Abstract
Background
Impulsivity is a complex trait often studied in substance abuse and overeating disorders, but the exact nature of impulsivity traits and their contribution to these disorders are still debated. Thus, understanding how to measure impulsivity is essential for comprehending addictive behaviors.
Objectives
Identify unique impulsivity traits specific to substance use and overeating.
Methods
Impulsive Sensation Seeking (ImpSS) and Barratt’s Impulsivity scales (BIS) Scales were analyzed with a non-parametric factor analytic technique (discriminant correspondence analysis) to identify group-specific traits on 297 individuals from five groups: Marijuana (n = 88), Nicotine (n = 82), Overeaters (n = 27), Marijuauna + Nicotine (n = 63), and Controls (n = 37).
Results
A significant overall factor structure revealed three components of impulsivity that explained respectively 50.19% (pperm<0.0005), 24.18% (pperm<0.0005), and 15.98% (pperm<0.0005) of the variance. All groups were significantly different from one another. When analyzed together, the BIS and ImpSS produce a multi-factorial structure that identified the impulsivity traits specific to these groups. The group specific traits are (1) Control: low impulse, avoids thrill-seeking behaviors; (2) Marijuana: seeks mild sensation, is focused and attentive; (3) Marijuana + Nicotine: pursues thrill-seeking, lacks focus and attention; (4) Nicotine: lacks focus and planning; (5) Overeating: lacks focus, but plans (short and long term).
Conclusions
Our results reveal impulsivity traits specific to each group. This may provide better criteria to define spectrums and trajectories – instead of categories – of symptoms for substance use and eating disorders. Defining symptomatic spectrums could be an important step forward in diagnostic strategies.
Keywords: Impulsivity, overeating, psychometrics, statistics, substance use
Introduction
Impulsivity is a complex trait often studied in personality disorders (1), and self-regulatory failures (2) such as substance use and overeating disorders (3). In substance use and overeating, high levels of impulsivity – a risk factor for addiction and dependence (4) – may be associated with an increase in drug (5) and alcohol use (6) as well as pathologic substance abuse (7), could impact treatment strategies (8,9), and could reveal subtypes of binge eating (10). Thus understanding impulsivity and its measurement is essential for understanding addictive behaviors (11).
“Impulsivity”, however, is a multifaceted and heterogeneous concept that includes aspects of disinhibition, inattention, sensation seeking, and deficits in decision-making (12). Further, these aspects exist under two broad categories of impulsivity: state impulsivity (i.e. “in the moment”) and trait impulsivity (i.e. the inherent characteristics of a person). While both types are associated with substance use (13), trait impulsivity is especially important because it contributes to the underlying risk for substance use. Trait impulsivity is mostly measured using self-assessment scales: often with the Impulsive Sensation Seeking (ImpSS) scale (14–17) and Barratt’s Impulsivity Scale [BIS; (18,19)].
Using the ImpSS or BIS, numerous studies have shown that “high impulsivity” exists in substance abuse groups – such as nicotine users (20), cocaine users (21), and drunk drivers (22) – and that impulsivity is associated with increased craving (23) and consumption (24) of food. Importantly, impulsivity traits could impact treatment strategies for substance use disorders (8,25). In practice, both the ImpSS and BIS are generally used as unidimensional indices with higher scores interpreted as “more impulsivity”. However, if impulsivity is multidimensional, the same score obtained by different individuals can reflect different realities and would, therefore, obscure unique impulsivity traits.
The traditional structure of the BIS (18,19) has been challenged (26) and recently revised to comprise two factors (26) and then again reframed as one factor (27) for the general population. Furthermore, recent work has shown that there are differing aspects of impulsivity in typically impulsive populations (28), illicit substance users (29), alcohol use disorders (30), and cigarette smoking (31). In sum, there appears to be diverse sets of impulsivity traits in substance use populations, and so there is a growing interest in parsing impulsivity traits because the exact contribution (32) and dimensionality (33,34) of impulsivity traits – especially with respect to addictive behaviors – is under intense debate.
To better understand the factor structure of trait impulsivity, we analyzed common measures of trait impulsivity in order to evaluate if specific multidimensional patterns of responses could characterize specific substance use and overeating groups. We measured impulsivity using ImpSS and BIS from five groups of participants: (i) a non-using Control group, (ii) Marijuana users, (iii) Nicotine users, (iv) individuals with high body-mass index (BMI) or binge-eating symptoms (henceforth referred to as Overeaters), and (v) Marijuana + Nicotine users. We used discriminant correspondence analysis [DiCA, (35)] – a factor analytic technique – to find the distinct patterns of impulsive traits that characterize these five groups. DiCA is a discriminant analysis extension of correspondence analysis (36) and multiple correspondence analysis (37) and both techniques have been used extensively in the analysis of self-assessments and surveys [e.g. memory (38), stress (39), schizophrenia (40), and opioid abuse (41)]. More importantly, recent work in autism and schizophrenia research (using DiCA) has shown that similar summary scores on self-assessments reflected unique patterns of traits for different populations (42). Thus, in this study, we expected to find a new factor structure of impulsivity where each of our groups were defined by distinct impulsivity traits.
Methods
This study was approved by the University of New Mexico and The University of Texas at Dallas Institutional Review Boards.
Participants
Participants were recruited from the general community in Albuquerque (NM) and took part in a larger set of studies to determine markers of addiction. Demographics are listed in Table 1. Some participants have been described in previous reports – Marijuana (43,44), Control (44), Nicotine (45), and Overeaters (46) – but this study has not been presented elsewhere. Substance use groups were recruited from three separate studies on: (i) marijuana use (Marijuana participants), (ii) overeating (Overeating participants), and (iii) nicotine use (Nicotine and Control participants). Marijuana group participants self-reported current marijuana use of at least four occasions per week over the previous 6 months (positive use verified via urinalysis). Eighty-two (out of 151) Marijuana study participants met criteria for current marijuana dependence [via the Structured Clinical Interview for DSM-IV-TR, Research Version (47)]. Nicotine group participants self-reported current nicotine use of at least 10 cigarettes per day (positive use verified via breath CO monitor). The Nicotine group had moderate-to-high nicotine dependence as evaluated by the Fagerström’s Test for Nicotine Dependence [FTND (48); M = 6.76, SD = 1.59]. Overeating group participants had a BMI ≥25 [(49); M = 32.28, SD = 7.93] or a minimum score of 18 on the Binge Eating Scale [BES (50); M = 21.00, SD = 10.35]. Non-using controls did not report any current regular use of illicit substances (including marijuana) in the past 6 months. Participants were excluded from the studies if they had (i) past or present diagnosis of a neurological disorder, (ii) psychosis or other substance use disorder besides their primary substance use disorder (assessed via the Psychotic Symptoms and Substance Use Disorders modules of the SCID), or (iii) currently taking prescribed psychoactive medication.
Table 1.
Demographics of the groups.
| Gender |
Age Mean (SD) |
Education Mean (SD) |
||
|---|---|---|---|---|
| Female | Male | |||
| Control | 30 | 7 | 29.89 (10.45) | 15.50 (2.36) |
| Marijuana | 28 | 60 | 24.14 (7.41) | 13.79 (2.55) |
| MJ + NIC | 14 | 49 | 25.79 (7.57) | 13.10 (1.91) |
| Nicotine | 30 | 52 | 30.32 (10.10) | 13.66 (2.35) |
| Overeating | 18 | 9 | 29.74 (10.64) | 14.74 (2.10) |
MJ + NIC stands for the Marijuana + Nicotine group. Distribution of gender per group, and mean (standard deviation) of Age and Education per group. See Supplementary Material, available online, for subsequent detailed analyses of demographics.
Our study included a total of 297 individuals, who had completed the ImpSS and the BIS, from the four a priori groups (as discussed in Participants): Marijuana (n = 88), Nicotine (n = 82), Overeaters (n = 27), and non-using Controls (n = 37). We further identified a subgroup of Marijuana users who reported at least daily nicotine use (according to the Smoking History Questionnaire), henceforth, referred to as Marijuana + Nicotine (n = 63). Usage characteristics for Marijuana, Nicotine, and Marijuana + Nicotine groups are described in Table 2.
Table 2.
Mean (standard deviation) usage characteristics of the Marijuana, Marijuana + Nicotine (MJ + NIC), Nicotine, and Control groups. Usage characteristics of nicotine and marijuana were not measured for the Overeaters group. Recent marijuana usage characteristics were not measured for the Nicotine or Control groups.
| Marijuana | MJ + NIC | Nicotine | Control | |
|---|---|---|---|---|
| Recent number of cigarettes per day* | 0.43 (1.57) | 10.17 (6.25)1 | 14.60 (7.60)1 | 0.11 (0.42)7 |
| Recent marijuana use per using day** | 3.33 (2.88)2 | 3.23 (1.69)2 | — | — |
| Marijuana use in last 90 days*** | 79.98 (17.04)3,4 | 81.32 (17.75)3,4 | 25.39 (35.80)3 | 0.27 (1.19)8 |
| Cigarette use in last 90 days*** | 5.99 (17.66)5 | 82.06 (19.45)5,6 | 89.95 (00.44)5,6 | 0.35 (1.40)9 |
Number of self-reported cigarettes on a typical using day from the Smoking History Questionnaire;
computed from questions about daily and weekly self-report estimates of number of times smoking marijuana from the Marijuana Use Questionnaire;
from Timeline Follow Back Calendar of the past 90 days.
Marijuana + Nicotine group reported smoking fewer cigarettes per day than the Nicotine group [t(142.3) = −3.85, p = 0.0002)],
but not fewer cannabis occasions per day than the Marijuana group [t(125.7) = −0.259, p = 0.80)].
The Marijuana and Marijuana + Nicotine groups used marijuana on more days than the Nicotine group [t(116.65) = 12.45, p<0.0001, t(121.94) = 12.43, p<0.0001 (respectively)],
but not less than one another [t(136.88) = 0.47, p = 0.64)].
The Nicotine and Marijuana + Nicotine groups smoked cigarettes on more days than the Marijuana group [t(86.11) = 44.33, p < 0.0001, t(125.82) = 24.57, p<0.0001 (respectively)],
with a slight difference between one another (t(62.05) = 3.22, p = 0.002).
Only two Control participants estimated any recent nicotine product use.
Both had only two occurrences. Only three Control participants estimated any nicotine product use in the past 90 days, only one of these individuals overlapped.
and only three Control participants estimated any marijuana use in the past 90 days: only one of these individuals overlapped. In total, 32 of the 37 Control participants reported no usage of nicotine or marijuana.
Measures
The Impulsive Sensation Seeking Scale (ImpSS) is a 19-item self-report questionnaire, which is a subscale of the Zuckerman-Kuhlman Personality Questionnaire (17). The ImpSS is intended to capture two factors: sensation-seeking and impulsivity. Participants respond to each item with the values TRUE or FALSE, which are respectively scored as 1 or 0 point. Summary scores range from 0–19 with higher scores indicating greater impulsive sensation seeking behavior.
The Barratt Impulsivity Scale (BIS) is a 30-item self-report questionnaire that captures various aspects of impulsivity (18): inattention, motor impulsiveness, self-control problems, cognitive complexity, perseverance, and cognitive instability. These aspects represent broader factors: Attentional Impulsiveness (attention and cognitive instability), Motor Impulsiveness (motor impulsiveness and perseverance), and Non-planning (self-control and cognitive complexity). On the 30-item BIS, participants respond to each item using a 4-response scale (1: Rarely/Never; 2: Occasionally; 3: Often; 4: Almost Always/Always). Summary scores range from 30–120 with higher scores indicating greater impulsiveness.
Statistical analyses
We performed two sets of analyses: ANOVAs and DiCA (35) – a technique that can identify qualitative differences in patterns of responses between groups (42). All analyses were performed with R (51). ANOVAs were performed with the “car” package (52), DiCA and inference tests were performed with the “TExPosition” and “TInPosition” packages (53). The Supplementary Material, available online, provides a detailed exposition of DiCA and inference tests.
ANOVAs
We performed one-factor between-subjects ANOVAs on the summary scores for the ImpSS and the BIS.
DiCA and data structure
For analysis with DiCA, both the ImpSS and BIS were recoded into question-response levels (disjunctive coding) as in (41,42,54). For example, a response of RARE for BIS question 5 (I do not “pay attention”) was recoded as a 0/1 pattern spanning four columns: {1,0,0,0} and a response of OFTEN was recoded as the pattern {0,0,1,0}. This process yielded 120 columns for the BIS (4 columns per 30 questions), and 38 columns for the ImpSS (2 columns per 19 questions). Because the instruments have different sizes, we normalized each instrument so that the variances of the ImpSS and BIS were equal [see (38,55) for more details]. With DiCA, we analyzed the BIS and ImpSS together.
DiCA requires a group × variable contingency table that represents the frequencies of each question-response level for each group. Correspondence analysis is then performed on this table. DiCA – like correspondence analysis or principal components analysis – integrates the variables of a matrix into linear combinations in order to create new uncorrelated (orthogonal) variables, called components. Items, groups, and individuals are assigned values called component (or factor) scores that describe how much items, groups, or individuals contribute to a component. Component scores are typically presented graphically two components at a time to create component maps.
Inference tests
Stability and reliability of the DiCA model were assessed via bootstrap (56,57), and permutation (58) resampling. Inference tests indicate if the omnibus model is significant, which components are significant, and which variables or groups significantly contribute to the component structure (see Supplementary Material, available online).
Results
ANOVA findings
ANOVAs were performed on the summary scores from the ImpSS and BIS. There was a significant effect of group on the BIS [F(4,292) = 8.09, p<0.0001]. Post-hoc comparisons showed that the Control and Marijuana groups were less impulsive than the Marijuana + Nicotine, Nicotine, and Overeating groups (Table 3). There were no significant differences between the remaining groups or between the Control and Marijuana groups. There was a significant effect of group on the ImpSS [F(4,292) = 6.71, p<0.0001]. Post-hoc comparisons showed that the Control group was significantly less impulsive than all other groups except the Overeating group (Table 3). There were no significant differences between the substance use and Overeating groups.
Table 3.
Impulsive Sensation Seeking (ImpSS) scale and Barratt’s Impulsivity Scale (BIS) summary score information scores for the groups.
| ImpSS | BIS | Control ImpSS, BIS |
Marijuana ImpSS, BIS |
MJ + NIC ImpSS, BIS |
Nicotine ImpSS, BIS |
|
|---|---|---|---|---|---|---|
| Control | 6.00 (4.48) | 57.11 (10.80) | ||||
| Marijuana | 8.66 (4.17) | 59.45 (11.05) | 0.015, 1.0 | |||
| MJ + NIC | 10.44 (4.06) | 66.41 (11.99) | 0.001, 0.001 | 0.113, 0.002 | ||
| Nicotine | 9.35 (4.38) | 64.88 (10.69) | 0.001, 0.005 | 1.0, 0.017 | 1.0, 1.0 | |
| Overeating | 8.74 (4.18) | 67.78 (11.25) | 0.113, 0.002 | 1.0, 0.008 | 0.82, 1.0 | 1.0, 1.0 |
Means (standard deviation) and all Bonferroni corrected p values for pairwise t-tests on the ImpSS and BIS summary scores.
DiCA findings
DiCA produced four components. Data were resampled 2000 times for permutation and bootstrap tests. An omnibus test of the inertia (sum of the eigenvalues) – whose significance was evaluated with a permutation test – indicated that the overall structure of the data was significant (Inertia = 0.0515, pperm<0.0005). Further permutation tests identified the first three components as significant (Component 1 = 50.19%, pperm<0.0005, Component 2 = 24.18%, pperm<0.0005, Component 3 = 15.98%, pperm<0.0005, respectively). The between group variance – which was evaluated by an R2-type statistic that measures the variance explained by the groups – was moderate but not significant (R2=0.196, pperm = 0.0695). All permutation results are presented graphically in Supplementary Figures S1–2, available online.
Two sets of bootstrap tests were conducted to test: (i) if groups were reliably different from one another, via confidence intervals [as in (35,59)], and (ii) which items significantly contributed to the variance, via the bootstrap ratio statistic [sometimes called a bootstrapped-t-value, (60)]. All confidence intervals separated the groups on at least one component; therefore, all groups were significantly different from one another (pboot<0.0005; see Figures 1a and 3a). Bootstrap ratio tests identified the groups (Table 3) and items (see Supplementary Tables S3–S6) that significantly contributed to the overall structure of the components, and these are discussed and illustrated throughout the following sections and the online Supplementary Material.
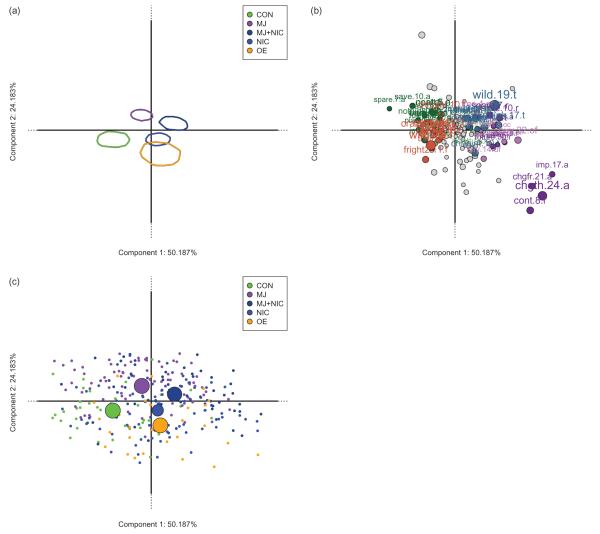
Figure 1.
(a) (top left) shows confidence intervals around the bootstrapped means of each group on Components 1 (horizontal) and 2 (vertical). (b) (top right) shows all the question-response items from the Impulsive Sensation Seeking (ImpSS) scale and Barratt’s Impulsivity Scale (BIS) colored by response level or gray. Colored items significantly contribute to Component 1, whereas gray items do not. Question-response items that appear closer to a group are more associated to that group than to any other group. For example, Marijuana + Nicotine is more associated to TRUE responses on the ImpSS than is any other group. (c) shows the distribution of individuals per group on Components 1 and 2.
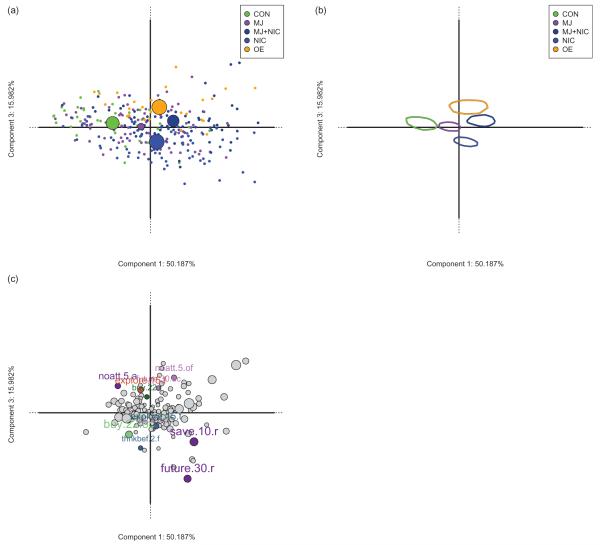
Figure 3.
(a) shows the distribution of individuals per group on Components 1 and 3. Note that Component 3 is driven by, and dissociates, the opposite response patterns of the Overeater and Nicotine groups. (b) shows confidence intervals around the bootstrapped means of each group on Components 1 (horizontal) and 3 (vertical). (c) shows all the question-response items from the Impulsive Sensation Seeking (ImpSS) scale and Barratt’s Impulsivity Scale (BIS) colored by response level or gray. Colored items significantly contribute to Component 3, whereas gray items do not. The significant items on Component 3 are the items that dissociate Overeaters from Nicotine groups.
Component 1
Many items from the ImpSS and BIS significantly contributed to Component 1. Figure 1(b) shows that Component 1 contrasts high impulsive sensation seeking traits (e.g. “I change things I like to do a lot” =Always) against low-to-no impulsive sensation seeking traits (e.g. “I sometimes do ‘crazy’ things just for fun” = FALSE). The Control, Marijuana + Nicotine, and Marijuana groups significantly contributed to Component 1 (Table 4).
Table 4.
The bootstrap ratios of each group. Italic values above/below ±2 are considered significant.
| Component 1 | Component 2 | Component 3 | |
|---|---|---|---|
| Control | −5.72 | −2.97 | 1.58 |
| Marijuana | −2.14 | 6.95 | 0.44 |
| MJ + NIC | 4.13 | 2.42 | 2.75 |
| Nicotine | 1.34 | −3.60 | −7.63 |
| Overeating | 1.16 | −5.11 | 6.88 |
Component 1 reflected, in part, summary scores of the groups from lowest to highest (left to right): Control, Marijuana, Nicotine, Overeaters, and Marijuana + Nicotine (Figures 1a and c; see also Tables 3–4 and Supplementary Table S3, online). To note, Marijuana and Control are grouped on Component 1 whereas Overeaters, Nicotine, and Marijuana + Nicotine are grouped on the opposite side; this pattern means that there are traits shared between Marijuana and Control, and traits shared between Overeaters, Nicotine, and Marijuana + Nicotine. In DiCA, the center (origin) of a component map is the average; thus the Marijuana and Control groups have below average impulsive traits, whereas the Overeating, Nicotine, and Marijuana + Nicotine groups have above average impulsive traits.
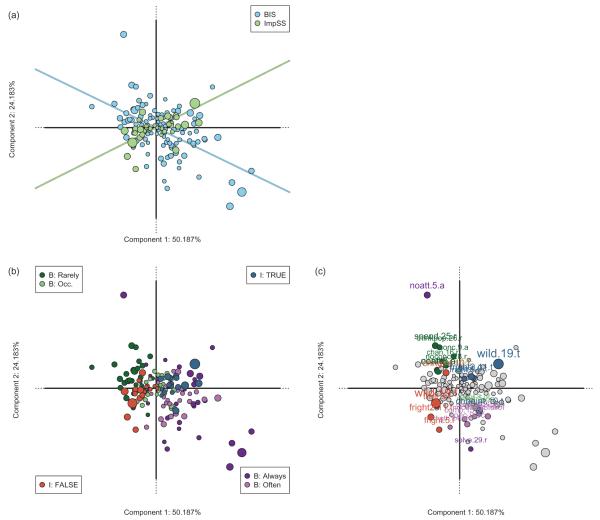
Component 2
All groups significantly contributed to Component 2 (Table 4). In contrast to Component 1, Control, Nicotine, and Overeaters are grouped together, whereas Marijuana and Marijuana + Nicotine are grouped together on Component 2 (Figure 1). Figure 2(a) shows each question-response item colored by the instrument to which they belong (i.e. ImpSS or BIS). Together, the ImpSS and BIS make an “X” shape on the component map, a configuration suggesting that – for these populations – the two instruments are orthogonal (see also Partial Projections section below). This dissociation of the instruments (Figure 2b), is best understood per quadrant: top right reflects high ImpSS, top left reflects low BIS, bottom left reflects low ImpSS, and bottom right reflects high BIS traits. Sensation seeking and attention items – specifically, active vs. avoidant sensation seeking (via ImpSS) and attention vs. inattention (via BIS) – significantly contributed to Component 2 (see Figure 2c and Supplementary Tables S3 and S4).
Figure 2.
(a) shows Impulsive Sensation Seeking (ImpSS) scale and Barratt’s Impulsivity Scale (BIS) question-response items on Components 1 (horizontal) and 2 (vertical), color-coded by which instrument they belong to (ImpSS in blue; BIS in green). Fit lines were computed from the correlation – within instruments – between Component 1 and Component 2 scores. The two instruments form an “X” shape on Components 1 and 2. (b) shows all the question-response items from the ImpSS and BIS colored by response level (including reverse coded questions). Figure legends indicate the types of responses/questions that appear in the four quadrants. (c) shows all the question-response items from the ImpSS and BIS colored by response level or gray. Colored items significantly contribute to Component 2, whereas gray items do not.
Component 3
Control, Nicotine, and Overeaters significantly contributed to Component 3 (Table 4; Figures 3a and b), and only a few question-response items (Figure 3c; Supplementary Table S5) significantly contributed to Component 3. Component 3 is driven by the dissociation between the Nicotine and Overeating groups. Significant items on Component 3 include planning, low attention, and poor-spending habits (see Figure 3c, Supplementary Table S5).
Partial projections
To assess the “X” shape of the ImpSS and BIS, we analyzed partial component scores for the individuals [(35,55), see also online Supplementary Material]. Partial component scores describe how each instrument contributed to the overall model.
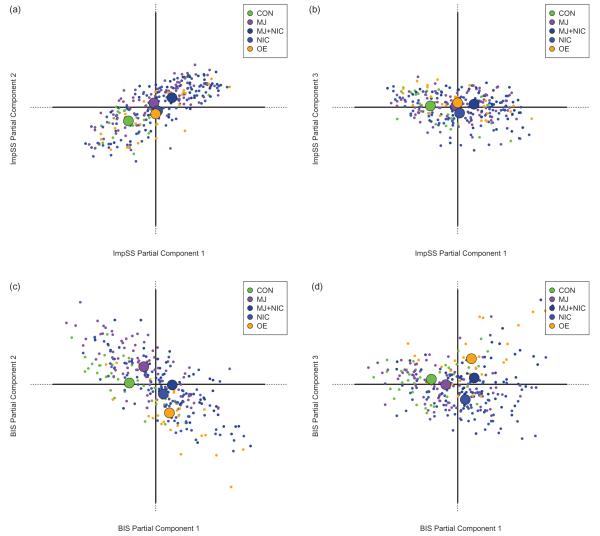
Figures 4(a and b) show the partial component scores for the ImpSS and indicate that the groups clustered in three classes, regardless of the component, corresponding to (1) low (Control), (2) medium (Marijuana, Overeaters, Nicotine), and (3) high (Marijuana + Nicotine) ImpSS scores. In contrast, the BIS partial component scores are much more diverse (Figures 4c and d) and distributed across all components. Furthermore, the Control and Marijuana groups have similar BIS patterns, where as the Overeating group has a fairly unique pattern unto itself.
Figure 4.
To note, (a) and (c) further suggest an orthogonal relationship between the Impulsive Sensation Seeking (ImpSS) scale and Barratt’s Impulsivity Scale (BIS). Additionally, the lack of dispersion amongst the ImpSS in (a) and (b) suggest that the ImpSS is unidimensional. In contrast, the BIS shows dispersion across all components (c) and (d) and suggests that the BIS captures several unique aspects of impulsivity. (a) shows the ImpSS partial projection of individuals and groups on Components 1 and 2. (b) shows the ImpSS partial projection of individuals and groups on Components 1 and 3. (c) shows the BIS partial projection of individuals and groups on Components 1 and 2. (d) shows the BIS partial projection of individuals and groups on Components 1 and 3.
Correlations between partial component scores (Table 5) show a strong and significant relationship between the BIS and the ImpSS on Component 1 (r = 0.61, pperm<0.0005), but, importantly, the correlation between Component 2 of the BIS and Component 2 of the ImpSS was negligible (r = −0.03, pperm = 0.5940).
Table 5.
Correlation (r) and p values between partial component scores for the Barratt’s Impulsivity Scale (BIS) and Impulsive Sensation Seeking (ImpSS) scale.
| ImpSS Comp 1 | ImpSS Comp 2 | ImpSS Comp 3 | |
|---|---|---|---|
| BIS Comp 1 | r = 0.612, pperm<0.0005 | r = 0.279, pperm<0.0005 | r = −0.373, pperm<0.0005 |
| BIS Comp 2 | r = −0.355, pperm<0.0005 | r = −0.030, pperm = 0.594 | r = 0.261, pperm<0.0005 |
| BIS Comp 3 | r = −0.018, pperm = 0.747 | r = −0.039, pperm = 0.508 | r = 0.137, pperm = 0.017 |
We provide permutation (pperm) p values; they are nearly identical to parametric p values. To note, Partial Component 1 of the BIS is significantly related to all Partial Components for the ImpSS. This suggests that the ImpSS is a largely unidimensional scale in respect to our population (see also Figures 4a and b). Importantly, the Partial Component 2 for BIS and ImpSS have nearly null correlation. This suggests that these instruments capture orthogonal factors of impulsivity (see also Figures 2a and b, 4a and c).
Further analyses
Given that participant characteristics could also influence impulsivity, we explored several connections between our factor structure, severity of disorder, and demographics. Additionally, we also explored how our factor structure based on self-reported impulsivity (trait) related to objective measures of impulsivity (state).
Severity
Following similar work in alcohol use disorders, we investigated how the component structure related to severity of respective disorders (61). Each group has a different index of severity: number of SCID marijuana dependency symptoms (47) for Marijuana and Marijuana + Nicotine (because they come from the same study), FTND (48) for Nicotine, and BMI and BES for Overeaters. We found that the FTND and BMI were unrelated to the factor structure (Table 6). However, severity indices for the Overeaters (via BES), Marijuana, and Marijuana + Nicotine (via SCID) groups were positively related to Component 1. Further, we observed negative correlations between severity score indices for the Overeaters (via BES), Marijuana, and Marijuana + Nicotine (via SCID) groups, and Component 2. No severity index was significantly related to Component 3 (Table 6).
Table 6.
Correlation (r) and p values between measures of disorder severity and our three impulsivity components.
| Comp 1 | Comp 2 | Comp 3 | |
|---|---|---|---|
| Marijuana SCID DSx | r = 0.266, pperm = 0.017 | r = −0.256, pperm = 0.021 | r = −0.169, pperm = 0.124 |
| MJ + NIC SCID DSx | r = 0.341, pperm = 0.008 | r = −0.296, pperm = 0.028 | r = 0.059, pperm = 0.676 |
| Nicotine FTND | r = −0.192, pperm = 0.094 | r = −0.080, pperm = 0.474 | r = −0.105, pperm = 0.345 |
| Overeating BMI | r = −0.250, pperm = 0.253 | r = −0.154, pperm = 0.459 | r = −0.147, pperm = 0.4895 |
| Overeating BES | r = 0.495, pperm = 0.015 | r = −0.421, pperm = 0.037 | r = 0.381, pperm = 0.0615 |
We provide permutation (pperm) p values; they are nearly identical to parametric p values. Here we provide correlations between our impulsivity components and: (1) the SCID (Dependence Symptoms; DSx) for Marijuana and Marijuana + Nicotine groups, (2) The Fagerström Test for Nicotine Dependence (FTND) for the Nicotine group, and (3) BMI and the Binge Eating Scale (BES) for the Overeating group. The Marijuana, Marijuana + Nicotine, and Overeating group (via the BES) have higher severity associated with higher overall impulsivity. BMI for Overeaters is not related to overall impulsivity. However, the FTND shows a mild negative, albeit non-significant, correlation with higher impulsivity in the Nicotine group. A similar pattern is expressed on Component 2 (“instrument dissociation”). This pattern could reflect that individuals who express higher severity are negatively correlated with sensation seeking (i.e. the ImpSS), and positively correlated with attentional and cognitive aspects of impulsivity (i.e. the BIS). Component 3 has only weak and non-significant correlations. However, the correlation with the BES in the Overeating group is due most likely to the fact that Component 3 is driven largely by this group.
Demographics
Comprehensive analyses of demographic characteristics (age, income, gender, and education) can be found in the online Supplementary Material. To note there was little-to-no effect of gender and no interactions between gender and groups. Two-factor between-groups ANOVAs showed only main effects of group association. Additional analyses within the DiCA model showed a significant effect of gender, however, this effect is very weak (R2 = 0.04). Finally, there was a mild association of age with Components 1 and 2.
State and trait impulsivity
In our studies, we had access to two measures of state impulsivity and/or attention: Continuous Performance Task [CPT, (62)], and Trail Making Task [“Trails”, (63)]. The results showed that our component structure based on self-reported trait measures is unrelated to the CPT and Trails (Table 7).
Table 7.
Correlation (r) and p values between the Continuous Performance Task (CPT) and Trail Making Test (Trails) with our impulsivity components.
| Comp 1 | Comp 2 | Comp 3 | |
|---|---|---|---|
| CPT d’ | r = 0.056, pperm = 0.544 | r = 0.001, pperm = 0.986 | r = 0.018, pperm = 0.854 |
| CPT β | r = 0.160, pperm = 0.086 | r = 0.016, pperm = 0.864 | r = −0.036, pperm = 0.704 |
| Trails (B–A) | r = 0.017, pperm = 0.837 | r = −0.082, pperm = 0.306 | r = −0.045, pperm = 0.578 |
CPT: d’ reflects detection accuracy, β reflects avoidance of commission errors. Trails is represented by Trails task B–Trails task A, which reflects executive function (via task switching). In general there is no correlation between the CPT – a laboratory measure of attention and state impulsivity – and our three trait-based impulsivity factors. Further, there is no correlation between the Trails – a measure of attention, and executive function – and our three trait-based impulsivity components.
Discussion
This study was conducted specifically to identify distinct impulsivity traits per group. DiCA revealed three components that describe orthogonal aspects of impulsivity. First, we discuss these components in the context of impulsivity. Next, we discuss the traits specific to the participants’ groups.
Components
Component 1 reflects “overall impulsivity”. This interpretation is supported by: (1) the large number of items from both measures that significantly contribute to Component 1 (Supplementary Table S2), (2) the large correlation of the partial component scores of individuals (Table 5), and (3) the fact that the component scores for the groups (horizontal axis in all figures) tend to reflect the total summary score (Table 3). Both Component 1 and summary scores showed an interesting relationship amongst the groups. Clearly, Overeaters, Nicotine, and Marijuana + Nicotine have high overall impulsivity; Control, as expected, has very low overall impulsivity. Unexpectedly, Marijuana also has a low overall impulsivity.
Component 2 reflects a general “instrument dissociation”. The instrument items (Figures 2a and b) and the partial component scores (Figures 4a and c) are effectively orthogonal; there is nearly zero correlation between the general structures of ImpSS and BIS on Component 2 (Table 5). Taken in context with Component 1 (left reflects lower overall impulsivity, right reflects higher overall impulsivity; Figures 1 and 2), the top of Component 2 reflects sensation seeking, whereas the bottom of Component 2 reflects attentional deficits.
Overall, this dissociation suggests that there are features of impulsivity traits captured by one instrument but not by the other, and importantly, that this dissociation helps characterize each group: (1) the separation between Control and Marijuana + Nicotine groups was due to sensation seeking questions (e.g. “I like doing things just for the thrill of it”) on the ImpSS, (2) the separation of Marijuana from Overeaters and Nicotine was largely due to questions about attention, focus, and concentration (e.g. “I concentrate easily”) on the BIS, and (3) the combination of the two components separated all groups from one another with the exception of Nicotine from Overeaters.
Component 3 largely reflects “forethought” or questions mostly about spending money, planning, interest changes, and the future (e.g. “I rarely like to think about my life will be in the future”, see Supplementary Table S4). Recall that the Nicotine and Overeating groups are the primary contributors – in opposite ways (Figure 3) – to Component 3 (Table 4). The Overeaters responses reflect acknowledgment in the affirmative of forethought, while the Nicotine group responses reflect acknowledgment in the negative of forethought.
Relation of structure with other measures
Because impulsivity is a contributing factor to both substance misuse and treatments for substance misuse, it is important to understand how impulsivity is related to other measures of impulsivity and severity of substance misuse.
First, we show that, in general, as severity of substance misuse increases, so do the factor scores on Component 1, as well as attentional (negative scores on Component 2) aspects of impulsivity (Table 6). However, these correlations only generally reflect that as severity increases, so do aspects of impulsivity.
Though both state and trait aspects of impulsivity contribute to substance misuse (13), we found no discernible relationship between the factors extracted by DiCA and the CPT and Trails, two neuropsychological measures of attention, impulsivity, and executive function (Table 7). However, this absence of correlation is not surprising (19,64,65) because the relationship between state and trait measures generally tend to be weak at best, but this absence of correlation could also indicate that trait and state measures are intrinsically different aspects of impulsivity.
Unique aspects of impulsivity in substance use
Some prior work has shown traces of unique impulsivity traits associated to different substance users. For example, Meda et al. (34) derived a five-factor model based on state and trait measures in healthy controls vs. “at-risk/addicted” participants. Huba, Newcomb, and Bentler (66) used Interbattery Factor Analysis (67) – a technique also known more recently as partial least squares correlation (68,69) – to examine the relationship between sensation-seeking and drug use in an adolescent population. Huba et al. (66) identified factors common to types of drugs used and sensation-seeking traits. Our results further identify the unique aspects of both impulsivity and sensation-seeking traits in each of our groups.
Non-using controls
In general, the control group had low responses to questions across both instruments. Specifically, DiCA showed that the control group was more associated with avoidance of thrill-seeking than the other groups (Figures 1 and 2).
Marijuana users
Though marijuana use has been associated with higher overall levels of impulsivity (70,71), our results suggest otherwise: the Marijuana group scored lower than other substance use and eating disorder groups on the BIS and ImpSS (Figure 1 and Table 3). Furthermore, DiCA revealed that the Marijuana group was more associated with high levels of focus and attention, and infrequent interest changes than any other group (Figure 2 and Supplementary Table S3).
Marijuana + Nicotine users
In general, users of multiple substances tend to have higher impulsivity than other substance abuse groups (72,73). We found that our Marijuana+Nicotine group scored very high on both the ImpSS and the BIS (Table 3). Furthermore, the Marijuana + Nicotine group is associated with pathological aspects of impulsivity: active thrill-seeking and lack of focus/attention (Figures 1, 2, and 4). Attentional issues are a shared characteristic amongst the Marijuana + Nicotine, Nicotine, and Overeating groups (Figures 1, 2, and 4).
Nicotine users
Results showed that Nicotine was more associated with lack of forethought, poor spending habits, and frequent interest changes than the other groups (Figures 1–3, Supplementary Table S4). Perkins et al. (74) showed increased novelty seeking and response disinhibition as a function of nicotine sensitivity. Additionally, nicotine exposure and higher levels of impulsivity are associated with immediate reward (75).
Overeating individuals
Loss of control over food has been of particular focus recently (46,76,77), especially with regard to the qualities that define addiction to – or substance abuse of – food (23,24). The Overeating and Nicotine groups share qualities of attentional issues (Figures 1 and 2). However, Overeating participants, as opposed to Nicotine, tend to plan for immediate and long-term future (i.e. “forethought”) (Figure 3 and Supplementary Table S3).
Broader implications
Measures of impulsivity
The BIS has been the subject of recent contention: (i) Stanford et al. (19) showed that the BIS and subsequent factors are reliable and strongly related to other measures of impulsivity, but (ii) Reise et al. (26) showed that the BIS is not as (psychometrically) reliable as claimed and, accordingly, suggested a different factor structure, whereas (iii) Steinberg et al. (27) reframed the BIS to create a simple unidimensional measure. Our results within substance use and overeating populations suggest a more nuanced story. We showed that (1) the BIS is not as related to the ImpSS as was expected; (2) while the traditional BIS factors are not necessarily evident, we do not see the same factors as Reise et al. (26); and (3) the BIS is not unidimensional amongst substance use and eating disorder populations, but the ImpSS is.
For measures of impulsivity in substance use and eating disorders
Following Reise et al. (26) and Steinberg et al. (27), we did not find the traditional BIS factor structure but we did find some aspects from the original BIS definition (22). Unlike Stanford et al. (19) – who found strong relationships between BIS and other measures – we revealed a clear orthogonal relationship between the BIS and ImpSS. We also showed that impulsivity, just within substance use and eating disorders groups, has a complex multidimensional structure that does not map to the traditional or revised structures of the ImpSS and especially the BIS. Further, some questions did not significantly contribute to our structure (Supplementary Table S6).
These findings suggest two conclusions: (1) the BIS and ImpSS may not be tailored to particular types of impulsivity traits within substance use and eating disorders, and (2) both measures could be truncated for use within substance use populations, and that – like the ImpSS – the BIS may benefit from using dichotomous responses. For example, the BIS question “I change my mind about what I like to do” generally does not contribute to the components. However, a similar ImpSS question, “I tend to change interests frequently”, does contribute to the component structure (see Supplementary Tables S3–6).
For substance use research
A clearer view of impulsive traits in substance use and eating disorders is an important step forward. Currently, the exact role impulsivity plays is not clear (5,6,12), but it is known to play an important role in behavorial (78) and neurobiological (79) responses in substance use, as well as being associated with disorder severity (58).
A deeper understanding of the role of trait impulsivity in substance use may provide insight into more effective treatments (8,9,80) or provide better predictive markers (81–83). Because trait impulsivity is considered an inherent characteristic of an individual (13), and given that genetics contribute to both personality traits (84) and addiction (85), trait impulsivity could be a useful intermediate (a.k.a. endo-) phenotype for substance use disorders (86,87), just as in other disorders (88).
In conjunction with diverse behavioral mechanisms (12,32,34), the unique impulsive traits in various disorders could help identify specific biological, neural, and cognitive mechanisms (87,89–91), and may provide better multidimensional criteria to define symptoms – instead of just broad diagnostic categories – specific to various self-regulatory failures, substance abuse, and addiction.
Limitations and Conclusions
Some limitations of our study should be mentioned. Lack of gender effects may be due, in part, to an unbalanced gender distribution within the groups. Additionally, because participants in the current study were from three separate studies, not all measures were available across groups. For example, measures of nicotine and marijuana use were unavailable for participants recruited for the overeating study, and, therefore some participants assigned to the Overeater group could also display traits shared with other groups. Such a configuration would decrease the separation between groups and so the differences between groups could, actually, be stronger than what we report.
Finally, there exist numerous measures of both trait and state impulsivity, which could further delineate aspects of substance abuse. It will also be important to define which state and trait measures capture similar and distinct aspects of impulsivity to help identify which state measures are comparable to trait measures.
To fully understand the role of impulsivity traits with respect to addictive behaviors, future studies could also benefit from a common index of disorder severity, additional substance using groups (e.g. cocaine, heroin, methamphetamine), a balanced gender distribution, and a unified recruitment strategy for all participants.
To conclude, our findings show that: (1) there is a novel factor structure to the BIS and ImpSS within substance use and overeating, and (2) this factor structure characterizes unique impulsivity traits to dissociate different substance use and eating disorder groups – an important step forward in rethinking diagnostic strategies.
Supplementary Material
Acknowledgements
Part of this work was supported by grants from NIDA for marijuana studies (K01 DA021632-01A1 to FMF) and The Mind Research Network for control, nicotine, and obesity studies (Institutional Grant to FMF). FMF and DB are currently supported by NIDA (R01 DA030344-01 and F31 DA035039-01A1, respectively). DB and HA created some of the open source software used for analysis in this manuscript (TExPosition and TInPosition). The authors would like to thank Ursula Myers and Michelle Coyazo for their role in data collection. They would also like to thank two anonymous reviewers and the editor for useful comments on previous drafts of this paper.
Footnotes
Declaration of interest The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Supplementary Material Available Online Supplementary Figures S1–4. Supplementary Tables S1–8. Supplementary material can be viewed and downloaded at http://informahealthcare.com/ada
References
- 1.Witt EA, Hopwood CJ, Morey LC, Markowitz JC, McGlashan TH, Grilo CM, Sanislow CA, et al. Psychometric characteristics and clinical correlates of NEO-PI-R fearless dominance and impulsive antisociality in the Collaborative Longitudinal Personality Disorders Study. Psycholog Assess. 2010;22:559–568. doi: 10.1037/a0019617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baumeister RF, Heatherton TF. Self-regulation failure: an overview. Psycholog Inquiry. 1996;7:1–15. [Google Scholar]
- 3.Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev. 2004;28:343–351. doi: 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 4.Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nature Neurosci. 2005;8:1450–1457. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- 5.Perry J, Carroll M. The role of impulsive behavior in drug abuse. Psychopharmacology. 2008;200:1–26. doi: 10.1007/s00213-008-1173-0. [DOI] [PubMed] [Google Scholar]
- 6.Fernie G, Peeters M, Gullo MJ, Christiansen P, Cole JC, Sumnall H, et al. Multiple behavioural impulsivity tasks predict prospective alcohol involvement in adolescents. Addiction. 2013;108:1916–1923. doi: 10.1111/add.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belin D, Mar AC, Dalley JW, Robbins TW, Everitt BJ. High impulsivity predicts the switch to compulsive cocaine-taking. Science. 2008;320:1352–1355. doi: 10.1126/science.1158136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldstein Ewing SW, LaChance HA, Bryan A, Hutchison KE. Do genetic and individual risk factors moderate the efficacy of motivational enhancement therapy? Drinking outcomes with an emerging adult sample. Addict Biol. 2009;14:356–365. doi: 10.1111/j.1369-1600.2009.00149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bankston SM, Carroll DD, Cron SG, Granmayeh LK, Marcus MT, Moeller FG, et al. Substance abuser impulsivity decreases with a nine-month stay in a therapeutic community. Am J Drug Alcohol Abuse. 2009;35:417–420. doi: 10.3109/00952990903410707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrard I, Crépin C, Ceschi G, Golay A, Van der Linden M. Relations between pure dietary and dietary-negative affect subtypes and impulsivity and reinforcement sensitivity in binge eating individuals. Eating Behaviors. 2012;13:13–19. doi: 10.1016/j.eatbeh.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell MR, Potenza MN. Addictions and personality traits: impulsivity and related constructs. Curr Behav Neurosci Rep. 2104;1:1–12. doi: 10.1007/s40473-013-0001-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evenden JL. Varieties of impulsivity. Psychopharmacology. 1999;146:348–361. doi: 10.1007/pl00005481. [DOI] [PubMed] [Google Scholar]
- 13.De Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addiction Biol. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horvath P, Zuckerman M. Sensation seeking, risk appraisal, and risky behavior. Personality Individ Differences. 1993;14:41–52. [Google Scholar]
- 15.Leo JAD, Dam NTV, Hobkirk AL, Earleywine M. Examining bias in the impulsive sensation seeking (ImpSS) Scale using Differential Item Functioning (DIF) – an item response analysis. Personality Individ Differences. 2011;50:570–576. [Google Scholar]
- 16.McDaniel SR, Mahan JE., III An examination of the ImpSS scale as a valid and reliable alternative to the SSS-V in optimum stimulation level research. Personality Individ Differences. 2008;44:1528–1538. [Google Scholar]
- 17.Zuckerman M, Kuhlman DM, Joireman J, Teta P, Kraft M. A comparison of three structural models for personality: the big three, the big five, and the alternative five. J Personality Soc Psychol. 1993;65:757–768. [Google Scholar]
- 18.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 19.Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, Patton JH. Fifty years of the Barratt Impulsiveness Scale: an update and review. Personality Indiv Differences. 2009;47:385–395. [Google Scholar]
- 20.Chase HW, Hogarth L. Impulsivity and symptoms of nicotine dependence in a young adult population. Nicotine Tob Res. 2011;13:1321–1325. doi: 10.1093/ntr/ntr114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ball SA. The validity of an alternative five-factor measure of personality in cocaine abusers. Psychological Assess. 1995;7:148–154. [Google Scholar]
- 22.Curran MF, Fuertes JN, Alfonso VC, Hennessy JJ. The association of sensation seeking and impulsivity to driving while under the influence of alcohol. J Addictions Offender Counsel. 2010;30:84–98. [Google Scholar]
- 23.Meule A, Lutz APC, Vögele C, Kübler A. Impulsive reactions to food-cues predict subsequent food craving. Eating Behav. 2014;15:99–105. doi: 10.1016/j.eatbeh.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 24.Murphy CM, Stojek MK, MacKillop J. Interrelationships among impulsive personality traits, food addiction, and Body Mass Index. Appetite. 2014;73:45–50. doi: 10.1016/j.appet.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC, Grabowski J. The impact of impulsivity on cocaine use and retention in treatment. J Substance Abuse Treat. 2001;21:193–198. doi: 10.1016/s0740-5472(01)00202-1. [DOI] [PubMed] [Google Scholar]
- 26.Reise SP, Moore TM, Sabb FW, Brown AK, London ED. The Barratt Impulsiveness Scale–11: Reassessment of its structure in a community sample. Psycholog Assess. 2013;25:631–642. doi: 10.1037/a0032161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinberg L, Sharp C, Stanford MS, Tharp AT. New tricks for an old measure: the development of the Barratt Impulsiveness Scale-Brief (BIS-Brief) Psychol Assess. 2013;25:216–226. doi: 10.1037/a0030550. [DOI] [PubMed] [Google Scholar]
- 28.Reid RC, Cyders MA, Moghaddam JF, Fong TW. Psychometric properties of the Barratt Impulsiveness Scale in patients with gambling disorders, hypersexuality, and methamphetamine dependence. Addict Behav. 2013 doi: 10.1016/j.addbeh.2013.11.008. [epub ahead of print] doi: j.addbeh.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 29.Vassileva J, Paxton J, Moeller FG, Wilson MJ, Bozgunov K, Martin EM, Gonzalez R, Vasilev G. Heroin and amphetamine users display opposite relationships between trait and neurobehavioral dimensions of impulsivity. Addict Behav. 2014;39:652–659. doi: 10.1016/j.addbeh.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Littlefield AK, Stevens AK, Sher KJ. Impulsivity and alcohol involvement: multiple, distinct constructs and processes. Curr Addict Rep. 2014;1:33–40. doi: 10.1007/s40429-013-0004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bloom EL, Matsko SV, Cimino CR. The relationship between cigarette smoking and impulsivity: a review of personality, behavioral, and neurobiological assessment. Addict Res Theory. 2013 [epub ahead of print] doi:10.3109/16066359.2013.867432. [Google Scholar]
- 32.Gullo MJ, Loxton NJ, Dawe S. Impulsivity: Four ways five factors are not basic to addiction. Addict Behav. 2014 doi: 10.1016/j.addbeh.2014.01.002. [epub ahead of print] doi:10.1016/j.addbeh.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 33.Ginley MK, Whelan JP, Meyers AW, Relyea GE, Pearlson GD. Exploring a multidimensional approach to impulsivity in predicting college student gambling. J Gambl Stud. 2014;30:521–536. doi: 10.1007/s10899-013-9374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meda SA, Stevens MC, Potenza MN, Pittman B, Gueorguieva R, Andrews MM, et al. Investigating the behavioral and self-report constructs of impulsivity domains using principal component analysis. Behav Pharmacol. 2009;20:390–399. doi: 10.1097/FBP.0b013e32833113a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams L, Abdi H, French R, Orange J. A tutorial on Multi-Block Discriminant Correspondence Analysis (MUDICA): a new method for analyzing discourse data from clinical populations. J Speech, Lang Hearing Res. 2010;53:1372–1393. doi: 10.1044/1092-4388(2010/08-0141). [DOI] [PubMed] [Google Scholar]
- 36.Greenacre MJ. Correspondence analysis in practice. CRC Press; Boca Raton, FL: 2007. [Google Scholar]
- 37.Greenacre M, Blasius J. Multiple correspondence analysis and related methods. CRC Press; Boca Raton, FL: 2006. [Google Scholar]
- 38.Palombo DJ, Williams LJ, Abdi H, Levine B. The survey of autobiographical memory (SAM): a novel measure of trait mnemonics in everyday life. Cortex. 2013;49:1526–1540. doi: 10.1016/j.cortex.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 39.von Humboldt S, Leal I, Laneiro T, Tavares P. Examining Occupational Stress, Sources of Stress and Stress Management Strategies through the Eyes of Management Consultants: A Multiple Correspondence Analysis for Latent Constructs. Stress Health. 2013;29:410–420. doi: 10.1002/smi.2487. [DOI] [PubMed] [Google Scholar]
- 40.Dumais A, Potvin S, Joyal C, Allaire J-F, Stip E, Lesage A, et al. Schizophrenia and serious violence: a clinical-profile analysis incorporating impulsivity and substance-use disorders. Schizophrenia Res. 2011;130:234–237. doi: 10.1016/j.schres.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 41.Chan G, Gelernter J, Oslin D, Farrer L, Kranzler HR. Empirically derived subtypes of opioid use and related behaviors. Addiction. 2011;106:1146–1154. doi: 10.1111/j.1360-0443.2011.03390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pinkham AE, Sasson NJ, Beaton D, Abdi H, Kohler CG, Penn DL. Qualitatively distinct factors contribute to elevated rates of paranoia in autism and schizophrenia. J Abnorm Psychol. 2012;121:767–777. doi: 10.1037/a0028510. [DOI] [PubMed] [Google Scholar]
- 43.Filbey FM, Schacht JP, Myers US, Chavez RS, Hutchison KE. Marijuana craving in the brain. Proc Natl Acad Sci USA. 2009;106:13016–13021. doi: 10.1073/pnas.0903863106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schacht JP, Hutchison KE, Filbey FM. Associations between cannabinoid receptor-1 (CNR1) variation and hippocampus and amygdala volumes in heavy cannabis users. Neuropsychopharmacology. 2012;37:2368–2376. doi: 10.1038/npp.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Myers US, Hutchison KE, Filbey FM. Large variability in smokers obscure the G x E effects on tobacco dependence. Psychiatry Res. 2010;177:369–370. doi: 10.1016/j.psychres.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Filbey FM, Myers US, Dewitt S. Reward circuit function in high BMI individuals with compulsive overeating: similarities with addiction. Neuroimage. 2012;63:1800–1806. doi: 10.1016/j.neuroimage.2012.08.073. [DOI] [PubMed] [Google Scholar]
- 47.First M, Spitzer R, Williams J, Gibbon M. Structured Clinical Interview for DSM-IV-TR (SCID-I)-Research Version. Biometrics Research, New York State Psychiatric Institute; New York, NY: 2002. [Google Scholar]
- 48.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K-O. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 49.Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68:808–816. doi: 10.1001/archgenpsychiatry.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 51.R Core Team . R: a language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: [Last accessed 14 February 2014]. 2013. Available from: http://R-project.org. [Google Scholar]
- 52.Fox J, Weisberg S. An R companion to applied regression. 2nd ed Sage; Thousand Oaks, CA: 2011. [Google Scholar]
- 53.Beaton D, Fatt CRC, Abdi H. An ExPosition of multivariate analysis with the singular value decomposition in R. Computat Stat Data Analysis. 2014;72:176–189. [Google Scholar]
- 54.Lebart L, Morineau A, Warwick KM. Multivariate descriptive statistical analysis: correspondence analysis and related techniques for large matrices. Wiley; New York: 1984. p. 264. [Google Scholar]
- 55.Abdi H, Williams LJ, Valentin D. Multiple factor analysis: principal component analysis for multitable and multiblock data sets. Wiley Interdisciplinary Reviews: Computational Statistics. 2013;5:149–179. [Google Scholar]
- 56.Chernick MR. Bootstrap methods: A guide for practitioners and researchers. Wiley-Interscience; Hoboken, NJ: 2008. [Google Scholar]
- 57.Hesterberg T. Bootstrap. Wiley Interdisciplinary Reviews: Computational Statistics. 2011;3:497–526. [Google Scholar]
- 58.Berry KJ, Johnston JE, Mielke PW. Permutation methods. Wiley Interdisciplinary Reviews: Computational Statistics. 2011;3:527–542. [Google Scholar]
- 59.Abdi H, Dunlop JP, Williams LJ. How to compute reliability estimates and display confidence and tolerance intervals for pattern classifiers using the Bootstrap and 3-way multidimensional scaling (DISTATIS) NeuroImage. 2009;45:89–95. doi: 10.1016/j.neuroimage.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 60.McIntosh AR, Lobaugh NJ. Partial least squares analysis of neuroimaging data: applications and advances. Neuroimage. 2004;23:S250–S263. doi: 10.1016/j.neuroimage.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 61.Courtney KE, Arellano R, Barkley-Levenson E, Galvan A, Poldrack RA, MacKillop J, et al. The relationship between measures of impulsivity and alcohol misuse: an integrative structural equation modeling approach. Alcohol Clin Exp Res. 2012;36:923–931. doi: 10.1111/j.1530-0277.2011.01635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Conners CK, Staff M. Conners’ Continuous Performance Test II (CPT II V. 5) Multi-Health Systems Inc; North Tonawanda, NY: 2000. [Google Scholar]
- 63.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Motor Skills. 1958;8:271–276. [Google Scholar]
- 64.Reynolds B, Ortengren A, Richards JB, de Wit H. Dimensions of impulsive behavior: personality and behavioral measures. Personality Indiv Differences. 2006;40:305–315. [Google Scholar]
- 65.Lane SD, Cherek DR, Rhoades HM, Pietras CJ, Tcheremissine OV. Relationships among laboratory and psychometric measures of impulsivity: implications in substance abuse and dependence. Addictive Disord Their Treat. 2003;2:33–40. [Google Scholar]
- 66.Huba GJ, Newcomb MD, Bentler PM. Comparison of canonical correlation and interbattery factor analysis on sensation seeking and drug use domains. Appl Psycholog Measurement. 1981;5:291–306. [Google Scholar]
- 67.Tucker LR. An inter-battery method of factor analysis. Psychometrika. 1958;23:111–136. [Google Scholar]
- 68.Krishnan A, Williams LJ, McIntosh AR, Abdi H. Partial Least Squares (PLS) methods for neuroimaging: a tutorial and review. NeuroImage. 2011;56:455–475. doi: 10.1016/j.neuroimage.2010.07.034. [DOI] [PubMed] [Google Scholar]
- 69.Beaton D, Filbey FM, Abdi H. Integrating partial least squares correlation and correspondence analysis for nominal data. In: Abdi H, Chin W, Esposito Vinzi V, Russolillo G, Trinchera L, editors. New perspectives in partial least squares and related methods. Springer-Verlag; New York, NY: 2013. pp. 81–94. [Google Scholar]
- 70.Day AM, Metrik J, Spillane NS, Kahler CW. Working memory and impulsivity predict marijuana-related problems among frequent users. Drug Alcohol Depend. 2013;131:171–174. doi: 10.1016/j.drugalcdep.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gruber SA, Sagar KA, Dahlgren MK, Racine M, Lukas SE. Age of onset of marijuana use and executive function. Psychol Addictive Behav. 2012;26:496–506. doi: 10.1037/a0026269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Verdejo-García A, Del Mar Sánchez-Fernández M, Alonso-Maroto LM, Fernández-Calderón F, Perales JC, Lozano O, et al. Impulsivity and executive functions in polysubstance-using rave attenders. Psychopharmacology (Berl) 2010;210:377–392. doi: 10.1007/s00213-010-1833-8. [DOI] [PubMed] [Google Scholar]
- 73.Martinotti G, Carli V, Tedeschi D, Di Giannantonio M, Roy A, Janiri L, et al. Mono- and polysubstance dependent subjects differ on social factors, childhood trauma, personality, suicidal behaviour, and comorbid Axis I diagnoses. Addictive Behav. 2009;34:790–793. doi: 10.1016/j.addbeh.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 74.Perkins K, Lerman C, Coddington S, Jetton C, Karelitz J, Scott J, et al. Initial nicotine sensitivity in humans as a function of impulsivity. Psychopharmacology. 2008;200:529–544. doi: 10.1007/s00213-008-1231-7. [DOI] [PubMed] [Google Scholar]
- 75.Hogarth L, Stillwell DJ, Tunney RJ. BIS impulsivity and acute nicotine exposure are associated with discounting global consequences in the Harvard game. Human Psychopharmacol: Clin Experiment. 2013;28:72–79. doi: 10.1002/hup.2285. [DOI] [PubMed] [Google Scholar]
- 76.Schag K, Schönleber J, Teufel M, Zipfel S, Giel KE. Food-related impulsivity in obesity and Binge Eating Disorder – a systematic review. Obesity Rev. 2013;14:477–495. doi: 10.1111/obr.12017. [DOI] [PubMed] [Google Scholar]
- 77.Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52:430–436. doi: 10.1016/j.appet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 78.Dunne EM, Freedlander J, Coleman K, Katz EC. Impulsivity, expectancies, and evaluations of expected outcomes as predictors of alcohol use and related problems. Am J Drug Alcohol Abuse. 2013;39:204–210. doi: 10.3109/00952990.2013.765005. [DOI] [PubMed] [Google Scholar]
- 79.McHugh MJ, Demers CH, Braud J, Briggs R, Adinoff B, Stein EA. Striatal-insula circuits in cocaine addiction: implications for impulsivity and relapse risk. Am J Drug Alcohol Abuse. 2013;39:424–432. doi: 10.3109/00952990.2013.847446. [DOI] [PubMed] [Google Scholar]
- 80.Stanger C, Ryan SR, Fu H, Landes RD, Jones BA, Bickel WK, et al. Delay discounting predicts adolescent substance abuse treatment outcome. Experim Clin Psychopharmacol. 2012;20:205–212. doi: 10.1037/a0026543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Conner BT, Hellemann GS, Ritchie TL, Noble EP. Genetic, personality, and environmental predictors of drug use in adolescents. J Substance Abuse Treat. 2010;38:178–190. doi: 10.1016/j.jsat.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 82.Kendler KS, Schmitt E, Aggen SH, Prescott CA. Genetic and environmental influences on alcohol, caffeine, cannabis, and nicotine use from early adolescence to middle adulthood. Arch Gen Psychiatry. 2008;65:674–682. doi: 10.1001/archpsyc.65.6.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shin SH, Chung Y, Jeon S-M. Impulsivity and substance use in young adulthood. Am J Addictions. 2013;22:39–45. doi: 10.1111/j.1521-0391.2013.00324.x. [DOI] [PubMed] [Google Scholar]
- 84.Munafò MR, Flint J. Dissecting the genetic architecture of human personality. Trends Cognit Sci. 2011;15:395–400. doi: 10.1016/j.tics.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 85.Loth E, Carvalho F, Schumann G. The contribution of imaging genetics to the development of predictive markers for addictions. Trends Cogn Sci. 2011;15:436–446. doi: 10.1016/j.tics.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 86.Congdon E, Canli T. The endophenotype of impulsivity: reaching consilience through behavioral, genetic, and neuroimaging approaches. Behav Cogn Neurosci Rev. 2005;4:262–281. doi: 10.1177/1534582305285980. [DOI] [PubMed] [Google Scholar]
- 87.Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cognit Sci. 2012;16:81–91. doi: 10.1016/j.tics.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 88.Lombardo LE, Bearden CE, Barrett J, Brumbaugh MS, Pittman B, Frangou S, et al. Trait impulsivity as an endophenotype for bipolar I disorder. Bipolar Disord. 2012;14:565–570. doi: 10.1111/j.1399-5618.2012.01035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Heatherton TF, Wagner DD. Cognitive neuroscience of self-regulation failure. Trends Cognit Sci. 2011;15:132–139. doi: 10.1016/j.tics.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Whelan R, Conrod PJ, Poline J-B, Lourdusamy A, Banaschewski T, Barker GJ, et al. Adolescent impulsivity phenotypes characterized by distinct brain networks. Nat Neurosci. 2012;15:920–925. doi: 10.1038/nn.3092. [DOI] [PubMed] [Google Scholar]
- 91.Belcher AM, Volkow ND, Moeller FG, Ferré S. Personality traits and vulnerability or resilience to substance use disorders. Trends Cognit Sci. 18:211–217. doi: 10.1016/j.tics.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.