Abstract
Objective
A standardized assay to determine the HPV status of head and neck squamous cell carcinoma (HNSCC) specimens has not yet been established, particularly for cytologic samples. The goal of this study was to determine whether the hybrid capture-2 (HC-2) assay, already widely used for the detection of high risk HPV in cervical brushings, is applicable to cytologic specimens obtained from patients with suspected HNSCCs.
Materials and methods
Fine needle aspirates (FNA) of cervical lymph nodes were pre-operatively obtained from patients with suspected HNSCCs and evaluated for the presence of HPV using the HC-2 assay. HPV analysis was performed on the corresponding resected tissue specimens using p16 immunohistochemistry (IHC) and HR-HPV in situ hybridization (ISH). A cost analysis was performed using the Center for Medicare & Medicaid Services.
Results
HPV status of the cervical lymph node metastases was correctly classified using the HC-2 assay in 84% (21/25) of cases. Accuracy was improved to 100% when cytologic evaluation confirmed the presence of cancer cells in the test samples. The estimated cost savings to CMS using the HC-2 assay ranged from $113.74 to $364.63 per patient.
Conclusions
HC-2 is a reliable method for determining the HPV status of HNSCCs. Its application to HNSCCs may reduce costs by helping to localize the primary site during the diagnostic work-up as well as decrease the interval time of determining the HPV status which would be relevant for providing prognostic information to the patient as well as determining eligibility for clinical trials targeting this unique patient population.
Keywords: HPV, Head and neck cancer, Squamous cell carcinoma, Hybrid capture 2, Fine needle aspiration, Cytology
Introduction
In the past decade, significant evidence has established high risk (HR) human papillomavirus (HPV) as the causative agent in an increasing proportion of incident cases of oropharyngeal squamous cell carcinoma (OPSCC) [1–6]. HPV infection is responsible for up to 80% of oropharyngeal cancers in the United States, and over 90% are caused by one viral type, HPV type 16 [7]. Determining the HPV status of OPSCC is important for several reasons. HPV status can provide prognostic information [8–10], assist with localization of the primary site to the oropharynx in patients presenting with metastatic squamous cell carcinoma to the neck [11,12], as well as determine patient eligibility for clinical trials tailored to this cancer population. Despite the importance of discerning HPV status, there is currently no standard approach for HPV testing of clinical samples. Instead, methods of HPV testing across laboratories vary considerably reflecting the biases and tendencies of individual investigators [13]. Current methods for HPV detection in head and neck clinical samples include type-specific polymerase chain reaction (PCR), real-time PCR (RT-PCR), immunohistochemical detection of surrogate markers such as p16, and HPV deoxyribonucleic acid (DNA) in situ hybridization (ISH). However, the application of these detection methods to cytologic specimens is very limited [14].
The hybrid capture 2 (HC-2) assay is a commercially available microplate analysis approved by the US Food and Drug Administration for the detection of HPV DNA as part of cervical cancer screening [15,16]. It is a liquid-phase hybridization assay that uses a RNA probe mixture for the detection of 13 high risk types of HPV including type 16 [16,17]. We have previously shown that this assay is a highly reliable method of determining HPV status in brushings and aspirates from surgically resected head and neck squamous cell carcinomas (HNSCCs) [18]; but, unrestricted access to tumor cells at the pathology bench may exaggerate its strengths and under-state its limitations as a preoperative tool where true cytologic samples are prone to variability in cellularity and viability. The purpose of this feasibility study is to expand the application of the HC-2 assay to cytologic specimens obtained in vivo from patients with metastatic HNSCC as well as perform a cost analysis of applying this assay in clinical practice.
Materials and methods
Patient recruitment
Patients who presented with cervical lymphadenopathy which was palpable on a head and neck examination were screened for eligibility in the Department of Otolaryngology – Head and Neck Cancer clinic at the Johns Hopkins Hospital (Baltimore, MD). Since cervical lymph nodes 1 cm or greater in size are more often palpable and easily aspirated in a clinical setting without the use of ultrasound-guided techniques, only patients with palpable lymph nodes ≥1 cm were included in this study. After appropriate consent was obtained, twenty-five patients who met the study criteria were enrolled. The clinical study was approved by the Institutional Review Board at the Johns Hopkins Hospital.
Fine needle aspiration biopsy
A fine needle aspiration biopsy (FNAB) of metastatic cervical lymph nodes was performed either in the clinic or in the operating room during an examination under anesthesia of the upper aerodigestive tract. The skin was prepped with an alcohol pad, and a 3 cc syringe (Becton-Dickinson, Franklin Lakes, NJ, USA) with a 25 gauge needle was used to inject 0.2 cc of 1% lidocaine with 1:100,000 epinephrine subcutaneously. The palpable lymph node was secured between two fingers and a 25 gauge needle on a 10 cc syringe was passed percutaneously into the lymph node. With the depressor pulled back to exert negative pressure on the syringe, the needle was passed 3–5 times. The aspirate from the needle was placed onto a Vista Vision HistoBond charged slide (VWR, Arlington Heights, IL, USA). The slide was air-dried and subsequently stained with a Diff-Quik stain. The slide was reviewed by a cytopathologist (ZM) to assess overall cellularity of the specimen. A second pass with a fresh needle was then made into the lymph node, and the aspirate placed into 1 mL of transport medium (Digene/Qiagen Corporation, Valencia, CA, USA) and the vial was stored at −20 °C until the HC-2 assay was performed.
CaSki and SiHa cell lines
Two HPV-associated cancer cell lines, CaSki and SiHa, were obtained from American Type Culture Collection (ATCC). The cells underwent digestion with 20 mg/mL of proteinase K (Roche) in the presence of 1% sodium dodecylsulfate (Bio-rad) at 48 °C for 2 days. DNA was then extracted using UltraPure Phenol:Chloroform:Isoamyl Alcohol reagents (Sigma–Aldrich, USA) following the manufacturer's instructions. DNA was then precipitated in 100% ethanol, centrifuged at 4150 rpm for 45 min, washed in 70% ethanol twice, dissolved in LoTE buffer, and stored at −20 °C. Starting at a concentration of 100 ng of total genomic DNA, the DNA from each cell line then was diluted serially 10-fold.
Hybrid capture 2 liquid-phase assay
A modified HC-2 HPV assay (Digene/Qiagen Corporation) was used to test the FNA samples for the presence of HR-HPV DNA. This test qualitatively screens for 13 HR-HPV types (including 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68) by in vitro nucleic acid hybridization with signal amplification using chemiluminescence on a microplate. Briefly, the collected samples in the transport medium were denatured to single-stranded DNA by mixing the samples with the denaturation reagent and incubated in a 65 °C water bath for 45 min. Samples were applied to the hybridization microplate, mixed with the HR-HPV specific RNA probe mixture, and incubated at 65 °C for 60 min. The capture step was then performed by applying the samples to microplate wells coated with RNA/DNA hybrid-specific antibodies and shaken at 1100 rpm at 25 °C for 60 min. The hybrid detection phase was then completed by mixing hybrid samples with alkaline phosphatase-conjugated antibodies (Detection reagent I), and signal amplification performed with incubation with Detection Reagent II. Sample scores were based on a ratio of the relative light unit (RLU) per positive control (CO). A RLU/CO score ≥2.5 was considered positive for the presence of high-risk HPV DNA. All RLU/CO scores <0.85 were considered negative for the presence of HR-HPV DNA. RLU/CO scores in the range of 0.85–2.5 were interpreted as equivocal for HR-HPV. Both positive and negative calibrators were used per the manufacturer's instructions and were run with each plate. In addition to quality control, calibration was performed with each run to ensure that the reagents and furnished calibrator material were functioning properly.
p16 Immunohistochemistry
HPV status on the resected cancers was confirmed within the tumor by overexpression of p16 which is induced by HPV E7 onco-protein activity. Briefly, five micron sections of formalin fixed paraffin-embedded (FFPE) tissue were deparaffinized and subjected to antigen retrieval using 10 mM of citrate buffer (92 °C for 30 min). Expression of p16 was evaluated using a mouse monoclonal antibody against p16 (MTM Laboratories, Heidelberg, Germany), the visualization was performed using the Ultra View polymer detection kit (Ventana). p16 expression was scored as positive if strong and diffuse nuclear and cytoplasmic staining was present in >70% of the tumor (Fig. 1).
Fig. 1.
Human papillomavirus-associated head and neck squamous cell carcinoma confirmed by p16 immunohistochemistry.
HPV DNA in situ hybridization
HPV DNA analysis also was performed on tissue specimens from patients who had undergone resections of their head and neck tumors. Briefly, five micron FFPE tissue sections from resected tumors or biopsies were conditioned with Ventana cell conditioner #2 and ISH-protease 3. Hybridization was performed using the HPV III Family16 probe set that captures the HR-HPV genotypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 and 66. The fluorescein-labeled probes that identify the HR genotypes were detected with the ISH iVIEW Blue Plus Detection Kit (Ventana Medical Systems, Inc., Tucson, AZ). Punctate hybridization signals localized to the tumor cell nuclei defined an HPV-associated tumor.
Cost analysis
The Center for Medicare & Medicaid Services (CMS) payor perspective was taken for this analysis. CMS uses two standardized coding systems for processing claims: International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) and Health Care Common Procedure Coding System (HCPCS), which incorporates the Current Procedural Terminology, Fourth Edition (CPT-4). CMS’ Physician fee schedule was used to identify medical procedures using HCPCS codes (code 10021 FNA biopsy in clinic; code 42800 biopsy of oropharynx and code 31535 laryngoscopy, direct operative with biopsy). Anesthesia services were identified using anesthesia CPT-4 codes (code 00170 for anesthesia for intra-oral procedures, including biopsy). The clinical laboratory fee schedule was used to estimate payments for HPV DNA detection (code 87621) and p16 immunohistochemistry (code 88342) for OPSCC. This payor perspective cost analysis would vary based on the health care structure of varying countries and institutes.
Results
Patient demographics
Twenty-five patients who presented with cervical lymphadenopathy which were easily palpated and greater than 1.0 cm in size were enrolled into the study. The relevant clinical and pathologic findings are summarized in Table 1. Twelve patients had HNSCC that was HPV-associated and originated in the palatine tonsils (n = 5), base of tongue (n = 6), and from an unknown primary site (n = 1). Six patients had HPV-negative HNSCC, and these arose in the palatine tonsil (n = 1), base of tongue (n = 2), hypopharynx (n = 1), skin of the auricle (n = 1) and from an unknown primary site (n = 1). In the remaining seven patients, the cervical lymphadenopathy was related to lymphoma (n = 2) or a non-neoplastic inflammatory process (n = 5).
Table 1.
Hybrid Capture 2 analysis of aspirated enlarged lymph nodes.
| Patient # | Tumor type | Tumor origin | p16 IHC | HPV-HR ISH | HC-2 (RLU) | Tumor in cytology |
|---|---|---|---|---|---|---|
| 1 | SCC | Tonsil | Positive | Positive | Positive (4.27) | Yes |
| 2 | SCC | Tonsil | Positive | Positive | Equivocal (1.05) | No |
| 3 | SCC | Tongue Base | Positive | Positive | Positive (9.96) | No |
| 4 | SCC | Tongue Base | Positive | Positive | Negative (0.38) | No |
| 5 | SCC | Tonsil | Positive | N/A | Positive (16.8) | Yes |
| 6 | SCC | Tongue Base | Positive | Positive | Positive (6.3) | Yes |
| 7 | SCC | Tonsil | Positive | Positive | Positive (167) | No |
| 8 | SCC | Tonsil | Positive | Positive | Negative (0.28) | No |
| 9 | SCC | Tongue Base | Positive | Positive | Positive (402.8) | Yes |
| 10 | SCC | Tongue Base | Positive | Positive | Positive (173.5) | No |
| 11 | SCC | Tongue Base | Positive | Positive | Negative (0.9) | No |
| 12 | SCC | Unknown | Positive | Positive | Positive (112) | N/A |
| 13 | SCC | Tongue Base | Negative | Negative | Negative (0.14) | Yes |
| 14 | SCC | Tongue Base | Negative | Negative | Negative (0.15) | Yes |
| 15 | SCC | Tonsil | Negative | Negative | Negative (0.44) | Yes |
| 16 | SCC | Unknown | Negative | Negative | Negative (0.15) | Yes |
| 17 | SCC | Hypopharynx | Negative | Negative | Negative (0.25) | Yes |
| 18 | Benign | Supraglottis | Negative | N/A | Negative (0.22) | No |
| 19 | Benign | Benign (Inflammation) | Negative | N/A | Negative (0.13) | No |
| 20 | SCC | Auricle | Negative | N/A | Negative (0.19) | No |
| 21 | Benign | Benign (Inflammation) | N/A | N/A | Negative (0.2) | No |
| 22 | Benign | Lymph Node | N/A | N/A | Negative (0.17) | No |
| 23 | CLL | Lymph Node | N/A | N/A | Negative (0.6) | No |
| 24 | Lymphoma | Lymph Node | N/A | N/A | Negative (0.18) | No |
| 25 | Benign | Benign (Inflammation) | N/A | N/A | Negative (0.22) | No |
HPV DNA detectable in FNAB of cervical lymph nodes using the HC-2 assay
The results from the p16 IHC and HC-2 assay are summarized in Table 1. HR-HPV ISH was also performed when tissue was available for testing (Table 1). Cytology was able to provide a diagnosis of cancer in 71% (17/24) of the cases and in only 36% (4/11) of the HPV-positive HNSCCs. In contrast, the HPV status of cervical lymph node metastases was correctly classified using the HC-2 assay in 84% (21/25) of cases. Of the 12 HPV-positive HNSCCs, HC-2 detected HPV DNA in 67% (8/12) of the FNAs. In the 4 HPV-positive HNSCCs where HPV DNA was not detected by HC-2, tumor cells also were not identified by cytologic evaluation of the FNA study samples (i.e. cellular inadequacy). Thus, accuracy of the HC-2 assay was improved to 100% when cytologic evaluation confirmed the presence of tumor cells in the test samples thus diminishing the impact of false negative results. All of the benign lymph nodes and non-HPV associated HNSCC cases were negative by the HC-2 assay. Overall, the positive predictive value of the HC-2 assay was 66% and the negative predictive value was 100%.
Minimum threshold of 30,000 viral copy numbers detectable by HC-2
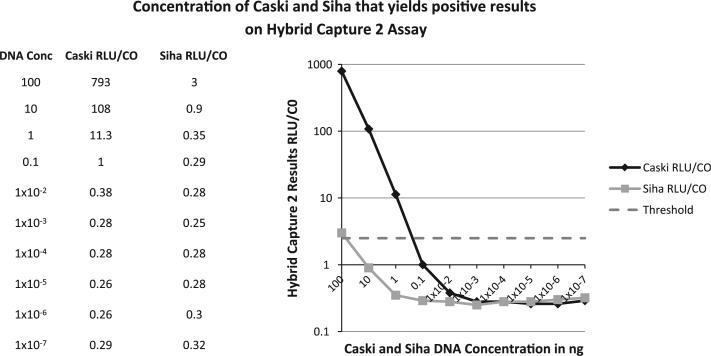
To determine the minimum viral copy number of HPV detectable by the HC-2 assay, we performed serial dilutions with the HPV-associated cancer cell lines, SiHa (which harbors 1–2 copies of HPV-16 DNA/genome) and CaSki (which harbors 600 copies of HPV-16 DNA/genome). A RLU/CO threshold greater than 2.5 was determined positive. With the HC-2 assay, we found that HPV DNA was detected in SiHa at a minimum concentration of 100 ng of DNA and in CaSki at a concentration between 1.0 and 0.1 ng of DNA (Fig. 2). Based on a haploid DNA weight of 3.3 pg and a diploid human genomic DNA weight of 6.6 pg, we determined that the HC-2 assay is able to detect a minimum of 30,000 HPV viral copy numbers.
Fig. 2.
Serial dilutions of HPV DNA to determine the minimum threshold of detection with the HC-2 liquid-phase assay. A RLU/CO of 2.5 was determined the threshold of HPV positivity. HPV DNA in the CaSki cell line (600 copies of HPV DNA/genome) is detected at concentrations of 100 ng, 10 ng and 1 ng and the signal becomes equivocal at 0.1 ng. The SiHa cell line (1–2 copies of HPV DNA/genome) is detected at a concentration of 100 ng and the signal is lost at lower dilutions.
Cost analysis of HC-2 assay in determining HPV status
The 2013 CMS payment to obtain a biopsy sample of the oropharynx in clinic and to perform p16 immunohistochemistry testing to diagnose HPV-associated disease is $232.75, whereas to obtain a biopsy sample in the operating room under general anesthesia and to perform p16 immunohistochemistry testing is $483.64. In contrast, to obtain a FNA biopsy sample of a metastatic cervical lymph node and to perform HC-2 testing to diagnose HPV-associated disease is $119.01. Therefore, the estimated cost savings to CMS ranges from $113.74 to $364.63 per patient depending on whether the biopsy was performed in clinic or in the operating room, respectively.
Discussion
We present the feasibility of using HC-2 in vivo for the detection of HPV DNA in FNAB of head and neck cancer patients. The HC-2 is a standardized assay and available in most medical centers to diagnose HPV-related neoplasia of the female cervix and may represent an efficient means of determining the HPV status of HNSCCs as well. We have previously shown that this assay is a highly reliable method of determining HPV status in brushings and aspirates from surgically resected head and neck squamous cell carcinomas (HNSCCs) [18] and the purpose of this study was to establish the feasibility and expand the application of the HC-2 assay to cytologic specimens obtained in vivo from patients with metastatic HNSCC. In those samples where cytology confirmed the presence of tumor cells, we found a 100% detection rate of HPV DNA in metastatic HPV-positive HNSCC using HC-2. Interestingly, we found that cytology was able to diagnose squamous cell cancer in only 36% of HPV-positive HNSCC samples due to the high frequency of acellular fine needle aspirates in the setting of cystic or necrotic cervical lymph nodes present in this patient population [19]. However, despite an insufficient amount of tumor cells within the needle aspirate, HC-2 was able to detect HPV DNA in 67% of FNA samples which is an almost two-fold diagnostic yield over conventional FNA cytology alone. Therefore, this assay may be a valuable diagnostic tool not only for solid but also cystic metastatic cervical lymph nodes which harbor HPV DNA from necrotic tumor cells.
Another advantage of the HC-2 assay in the diagnostic evaluation of HPV-positive HNSCC is that there is no need to generate a tumor block for HPV testing which is the current clinical practice; rather, the FNA aspirate can be used directly to evaluate for the presence of HPV DNA. Similar to the clinical work-up of thyroid cancer, we propose an algorithm that at the time of the initial diagnostic FNAB, a second pass be obtained in the clinic and the aspirate placed in the HC-2 transport medium and stored for future molecular testing of HPV DNA. If HNSCC is diagnosed cytologically or if the FNA is non-diagnostic and there is a high suspicion for an HPV-associated malignancy, the stored FNA sample can be submitted for molecular genetic testing to evaluate for the presence of HPV DNA using the HC-2 assay.
Furthermore, diagnosing HPV-positive HNSCC with a FNA biopsy using the HC-2 assay may provide cost savings for the payer. Medicare reimbursement rates used in the analysis showed that up to $364.63 per patient could be saved if HPV-positive disease is diagnosed with a FNAB procedure using the HC-2 assay as compared to a biopsy performed either in the clinic or in the operating room using p16 IHC. We are not advocating that the FNAB approach of diagnosing HPV-positive HNSCC replace the need to perform an operative staging endoscopy. Rather, HC-2 would be useful in patients with inoperable disease in whom staging endoscopy would unlikely add value, in patients whom inadequate tissue remains following biopsy for HPV testing and, most importantly, to help direct the surgeon to the palatine and lingual tonsils to identify the primary site at the time of the diagnostic endoscopy, especially when patients present when cervical lymphadenopathy in the absence of a clinically obvious primary tumor.
The limitations of the HC-2 assay are several. First, in this assay, HPV DNA is not amplified and the negative predictive value may be compromised in cases in which HPV viral copy number is low. We have determined that a minimum number of 30,000 HPV viral copy numbers is required in the sample in order to detect HPV DNA with this assay. This limitation is highlighted in a pilot study with oropharyngeal brushings of the primary site in which half of the cases failed to detect HPV DNA for those discrete, submucosal tumors (data not shown). Since HPV-associated HNSCC start in the crypts, there may be an insufficient amount of viral copy numbers on the surface epithelium from where the brushings were obtained. Second, the HC-2 assay has no internal gene control, such as a housekeeping gene, which can be used to determine sample sufficiency. Therefore, it is not possible to determine if the results are due to an insufficient amount of DNA or whether the result is a true negative. This limitation is addressed by the Cervista® HPV HR test. Like the HC-2 method, the Cervista® HPV HR test is a liquid phase assay that is clinically validated for HPV detection in cervical cytologic specimens. Its analytical sensitivity is comparable to that of HC-2, but the addition of a housekeeping gene as an internal control to ensure sufficient cellularity diminishes the likelihood of false negative results.
Despite these limitations, our data demonstrate that HC-2 is a reliable method for determining the HPV status of HNSCC. Furthermore, given the accuracy of the HC-2 assay with the presence of cancer cells, this method can increase the diagnostic yield of fine needle aspiration cytology. Application to lymph node aspirates may reduce cost, decrease the interval time in diagnosing HPV-positive HNSCC, and direct the surgeon to the palatine and lingual tonsils at the time of the diagnostic endoscopy. Future studies need to be performed to determine the utility of HC-2 assay in oropharyngeal brushings and in the screening of non-cancer patients for the detection of persistent oral HPV infection which is one of the main risk factors for the development of HPV-positive HNSCC.
Acknowledgement
This work was funded by the NIH/NCI Grant 1R21CA176332-01 (SIP).
Footnotes
Conflict of interest statement
None declared.
References
- 1.D'Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356:1944–56. doi: 10.1056/NEJMoa065497. [DOI] [PubMed] [Google Scholar]
- 2.Herrero R, Castellsagué X, Pawlita M, Lissowska J, Kee F, Balaram P, et al. Human papillomavirus and oral cancer: the International Agency for Research on Cancer multicenter study. J Natl Cancer Inst. 2003;95(23):1772–83. doi: 10.1093/jnci/djg107. [DOI] [PubMed] [Google Scholar]
- 3.Applebaum KM, Furniss CS, Zeka A, Posner MR, Smith JF, Bryan J, et al. Lack of association of alcohol and tobacco with HPV16-associated head and neck cancer. J Natl Cancer Inst. 2007;99:1801–10. doi: 10.1093/jnci/djm233. [DOI] [PubMed] [Google Scholar]
- 4.Smith EM, Ritchie JM, Summersgill KF, Hoffman HT, Wang DH, Haugen TH, et al. Human papillomavirus in oral exfoliated cells and risk of head and neck cancer. J Natl Cancer Inst. 2004;96:449–55. doi: 10.1093/jnci/djh074. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz SM, Daling JR, Doody DR, Wipf GC, Carter JJ, Madeleine MM, et al. Oral cancer risk in relation to sexual history and evidence of human papillomavirus infection. J Natl Cancer Inst. 1998;90:1626–36. doi: 10.1093/jnci/90.21.1626. [DOI] [PubMed] [Google Scholar]
- 6.Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709–20. doi: 10.1093/jnci/92.9.709. [DOI] [PubMed] [Google Scholar]
- 7.Marur S, D'Souza G, Westra WH, Forastiere AA. HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol. 2010;11:781–9. doi: 10.1016/S1470-2045(10)70017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar B, Cordell KG, Lee JS, Warden FP, Prince ME, Tran HH, et al. EGFR, p16, HPV titer, Bcl-xL and p53, sex, and smoking as indicators of response to therapy and survival in oropharyngeal cancer. J Clin Oncol. 2008;26:3128–37. doi: 10.1200/JCO.2007.12.7662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Licitra L, Perrone F, Bossi P, Suardi S, Marcomini B, DaRiva L, et al. High-risk human papillomavirus affects prognosis in patients with surgically treated oropharyngeal squamous cell carcinoma. J Clin Oncol. 2006;24:5630–6. doi: 10.1200/JCO.2005.04.6136. [DOI] [PubMed] [Google Scholar]
- 11.Begum S, Gillison ML, Ansari-Lari MA, Shah K, Westra WH. Detection of human papillomavirus in cervical lymph nodes: a highly effective strategy for localizing site of tumor origin. Clin Cancer Res. 2003;9:6469–75. [PubMed] [Google Scholar]
- 12.Begum S, Gillison ML, Nicol TL, Westra WH. Detection of human papillomavirus-16 in fine-needle aspirates to determine tumor origin in patients with metastatic squamous cell carcinoma of the head and neck. Clin Cancer Res. 2007;13:1186–91. doi: 10.1158/1078-0432.CCR-06-1690. [DOI] [PubMed] [Google Scholar]
- 13.Westra WH. The morphologic profile of HPV-related head and neck squamous cell carcinoma: implications for diagnosis, prognosis and clinical management. Head Neck Pathol. 2012;6(Suppl 1):S48–54. doi: 10.1007/s12105-012-0371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holmes BJ, Westra WH. The expanding role of cytopathology in the diagnosis of HPV-related squamous cell carcinoma of the head and neck. Diagn Cytopathol. 2013 Jun;8:253. doi: 10.1002/dc.23014. [DOI] [PubMed] [Google Scholar]
- 15.Cervix Cancer Screening. IARC Press; Lyon: 2005. IARC Working Group on the Evaluation of Cancer Preventive Strategies. [Google Scholar]
- 16.Carozzi FM, Del Mistro A, Confortini M, Sani C, Puliti D, Trevisan R, et al. Reproducibility of HPV DNA testing by hybrid capture 2 in a screening setting. Am J Clin Pathol. 2005;124:716–21. doi: 10.1309/84E5-WHJQ-HK83-BGQD. [DOI] [PubMed] [Google Scholar]
- 17.Bozzetti M, Nonnenmacher B, Mielzinska I, Villa L, Lorincz A, Bretenback VV, et al. Comparison between hybrid capture II and polymerase chain reaction results among women at low risk for cervical cancer. Ann Epidemiol. 2000;10:466. doi: 10.1016/s1047-2797(00)00147-2. [DOI] [PubMed] [Google Scholar]
- 18.Bishop JA, Maleki Z, Valsamakis V, Ogawa T, Chang X, Pai SI, et al. Application of the hybrid capture 2 assay to squamous cell carcinomas of the head and neck: a convenient liquid phase approach for the reliable determination of human papillomavirus status. Cancer Cytopathol. 2012;120(1):18–25. doi: 10.1002/cncy.20175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldenberg D, Begum S, Westra WH, Khan Z, Sciubba J, Pai SI, et al. Cystic lymph node metastasis in patients with head and neck cancer: an HPV-associated phenomenon. Head Neck. 2008;30(7):898–903. doi: 10.1002/hed.20796. [DOI] [PubMed] [Google Scholar]