortions, while in Africa deaths declined from 680 to 460 per 100,000 abortions (and to 520 per 100,000 in SSA). An estimated 41% (8.7 million) of all unsafe abortions involve adolescents (Shah & Åhman, 2012), who experience a higher risk of complications. Women under the age of 25 account for almost half of all abortion-related deaths (UN-ECOSOC, 2014b; WHO, 2007b, 2011). (See Santhya & Jeejeeboy, 2014, for a thorough review of SRH needs among adolescents).
Diagnosis, treatment and surveillance of STIs remain woefully inadequate
Among key SRH clinical outcomes, data on STIs are among the least reliable at the regional or global level, precluding our ability to report on global trends since 1994. While diagnostic methods have improved for many STIs, discontinuities in national surveillance systems, and the sheer inadequacy of incidence or prevalence studies, undermine the reliability of aggregate regional or global data (WHO, 2012a).
Data on the prevalence of syphilis are the most complete, due in part to the availability of a cheap and simple diagnostic test, and initiatives to screen and treat syphilis among pregnant women (WHO, 2012a). An estimated 1.3 million pregnant women annually have active syphilis infections, and failure to screen and treat pregnant women for syphilis leads to an estimated ~200,000 stillbirths, ~90,000 neonatal deaths, ~60,000 preterm or low birth weight infants, and ~150,000 infected newborns each year (Newman et al., 2013). Screening and treatment is highly effective if undertaken in the first or second trimester of pregnancy (Hawkes, Gomez, Broutet, & Heimesaat, 2013), strengthening the rationale for comprehensive and early ANC for all pregnant women.
WHO consultations have called for a concerted global effort to build systematic screening, treatment and reporting for STIs (WHO, 2002, 2007a, 2012a), highlighting the poor quality and coverage of available data on STI incidence outside of Europe and a few industrialised countries, the fact that global estimates of major infections (e.g. trichomoniasis), are based on very few data points (WHO, 2002), and an increasing need to monitor reports of decreased susceptibility of Neisseria gonorrhoeae to cephalosporins (WHO, 2012a). Although infection with STIs enhances the transmission of HIV, the quality and coverage of STI services even for HIV-infected persons is fragmented (Church & Mayhew, 2009; Mak et al., 2013). Additionally, HIV-related investments have not resulted in the clinical infrastructure needed to screen, diagnose, treat and monitor STIs for much of the developing world (Dehne, Snow, & O'Reilly, 2000; Mullick, Watson-Jones, Beksinska, & Mabey, 2005; WHO, 2007a).
Infertility
The ICPD POA included commitments to prevent and address infertility, which is not only a great personal sadness for many women and couples but in many parts of the world is also a cause for social exclusion, divorce and even violence against women. Recent estimations of infertility suggest stable prevalence estimates for primary (i.e. before the experience of any pregnancy) and secondary (i.e. following the experience of pregnancy) infertility since 1990 (Mascarenhas et al., 2012). The only measurable decline observed since 1990 was a modest decline in the prevalence of primary infertility in SA and SSA, regions with some of the highest prevalence rates in 1990. There is continuing need for better research on the full range of different STIs (as noted above), as they can have differing effects on the probability of conception, pregnancy loss and stillbirth. Due to population growth, the absolute number of couples affected by infertility worldwide rose from 42 million in 1990 to 48·5 million in 2010 (Mascarenhas et al., 2012), and while assisted reproduction has matured as a clinical service in developed countries over the past two decades, infertile couples in developing countries have limited access to the benefits of such scientific progress (Vayena, Peterson, Adamson, & Nygren, 2009; WHO, 2003).
Unmet SRH needs and the rights of persons living with HIV and AIDS
In 1993, an estimated 14 million people were living with HIV, but within a decade an estimated 32 million people were infected. Governments and global aid institutions mobilised in response, but not before deaths from AIDS had reached a peak of 2.3 million per year in 2005, with HIV rising from the 33rd largest cause of disability-adjusted life years (DALYS) in 1990, to the 5th largest in 2010 (UN-ECOSOC, 2014b).
In 2012 ARV therapy reached 9.7 million people in LMICs, representing 34% of treatment eligible persons (UNAIDS, 2013; WHO, 2013b). The percentage of pregnant women living with HIV who have access to ART reached an estimated 67% globally in 2013, contributing to an estimated 40% decline in transmission of HIV from mothers to their children since 2009 (WHO, 2014a). Yet, access remains uneven: among 22 priority countries needing increased coverage of ART, 4 provide ART to less than 50% of pregnant women living with HIV, and only 5 have coverage levels of 80% or higher (UNAIDS, 2013; UN-ECOSOC, 2014b).
SSA is home to three quarters of all HIV-infected persons. Women aged 15–49 comprise 61% of those infected, with the highest rates of infection coinciding with peak reproductive years, ages 18 to 30 (UNAIDS, 2013). Increased access to ART has been associated with a rebound in fertility desires among persons living with HIV (Maier et al., 2009; Rudy, Murphy, Harris, Muenz, & Ellen, 2009), and in some countries, increased incidence of pregnancy (Myer et al., 2010). For women living with HIV, pregnancy demonstrates continuing health as well as confidence and investment in the future (UNICEF, WHO, & UNFPA, 1997). However, tacit discriminatory and stigmatising attitudes against the childbearing of persons living with HIV and AIDS, particularly by health providers, may hinder women's ability to pursue their fertility aspirations (Cooper, Harries, Myer, Orner, & Bracken, 2007; Myer et al., 2010). At the same time, women living with HIV desire fewer children than do their HIV-negative counterparts, even in the context of widespread access to ART (Kaida et al., 2011; Snow, Mutumba, Resnicow, & Mugyenyi, 2013), leading to increased need for contraceptive methods and counselling.
Contraceptive use averts even more HIV-positive births than ART (Reynolds, Janowitz, Wilcher, & Cates, 2008), yet rates of contraceptive use among HIV-positive persons vary considerably (Kakaire, Kaye, & Osinde, 2010; Polis et al., 2011; Snow et al., 2013), and unmet need for contraception remains high: in Uganda, nearly 75% of sexually active men and women living with HIV wanted no more children but were not using a condom or other contraceptive (Nakayiwa et al., 2006).
Current WHO guidelines for contraceptive use by women living with HIV and AIDS (WHO, 2012c) allow all methods except the IUD, and also strongly recommend dual protection – a condom and another method. However, certain classes of ART (Mascarenhas et al., 2012), including non-nucleoside reverse transcriptase inhibitors (NNRTIs) and protease inhibitors, in addition to Rifampicin, an anti-tuberculosis (TB) drug (TB is a common co-morbidity in HIV and AIDS), interact with hormonal contraceptives and potentially reduce their efficacy (Coll, Lopez, & Hernandez, 2008; WHO, 2012c). Concerns over a possible role of progestin-only injectable contraception, i.e. depot medroxyprogesterone acetate (DMPA), in HIV acquisition have not abated, but demand more and better research (Heffron et al., 2012; The Lancet Infectious Diseases 2012; Morrison et al., 2010). Assisted reproductive technologies for persons living with HIV and AIDS, particularly HIV-discordant couples, are not widely available in developing countries (Lampe, Smith, Anderson, Edwards, & Nesheim, 2011; Matthews & Mukherjee, 2009; Van Leeuwen, Repping, Prins, Reiss, & Van Der Veen, 2009). Therefore, irrespective of whether women living with HIV desire additional children or not, the weak integration of HIV and SRH services in many countries constrains access to much-needed counselling, technologies and support.
Young people living with HIV/AIDS are especially vulnerable
While HIV and AIDS services have not fully addressed the SRH needs of HIV-affected women, they are even less adequate for adolescents and youth living with HIV and AIDS who may not be welcome in either paediatric or adult services (UNFPA, 2009). Young people, infected or otherwise affected by HIV and AIDS, face greater challenges than adults with adherence, accessing routine care, and managing disclosure, and require tailored clinical and social support. HIV-affected youth are increasingly recognised to be at increased risk of psychiatric and psychological disorders (Benton & Ifeagwu, 2008; Havens & Mellins, 2009) due to the complexity of health and social stresses with which they are coping, including a greater likelihood of parental illness, orphanhood, poverty and lack of social protection, HIV-related co-morbidities, difficulties accessing health and social welfare services and the burden of managing a chronic disease from a young age. Developing comprehensive and integrated adolescent SRH services that include support for HIV-affected youth is a global priority.
The persistent fragility of health systems obstructs progress
For numerous countries reviewed in Table 1, the distributions of skilled attendance and modern CPR by household wealth were characterised by two striking patterns: in Eastern Europe and Central Asia, almost universal skilled birth attendance coincided with almost universally low CPR (e.g. see Albania, Azerbaijan, Bosnia and Herzegovnia, Macedonia); while in EAP, and SA, modern CPR was more equitably distributed by wealth than skilled attendance for pregnant women.
In EAP, and SA, access to skilled birth remains highly skewed by wealth, while modern contraceptives are used by many women living in the poorest households. This suggests not only that demand for contraception is comparatively high in the region, but also that investments in family planning delivery, admittedly easier to provide, have outpaced those to ensure life-saving delivery care. These contrasts are especially stark in Bhutan, Nepal and India, where modern CPR was 69%, 36% and 35%, respectively, among women living in the lowest wealth quintile, while skilled attendance reached only 34%, 21% and 21%, of pregnant women in this quintile.
In Bangladesh, early emphasis on family planning led to dramatic declines in both TFR and the unmet need for contraception, and CPR is highly equitable across wealth quintiles (Table 1). Jahan and Afsana (2014) describe how ICPD led to gradual expansion of programmes to address other dimensions of reproductive health, but the persistent weakness of the health system has hindered progress in providing skilled delivery care, which is accessible to only 12% of women in the lowest wealth quintile (Afsana & Wahid, 2013; ICDDR, B & Center for Reproductive Health, 2012; Khan, Jahan, & Begum, 1986; NIPORT, MEASURE DHS, & ICDDR, B, 2011; NIPORT, Mitra Associates, & ICF International, 2011; Rochat et al., 1981; Sen, 2013).
Bangladesh is far from alone, as fewer than 55% of women in SSA deliver with a skilled birth attendant (Ngo et al., 2011). The need for sustained attention to building health systems that can provide skilled delivery care to poor women is evident across numerous countries, especially in Africa and SA. Among 49 countries with the lowest per capita income, for example, only 5 meet the minimum WHO thresholds for health worker density, and in the 58 countries where 91% of all maternal deaths occur, it is estimated that 20% of maternal deaths could be averted if the current number of trained midwives was doubled (UNFPA, 2011; WHO, 2013a).
While actions are needed in the short term to redress these shortfalls, they should be designed within a framework of long-term commitments to strengthen the quality, integration and capacity of health systems, including critical dimensions of infrastructure such as human resources for SRH (WHO, 2009a, 2013e), medical records systems that allow for continuity of care (AbouZahr & Wardlaw, 2001; Allen et al., 2007; Forster et al., 2008; Ginsburg, Hoblitzelle, Sripipatana, & Wilfert, 2007), health management information systems (HMIS), commodity security and health financing for SRH services (WHO, 2013f). Attention to continuity of care is especially needed, given the rapid pace of urbanisation, increasing internal mobility, especially by young people, and the interdependence of pre-pregnancy, maternal, child and long-term health. A study of prevention of mother-to-child transmission of HIV (PMTCT) programmes in 18 countries found that only 9% of infants born to HIV-positive mothers could be identified at their first immunisation visit (Ginsburg et al., 2007), highlighting the absence of medical records systems that could be linked between health facilities (Forster et al., 2008). Emerging technologies including mobile phones hold promise for linking people to better SRH care, and efforts to integrate rural and urban, community and hospital, primary and referral health care via Internet- and phone-based communication systems are evolving rapidly (WHO, 2011), offering a possibility for under-resourced health systems to connect remote providers and patients to centres of SRH excellence. (See Sen & Govender, 2014, for a more thorough discussion of health system strengthening.)
Donor assistance to population and SRH was estimated at 12 billion US dollars per annum in 2011, with 66% of these funds directed to HIV/AIDS activities (UN-ECOSOC, 2014b). A recent analysis of the impact of HIV donor aid per capita on maternal and child health service provision across SSA from 2003 to 2010 suggests only marginal gains for SRH from HIV-directed aid, and only in the most under-resourced health systems where the HIV burden was not high (Mellins et al., 2011). In this paper comparing maternal and child health service indicators with HIV disbursements from the previous year, HIV development assistance was associated with no measurable gains in ANC coverage, except in health systems where HIV prevalence and health worker densities were lowest. Illustrating these very challenges at country level, Nigeria has shown extraordinary success in bettering access to AIDS-related therapy (see Ahonsi, 2014), but these investments have not contributed to increasing public access to other SRH services, and few of the successful, NGO-led SRH service projects scattered across Nigeria have received the requisite federal funding to take them to scale (British Council & UKaid, 2013; Cooke & Tahir, 2013; Esiet & Whitaker, 2002; Mandara, 2012; Mellins et al., 2011; National Agency for the Control of AIDS, 2013; National Population Commission & UNFPA, 2013; Shittu et al., 2010;WHO, 2014b).
Research and knowledge systems improved but still seriously inadequate
A challenge after ICPD was how to improve SRH in countries that lacked reliable information on SRH needs – a lack of data that was especially striking in the poorest, and therefore many of the highest burden countries. A singular achievement since ICPD has been the improved scope and quality of available SRH epidemiologic and behavioural data from developing countries, due to expansions in the topics covered by DHS surveys, supplemented by the MICS, as well as growth in the network of demographic surveillance sites (UN-ECOSOC, 2014b). But despite gains in available knowledge, national capacity for the effective use of these data for planning and programme evaluation remains weak.
In addition, SRH data are inadequate for monitoring quality and holding governments accountable for several dimensions of SRH, including the accurate diagnosis and surveillance of STIs; balanced contraceptive method mix; integrated SRH care for HIV-affected persons, especially for adolescents and youth; and continuity of SRH care, especially for rural residents and the poor.
Outstanding needs
Maternal mortality and HIV/AIDS-related outcomes have seen comparatively better progress than other dimensions of SRH in the past two decades, accomplishments that reflect targeted commitments by national governments and donors to meet the MDGs, and large investments in programming to stem the AIDS crisis. Such progress illustrates the level of achievements that are possible with a combination of targeted activism, funding and global accountability structures.
Yet inadequate coverage of skilled birth attendance and low contraceptive use for women from the poorest households, particularly in Africa and Asia, as well as weaker progress in other dimensions of SRH care, underscore the need to further strengthen access, comprehensiveness, integration and quality of SRH prevention and care for all persons. Aggregate progress in reducing MMR and HIV/AIDS has coincided with very limited success in strengthening the global response to STIs, and current capacity for diagnosis, treatment and surveillance of these and other SRH morbidities remains weak. The difficulties of providing fertility counselling and services, as well as long-term care for HIV-affected mothers and their infants, and young people living with HIV, highlight the continuing need to better integrate HIV and AIDS and SRH prevention and care, and to invest in medical records and HMIS that will enable providers to respond effectively to synergistic SRH needs over a lifetime.
An adequate number and rational distribution of skilled SRH health workers, especially those with midwifery skills that can address almost all SRH services, are essential to meeting these needs, and must be complemented by heightened investments to ensure a vibrant SRH knowledge sector, serving both government and civil society policy-making, planning and accountability. The need for improved health systems that provide all persons with comprehensive and integrated SRH prevention and care is no less urgent today than in 1994, and remains pivotal to fulfilling commitments of the ICPD and the Key Actions for Further Implementation.
Acknowledgements
This work was carried out with the aid of a grant from Canada's International Development Research Centre. We gratefully acknowledge the contributions of Nkeiruka Didigu, Karin Ringheim, Leslie Berman, Ionica Berevoescu, Guillem Fortuny and Melissa Garcia to the review of sexual and reproductive health progress for the Framework of actions for the follow-up to the Programme of Action of the International Conference on Population and Development Beyond 2014 (UN-ECOSOC, 2014a, 2014b), which was a critical background source for this paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- AbouZahr C., Wardlaw T. Maternal mortality at the end of a decade: Signs of progress? Bulletin of the World Health Organization. 2001:561–573. [PMC free article] [PubMed] [Google Scholar]
- Acharya D., Vaidyanathan F., Muraleedharan V., Dheenadayalan D., Dash U. Do the poor benefit from public spending in India? Results from benefit (utilization) incidence analysis in Tamil Nadu and Orissa. London: Consortium for Research on Equitable Health Systems. 2011 http://www.crehs.lshtm.ac.uk/india_BUIA.pdf Retrieved from. [Google Scholar]
- Afsana K., Wahid S. S. Health care for poor people in the urban slums of Bangladesh. The Lancet. 2013:2049–2051. doi: 10.1016/S0140-6736(13)62295-3. [DOI] [PubMed] [Google Scholar]
- Ahman E., Shah I. H. New estimates and trends regarding unsafe abortion mortality. International Journal of Gynecology & Obstetrics. 2011;(2):121–126. doi: 10.1016/j.ijgo.2011.05.027. [DOI] [PubMed] [Google Scholar]
- Ahonsi B. Accelerating the quest for integrated and comprehensive sexual and reproductive health services in Nigeria. Global Public Health. 2014 doi: 10.1080/17441692.2014.986162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkema L., Kantorova V., Menozzi C., Biddlecom A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: A systematic and comprehensive analysis. The Lancet. 2013:1642–1652. doi: 10.1016/S0140-6736(12)62204-1. [DOI] [PubMed] [Google Scholar]
- Allen C., Jazayeri D., Miranda J., Biondich P. G., Mamlin B. W., Wolfe B. A., et al. Fraser H. S. F. Experience in implementing the OpenMRS medical record system to support HIV treatment in Rwanda. Studies in Health Technology and Informatics. 2007:382–386. [PubMed] [Google Scholar]
- Baggaley R. F., Burgin J., Campbell O. M. R., Gravenor M. B. The potential of medical abortion to reduce maternal mortality in Africa: What benefits for Tanzania and Ethiopia? PLoS One. 2010;(10):e13260. doi: 10.1371/journal.pone.0013260.s001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton T. D., Ifeagwu J. A. HIV in adolescents: What we know and what we need to know. Current Psychiatry Reports. 2008;(2):109–115. doi: 10.1007/s11920-008-0020-7. [DOI] [PubMed] [Google Scholar]
- Berer M. Making abortion safe and legal. The ethics and dynamics of change. Reproductive Health Matters. 1993;(2):5–10. doi: 10.1016/0968-8080(93)90002-B. [DOI] [Google Scholar]
- Bilian X. Chinese experience with intrauterine devices. Contraception. 2007;(6):S31–S34. doi: 10.1016/j.contraception.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Brache V., Faundes A. Contraceptive vaginal rings: A review. Contraception. 2010:418–427. doi: 10.1016/j.contraception.2010.04.012. [DOI] [PubMed] [Google Scholar]
- British Council & UKaid . Abuja: Author; 2013. Gender in Nigeria Report 2012: Improving the lives of girls and women in Nigeria.http://www.britishcouncil.org.ng/files/2012/12/GenderReport-full.pdf Retrieved from. [Google Scholar]
- Campbell O. M., Graham W. J. Strategies for reducing maternal mortality: Getting on with what works. The Lancet. 2006:1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- Church K., Mayhew S. H. Integration of STI and HIV prevention, care, and treatment into family planning services: A review of the literature. Studies in Family Planning. 2009:171–186. doi: 10.1111/j.1728-4465.2009.00201.x. [DOI] [PubMed] [Google Scholar]
- Cleland J., Shah I. H. The contraceptive revolution: Focused efforts are still needed. The Lancet. 2013:1604–1606. doi: 10.1016/S0140-6736(13)60588-7. [DOI] [PubMed] [Google Scholar]
- Coll O., Lopez M., Hernandez S. Fertility choices and management for HIV-positive women. Current Opinion in HIV and AIDS. 2008:186–192. doi: 10.1097/COH.0b013e3282f51219. [DOI] [PubMed] [Google Scholar]
- Cooke J. G., Tahir F. Maternal health in Nigeria: with leadership, progress is possible. Washington, DC: CSIS Global Health Policy Center; 2013. http://csis.org/files/publication/130111_Cooke_MaternalHealthNigeria_Web.pdf Retrieved from. [Google Scholar]
- Cooper D., Harries J., Myer L., Orner P., Bracken H. “Life is still going on”: Reproductive intentions among HIV-positive women and men in South Africa. Social Science & Medicine. 2007:274–283. doi: 10.1016/j.socscimed.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Curtis S. L. Contraceptive use dynamics research needs post fertility transition. Revista Brasileira de Estudos de População. 2012:191–193. [Google Scholar]
- Darroch J. E. Male fertility control – Where are the men? Contraception. 2008;(4):S7–S17. doi: 10.1016/j.contraception.2008.04.117. [DOI] [PubMed] [Google Scholar]
- Dehne K. L., Snow R., O'Reilly K. Integration of prevention and care of sexually transmitted infections with family planning services: What is the evidence for public health benefits? Bulletin of the World Health Organization. 2000:628–639. [PMC free article] [PubMed] [Google Scholar]
- Diniz S. G., Araújo M. J. Reproductive health and rights in Brazil 20 years post ICPD. Global Public Health. 2014 doi: 10.1080/17441692.2014.986167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diniz D., Medeiros M. Itineraries and methods of illegal abortion in five Brazilian state capitals. Ciência & Saúde Coletiva. 2012:1671–1681. doi: 10.1590/s1413-81232012000700002. [DOI] [PubMed] [Google Scholar]
- Diniz S. G., d'Oliveira A. F. P. L., Lansky S. Equity and women's health services for contraception, abortion and childbirth in Brazil. Reproductive Health Matters. 2012;(40):94–101. doi: 10.1016/S0968-8080(12)40657-7. [DOI] [PubMed] [Google Scholar]
- do Carmo Leal M., da Silva A. A., Dias M. A., da Gama S. G., Rattner D., Moreira M., Szwarcwald C. Birth in Brazil: National survey into labour and birth. Reproductive Health. 2012;(1):15. doi: 10.1590/S0102-311X2008001200020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzuba I. G., Winikoff B., Peña M. Medical abortion: A path to safe, high-quality abortion care in Latin America and the Caribbean. The European Journal of Contraception and Reproductive Health Care. 2013:441–450. doi: 10.3109/13625187.2013.824564. [DOI] [PubMed] [Google Scholar]
- Esiet A. O., Whitaker C. Coming to terms with politics and gender: The evolution of an adolescent reproductive health program in Nigeria. In: Haberland N, Measham D, editors. Responding to Cairo. Case studies of changing practice in reproductive health and family planning. New York, NY: Population Council; 2002. pp. 149–167.http://www.popline.org/node/189006#sthash.JvLYbiRQ.dpuf Retrieved from. [Google Scholar]
- fhi360 . Reproductive health coalition product brief: Contraceptive implants. Durham, NC: Author; 2013. http://www.fhi360.org/resource/reproductive-health-supplies-coalition-product-brief-contraceptive-implants Retrieved from. [Google Scholar]
- Forster M., Bailey C., Brinkhof M. W., Graber C., Boulle A., Spohr M., et al. Jahn A. Electronic medical record systems, data quality and loss to follow-up: Survey of antiretroviral therapy programmes in resource-limited settings. Bulletin of the World Health Organization. 2008:939–947. doi: 10.2471/BLT.07.049908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrysch S., Zanger P., Campbell O. M. R. Emergency obstetric care availability: A critical assessment of the current indicator. Tropical Medicine & International Health. 2012;(1):2–8. doi: 10.1111/j.1365-3156.2011.02851.x. [DOI] [PubMed] [Google Scholar]
- Ginsburg A. S., Hoblitzelle C. W., Sripipatana T. L., Wilfert C. M. Provision of care following prevention of mother-to-child HIV transmission services in resource-limited settings. AIDS. 2007:2529–2532. doi: 10.1097/QAD.0b013e3282f155f4. [DOI] [PubMed] [Google Scholar]
- Gupta M. D., Desikachari B., Somanathan T., Padmanaban P. Washington, DC: World Bank; 2009. How to improve public health systems: Lessons from Tamil Nadu.Policy Research Working Paper, No. wps5073. [Google Scholar]
- Harper C. C., Blanchard K., Grossman D., Henderson J. T., Darney P. D. Reducing maternal mortality due to elective abortion: Potential impact of misoprostol in low-resource settings. International Journal of Gynecology & Obstetrics. 2007;(1):66–69. doi: 10.1016/j.ijgo.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Havens J. F., Mellins C. A. Psychiatric aspects of HIV/AIDS. In: Rutter M, Bishop D. V. M., Pine D. S, Scott S, Stevenson J, Taylor E, Thapar A, editors. Rutter's child and adolescent psychiatry. 5th ed. Oxford: Blackwell; 2008. [DOI] [Google Scholar]
- Hawkes S. J., Gomez G. B., Broutet N., Heimesaat M. M. Early antenatal care: Does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta-analysis. PLoS One. 2013;(2):e56713. doi: 10.1371/journal.pone.0056713.s001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffron R., Donnell D., Rees H., Celum C., Mugo N., Were E., Baeten J. M. Use of hormonal contraceptives and risk of HIV-1 transmission: A prospective cohort study. The Lancet Infectious Diseases. 2012;(1):19–26. doi: 10.1016/S1473-3099(11)70247-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICDDR, B, & Center for Reproductive Health . Saving money, saving lives: The Bangladesh Menstrual Regulation Program. Dhaka: Author; 2012. file:///Users/massymutumba/Downloads/CRH-KT-010-JAN-2012.pdf Retrieved from. [Google Scholar]
- ICF International The Demographic and Health Surveys (DHS . 2014 http://www.icfi.com/insights/projects/research-and-evaluation/demographic-and-health-surveys Retrieved from.
- International Institute for Population Science (IIPS) District Level Household and Facility Survey (DLHS-3), 2007–2008 . 2010 http://www.rchiips.org/pdf/INDIA_REPORT_DLHS-3.pdf Retrieved from.
- International Institute for Population Science (IIPS) & Macro International . National Family Health Survey (NFHS-3), 2005–2006: Tamil Nadu Fact Sheet. Mumbai: Author; 2007. http://www.rchiips.org/nfhs/pdf/TamilNadu.pdf Retrieved from. [Google Scholar]
- Jahan R., Afsana K. Sustaining progress toward comprehensive reproductive health services in Bangladesh. Global Public Health. 2014 doi: 10.1080/17441692.2014.986164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain A. K. Measuring the effect of fertility decline on the maternal mortality ratio. Studies in Family Planning. 2011;(4):247–260. doi: 10.1111/j.1728-4465.2011.00288.x. [DOI] [PubMed] [Google Scholar]
- Kaida A., Laher F., Strathdee S. A., Janssen P. A., Money D., Hogg R. S., Gray G. Childbearing intentions of HIV-positive women of reproductive age in Soweto, South Africa: The influence of expanding access to HAART in an HIV hyperendemic setting. American Journal of Public Health. 2011:350–358. doi: 10.2105/AJPH.2009.177469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakaire O., Kaye D. K., Osinde M. O. Contraception among persons living HIV with infection attending an HIV care and support centre in Kabale, Uganda. Journal of Public Health and Epidemiology. 2010:180–188. [Google Scholar]
- Kaufman J. The cost of IUD failure in China. Studies in Family Planning. 1993;(3):194–196. [PubMed] [Google Scholar]
- Khan A. R., Jahan F. A., Begum S. F. Maternal mortality in rural Bangladesh: The Jamalpur district. Studies in Family Planning. 1986;(1):7–12. [PubMed] [Google Scholar]
- Koenig M. A., Foo G. H. C., Joshi K. Quality of care within the Indian family welfare programme: A review of recent evidence. Studies in Family Planning. 2000;(1):1–18. doi: 10.1111/j.1728-4465.2000.00001.x. [DOI] [PubMed] [Google Scholar]
- Lampe M. A., Smith D. K., Anderson G. J. E., Edwards A. E., Nesheim S. R. Achieving safe conception in HIV-discordant couples: The potential role of oral preexposure prophylaxis (PrEP) in the United States. American Journal of Obstetrics and Gynecology. 2011:488.e1–488.e8. doi: 10.1016/j.ajog.2011.02.026. [DOI] [PubMed] [Google Scholar]
- Lancet Maternal Survival Series Steering Group Campbell O. M., Graham W. J. Maternal Survival 2 Strategies for reducing maternal mortality: Getting on with what works. The Lancet. 2006:1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- Maier M., Andia I., Emenyonu N., Guzman D., Kaida A., Pepper L., Bangsberg D. R. Antiretroviral therapy is associated with increased fertility desire, but not pregnancy or live birth, among HIV+ women in an early HIV treatment program in rural Uganda. AIDS and Behavior. 2009;(1):28–37. doi: 10.1007/s10461-008-9371-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak J., Birdthistle I., Church K., Preez N. F., Kivunaga J., Kikuvi J., et al. Mayhew S. H. Need, demand and missed opportunities for integrated reproductive health-HIV care in Kenya and Swaziland: Evidence from household surveys. AIDS. 2013:S55–S63. doi: 10.1097/QAD.0000000000000046. [DOI] [PubMed] [Google Scholar]
- Mandara M. Family planning in Nigeria and prospects for the future. International Journal of Gynecology & Obstetrics. 2012;(1):1–4. doi: 10.1016/j.ijgo.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Mascarenhas M. N., Flaxman S. R., Boerma T., Vanderpoel S., Stevens G. A., Low N. National, regional, and global trends in infertility prevalence since 1990: A systematic analysis of 277 health surveys. PLoS Medicine. 2012;(12):e1001356. doi: 10.1371/journal.pmed.1001356.s003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews L. T., Mukherjee J. S. Strategies for harm reduction among HIV-affected couples who want to conceive. AIDS and Behavior. 2009;(1):5–11. doi: 10.1007/s10461-009-9551-0. [DOI] [PubMed] [Google Scholar]
- MEASURE Evaluation PRH Family planning and reproductive health indicators database. Maternal and neonatal effort index (MNPI. 2014 http://www.cpc.unc.edu/measure/prh/rh_indicators/specific/sm/maternal-neonatal-program-index-mnpi Retrieved from. [Google Scholar]
- Mellins C. A., Tassiopoulos K., Malee K., Moscicki A.-B., Patton D., Smith R.,, et al. Seage III G. R. Behavioral health risks in perinatally HIV-exposed youth: Co-occurrence of sexual and drug use behavior, mental health problems, and nonadherence to antiretroviral treatment. AIDS Patient Care and STDs. 2011:413–422. doi: 10.1089/apc.2011.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministerio de Saude . 2009. Pesquisa Nacional de Demografia e Saude da Crianca e da Mulher (PNDS-2006) [National Survey on Demography and the Health of Children and Women] Retrieved from http://bvsms.saude.gov.br/bvs/pnds/index.php. [Google Scholar]
- Morrison C. S., Chen P.-L., Kwok C, Richardson B. A., Chipato T., Mugerwa R., et al. Salata R. A. Hormonal contraception and HIV acquisition: Reanalysis using marginal structural modeling. AIDS. 2010:1778–1781. doi: 10.1097/QAD.0b013e32833a2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullick S., Watson-Jones D., Beksinska M., Mabey D. Sexually transmitted infections in pregnancy: Prevalence, impact on pregnancy outcomes, and approach to treatment in developing countries. Sexually Transmitted Infections. 2005:294–302. doi: 10.1136/sti.2002.004077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraleedharan V., Dash U., Gilson L. Tamil Nadu 1980s–2005: A success story in India. In: Balabanova D, McKee M, Mills A, editors. ‘Good health at low cost’: 25 years on. London: London School of Hygiene & Tropical Medicine; 2009. pp. 159–192. [Google Scholar]
- Myer L., Carter R. J., Katyal M., Toro P., El-Sadr W. M., Abrams E. J., Mofenson L. Impact of antiretroviral therapy on incidence of pregnancy among HIV-infected women in Sub-Saharan Africa: A cohort study. PLoS Medicine. 2010;(2):e1000229. doi: 10.1371/journal.pmed.1000229.t003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakayiwa S., Abang B., Packel L., Lifshay J., Purcell D. W., King R., Bunnell R. Desire for children and pregnancy risk behavior among HIV-infected men and women in Uganda. AIDS and Behavior. 2006;(1):95–104. doi: 10.1007/s10461-006-9126-2. [DOI] [PubMed] [Google Scholar]
- National Agency for the Control of AIDS . President's comprehensive response plan for HIV/AIDS in Nigeria. Abuja: Author; 2013. http://www.zero-hiv.org/wp-content/uploads/2013/09/PCRP-2013-2015-real-2-Aug-2013.pdf Retrieved from. [Google Scholar]
- National Population Commission & UNFPA . ICPD beyond 2014 review: Nigeria country implementation profile. Abuja: Author; 2013. http://icpdbeyond2014.org/about/view/19-country-implementation-profiles Retrieved from. [Google Scholar]
- Nelson A. New low-dose, extended-cycle pills with levonorgestrel and ethinyl estradiol: An evolutionary step in birth control. International Journal of Women's Health. 2010:99. doi: 10.2147/ijwh.s4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman L., Kamb M., Hawkes S., Gomez G., Say L., Seuc A., et al. Menendez C. Global estimates of syphilis in pregnancy and associated adverse outcomes: Analysis of multinational antenatal surveillance data. PLoS Medicine. 2013;(2):e1001396. doi: 10.1371/journal.pmed.1001396.s001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngo T. D., Park M. H., Shakur H., Free C. Comparative effectiveness, safety and acceptability of medical abortion at home and in a clinic: A systematic review. Bulletin of the World Health Organization. 2011:360–370. doi: 10.2471/BLT.10.084046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIPORT, MEASURE DHS, & ICDDR, B . Bangladesh Maternal Mortality and Health Care Survey 2010. Dhaka: Author; Retrieved from http://www.cpc.unc.edu/measure/publications/tr-12-87. [Google Scholar]
- NIPORT, Mitra Associates, & ICF International . Bangladesh Maternal Mortality and Health Care Survey 2010. Dhaka: Author; 2011. http://www.cpc.unc.edu/measure/publications/tr-12-87 Retrieved from. [Google Scholar]
- Oliveira I. T. d., Dias J. G., Padmadas S. S., Leone T. Dominance of sterilization and alternative choices of contraception in India: An appraisal of the socioeconomic impact. PLoS One. 2014;(1):e86654. doi: 10.1371/journal.pone.0086654.t002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmanaban P., Raman P. S., Mavalankar D. V. Innovations and challenges in reducing maternal mortality in Tamil Nadu, India. Journal of Health, Population, and Nutrition. 2009:202. doi: 10.3329/jhpn.v27i2.3364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polis C. B., Gray R. H., Lutalo T., Nalugoda F., Kagaayi J., Kigozi G., Wawer M. J. Trends and correlates of hormonal contraceptive use among HIV-infected women in Rakai, Uganda, 1994–2006, 1994–2006. Contraception. 2011:549–555. doi: 10.1016/j.contraception.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Power J., French R., Cowan F. Subdermal implantable contraceptive versus other forms of reversible contraceptives or other implants as effective methods of preventing pregnancy (review. Cochrane Database of Systematic Reviews. 2007;(3) doi: 10.1002/14651858.CD001326.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata N., Sreenivas A., Vahidnia F., Potts M. Saving maternal lives in resource-poor settings: Facing reality. Health Policy. 2009;(2):131–148. doi: 10.1016/j.healthpol.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Ramasundaram S., Allaudin K., Charles B., Gopal K., Krishnamurthy P., Poornalingam R., Warren D. HIV/AIDS control in India – Lessons from Tamil Nadu. 2001 Genevahttp://library.cphs.chula.ac.th/Ebooks/HealthCareFinancing/WG5/paperno.WG5_23.pdf Retrieved from. [Google Scholar]
- Reynolds H. W., Janowitz B., Wilcher R., Cates W. Contraception to prevent HIV-positive births: Current contribution and potential cost savings in PEPFAR countries. Sexually Transmitted Infections. 2008;(Suppl 2):ii49–ii53. doi: 10.1136/sti.2008.030049. [DOI] [PubMed] [Google Scholar]
- Rochat R. W., Jabeen S., Rosenberg M. J., Measham A. R., Khan A. R., Obaidullah M., Gould P. Maternal and abortion related deaths in Bangladesh, 1978–1979, 1978–1979. International Journal of Gynecology & Obstetrics. 1981:155–164. doi: 10.1016/0020-7292(81)90056-4. [DOI] [PubMed] [Google Scholar]
- Ronsmans C., Etard J.-F., Walraven G., Høj L., Dumont A., Bernis L., Kodio B. Maternal mortality and access to obstetric services in West Africa. Tropical Medicine & International Health. 2003:940–948. doi: 10.1046/j.1365-3156.2003.01111.x. [DOI] [PubMed] [Google Scholar]
- Ross J., Hardee K., Mumford E., Eid S. Contraceptive method choice in developing countries. International Family Planning Perspectives. 2002:1), 32–40. [Google Scholar]
- Rudy B. J., Murphy D. A., Harris D. R., Muenz L., Ellen J. Patient-related risks for nonadherence to antiretroviral therapy among HIV-infected youth in the United States: A study of prevalence and interactions. AIDS Patient Care and STDs. 2009:185–194. doi: 10.1089/apc.2008.0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santhya K. G., Jejeebhoy S. J. Sexual and reproductive health and rights of adolescent girls: Evidence from low and middle-income countries. Global Public Health. 2014 doi: 10.1080/17441692.2014.986169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgh G., Singh S., Shah I. H., Åhman E., Henshaw S. K., Bankole A. Induced abortion: Incidence and trends worldwide from 1995 to 2008. The Lancet. 2012:625–632. doi: 10.1016/S0140-6736(11)61786-8. [DOI] [PubMed] [Google Scholar]
- Seiber E. E., Bertrand J. T., Sullivan T. M. Changes in contraceptive method mix in developing countries. International Family Planning Perspectives. 2007;(3):117–123. doi: 10.1363/3311707. [DOI] [PubMed] [Google Scholar]
- Sen A. What's happening in Bangladesh. The Lancet. 2013:1966–1968. doi: 10.1016/S0140-6736(13)62162-5. [DOI] [PubMed] [Google Scholar]
- Sen G., Govender V. Sexual and reproductive health and rights in changing health systems. Global Public Health. 2014 doi: 10.1080/17441692.2014.986161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah I. H., Åhman E. Unsafe abortion differentials in 2008 by age and developing country region: High burden among young women. Reproductive Health Matters. 2012:169–173. doi: 10.1016/S0968-8080(12)39598-0. [DOI] [PubMed] [Google Scholar]
- Shittu O., Ejembi C., Adaji S., Abdul M., Idris S., Abdulkarim B., et al. Okonofua F.2010The current state of reproductive health in rural northern Nigeria in the context of the pursuit of the MDGs: Perspectives from a community-based research training program African Journal of Reproductive Health: Special Issue 315–18. [Google Scholar]
- Silva J., Surita F. Adolescent pregnancy: Current situation. Revista Brasileira de Ginecologia e Obstetrícia. 2012:191–193. doi: 10.1590/s0100-72032012000800001. [DOI] [PubMed] [Google Scholar]
- Singh A., Pallikadavath S., Ram F., Ogollah R., Noor A. M. Inequalities in advice provided by public health workers to women during antenatal sessions in rural India. PLoS One. 2012;(9):e44931. doi: 10.1371/journal.pone.0044931.t006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow R. C., Mutumba M., Resnicow K., Mugyenyi G. The social legacy of AIDS: Fertility aspirations among HIV-affected women in Uganda. American Journal of Public Health. 2013:278–285. doi: 10.2105/AJPH.2012.300892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State Health Society . Project Implementation Plan (PIP) 2012–2013. Chennai: State Health Society; 2012. http://nrhmtn.gov.in/pip/pip12_13.pdf Retrieved from. [Google Scholar]
- Stover J., Ross J. How increased contraceptive use has reduced maternal mortality. Maternal and Child Health Journal. 2010:687–695. doi: 10.1007/s10995-009-0505-y. [DOI] [PubMed] [Google Scholar]
- Sullivan T. M., Bertrand J. T., Rice J., Shelton J. D. Skewed contraceptive method mix: Why it happens, why it matters. Journal of Biosocial Science. 2006:501. doi: 10.1017/S0021932005026647. [DOI] [PubMed] [Google Scholar]
- UNAIDS Global Report in the Global AIDS Epidemic 2013 . 2013 http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf Retrieved from.
- UNICEF Multiple Indicator Cluster Surveys (MICS . 2014 http://www.unicef.org/statistics/index_24302.html Retrieved from.
- UNICEF, WHO, & UNFPA . New York, NY: UNICEF; 1997. Guidelines for monitoring the availability and use of obstetric services.http://www.childinfo.org/files/maternal_mortality_finalgui.pdf Retrieved from. [Google Scholar]
- United Nations . New York, NY: Author; 2013. The Millennium Development Goals Report 2013. Retrieved from http://mdgs.un.org/unsd/mdg/Resources/Static/Products/Progress2013/English2013.pdf. [Google Scholar]
- United Nations Department for Economic and Social Affairs (UNDESA), Population Division Levels and trends of contraceptive use as assessed in 1994 . 1996 Retrieved from http://www.un.org/esa/population/pubsarchive/catalogue/catsst.htm#9.
- United Nations Department of Economic and Social Affairs (UNDESA), Population Division . New York, NY: Author; 2014a. World Contraceptive Patterns 2013.http://www.un.org/en/development/desa/population/publications/family/contraceptive-wallchart-2013.shtml Retrieved from. [Google Scholar]
- United Nations Department of Economic and Social Affairs (UNDESA), Population Division . New York, NY: Author; 2014b. Model-based Estimates and Projections of Family Planning Indicators, 2014. [Google Scholar]
- United Nations Department of Economic and Social Affairs (UNDESA), Population Division . New York, NY: Author; 2013a. World Population Prospects: The 2012 Revision.http://esa.un.org/unpd/wpp/Documentation/publications.htm Retrieved from. [Google Scholar]
- United Nations Department of Economic and Social Affairs (UNDESA), Population Division . New York, NY: Author; 2013b. World Contraceptive Use 2012.http://www.un.org/esa/population/publications/WCU2012/MainFrame.html Retrieved from. [Google Scholar]
- United Nations Economic and Social Council (UN-ECOSOC) New York, NY: Author; 2014a. Framework of actions for the follow-up to the Programme of Action of the International Conference on Population and Development beyond 2014 (Summary). A report of the Secretary-General (E/CN.9/2014/4.http://icpdbeyond2014.org/uploads/browser/files/sg_report_on_icpd_operational_review_final.unedited.pdf Retrieved from. [Google Scholar]
- United Nations Economic and Social Council (UN-ECOSOC) New York, NY: Author; 2014b. Framework of actions for the follow-up to the Programme of Action of the International Conference on Population and Development beyond 2014. A report of the Secretary-General (A/69/62.http://issuu.com/shiralevine/docs/icpd_review_global_report_a_69_62_e Retrieved from. [Google Scholar]
- United Nations Population Fund (UNFPA) International Conference on Population and Development (ICPD) Programme of Action. Cairo: Author; 1995. https://http://www.unfpa.org/public/global/publications/pid/1973 Retrieved from. [Google Scholar]
- United Nations Population Fund (UNFPA) Key actions for the further implementations of the Programme of Action of the International Conference on Population and Development. Author; 1999. http://www.unfpa.org/webdav/site/global/shared/documents/publications/1999/key_actions_en.pdf New York, NY. Retrieved from. [Google Scholar]
- United Nations Population Fund (UNFPA) Expanding access to youth-friendly services. New York, NY: Author; 2009. [Google Scholar]
- United Nations Population Fund (UNFPA) State of the world's population. 2011 http://www.unfpa.org/sowmy/resources/docs/main_report/en_SOWMR_Full.pdf Retrieved from. [Google Scholar]
- United Nations Population Fund (UNFPA) State of world population 2012. By choice, not by chance: Family planning, human rights and development (Report No. 978-1-61800-009-5. 2012a https://http://www.unfpa.org/public/home/publications/pid/12511 Retrieved from.
- United Nations Population Fund (UNFPA) Urgent response: Providing emergency obstetric and newborn care . 2012b http://www.unfpa.org/webdav/site/global/shared/factsheets/srh/EN-SRHfactsheet-Urgent.pdf Retrieved from.
- Vaidyanathan G. Sexual and reproductive health services in Tamil Nadu – Progress and way forward. Global Public Health. 2014 doi: 10.1080/17441692.2014.986165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Leeuwen E., Repping S., Prins J., Reiss P., Van Der Veen F. Assisted reproductive technologies to establish pregnancies in couples with an HIV-1-infected man. Netherlands Journal of Medicine. 2009:322–327. [PubMed] [Google Scholar]
- Vayena E., Peterson H. B., Adamson D., Nygren K.-G. Assisted reproductive technologies in developing countries: Are we caring yet. Fertility and Sterility. 2009:413–416. doi: 10.1016/j.fertnstert.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Victora C. G., Aquino E. M., do Carmo Leal M., Monteiro C. A., Barros F. C., Szwarcwald C. L. Maternal and child health in Brazil: Progress and challenges. The Lancet. 2011:1863–1876. doi: 10.1016/S0140-6736(11)60138-4. [DOI] [PubMed] [Google Scholar]
- Vieira E. Legal abortion: Provider's knowledge and its public policy implications. Revista Brasileira de Ginecologia e Obstetrícia. 2012:1–3. [PubMed] [Google Scholar]
- Visaria L. Innovations in Tamil Nadu. Paper presented at Unhealthy Trends: A Symposium on the State of our Public Health System; 2000. Retrieved from. [Google Scholar]
- World Health Organization (WHO) The incidence and prevalence of sexually transmitted infections. A report of a WHO consultation, February 27–March 1, 2002, Treviso, Italy 2002
- World Health Organization (WHO). Progress in reproductive health research. Assisted Reproductive in Developing Countries – Facing up to the Issues, Geneva.2003. [Google Scholar]
- World Health Organization (WHO). Global strategy for prevention and control of sexually transmitted infections: 2006–2015. Breaking the chain of transmission. Geneva: Author; 2007a. [Google Scholar]
- World Health Organization (WHO). Unsafe abortion: Global and regional estimates of incidence of unsafe abortion and associated mortality in 2003. Geneva: Author; 2007b. http://www.who.int/reproductivehealth/publications/unsafeabortion_2003/ua_estimates03.pdf Retrieved from. [Google Scholar]
- World Health Organization (WHO). Geneva: Author; 2009a. Monitoring the geographical distribution of the health workforce in rural and underserved areas.Spotlight on Health Workforce Statistics, Issue 8. [Google Scholar]
- World Health Organization (WHO). New Delhi. Safer pregnancy in Tamil Nadu: From vision to reality. 2009b http://www.who.int/maternal_child_adolescent/documents/tamil_nadu_report/en/ Retrieved from.
- World Health Organization (WHO). Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. Geneva: Author; 2011. [Google Scholar]
- World Health Organization (WHO). Baseline report on Global Sexually Transmitted Surveillance. Geneva: Author; 2012a. [Google Scholar]
- World Health Organization (WHO). Unsafe abortion incidence and mortality: Global and regional levels in 2008 and trends during 1990–2008 . 2012b http://apps.who.int/iris/bitstream/10665/75173/1/WHO_RHR_12.01_eng.pdf Retrieved from.
- World Health Organization (WHO). Geneva. WHO upholds guidance on hormonal contraceptive use and HIV. 2012c http://www.who.int/mediacentre/news/notes/2012/contraceptives_20120216/en/ Retrieved from.
- World Health Organization (WHO). Geneva. Achieving the health-related MDGs. It takes a workforce. 2013a http://www.who.int/hrh/workforce_mdgs/en/ Retrieved from.
- World Health Organization (WHO). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach. Geneva: 2013b. http://www.who.int/hiv/pub/guidelines/arv2013/download/en/ Retrieved from. [PubMed] [Google Scholar]
- World Health Organization (WHO). Country policies and strategies for combating gender based violence. New Delhi: 2013c. http://searo.who.int/entity/gender/data/bangladesh.pdf Retrieved from. [Google Scholar]
- World Health Organization (WHO). Maternal health. 2013d http://www.who.int/topics/maternal_health/en/ Retrieved from. [Google Scholar]
- World Health Organization (WHO). Executive Summary; Geneva: 2013e. A universal truth: No health without a workforce. [Google Scholar]
- World Health Organization (WHO). The world health report: Research on universal health coverage 2013. Geneva: 2013f. [Google Scholar]
- World Health Organization (WHO). Geneva. Global update on the health sector response to HIV, 2014. 2014a http://www.who.int/hiv/pub/progressreports/update2014/en/ Retrieved from.
- World Health Organization (WHO). Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, the World Bank and United Nations Population Division. Geneva: 2014. [Google Scholar]
- World Health Organization . mHealth: New horizons for health through mobile technologies. A global survey on eHealth. Geneva: Author; 2011. http://www.who.int/goe/publications/goe_mhealth_web.pdf Retrieved from. [Google Scholar]
- World Health Organization . WHO issues new HIV recommendations calling for earlier treatment. Geneva: Author; 2013. http://www.who.int/mediacentre/news/releases/2013/new_hiv_recommendations_20130630/en/ Retrieved from WHO Media Center. [Google Scholar]
- Zheng X., Tan L., Ren Q., Cui Z., Wu J., Lin T., et al. Chen H. Trends in contraceptive patterns and behaviors during a period of fertility transition in China: 1988–2006. Contraception. 2012;(3):204–213. doi: 10.1016/j.contraception.2011.12.006. [DOI] [PubMed] [Google Scholar]


