Abstract
We estimated hypertension and diabetes prevalence among US homeless adults compared with the general population, and investigated prevalence trends. We systematically searched 5 databases for published studies (1980–2014) that included hypertension or diabetes prevalence for US homeless adults, pooled disease prevalence, and explored heterogeneity sources. We used the National Health Interview Survey for comparison.
We included data from 97 366 homeless adults. The pooled prevalence of self-reported hypertension was 27.0% (95% confidence interval = 23.8%, 29.9%; n = 43 studies) and of diabetes was 8.0% (95% confidence interval = 6.8%, 9.2%; n = 39 studies). We found no difference in hypertension or diabetes prevalence between the homeless and general population.
Additional health care and housing resources are needed to meet the significant, growing burden of chronic disease in the homeless population.
In 2012, the estimated US homeless population was a little more than 630 000 individuals at any single point in time.1 There are 2.5 to 3.5 million people, or 0.9% to 1.2% of the US population, homeless over the course of a year.2 Lifetime prevalence of homelessness has been estimated to be even higher, at 7.4%.3 These estimates share a definition of homelessness known as “literal homelessness,” referring to individuals with no stable residence living either in a temporary shelter or unsheltered location not meant for habitation (e.g., the street, a subway station, or a parked car). Another definition of homelessness, used by the US Department of Education, for example, would include those who are “doubled-up,” or staying in temporary arrangements with friends or family.4
Homeless individuals have significant health needs in several domains, including chronic diseases, communicable diseases, mental health, and substance abuse.5 In addition, other common reasons for seeking health care include environmental insults such as injuries, insect bites, and complications from heat and cold exposure. All contribute to significant premature mortality in this population,6–10 with an average estimated life expectancy of 42 to 52 years for chronically homeless individuals.11 Factors contributing to the health problems of homeless people include extreme poverty, inadequate access to health care, nonadherence to therapy, and the adverse health effects of homelessness itself.12,13 Those who are homeless identify lack of health insurance and financial resources as key barriers to accessing health care.13 Homeless individuals may be exposed to harsh outdoor environments or crowding in temporary shelters. They may even lack access to clean water and basic hygiene supplies. For these reasons, a cycle is created in which poor health is a risk factor for homelessness and homelessness increases health needs.5
There is growing consensus that the adult homeless population in the United States is aging.14–16 This trend, which applies primarily to single homeless adults rather than families, is hypothesized to result from multiple economic and social challenges facing the cohort born in the late 1950s to early 1960s, including the economic recession of the 1980s and the crack cocaine epidemic.15
Although the mean age of the homeless population is increasing, the adult homeless population is still overall younger than the US population.17 The much lower proportion of adults aged older than 62 years in the homeless population reflects the premature mortality of this group. Age is a well-known risk factor for many chronic diseases, including hypertension and diabetes. The homeless have been shown to have rates of chronic disease in middle age that are comparable to those of older adults.18 Thus, the effects of an aging trend among the homeless on chronic disease rates may be magnified.
Reported rates of diabetes and hypertension in the homeless population range from 2% to 18% for diabetes and 18% to 41% for hypertension.19–23 Reasons for this variation include different disease measurement approaches (e.g., self-report vs physiological methods), study setting, sampling, and when the study was conducted. Among the homeless population, cardiovascular disease has been identified as the second leading cause of death, after injuries or overdoses.6
In the general US population, both hypertension and diabetes are common chronic diseases. The incidence and prevalence of hypertension are increasing in the United States; the number of adults with hypertension more than doubled between 1995 and 2005.24 Hypertension occurs in 29% to 31% of US adults and is the most common reason for prescription medication.25 Hypertension is more common in African Americans than in Whites and in men than in women.26 Treating hypertension reduces the risk of developing heart failure, myocardial infarction, and stroke.27 In 2010, the estimated prevalence of diagnosed diabetes for US adults was 8.2% and has been sharply increasing since the mid-1990s.28 Diabetes is also more common in racial minorities.29 It is the seventh leading cause of death and a major contributor to cardiovascular disease, the leading cause of US deaths.29
In the homeless population, African American race is overrepresented by about 200%.30 Rates of heavy alcohol use, which contributes to the development of hypertension, are also high in the homeless population.31 In addition, diets provided by food pantries and meal programs are often high in sodium,32 which may contribute to or exacerbate hypertension. Furthermore, a paradoxical association has been made between food insecurity and obesity, another risk factor for both diseases.33 In a national sample of chronically homeless adults, 57% were overweight or obese.34 Finally, it has been hypothesized that the chronic stress of homelessness could contribute to the development of hypertension, though this has not been explicitly studied.
Homeless adults are known to be high utilizers of the health care system.35 They are up to 5 times more likely to be admitted to the hospital than the general population36 and often obtain care in the emergency department because of poor access to primary care services.37 A subpopulation of the homeless are “superutilizers” with extreme levels of health care use.38 These utilization patterns are associated with high health care costs39 and suggest that the current safety net is inadequate to support the health care needs of the homeless population. Identification of key trends in chronic disease rates among the homeless population will help public health organizations plan for allocation of appropriate resources to meet the growing health needs of this population.
In light of the variations in previously published rates of diabetes and hypertension in the homeless population and indications of an aging trend in the homeless population over time, the primary aim of this study was to determine the prevalence of hypertension and diabetes in homeless adults in the United States between 1980 and 2014. Secondary aims were (1) to compare the prevalence of each disease to the background prevalence in the United States, (2) to investigate trends in the prevalence of each disease over time between 1980 and 2014, and (3) to explain the variation in estimates of disease prevalence among the various studies.
METHODS
This study adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations for reporting on systematic reviews.40
Search Strategy
We conducted a systematic search of published articles with Medline, PsychINFO, Cumulative Index to Nursing and Allied Health Literature, Cochrane, and Science Citation Index. Search terms varied slightly on the basis of controlled vocabulary for all databases except Science Citation Index (which lacks a controlled vocabulary). We chose the search terms following a review of Medical Subject Heading terms used in a variety of articles known to meet inclusion criteria. As a representative example, the Medline search strategy is shown in Table 1. (A complete list of search strategies for all databases is provided in Table A, available as a supplement to the online version of this article at http://www.ajph.org.)
TABLE 1—
Sample Medline Search Strategy Using Controlled Vocabulary
| Homeless | [Homeless persons OR homeless.mp OR street people.mp OR homeless*.mp] AND |
| Diabetes | [Diabetes mellitus OR diabetes mellitus.mp OR |
| Hypertension | Hypertension OR hypertension.mp OR high blood pressure.mp OR |
| Chronic disease | Chronic disease OR chronic disease.mp OR |
| Health status | Health status OR health status.mp] |
We limited the search to studies published after January 1, 1980, and to the English language because the review only includes studies conducted in the United States. The final search date was April 24, 2014. We did not include unpublished data in the analysis because of difficulty assessing the study design and quality of these studies and problems with a lack of a systematic method of rigorously searching for such sources. However, we evaluated published theses for eligibility. We also searched the reference lists of the studies that met eligibility criteria, as well as those of review articles about chronic disease, hypertension, diabetes, or cardiovascular disease in the homeless population.
Eligibility Criteria and Review Process
We established criteria for eligibility before beginning review of search results. Inclusion criteria were publication in the English language on or after January 1, 1980, and studies conducted in the United States that presented prevalence data on diabetes and hypertension among homeless adults. Studies that we excluded were those that were unpublished; did not contain primary data; were not in English or were conducted outside the United States; were published before January 1, 1980; were not conducted in homeless adults; included children aged younger than 18 years; did not contain hypertension or diabetes prevalence data; or presented duplicate data of other included studies. (See Supplement B, available as a supplement to the online version of this article at http://www.ajph.org, for a full description of eligibility criteria.)
We removed exact duplicates automatically; we removed near duplicates after manual review. The primary reviewer (R. S. B.) then performed a preliminary review by title and abstract to remove articles that were clearly not relevant to the study question or did not meet eligibility criteria. Two reviewers (R. S. B. and E. J. P.) independently reviewed the remaining articles in full text, and they each noted whether the article should be included or excluded, and if so, the reason for exclusion. If an article had multiple reasons for exclusion, they chose the primary reason for exclusion in the order in which they were listed on the eligibility form (Supplement B, available as a supplement to the online version of this article at http://www.ajph.org). They discussed all articles until they reached consensus about study eligibility; a third reviewer resolved remaining discrepancies (L. N. M.).
Data Collection and Quality Assessment
The principal investigator created a preliminary data abstraction form based upon data elements of interest and piloted with included studies. Three independent reviewers (R. S. B., L. N. M., and J. L. J.) performed data abstraction. For each article, a primary reviewer first abstracted all available data elements. A secondary reviewer then confirmed all data. Discrepancies were discussed and consensus achieved.
The goal of quality assessment was to determine the quality of the disease prevalence estimate provided by each study. Thus, the quality scores are an assessment of the study’s quality in estimating disease prevalence and not in achieving the individual aims of each study.
Two independent investigators (R. S. B. and J. S. J.) conducted quality ratings by using an adaptation of the disease prevalence quality tool created by Loney et al.41 This tool, originally developed to assist in evaluating studies of the prevalence of dementia, has subsequently been adapted to evaluate the quality of prevalence estimates of other conditions.42 We assessed 3 overall factors contributing to quality of prevalence estimate: validity of the study methods, accurate interpretation of the results, and applicability of the results. As listed in Table 2, we modified the tool by separating the interpretation of results by use of appropriate statistical methods and analysis by subgroups (item 7 of the original tool) into 2 items. This separation gave us 9 total items and produced a score of 0 to 9. (For more information about application of this quality assessment tool, see Supplement C, available as a supplement to the online version of this article at http://www.ajph.org). We calculated interrater reliability between reviewers by using the Spearman rank correlation coefficient, defining high correlation as a coefficient greater than 0.75.43
TABLE 2—
Adapted Quality Assessment Tool for Systematic Review of Hypertension and Diabetes Prevalence in Homeless Adults in the United States, 1980–2014
| Questions | Loney41—Prevalence of Dementiaa | Adaptation—Prevalence of Hypertension and Diabetes in Homeless Adultsb |
| Are the study methods valid? | Are the study design and sampling method appropriate for the research question? | Is a probability sample taken or the whole population surveyed? |
| Is the sampling frame appropriate? | Is the sampling frame (list or method for study recruitment) appropriate? | |
| Is the sample size adequate? | Is the sample size adequate? | |
| Are objective, suitable, and standard criteria used for the measurement of the health outcome? | Are objective, suitable, standard methods used for the measurement of the health outcome? | |
| Is the health outcome measured in an unbiased fashion? | Is the health outcome measured with the same method for all participants? | |
| Is the response rate adequate? Are the refusers described? | Is the response rate adequate? Are those who refused or were not included described? | |
| What is the interpretation of the results? | Are the estimates of prevalence or incidence given with confidence intervals and in detail by subgroup, if appropriate? | Are adequate statistical methods presented in the manuscript? |
| Are the estimates of prevalence given in detail by subgroups? | ||
| What is the applicability of the results? | Are the study participants and the setting described in detail and similar to those of interest to you? | Are the study participants and the setting described in detail? Do the participants seem to represent the overall population of homeless adults? |
0 or 1 point each; total score 0–8.
0 or 1 point each; total score 0–9.
Comparison With the General Population
We made all comparisons by using data from the National Health Interview Survey (NHIS), a national probability survey containing self-reported chronic disease information. It has been conducted in the United States annually between 1980 and 2013 (data currently available through 2012). We chose a nationally representative sample of self-reported disease data rather than a sample containing physiological measurements because few studies using physiological measurements from the homeless sample were available to use for comparison.
Annual prevalence rates of diabetes from NHIS were available in published summary.44 For hypertension, we manually extracted annual self-reported disease prevalence from the NHIS Web-tool Integrated Health Interview Series45 by using the NHIS variable “hypertenev,” which asked respondents “Have you ever been told that you have hypertension?”
Analysis
Study description and synthesis of results.
We used descriptive statistics to summarize the number and percentage of studies with various characteristics, including types of study design, sample selection, sample recruitment locations, year of data collection, and study region. We also described sample characteristics, including definition of homelessness used, prevalence of chronic homelessness, sample age, race, gender, employment status, veteran status, and insurance status.
We calculated prevalence estimates for hypertension and diabetes by using a random effects model with study-level prevalence estimates, and we used the Wilson method to calculate 95% confidence intervals for those estimates.46 We used the same methods to calculate prevalence estimates for mental health diagnoses, substance use disorders, and other medical conditions.
Risk of bias.
We appraised study quality with the adapted standardized tool. We averaged scores from both reviewers to yield an overall quality rating for each study. We determined a cut-off point for a binary division between lower- and higher-quality scores by visual analysis of score distribution. On the basis of this distribution, we established a cut-off to define lower-quality studies as those with an average score less than or equal to 4, and higher-quality defined as an average score greater than 4. We examined this binary score as a potential source of heterogeneity between studies. Furthermore, we performed component analysis of the 9 individual items included, to identify which, if any, items were of primary importance to study quality.
Additional analyses.
We assessed the presence of heterogeneity visually by using Galbraith plots,47 and I 2.48 We interpreted degree of heterogeneity as low, moderate, and high corresponding to I 2 values of 25%, 50%, and 75%, respectively.49 We explored heterogeneity in our data by using meta-regression. Potential variables that could contribute to heterogeneity included year of publication; mean study age; gender; race; prevalence of substance abuse, smoking, and chronic homelessness; study design; and method of sample selection. We evaluated trends in the mean sample age by study year by using a nonparametric test for trend across ordered groups, developed by Cuzick,50 which is an extension of the Wilcoxon rank-sum test and incorporates a correction for ties. In addition, we compared the pooled prevalence of hypertension and diabetes in the homeless population with the estimated prevalence in the general US population from NHIS by adding the NHIS prevalence rates, by year, with standard errors to the meta-analysis data set.
We used random effects meta-regression to compare the prevalence rates between the homeless and general population, with and without adjustment for study year. In brief, meta-regression pools data by using a least-squares approach with analytic weighting of study by ζ, a measure of between-study heterogeneity. We compared the rates of change in prevalence of both diseases over time observed in the homeless and general population data sets by testing for the significance of the interaction between the groups (homeless vs general population) and study year. We used an alpha of .05 throughout. We performed all analyses with Stata version 13.1 (StataCorp LP, College Station, TX).
RESULTS
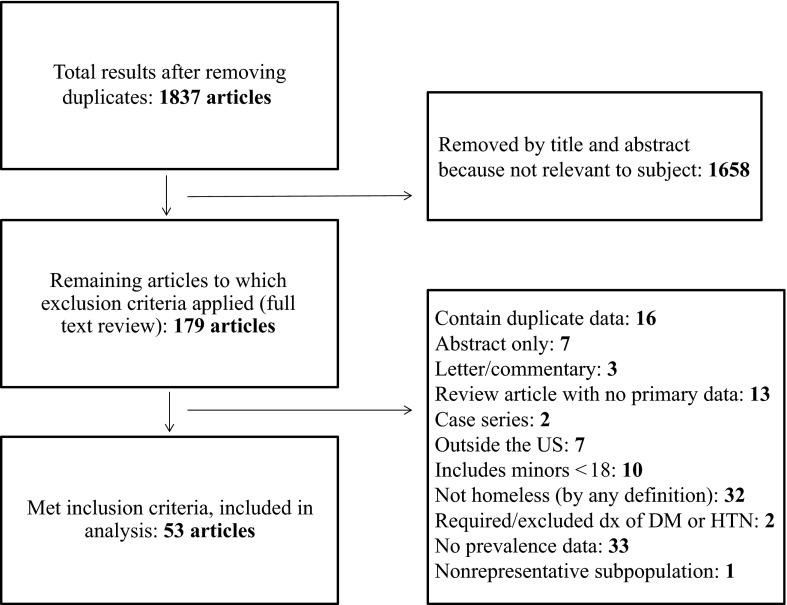
We identified a total of 1837 unduplicated articles with our search strategy. Of these, we eliminated 1658 by title and abstract. We examined the remaining 179 articles in full text, yielding 53 articles for inclusion. Reasons for exclusion are detailed in the PRISMA flowchart (Figure 1).
FIGURE 1—
Systematic review search results and reasons for exclusions: diabetes and hypertension prevalence in homeless adults in the United States, 1980–2014.
Note. DM = diabetes mellitus; dx = diagnosis; HTN = hypertension.
Description of Studies Included
The 53 included studies had considerable heterogeneity in their individual study aims. Many described the health status of a local homeless population,14,21,51–60 whereas others examined health behaviors or health risks.61–63 Although the search strategy targeted studies that included the prevalence of hypertension or diabetes, some studies had broad health foci, and others focused on specific conditions.64–67 Two studies examined the nutritional status of the diets of homeless individuals.32,68 Other studies explored health care access or utilization among the homeless.34,53,69–71 There were 2 subpopulations targeted by multiple studies: older homeless individuals53,72–76 and women.32,61,75,77,78
All included studies shared an observational study design. The majority of included studies were prospective cross-sectional samples, whereas 23% of studies were retrospective medical chart reviews. Sample selection was by probability or census in more than 50% of studies. The majority of studies had fewer than 200 participants; 76% of studies included fewer than 400 participants. However, 6 studies had more than 1000 participants and 3 had more than 3000. A total of 97 366 homeless adult participants were sampled across all the included studies. The sampling frame overall focused on temporary housing shelters and medical clinics serving the homeless, with fewer than 25% of studies including unsheltered homeless. Studies were concentrated on the East Coast, but sampled all regions of the United States; 6 studies were regional or national. The included studies focused on urban regions, with only a single study targeting the rural homeless.77 (See Tables 3 and 4 for detailed study characteristics.)
TABLE 3—
Summary Characteristics of Included Studies on Diabetes and Hypertension Prevalence in Homeless Adults in the United States, 1980–2014
| Study Characteristic (No. of Studies Reporting) | No. of Studies (%) |
| Study design (n = 53) | |
| Observational | 53 (100) |
| Prospective | 41 (77.4) |
| Retrospective | 12 (22.6) |
| Sample selection (n = 53) | |
| Census | 17 (32.1) |
| Probability | 13 (24.5) |
| Convenience | 16 (30.2) |
| Not specified | 7 (13.2) |
| Sample size (n = 53) | |
| < 200 | 31 (58.5) |
| 200–399 | 9 (17.0) |
| 400–599 | 4 (7.6) |
| 600–799 | 1 (1.9) |
| 800–999 | 2 (3.8) |
| 1000–1999 | 1 (1.9) |
| 2000–2999 | 2 (3.8) |
| 3000–3999 | 1 (1.9) |
| ≥ 4000 | 2 (3.8) |
| Sample recruitment locationsa (n = 44) | |
| Emergency shelter | 22 |
| Medical clinic | 18 |
| Meal program | 11 |
| Street or homeless enclaves | 11 |
| Homeless service agencies | 8 |
| Day shelter | 6 |
| Transitional housing | 4 |
| Mental health facility | 2 |
| Substance abuse program | 2 |
| Single room occupancy | 2 |
| Mobile outreach | 2 |
| Hospital | 2 |
| Flophouses or slum apartments | 1 |
| Year of study (n = 55b; average used if spans multiple yrs) | |
| 1980–1989 | 13 (23.6) |
| 1990–1999 | 13 (23.6) |
| 2000–2010 | 24 (43.6) |
| ≥ 2011 | 5 (9.1) |
| US region (n = 53) | |
| Northeast | 19 (35.9) |
| Midwest | 9 (17.0) |
| South | 9 (17.0) |
| West | 10 (18.9) |
| National or multiple regions | 6 (11.3) |
| Population (n = 53) | |
| Urban only | 48 (90.6) |
| Rural only | 1 (1.9) |
| Both | 3 (5.7) |
| Unclear | 1 (1.9) |
| Special target subpopulationa (n = 53) | |
| Women | 5 (9.4) |
| Older adults | 7 (13.2) |
| Veterans | 9 (17.0) |
| Chronically homeless | 2 (3.8) |
May be more than 1 per study.
Used Hahn14 × 3, once for each chronological wave of data presented.
TABLE 4—
Sample and Study Characteristics of Included Studies on Diabetes and Hypertension Prevalence in Homeless Adults in the United States, 1980–2014
| Study and Year | Location | Special Population | Sampling Method | HTN or DM Prevalence | Diagnostic Method | Mean Age, Years | No. of Participants |
| Ballard 200961 | Greensboro, NC | Women | Convenience, shelter | Both | Self-report | 42 | 111 DM; 116 HTN |
| van den Berk-Clark and McGuire 201376 | Los Angeles, CA | Older adults, veterans | Transitional shelter | Both | Self-report | 74 | 59 |
| Bharel et al. 201338 | Boston, MA | Medicaid-insured | Clinic | Both | Provider diagnosis (ICD-9) | 45.5 | 6494 |
| Bowdler 198951 | Richmond, VA | NA | Convenience, medical clinic | HTN | Chart review | 28.7 | 90 |
| Brickner et al. 199264 | New York, NY | NA | Unspecified sampling method, medical clinic | HTN | Measured BP > 140/90 mm Hg | 5436 | |
| Brown et al. 201272 | Boston, MA | Older adults | Probability, shelter, and day shelter | Both | Self-report | 56 | 247 |
| Burt 199979 | Multiple—national | NA | Probability, every type of homeless assistance agency | Both | Self-report | 2938 | |
| Child et al. 199880 | Boston, MA | NA | Census, medical clinic | HTN | Measured BP ≥ 140/90 mm Hg or antihypertensive medicines | 252 | |
| Cohen et al. 198873 | New York, NY | Older adult men | Unspecified sampling method, street, flophouses, slum apartments | Both | Self-report | 62 | 281 |
| Craft-Rosenberg et al. 200077 | Iowa, city unspecified | Women-only rural | Census, shelter | Both | Self-report | 35.5 | 31 |
| Cronley 201381 | Fort Worth, TX | NA | Shelter, homeless service agencies | DM | Self-report | 48.7 | 97 |
| Dellon 199552 | Providence, RI | NA | Convenience, homeless service agency | Both | Self-report | 38 | 102 |
| Drake 199232 | Kansas City, MO | Women | Convenience, shelter | Both | Self-report | 24.2 | 96 |
| Ferenchick 199265 | Lansing, MI | NA | Census, medical clinic | Both | Chart review | 34.3 | 181 |
| Folsom et al. 200253 | San Diego, CA | Mental illness | Census, medical clinic | Both | Chart review | 51.4 | 94 |
| Gallagher et al. 199769 | Los Angeles, CA | NA | Probability, shelters, meal programs, street | HTN | Unspecified physical examination | 38.1 | 363 |
| Garibaldi et al. 200582 | Philadelphia and Pittsburgh, PA | NA | Probability, street, meal programs, shelter, SRO, transitional housing | HTN | Self-report | 531 | |
| Gelberg et al. 199066 | Los Angeles, CA | NA | Census, medical clinic | Both | HTN: self-report or BP ≥ 140/90 mm Hg; DM: self-report | 33.3 | 207 self-report; 186 measured |
| Gelberg et al. 199018 | Los Angeles, CA | NA | Probability, street, shelter, meal program, service agencies | Both | HTN: self-report or BP ≥ 160/90 mm Hg; DM: self-report | 34 | 529 self-report; 505 measured |
| Gibson et al. 200883 | Bedford, MA, and Dallas, TX | Veterans | Convenience, VA homeless programs | Both | Self-report | 46 | 112 |
| Glied et al. 199670 | New York, NY | NA | Probability, shelter | DM | Self-report | 35.5 | 2335 |
| Goldstein et al. 201084 | Multiple—Mid-Atlantic region | NA | Census, homeless veteran service providers, general homeless services | HTN | Self-report | 3595 | |
| Hahn et al. 200614 | San Francisco, CA | NA | Probability, homeless service providers, SROs, shelters, meal programs | Both | Self-report | 42.1 | 1716 |
| Han et al. 200385 | Multiple—East Coast region | NA | Probability, meal programs | Both | Self-report | 41.1 | 941 |
| Kim et al. 200867 | Philadelphia, PA | Men | Unspecified sampling method, shelter | Both | DM: self-report or random glucose ≥ 200; HTN: self-report, medicines, or BP ≥ 140/90 mm Hg | 42.4 | 226 DM; 168 HTNa |
| Kramer and Barker 199674 | Los Angeles, CA | Older adult Native Americans | Convenience, shelters, flop houses, street | Both | Self-report | 53 | 53 |
| Larson 200286 | Nashville, TN | NA | Convenience, day shelter | Both | Self-report | 37.4 | 145 |
| Lebrun-Harris et al. 201387 | Multiple—national | NA | Probability, medical clinic | Both | Self-report | 618 | |
| Lee et al. 200754 | Honolulu, HI | Micronesian | Census, medical clinic | Both | Self-report | 47 | |
| Levitt et al. 200921 | New York, NY | Chronically unsheltered | Census, street | Both | Self-report | 46.2 | 1093 |
| Linton and Shafer 201488 | Phoenix, AZ | Unsheltered, chronically homeless | Street | DM | Self-report | 47 | 260 |
| Luder et al. 199068 | New York, NY | NA | Convenience, day shelter, transitional housing, medical clinic | Both | Self-report | 52.5 | 55 DM; 96 HTN |
| Macnee et al. 199623 | Johnson City, TN | NA | Convenience, medical clinic | Both | Self-report and “screen” not further specified | 58 DM; 131 HTN | |
| Mason et al. 199262 | Utah, city unspecified | Men | Census, shelter | Both | Self-report | 41 | 100 |
| Muirhead et al. 201189 | Chattanooga, TN | NA | Convenience, meal program | Both | Self-report | 43.2 | 95 |
| Notaro 201355 | Urbana-Champaign, IL | NA | Census, medical clinic | DM | Chart review, specified provider diagnosis | 122 | |
| O’Toole et al. 199990 | Multiple—Pennsylvania | NA | Convenience, street, shelter | HTN | Self-report | 194 | |
| O’Toole et al. 201091 | Providence, RI | Veterans | Census, medical clinic | Both | Chart review, specified provider diagnosis | 51.8 | 177 |
| O’Toole et al. 201392 | Providence, RI | Veterans | Medical clinic | Both | Provider diagnosis (ICD-9) | 51.2 | 127 |
| Ritchey et al. 199163 | Birmingham, AL | NA | Probability, shelters, meal programs, street | HTN | Self-report | 33.4 | 100 |
| Ropers and Boyer 198756 | Los Angeles, CA | NA | Probability, shelters, meal programs, street | Both | Self-report | 37.45 | 269 |
| Rowland 199593 | Buffalo, NY | NA | Probability, shelter, meal program, inpatient psych, inpatient rehab, street | Both | Self-report | 31.5 | 413 |
| Savage et al. 200657 | Cincinnati, OH | NA | Census, medical clinic | Both | Self-report | 43 | 110 |
| Schaffer et al. 200094 | St Paul, MN | NA | Convenience, shelter, day shelter | HTN | Self-report | 37 | 101 |
| Schanzer et al. 200771 | New York, NY | Newly homeless | Unspecified sampling method, shelter | Both | Self-report | 36.9 | 351 |
| Tsai et al. 201395 | Multiple—national | NA | Unspecified sampling method | Both | Self-report | 45.5 | 725 |
| Tsai et al. 201396 | National | Veterans | Medical clinic, emergency room | DM | Provider diagnosis (ICD-9) | 51.8 | 64 091 |
| Vijayaraghavan et al. 201278 | New York, NY | Women | Probability, shelter | Both | Self-report | 37.9 | 329 |
| Viron et al. 201497 | Boston, MA | Mental illness | Transitional shelter | Both | Chart review, any source | 43.4 | 60 |
| Washington 200575 | Detroit, MI | Women, older adults, African Americans | Convenience, shelter, warming center, clinic, hospital, mental health clinic, meal program | Both | Self-report | 52.6 | 100 |
| Weinstein et al. 201358 | Philadelphia, PA | Mental illness , Chronically homeless |
Census, multiservice housing first program | Both | Self-report, chart review, best available | 49.7 | 123 |
| Wiersma et al. 201059 | Atlanta, GA | NA | Convenience, shelter | DM | Self-report | 46 | 78 |
| Wojtusik and White 199860 | San Francisco, CA | NA | Convenience, mobile outreach van | Both | Self-report | 41 | 128 |
Notes. BP = blood pressure; DM = diabetes mellitus; HTN = hypertension; ICD-9 = International Classification of Diseases, Ninth Revision; NA = not applicable; SRO = single-room occupancy; VA = Veterans Affairs.
n = 226 for reported DM and 168 for reported HTN, but n = 286 for measured DM and 287 for measured HTN.
Participant Characteristics
Participant characteristics are detailed in Table 5. The average age was 43.3 years (SD = 9.0), and 69% of the sample was male. However, 6 studies were predominantly female. Forty percent of study participants were White, and 47% were African American. Forty-two percent could be classified as literally homeless. Twenty percent of all study participants were employed, and 58% had health insurance. Forty-nine percent of homeless in the included studies were veterans.
TABLE 5—
Demographic Characteristics of Included Study Participants in Meta-analysis of Diabetes and Hypertension Prevalence in Homeless Adults in the United States, 1980–2014
| Sample Characteristic (No. of Studies Reporting) | Number (%) or Mean % ±SD |
| % of sample malea (n = 53) | |
| 0%–19.9% | 5 (9.4) |
| 20%–39.9% | 1 (1.9) |
| 40%–59.9% | 6 (11.3) |
| 60%–79.9% | 22 (41.5) |
| 80%–100% | 19 (35.9) |
| Age, yb (n = 45) | 43.3 ±9.0 |
| Age, yc (n = 39) | 41.1 ±6.7 |
| Homeless category (n = 53) | |
| Literally homelessd | 22 (41.5) |
| Other | 31 (58.5) |
| Chronically homelessa (n = 14) | 0.44 ±0.26 |
| Race/ethnicitya,e | |
| White (n = 44) | 0.40 ±0.23 |
| African American (n = 39) | 0.47 ±0.24 |
| Other (n = 36) | 0.20 ±0.22 |
| Employed (n = 21) | 0.20 ±0.14 |
| Veterans (n = 18) | 0.49 ±0.34 |
| Have health insurance (n = 26) | 0.58 ±0.28 |
Used Hahn14 × 3, once for each chronologic wave of data presented.
Includes studies targeting older adults.
Excludes studies targeting older adults.
Individuals with no stable residence living either in a temporary shelter or unsheltered location not meant for habitation (e.g., the street, a subway station, or a parked car).
Does not sum to 100% because all studies did not include data for each race.
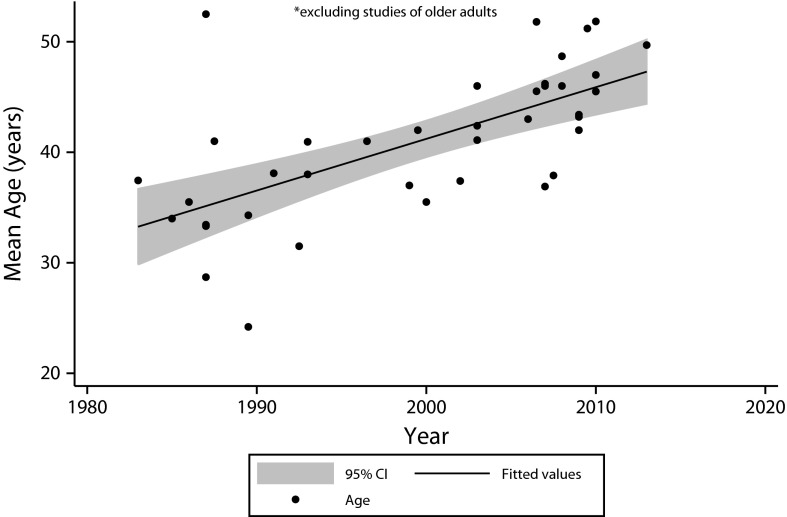
When we plotted the mean ages of the samples over time, after we excluded studies targeting older adults (Figure 2), we observed a statistically significant aging trend (P < .001). Sample mean ages increased from the mid-30s in the 1980s to the mid-40s by 2013.
FIGURE 2—
Trends in homeless adult mean sample age for included studies: United States, 1980–2014.
Note. CI = confidence interval. Studies of older adults were excluded. For trend, P < .001.
Disease Prevalence Findings
The pooled prevalence of self-reported diabetes, based on 39 studies, was 8.0% (95% confidence interval [CI] = 6.8%, 9.2%; Q = 245.93; I 2 = 84.5%). Seven studies assessed diabetes prevalence with physiological measurement, combined for a prevalence of 12.4% (95% CI = 8.9, 15.9%; Q = 180.97; I 2 = 96.7%). The pooled prevalence of self-reported hypertension, based on 43 included studies, was 27.0% (95% CI = 23.8%, 30.2%; Q = 869.35; I 2 = 95.2%). Nine studies that measured blood pressure had a pooled hypertension prevalence of 25.7% (95% CI = 19.5%, 31.9%; Q = 374.16; I 2 = 97.9%).
We made a comparison between measured and reported disease prevalence for studies that included both. There were 4 studies that included both self-reported hypertension and blood pressure measurements for a combined sample size of 990 participants. There was no significant difference in hypertension prevalence between the self-reported diagnoses and diagnoses determined by blood pressure measurement (P = .51). Only 2 studies included both self-reported diabetes and glucose measurements for a combined sample of 284 participants; again, we found no significant difference in diabetes prevalence between self-reported diagnosis and glucose measurement (P = .97).
Rates of other chronic diseases are also reported in Table 6. Rates of chronic respiratory disease were high, and nearly three quarters of the homeless smoked. Rates of mental health diagnoses and drug and alcohol abuse were also high. Studies were too variable in their individual definitions of overall mental illness or substance abuse to present prevalence that was not diagnosis-specific.
TABLE 6—
Behavioral Health and Medical Disease Prevalence in Homeless Adults in the United States, 1980–2014
| Diagnosisa | Prevalence, % (95% CI) | I 2, % | Q (df) |
| Hypertension | 27.0 (23.8, 30.2) | 95.2 | 869.35 (42) |
| Diabetes | 8.0 (6.8, 9.2) | 84.5 | 245.93 (38) |
| Asthma | 14.6 (12.6, 16.6) | 80.5 | 112.70 (22) |
| COPD | 11.0 (6.5, 15.5) | 99.3 | 2452.57 (18) |
| Cirrhosis | 4.4 (2.3, 6.6) | 97.9 | 188.83 (4) |
| Cancer | 4.1 (2.7, 5.6) | 96.1 | 407.56 (16) |
| CVA | 4.3 (2.8, 5.9) | 92.8 | 179.83 (13) |
| Chronic renal disease | 4.9 (3.9, 5.8) | 56.0 | 15.92 (7) |
| Dental disease | 41.7 (24.0, 59.3) | 99.5 | 2648.66 (12) |
| Hepatitis | 13.6 (8.3, 19.0) | 96.6 | 353.96 (12) |
| HIV | 4.6 (3.5, 5.8) | 95.3 | 360.41 (17) |
| Hyperlipidemia | 26.2 (17.6, 34.8) | 90.6 | 64.16 (6) |
| Depression | 40.6 (33.6, 47.5) | 99.3 | 2579.47 (19) |
| Anxiety | 31.8 (24.4, 39.2) | 99.0 | 815.31 (8) |
| PTSD | 16.7 (7.7, 25.7) | 99.7 | 2019.12 (7) |
| Bipolar disorder | 17.9 (11.1, 24.8) | 99.0 | 776.69 (8) |
| Schizophrenia | 18.2 (14.4, 22.1) | 98.1 | 527.04 (10) |
| Substance abuse | |||
| Alcohol abuse | 34.9 (29.2, 40.6) | 99.1 | 2859.60 (25) |
| Drug abuse | 33.1 (25.7, 40.5) | 99.4 | 3024.27 (18) |
| Tobacco use or smoking | 70.8 (62.3, 79.3) | 96.5 | 395.84 (14) |
Notes. CI = confidence interval; COPD = chronic obstructive pulmonary disease; CVA = cerebrovascular accident (stroke); df = degrees of freedom; PTSD = posttraumatic stress disorder.
All diagnoses by self-report.
Risk of Bias
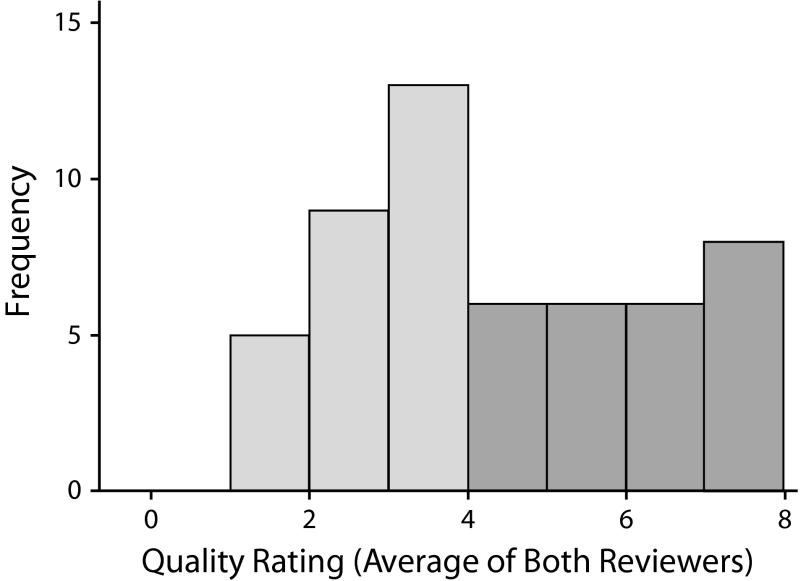
There was high interrater reliability for bias assessment (Spearman’s ρ = 0.83). The distribution of averaged quality scores between the raters is shown in Figure 3 and reflects a wide range of study quality. Study quality was significantly associated with lower diabetes prevalence (P = .03) but not with hypertension prevalence (P = .24).
FIGURE 3—
Distribution of quality ratings of included studies using modified Loney tool.41
Note. We included 53 studies in the analysis.
When we evaluated quality by using each individual quality measure (component analysis), use of appropriate sampling frame and applicability to the general homeless population was associated with lower diabetes prevalence (P = .03 and .01, respectively) and use of a probability sampling method was associated with lower hypertension prevalence (P = .02). See Table 7 for the full component analysis.
TABLE 7—
Quality Assessment Component Effects on Prevalence of Diabetes and Hypertension in Homeless Adults in the United States, 1980–2014
| Reported Prevalence, Item Score (1 vs 0) | Coefficient (SE) | P |
| Diabetes | ||
| Probability sample | -0.038 (0.019) | .054 |
| Sampling frame | -0.042 (0.019) | .033* |
| Sample size | -0.034 (0.023) | .152 |
| Diagnostic methods | 0.023 (0.041) | .573 |
| Consistent methods | -0.019 (0.045) | .679 |
| Response rate | -0.003 (0.029) | .908 |
| Statistical methods | -0.048 (0.028) | .096 |
| Subgroups | -0.020 (0.023) | .407 |
| Applicability | -0.053 (0.020) | .011* |
| Hypertension | ||
| Probability sample | -0.116 (0.046) | .015* |
| Sampling frame | -0.055 (0.049) | .273 |
| Sample size | -0.040 (0.066) | .545 |
| Diagnostic methods | 0.049 (0.099) | .619 |
| Consistent methods | 0.150 (0.081) | .072 |
| Response rate | -0.100 (0.061) | .106 |
| Statistical methods | 0.029 (0.065) | .658 |
| Subgroups | -0.016 (0.055) | .770 |
| Applicability | -0.097 (0.051) | .062 |
*P < .05.
Heterogeneity Analyses
We observed a high degree of heterogeneity in the pooled prevalence rates of diabetes and hypertension. The impacts of study-level characteristics are shown in Table 8. We found mean sample age and year of study to be significantly associated with increasing prevalence of both diabetes and hypertension, and together to account for 18.5% of the variation in diabetes prevalence and 47% of the variation in hypertension prevalence. In addition, having health insurance was associated with increased prevalence of diabetes (P < .001); however, insurance status was not significantly associated with hypertension prevalence (P = .12).
TABLE 8—
Meta-regression of Variables Contributing to Heterogeneity in Hypertension and Diabetes Prevalence in Homeless Adults in the United States, 1980–2014
| Diabetes (Reported) |
Hypertension (Reported) |
|||
| Variable | Coefficient (SE) | P | Coefficient (SE) | P |
| Retrospective versus prospective | 0.046 (0.035) | .193 | -0.059 (0.061) | .34 |
| Region (Ref: East Coast) | ||||
| Midwest | 0.002 (0.040) | .958 | -0.063 (0.069) | .372 |
| South | 0.012 (0.031) | .694 | 0.016 (0.077) | .835 |
| West Coast | -0.014 (0.026) | .592 | -0.004 (0.063) | .955 |
| National | 0.007 (0.040) | .84 | -0.004 (0.080) | .957 |
| Sample selection method (Ref: census) | ||||
| Convenience | 0.010 (0.028) | .732 | 0.044 (0.062) | .48 |
| Probability | -0.027 (0.026) | .321 | 0.010 (0.061) | .877 |
| Unspecified | -0.010 (0.034) | .748 | 0.084 (0.081) | .307 |
| Age, mean of sample | 0.005 (0.001) | <.001 | 0.011 (0.002) | <.001 |
| Year of publicationa | 0.002 (0.000) | <.001 | 0.004 (0.001) | .016 |
| Year of publication, adjusted for age | 0.001 (0.001) | .382 | 0.002 (0.002) | .511 |
| Male, % of sample | -0.024 (0.036) | .507 | 0.055 (0.083) | .511 |
| Race/ethnicity, % of sample | ||||
| African American | -0.035 (0.055) | .533 | 0.012 (0.126) | .924 |
| White | -0.079 (0.056) | .171 | -0.099 (0.120) | .419 |
| Other | 0.154 (0.061) | .018 | 0.037 (0.133) | .782 |
| With health insurance, % of sample | 0.125 (0.029) | <.001 | 0.244 (0.149) | .12 |
| Chronically homeless, % of sample | 0.076 (0.035) | .068 | 0.172 (0.182) | .365 |
| Prevalence of depression | 0.215 (0.079) | .018 | 0.195 (0.234) | .422 |
| Prevalence of alcohol abuse | -0.112 (0.152) | .471 | 0.099 (0.211) | .645 |
| Prevalence of drug abuse | -0.116 (0.070) | .119 | 0.032 (0.202) | .877 |
| Prevalence of tobacco use | 0.097 (0.198) | .633 | 0.147 (0.255) | .576 |
Excluding studies of only older adults.
We did not find prevalence of alcohol abuse (P = .47 and P = .65 for diabetes and hypertension, respectively) and tobacco use (P = .63 and P = .58, respectively) to be significantly associated with change in prevalence of either disease, nor were gender (P = .51 and P = .51, respectively) or African American race (P = .53 and P = .92, respectively). Proportion of the sample with depression was significantly associated with increased prevalence of diabetes (P = .02) but not significantly associated with hypertension prevalence (P = .42). There was a marginally significant association between anxiety and increased prevalence of hypertension (P = .05), but it was not associated with diabetes prevalence (P = .42). Bipolar disorder (P = .84 and P = .91 for diabetes and hypertension, respectively) and schizophrenia rates (P = .97 and P = .87, respectively) did not significantly change the prevalence of either disease.
Comparison With the General Population
The pooled prevalence of hypertension in the general population from 1982 to 2011 was 25.0% (95% CI = 24.0%, 26.1%; Q = 1.6 × 107; df = 22; I 2 = 100%), compared with the homeless sample, which had a prevalence of 27.0% (95% CI = 23.8%, 30.2%; Q = 869.35; df = 42; I 2 = 95.2%). There was no significant difference between the hypertension prevalence in the homeless sample and the general population, with or without adjustment for study year (P = .48 and P = .45, respectively).
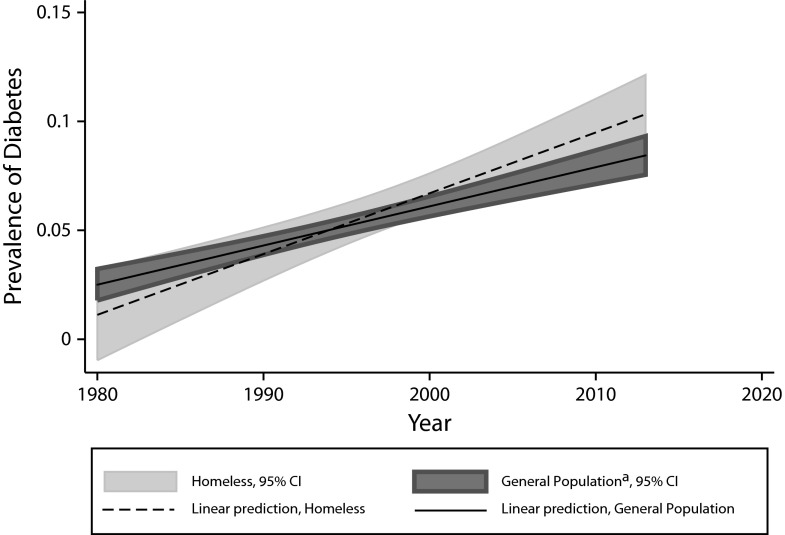
The pooled prevalence of diabetes in the general population from 1980 to 2011 was 5.2% (95% CI = 4.6%, 5.9%; Q = 85.19; df = 22; I 2 = 63.6%), compared with the homeless sample, which had a prevalence of 8.0% (95% CI = 6.8%, 9.2%; Q = 245.93; df = 38; I 2 = 84.5%). We found a significantly higher prevalence of diabetes in the homeless sample than the general population in unadjusted analysis (coefficient = 0.026; 95% CI = 0.008, 0.044; P = .006). However, after we adjusted for study year, this difference was no longer significant (P = .80).
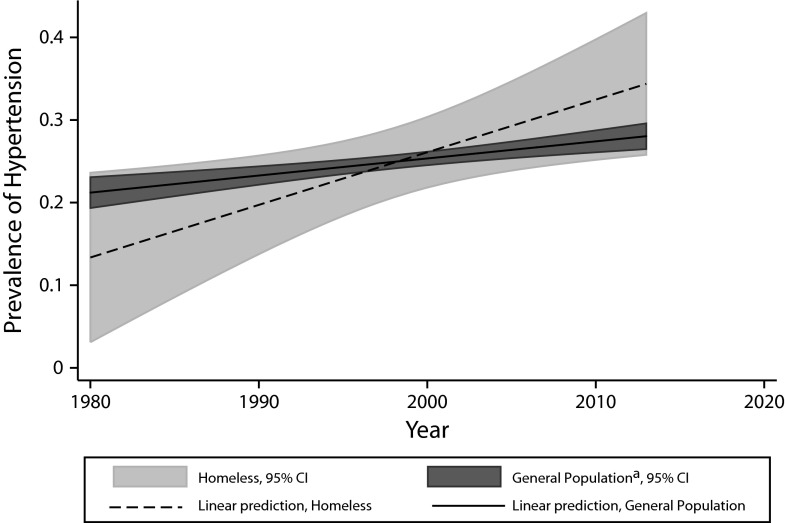
Trends in Disease Prevalence Over Time
The prevalence of hypertension was found to be increasing over time, by study year, in both the homeless data set and in the general population (P < .001 for both groups). Likewise, the prevalence of diabetes was also found to be increasing over time (P = .02, homeless sample, and P < .001, general population).
The estimate provided by meta-regression is an absolute increase in diabetes prevalence of about 0.2% per year and in hypertension of 0.4% per year. However, the rates of increase in disease prevalence between the homeless and general population were not statistically different in either the diabetes or hypertension prevalence analyses (P = .06 and P = .34, respectively; Figures 4 and 5).
FIGURE 4—
Prevalence of self-reported diabetes in homeless and nonhomeless adults in the United States: 1980–2014.
Note. CI = confidence interval.
aData are from the National Health Interview Survey.44
FIGURE 5—
Prevalence of self-reported hypertension in homeless and nonhomeless adults in the United States: 1980–2014.
Note. CI = confidence interval.
Source. Data are from the National Health Interview Survey.
DISCUSSION
Among homeless American adults, approximately 27% have hypertension and 8% have diabetes mellitus. Our sample included an overrepresentation of men and African Americans, mirroring the general homeless population in the United States.30 There is evidence that the prevalence of both diseases is increasing as this population ages. Given the observed trends of increasing prevalence of both hypertension and diabetes in the homeless and general populations over the past 30 years, a simple comparison between prevalence in both groups could not be made without considering the change over time. Our data suggest a widening gap in the rate of increase of diabetes and hypertension between the homeless and general population. This is an expected consequence of the aging of the homeless population relative to the general US population.
We did not find a significant difference in the overall pooled prevalence of diabetes or hypertension between the homeless and general population, nor a statistically significant difference in the change in prevalence over time between the 2 groups. There is inadequate data in this study to evaluate whether there are differences in prevalence at the present time. The power of meta-regression to compare these 2 groups is limited, however, given the heterogeneity of the prevalence estimates in the homeless population. The question of comparing disease prevalence rates between the homeless and general populations would be an important area for further investigation by direct comparison.
We did not find a significant difference in hypertension or diabetes prevalence between estimates from patient self-report and estimates derived from measurement of blood pressure or blood sugar. This finding could have important implications for future research of these diseases in the homeless by decreasing the complexity and expense incurred by taking physiological measurements. However, the limited available data would suggest caution in accepting this finding.
There were few studies that screened for diabetes or hypertension by using physiological measurement, presented data from treating physician diagnosis, or confirmed previous diagnosis with a rigorous methodology. A single random glucose measurement, the method used in the available screening studies, is considered an acceptable method of diabetes screening only if accompanied by classic symptoms of hyperglycemia.96 Because of its low sensitivity of 39% to 55%,98 it is the least preferred method of screening when compared with fasting glucose, oral glucose tolerance testing, or hemoglobin A1C. The studies that used physiological measurement to estimate hypertension prevalence also had limitations that made them less likely to detect a higher prevalence than estimates based on self-report. Those with normal blood pressure measurements who were taking antihypertensive medications were not counted as having hypertension in all of the studies, and 1 study only reported blood pressure measurements with a threshold above 160/90 mm Hg.18 None of the studies measured blood pressure on separate occasions, as recommended in establishing the diagnosis.
In the general population, approximately one third of patients with diabetes and one fifth of people with hypertension are unaware of their diagnosis.29,99 With the numerous challenges faced by the homeless in receiving medical care, it is likely that unawareness may be even higher in this population. This is supported by this study’s finding that those with health insurance, who have less financial barrier to accessing health care, are more likely to self-report a diagnosis of diabetes than those without health insurance. Thus, the reported prevalence of both diseases presented in this analysis is likely to underreport the actual disease prevalence. Determination of the rate of underdiagnosis of these conditions in the homeless population would be a subject for further research. The recent introduction of random A1C for diabetes screening, without requirement of fasting or glucose tolerance testing, helps to simplify diabetes screening in future research in the homeless.
This study adds to the growing body of evidence of the aging of the homeless population. Despite the limitations of using mean sample age as the observation level, we observed a clear trend over the past 30 years. Over this period, homeless adults, as a group, appear to be aging at the rate of almost 6 months per year, similar to the estimates provided by other studies.14,100 One significant advantage of the estimate provided by this project compared with others that have described the aging trend is the systematic review yielded a broad data sample, including different regions of the country, a variety of settings, and multiple homeless subpopulations.
Furthermore, this study begins to explore the impact of the aging trend on the prevalence of chronic diseases. As expected, hypertension and diabetes prevalence have increased over the past 3 decades. Over the next decade, as the homeless population continues to age, this may translate into dramatic increases in cardiovascular disease and diabetic complications. This growing disease burden will have a critical impact not only on affected homeless individuals, but also on safety net primary care providers, hospitals, homeless service programs including medical respite care, Medicaid agencies, and others.
Although not explored in this study, there is likely an increase in rates of other chronic diseases. The relatively high rates of chronic respiratory diseases are similar to rates in other literature,101 and are likely associated with the well-known high rates of smoking among homeless adults.6 The sample participants also had high rates of mental health and substance use diagnoses. Taken together, these findings are consistent with previous research identifying causes of (or determinants of) premature mortality of the homeless population.
This systematic review demonstrates a broad literature base investigating chronic diseases experienced by homeless adults, including some large and methodologically rigorous studies. The included studies targeted a wide variety of homeless subpopulations, including young women raising children, single men, the chronically homeless, older homeless adults, clinic patients, unsheltered homeless, and several racial or ethnic subgroups. The overall sample has excellent applicability to the general homeless population.
Limitations
Participants in the meta-analysis sample may be somewhat older than the general homeless population, as captured in the 2012 Annual Homeless Assessment Report (Table 9). This difference lies in the relative proportions of adults aged 30 years and younger versus those aged between 31 and 50 years in the meta-analysis sample. As such, it is not affected by the inclusion of 5 studies targeting older adults. The proportion of the homeless population aged 51 years and older in the meta-analysis sample is actually slightly lower than in the general population.
TABLE 9—
Age Distribution of Participants From Included Studies Compared With General Population Sheltered Adults: United States, 1980-2014
| Age, Years | Meta-analysis Sample,a % | 2012 Sheltered Homeless Population (Adults Only),16 % |
| 18–30 | 4.4 | 30.4 |
| 31–50 | 73.3 | 45.3 |
| 51–61 | 17.8 | 20.2 |
| ≥62 | 4.4 | 4.1 |
Percentages listed are of sample mean ages.
It is possible that the 16 clinic-based studies included skewed the sample toward middle-aged adults, who are more likely to have medical conditions that cause them to seek care. This may result in higher pooled prevalence rates of diabetes and hypertension than in the true homeless population. Of note, the true age distribution of the meta-analysis sample is only estimated by the distribution of sample mean age given in Table 9.
The quality of the pooled estimate is constrained by the quality of the studies included in the analysis. Likewise, certain variables that would have been useful for heterogeneity analysis, such as rates of obesity, were unavailable. The relatively higher number of young adults relative to middle-aged adults and higher prevalence of chronic homelessness should be considered before one generalizes these results to the entire homeless adult population; furthermore, because of the heterogeneity of the homeless population, generalizability to all subgroups is difficult. The majority of available studies used self-reported data. Finally, all included studies used a cross-sectional design; causality between homelessness and having a diagnosis of hypertension or diabetes cannot be inferred.
Important findings of this study, namely that hypertension and diabetes rates in the aging homeless population are increasing, are particularly salient in light of recent changes in our health care system. Through the Affordable Care Act and Medicaid expansion in 28 states, including Washington, DC, homeless individuals are experiencing increased access to health insurance. A recent study comparing health service utilization in chronically homeless persons with and without health insurance100 has demonstrated increased use of outpatient medical services and preventive care among homeless individuals with insurance. Furthermore, a significant randomized controlled study assessing the impact of receiving Medicaid on the uninsured found that newly obtaining Medicaid is associated with receiving a new diagnosis of diabetes.102 Major efforts will be needed to encourage newly eligible homeless adults to enroll in Medicaid, to increase availability of primary care providers for this population, to encourage clinicians to screen for these and other conditions in newly insured homeless, and to continue efforts to address the many other nonfinancial barriers to ongoing chronic disease management for the homeless.
Conclusions
In this systematic review and meta-analysis of the prevalence of hypertension and diabetes in homeless adults, we found that both conditions have had increasing prevalence over the past 30 years. These differences are, to a large extent, attributable to the aging of the homeless population. This study builds upon the existing literature regarding this aging trend by drawing from a broad sample and directly linking aging trends to chronic disease rates. With heterogeneity analyses, we identified several other factors that contribute to variations in estimated diabetes prevalence, including insurance status and depression.
Although the homeless population today has significant unmet health needs, which contribute to devastatingly premature morbidity and mortality, this study suggests that over the next 2 decades there will be an increasing burden of cardiovascular disease in this population. Increased access to Medicaid will help reduce financial barriers to care, but the many remaining barriers will need attention. Preventive measures such as improving nutritional content in meal programs, increasing the availability of treatment of alcohol abuse, and encouraging physical activity may help decrease the incidence of new hypertension and diabetes. Efforts are urgently needed to increase access to care for the homeless individuals who already have diabetes or hypertension, and to prevent future disease.
Acknowledgments
This project was supported by an Institutional National Research Service Award (US Health Resources and Services Administration, T32-HP10030) and by the National Center for Advancing Translational Sciences (National Institutes of Health, 8UL1TR000055).
We acknowledge and are grateful for the expertise and contribution of Ruta Brazauskas, PhD, to data interpretation.
Note. The article’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Human Participant Protection
This study, which used only published group-level data, did not constitute human participants research and did not undergo review by an institutional review board.
References
- 1.Cortes A, Henry M, de la Cruz RJ, Brown S. The 2012 point-in-time estimates of homelessness. US Department of Housing and Urban Development, Office of Community Planning and Development. 2012. Available at: https://www.onecpd.info/resources/documents/2012AHAR_PITestimates.pdf. Accessed May 2, 2014.
- 2.Burt MR, Aron LY, Valente J. Washington, DC: Urban Institute; 2001. How many homeless people are there? Helping America’s homeless: emergency shelter or affordable housing? pp. 23–54. [Google Scholar]
- 3.Link BG, Susser E, Stueve A, Phelan J, Moore RE, Struening E. Lifetime and five-year prevalence of homelessness in the United States. Am J Public Health. 1994;84(12):1907–1912. doi: 10.2105/ajph.84.12.1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McKinney–Vento Homeless Education Assistance Improvements Act of 2001. USC 42 §725. [PMC free article] [PubMed]
- 5.Bonin E, Brehove T, Carlson C . Adapting Your Practice: General Recommendations for the Care of Homeless Patients. Nashville, TN: Health Care for the Homeless Clinicians’ Network, National Health Care for the Homeless Council Inc; 2010. p. 51. [Google Scholar]
- 6.Baggett TP, Hwang SW, O’Connell JJ et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173(3):189–195. doi: 10.1001/jamainternmed.2013.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hwang SW, Orav EJ, O’Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997;126(8):625–628. doi: 10.7326/0003-4819-126-8-199704150-00007. [DOI] [PubMed] [Google Scholar]
- 8.Barrow SM, Herman D, Cordova P, Struening E. Mortality among homeless shelter residents in New York City. J Public Health (Bangkok) 1999;89(4):529–534. doi: 10.2105/ajph.89.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hibbs JR, Benner L, Klugman L et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304–309. doi: 10.1056/NEJM199408043310506. [DOI] [PubMed] [Google Scholar]
- 10.Morrison DS. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol. 2009;38(3):877–883. doi: 10.1093/ije/dyp160. [DOI] [PubMed] [Google Scholar]
- 11.O’Connell JJ. Premature Mortality in Homeless Populations: A Review of the Literature. Nashville, TN: National Health Care for the Homeless Council Inc; 2005. p. 19. [Google Scholar]
- 12.Wood D, editor. Delivering Health Care to Homeless Persons. The Diagnosis and Management of Medical and Mental Health Conditions. New York, NY: Springer Publishing; 1992. [Google Scholar]
- 13.Stark LR. Homelessness: A Prevention-Oriented Approach. Baltimore, MD: Johns Hopkins University Press; 1992. pp. 151–164. [Google Scholar]
- 14.Hahn JA, Kushel MB, Bangsberg DR, Riley E, Moss AR. Brief report: the aging of the homeless population: fourteen-year trends in San Francisco. J Gen Intern Med. 2006;21(7):775–778. doi: 10.1111/j.1525-1497.2006.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Culhane DP, Metraux S, Byrne T, Stino M, Bainbridge J. The age structure of contemporary homelessness: evidence and implications for public policy. Analyses Soc Issues Public Policy. 2013;13(1):228–244. [Google Scholar]
- 16.Israel N, Toro PA, Ouellette N. Changes in the composition of the homeless population: 1992–2002. Am J Community Psychol. 2010;46(1-2):49–59. doi: 10.1007/s10464-010-9326-9. [DOI] [PubMed] [Google Scholar]
- 17.Solari CD, Cortes A, Brown S. The 2012 Annual Homeless Assessment Report (AHAR) to Congress. Washington, DC: US Department of Housing and Urban Development; 2012. [Google Scholar]
- 18.Gelberg L, Linn L, Mayer-Oakes S. Differences in health status between older and younger homeless adults. J Am Geriatr Soc. 1990;38(11):1220–1229. doi: 10.1111/j.1532-5415.1990.tb01503.x. [DOI] [PubMed] [Google Scholar]
- 19.Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW. Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey. Open Med. 2011;5(2):e94–e103. [PMC free article] [PubMed] [Google Scholar]
- 20.Gelberg L, Linn L. Assessing the physical health of homeless adults [erratum appears in JAMA 1989;262(22):3132] JAMA. 1989;262(14):1973–1979. [PubMed] [Google Scholar]
- 21.Levitt AJ, Culhane D, DeGenova J, O’Quinn P, Bainbridge J. Health and social characteristics of homeless adults in Manhattan who were chronically or not chronically unsheltered. Psychiatr Serv. 2009;60(7):978–981. doi: 10.1176/ps.2009.60.7.978. [DOI] [PubMed] [Google Scholar]
- 22.Zlotnick C, Zerger S. Survey findings on characteristics and health status of clients treated by the federally funded (US) Health Care for the Homeless Programs. Health Soc Care Community. 2009;17(1):18–26. doi: 10.1111/j.1365-2524.2008.00793.x. [DOI] [PubMed] [Google Scholar]
- 23.Macnee CL, Hemphill JC, Letran J. Screening clinics for the homeless: evaluating outcomes. J Community Health Nurs. 1996;13(3):167–177. doi: 10.1207/s15327655jchn1303_4. [DOI] [PubMed] [Google Scholar]
- 24.Tu K, Chen Z, Lipscombe LL. Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ. 2008;178(11):1429–1435. doi: 10.1503/cmaj.071283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 26.Burt VL, Whelton P, Roccella EJ et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25(3):305–313. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 27.Turnbull F, Neal B, Ninomiya T et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336(7653):1121–1123. doi: 10.1136/bmj.39548.738368.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Increasing prevalence of diagnosed diabetes—United States and Puerto Rico, 1995–2010. MMWR Morb Mortal Wkly Rep. 2012;61(45):918–921. [PubMed] [Google Scholar]
- 29. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011.
- 30.Cortes A, Leopold J, Rothschild L, Buron L, Khadduri J, Culhane DP. The 2010 Annual Homeless Assessment Report to Congress. 2011. Available at: http://works.bepress.com/dennis_culhane/105. Accessed May 2, 2014.
- 31.Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46:1115–1128. doi: 10.1037//0003-066x.46.11.1115. [DOI] [PubMed] [Google Scholar]
- 32.Drake MA. The nutritional status and dietary adequacy of single homeless women and their children in shelters. Public Health Rep. 1992;107(3):312–319. [PMC free article] [PubMed] [Google Scholar]
- 33.Dinour LM, Bergen D, Yeh M-C. The food insecurity–obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107(11):1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 34.Tsai J, Rosenheck RA. Obesity among chronically homeless adults: is it a problem? Public Health Rep. 2013;128(1):29–36. doi: 10.1177/003335491312800105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805–821. doi: 10.1097/00005650-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 36.Martell JV, Seitz RS, Harada JK, Kobayashi J, Sasaki VK, Wong C. Hospitalization in an urban homeless population: the Honolulu Urban Homeless Project. Ann Intern Med. 1992;116(4):299–303. doi: 10.7326/0003-4819-116-4-299. [DOI] [PubMed] [Google Scholar]
- 37.Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41(4):547–556. doi: 10.1016/0277-9536(94)00364-y. [DOI] [PubMed] [Google Scholar]
- 38.Bharel M, Lin WC, Zhang J, O'Connell E, Taube R, Clark RE. Health care utilization patterns of homeless individuals in Boston: preparing for Medicaid expansion under the Affordable Care Act. Am J Public Health. 2013;103(suppl 2):S311–S317. doi: 10.2105/AJPH.2013.301421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740. doi: 10.1056/NEJM199806113382406. [DOI] [PubMed] [Google Scholar]
- 40.Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 41.Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can. 1998;19(4):170–176. [PubMed] [Google Scholar]
- 42.Woodbury MG, Houghton PE. Prevalence of pressure ulcers in Canadian healthcare settings. Ostomy Wound Manage. 2004;50(10):22–24, 26, 28, 30, 32, 34, 36–38. [PubMed] [Google Scholar]
- 43.Colton T. Statistics in Medicine. Boston, MA: Little, Brown and Company; 1974. p. 211. [Google Scholar]
- 44.Centers for Disease Control and Prevention. Crude and age-adjusted percentage of civilian, noninstitutionalized adults with diagnosed diabetes, United States, 1980–2011. Available at: http://www.cdc.gov/diabetes/statistics/prev/national/figageadult.htm. Accessed May 2, 2014.
- 45. Integrated Health Interview Series. Available at: https://www.ihis.us/ihis/sda.shtml. Accessed December 23, 2013.
- 46.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 47.Galbraith RF. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988;7(8):889–894. doi: 10.1002/sim.4780070807. [DOI] [PubMed] [Google Scholar]
- 48.Higgins JPT, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23(11):1663–1682. doi: 10.1002/sim.1752. [DOI] [PubMed] [Google Scholar]
- 49.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.A Wilcoxon-type test for trend. Stat Med. 1985;4(4):543–547. doi: 10.1002/sim.4780040416. [DOI] [PubMed] [Google Scholar]
- 51.Bowdler JE. Health problems of the homeless in America. Nurse Pract. 1989;14(7):44–51. [PubMed] [Google Scholar]
- 52.Dellon ES. The health status of the Providence-area homeless population. R I Med. 1995;78(10):278–283. [PubMed] [Google Scholar]
- 53.Folsom DP, McCahill M, Bartels SJ, Lindamer LA, Ganiats TG, Jeste DV. Medical comorbidity and receipt of medical care by older homeless people with schizophrenia or depression. Psychiatr Serv. 2002;53(11):1456–1460. doi: 10.1176/appi.ps.53.11.1456. [DOI] [PubMed] [Google Scholar]
- 54.Lee DF, Lindshield CJ, Kuribayashi T, Kleinschmidt CK, Lee EK, Omori JS. Health problems of Micronesian patients at a student-run free homeless clinic. Pac Health Dialog. 2007;14(1):254–262. [PubMed] [Google Scholar]
- 55.Notaro SJ, Khan M, Kim C, Nasaruddin M, Desai K. Analysis of the health status of the homeless clients utilizing a free clinic. J Community Health. 2013;38(1):172–177. doi: 10.1007/s10900-012-9598-0. [DOI] [PubMed] [Google Scholar]
- 56.Ropers RH, Boyer R. Perceived health status among the new urban homeless. Soc Sci Med. 1987;24(8):669–678. doi: 10.1016/0277-9536(87)90310-8. [DOI] [PubMed] [Google Scholar]
- 57.Savage CL, Lindsell CJ, Gillespie GL, Dempsey A, Lee RJ, Corbin A. Health care needs of homeless adults at a nurse-managed clinic. J Community Health Nurs. 2006;23(4):225–234. doi: 10.1207/s15327655jchn2304_3. [DOI] [PubMed] [Google Scholar]
- 58.Weinstein L, LaNoue M, Collins E, Henwood B, Drake R. Health care integration for formerly homeless people with serious mental illness. J Dual Diagn. 2013;9:72–77. [Google Scholar]
- 59.Wiersma P, Epperson S, Terp S et al. Episodic illness, chronic disease, and health care use among homeless persons in Metropolitan Atlanta, Georgia, 2007. South Med J. 2010;103(1):18–24. doi: 10.1097/SMJ.0b013e3181c46f79. [DOI] [PubMed] [Google Scholar]
- 60.Wojtusik L, White MC. Health status, needs, and health care barriers among the homeless. J Health Care Poor Underserved. 1998;9(2):140–152. doi: 10.1353/hpu.2010.0379. [DOI] [PubMed] [Google Scholar]
- 61. Ballard FA. Homeless Sheltered Women’s Health Promotion Behaviors [dissertation]. Greensboro, NC: University of North Carolina Greensboro; 2009.
- 62.Mason DJ, Jensen M, Boland DL. Health behaviors and health risks among homeless males in Utah. 1992. Available at: http://psycnet.apa.org/psycinfo/1993-18966-001. Accessed May 2, 2014. [DOI] [PubMed]
- 63.Ritchey FJ, La Gory M, Mullis J. Gender differences in health risks and physical symptoms among the homeless. J Health Soc Behav. 1991;32(1):33–48. [PubMed] [Google Scholar]
- 64.Brickner P, McAdam J, Vicic W, Doherty P. Strategies for the delivery of medical care: focus on tuberculosis and hypertension. In: Robertson MJ, Greenblatt M, editors. Homelessness: A National Perspective. New York NY: Plenum Press; 1992. pp. 165–174. [Google Scholar]
- 65.Ferenchick GS. The medical problems of homeless clinic patients: a comparative study. J Gen Intern Med. 1992;7(3):294–297. doi: 10.1007/BF02598086. [DOI] [PubMed] [Google Scholar]
- 66.Gelberg L, Linn LS, Usatine RP, Smith MH. Health, homelessness, and poverty: a study of clinic users. Arch Intern Med. 1990;150(11):2325–2330. [PubMed] [Google Scholar]
- 67.Kim DH, Daskalakis C, Plumb JD et al. Modifiable cardiovascular risk factors among individuals in low socioeconomic communities and homeless shelters. Fam Community Health. 2008;31(4):269–280. doi: 10.1097/01.FCH.0000336090.37280.2e. [DOI] [PubMed] [Google Scholar]
- 68.Luder E, Ceysens-Okada E, Koren-Roth A, Martinez-Weber C. Health and nutrition survey in a group of urban homeless adults. J Am Diet Assoc. 1990;90(10):1387–1392. [PubMed] [Google Scholar]
- 69.Gallagher TC, Andersen RM, Koegel P, Gelberg L. Determinants of regular source of care among homeless adults in Los Angeles. Med Care. 1997;35(8):814–830. doi: 10.1097/00005650-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 70.Glied S, Hoven C, Moore R, Garrett AB. Medicaid and service use among homeless adults. 1996. Available at: http://www.nber.org/papers/w5834. Accessed May 2, 2014. [PubMed]
- 71.Schanzer B, Dominguez B, Shrout PE, Caton CL. Homelessness, health status, and health care use. Am J Public Health. 2007;97(3):464–469. doi: 10.2105/AJPH.2005.076190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. J Gen Intern Med. 2012;27(1):16–22. doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cohen C, Teresi J, Holmes D. The physical well-being of old homeless men. J Gerontol. 1988;43(4):S121–S128. doi: 10.1093/geronj/43.4.s121. [DOI] [PubMed] [Google Scholar]
- 74.Kramer J, Barker J. Homelessness among older American Indians, Los Angeles, 1987–1989. Hum Organ. 1996;55:396–408. [Google Scholar]
- 75.Washington OG. Identification and characteristics of older homeless African American women. Issues Ment Health Nurs. 2005;26(2):117–136. doi: 10.1080/01612840590901572. [DOI] [PubMed] [Google Scholar]
- 76.van den Berk-Clark C, McGuire J. Elderly homeless veterans in Los Angeles: chronicity and precipitants of homelessness. Am J Public Health. 2013;103(suppl 2):S232–S238. doi: 10.2105/AJPH.2013.301309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Craft-Rosenberg M, Powell SR, Culp K. Health status and resources of rural homeless women and children. West J Nurs Res. 2000;22(8):863–878. doi: 10.1177/01939450022044845. [DOI] [PubMed] [Google Scholar]
- 78.Vijayaraghavan M, Tochterman A, Hsu E, Johnson K, Marcus S, Caton CL. Health, access to health care, and health care use among homeless women with a history of intimate partner violence. J Community Health. 2012;37(5):1032–1039. doi: 10.1007/s10900-011-9527-7. [DOI] [PubMed] [Google Scholar]
- 79.Burt MR. Homelessness: Programs and the People They Serve. Darby, PA: Diane Publishing; 1999. [Google Scholar]
- 80.Child J, Bierer M, Eagle K. Unexpected factors predict control of hypertension in a hospital-based homeless clinic. Mt Sinai J Med. 1998;65(4):304–307. [PubMed] [Google Scholar]
- 81.Cronley CM. Do official hospitalization records predict self-reported medical vulnerablity? A test of the post-dictive validity of the vulnerability index. Abstract presented at: Society for Social Work and Research 17th Annual Conference: Social Work for a Just Society: Making Visible the Stakes and Stakeholders; January 18, 2013; San Diego, CA. Available at: https://sswr.confex.com/sswr/2013/webprogram/Paper17760.html. Accessed May 2, 2014.
- 82.Garibaldi B, Conde-Martel A, O’Toole TP. Self-reported comorbidities, perceived needs, and sources for usual care for older and younger homeless adults. J Gen Intern Med. 2005;20(8):726–730. doi: 10.1111/j.1525-1497.2005.0142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gibson G, Reifenstahl EF, Wehler CJ et al. Dental treatment improves self-rated oral health in homeless veterans—a brief communication. J Public Health Dent. 2008;68(2):111–115. doi: 10.1111/j.1752-7325.2007.00081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Goldstein G, Luther JF, Haas GL, Appelt CJ, Gordon AJ. Factor structure and risk factors for the health status of homeless veterans. Psychiatr Q. 2010;81(4):311–323. doi: 10.1007/s11126-010-9140-4. [DOI] [PubMed] [Google Scholar]
- 85.Han B, Wells BL, Taylor AM. Use of the Health Care for the Homeless Program services and other health care services by homeless adults. J Health Care Poor Underserved. 2003;14(1):87–99. [PubMed] [Google Scholar]
- 86.Larson CO. Use of the SF-12 instrument for measuring the health of homeless persons. Health Serv Res. 2002;37(3):733–750. doi: 10.1111/1475-6773.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lebrun-Harris LA, Baggett TP, Jenkins DM et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013;48(3):992–1017. doi: 10.1111/1475-6773.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Linton KF, Shafer MS. Factors associated with the health service utilization of unsheltered, chronically homeless adults. Social Work Public Health. 2014:2973–2980. doi: 10.1080/19371918.2011.619934. [DOI] [PubMed] [Google Scholar]
- 89.Muirhead L, Roberson AJ, Secrest J. Utilization of foot care services among homeless adults: implications for advanced practice nurses. J Am Acad Nurse Pract. 2011;23(4):209–215. doi: 10.1111/j.1745-7599.2011.00598.x. [DOI] [PubMed] [Google Scholar]
- 90.O’Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Utilization of health care services among subgroups of urban homeless and housed poor. J Health Polit Policy Law. 1999;24(1):91–114. doi: 10.1215/03616878-24-1-91. [DOI] [PubMed] [Google Scholar]
- 91.O’Toole TP, Buckel L, Bourgault C et al. Applying the chronic care model to homeless veterans: effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health. 2010;100(12):2493–2499. doi: 10.2105/AJPH.2009.179416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.O’Toole TP, Bourgault C, Johnson EE et al. New to care: demands on a health system when homeless veterans are enrolled in a medical home model. Am J Public Health. 2013;103(suppl 2):S374–S379. doi: 10.2105/AJPH.2013.301632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Rowland LL. Predicting Longitudinal Health Outcomes in a Probability Sample of Homeless Adults [dissertation]. Detroit, MI: Wayne State University; 1995.
- 94.Schaffer MA, Mather S, Gustafson V. Service learning: a strategy for conducting a health needs assessment of the homeless. J Health Care Poor Underserved. 2000;11(4):385–399. doi: 10.1353/hpu.2010.0746. [DOI] [PubMed] [Google Scholar]
- 95.Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225–S231. doi: 10.2105/AJPH.2013.301307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Viron M, Bello I, Freudenreich O, Shtasel D. Characteristics of homeless adults with serious mental illness served by a state mental health transitional shelter. Community Ment Health J. 2014;50(5):560–565. doi: 10.1007/s10597-013-9607-5. [DOI] [PubMed] [Google Scholar]
- 98.Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab. 2008;93(7):2447–2453. doi: 10.1210/jc.2007-2174. [DOI] [PubMed] [Google Scholar]
- 99.Roger VL, Go AS, Lloyd-Jones DM et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tsai J, Rosenheck RA, Culhane DP, Artiga S. Medicaid expansion: chronically homeless adults will need targeted enrollment and access to a broad range of services. Health Aff (Millwood) 2013;32(9):1552–1559. doi: 10.1377/hlthaff.2013.0228. [DOI] [PubMed] [Google Scholar]
- 101.Snyder LD, Eisner MD. Obstructive lung disease among the urban homeless. Chest. 2004;125(5):1719–1725. doi: 10.1378/chest.125.5.1719. [DOI] [PubMed] [Google Scholar]
- 102.Baicker K, Taubman SL, Allen HL et al. The Oregon Experiment—effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]