Abstract
Introduction
The Pediatric Assessment Triangle (PAT) is a rapid evaluation tool that establishes a child’s clinical status and his or her category of illness to direct initial management priorities. Recently the PAT has been incorporated widely into the pediatric resuscitation curriculum. Although intuitive, its performance characteristics have yet to be quantified. The purpose of this research is to determine quantitatively its accuracy, reliability, and validity as applied by nurses at triage.
Methods
In this prospective observational study, triage nurses performed the PAT on all patients presenting to the pediatric emergency department of an urban teaching hospital. Researchers performed blinded chart review using the physician’s initial assessment and final diagnosis as the criterion standard for comparison.
Results
A total of 528 children were included in the analysis. Likelihood ratios (LRs) were found for instability and category of pathophysiology using the PAT. Children deemed stable by initial PAT were almost 10 times more likely to be stable on further assessment (LR 0.12, 95% confidence interval [CI] 0.06-0.25). The PAT further specified categories of pathophysiology: respiratory distress (LR+ 4, 95% CI 3.1-4.8), respiratory failure (LR+ 12, 95% CI 4.0-37), shock (LR+ 4.2, 95% CI 3.1-5.6), central nervous system/metabolic disorder (LR+ 7, 95% CI 4.3-11), and cardiopulmonary failure (LR+ 49, 95% CI 20-120).
Discussion
The structured assessment of the initial PAT, as performed by nurses in triage, readily and reliably identifies high-acuity pediatric patients and their category of pathophysiology. The PAT is highly predictive of the child’s clinical status on further evaluation.
Keywords: Pediatric Assessment Triangle, PAT, Triage, Pediatric emergency medicine, Pediatric resuscitation, Evaluation of children
The Pediatric Assessment Triangle (PAT) generates a rapid, global assessment using only visual and auditory clues; it requires no equipment and takes seconds to perform.1-3 The PAT was designed to enable the provider to articulate formally a general impression of the child, establish the severity of the presentation and category of pathophysiology, and determine the type and urgency of intervention. Using the PAT, the provider makes observations of 3 components: appearance, work of breathing, and circulation to the skin (Figure 1).
FIGURE 1.
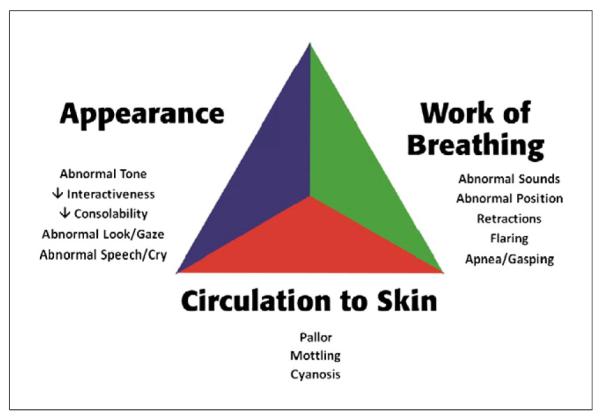
The Pediatric Assessment Triangle and its components.
Appearance is delineated by the “TICLS” mnemonic: Tone, Interactiveness, Consolability, Look or Gaze, and Speech or Cry. This arm of the PAT reflects a child’s age, stage of development, and ability to interact with the environment. Important clues such as the infant’s tone, consolability, interaction with caregivers and others, and strength of cry can inform the provider of the child’s appearance as normal or abnormal (for age and development).
Work of breathing describes the child’s respiratory status, especially the degree to which the child must work in order to oxygenate and ventilate. Clinical signs such as abnormal airway sounds (eg, stridor, grunting, and wheezing), abnormal positioning, retractions, or flaring of the nostrils on inspiration determine an abnormal/increased work of breathing.
Circulation to the skin reflects the general perfusion of blood throughout the body. The provider notes the color and color pattern of the skin and mucous membranes. In the context of blood loss/fluid loss or changes in venous tone, compensatory mechanisms shunt blood to vital organs such as the heart and brain and away from the skin and periphery of the body. By noting changes in skin color and skin perfusion (such as pallor, cyanosis, or mottling), the provider may recognize early signs of shock.
An abnormality noted in any of the arms of the PAT denotes an unstable child, that is, a child who will require some immediate clinical intervention. The pattern of affected arms within the PAT further categorizes the child into 1 of 5 categories: respiratory distress, respiratory failure, shock, central nervous system or metabolic disorder, and cardiopulmonary failure (Table 1). The specific category then dictates the type and urgency of intervention.
TABLE 1.
Components of the Pediatric Assessment Triangle and the general impression
| Appearance | Work of breathing | Circulation to skin | |
|---|---|---|---|
| Stable | Normal | Normal | Normal |
| Respiratory distress | Normal | Abnormal | Normal |
| Respiratory failure | Abnormal | Abnormal | Normal |
| Shock | Normal or Abnormal | Normal | Abnormal |
| Central nervous system/metabolic disturbance | Abnormal | Normal | Normal |
| Cardiopulmonary failure | Abnormal | Abnormal | Abnormal |
Adapted from Dieckmann RA, Brownstein D, Gausche-Hill M, eds. Pediatric Education for Prehospital Professionals: PEPP Textbook. Sudbury, MA: Jones & Bartlett Publishers; 2000.
Although the process is intuitive, we sought to evaluate quantitatively the accuracy, validity, and reliability of the general impression and the category of pathophysiology as utilized by experienced nurses in the triage of children. The PAT is meant to supply a common vernacular among clinicians; in this light, its performance characteristics also should be standardized.
Methods
STUDY DESIGN AND SETTING
This prospective observational study was conducted from August 17, 2005, through March 31, 2006, at a Los Angeles County teaching hospital. Approximately 23,000 patients per year are treated at the pediatric emergency department, with patients ranging in age from birth to 18 years. The study was approved by the Institutional Review Board with a waiver of consent.
STUDY PROTOCOL
Triage nurses were formally trained in the use of the PAT and were tested for competency by a written examination after a comprehensive multimedia lecture. During the study period, successfully trained nurses completed a PAT card separate from the medical record for all patients upon their initial presentation to the pediatric emergency department. Blank cards were included with each triage form to ensure compliance. Triage nurses noted PAT-specific findings and determined the general impression (as defined in Table 1). After completion in triage, cards were collected in a secured box. Exclusion criteria for analysis were patients who were 14 years or older, had a developmental delay, had congenital abnormality, were dependent on technology, had incomplete or unintelligible PAT cards, and had charts that could not be obtained for review. (Children with congenital abnormalities or a developmental delay have an abnormal baseline, and the PAT was not specifically designed for the rapid evaluation of these children with special needs.)
SAMPLE SIZE
Based on projected patient volumes, we chose a sample size of 25 patients per category and calculated the corresponding expected minimal detectable positive likelihood ratio (LR+ min) and the maximal detectable negative likelihood ratio (LR− max) with 95% confidence.4 This sample size ensured a minimum LR+ threshold of 2.8 (LR+ min ≥ 2.8) and a maximum LR− threshold of 0.4 (LR− max ≤ 0.4) in each category with 95% confidence.
MEASUREMENTS
Two pediatric emergency physicians and a pediatric nurse practitioner (PNP) who were blinded to the initial nursing triage assessment conducted a written chart review. A chart review was conducted on all unstable patients and on a random subset of stable patients as identified by the nurse at triage using the PAT. This subset consisted of the first 25 stable patients each month of the study duration. A list of eligible patients was generated by medical record number, date of birth, and date of visit. Investigators reviewed the chart for PAT-specific criteria and observations, thus reconstructing the physician’s PAT at the time of presentation.
DATA ANALYSIS
The physician’s chart-based PAT served as the criterion standard with which to compare the nurse’s initial PAT. Sensitivity, specificity, and positive and negative likelihood ratios were calculated (SAS software, version 9.2, SAS Institute Inc, Cary, NC, and VassarStats, Vassar College, Poughkeepsie, NY) for stability and for category of pathophysiology. The 3 chart reviewers extracted the PAT from the same 38 randomly chosen charts to measure inter-rater reliability (IRR; Fleiss’ κ coefficient). P values were calculated for Fleiss’ κ (A Language and Environment for Statistical Computing, version 2.11.0, R Foundation for Statistical Computing, Vienna, Austria). We used a bias-corrected resampling estimator5 (bootstrap) for constructing the 95% confidence interval around each κ statistic; 1000 repetitions of the bootstrap sample were used for each calculated interval (Stata Statistical Software, Release 11, StataCorp, College Station, TX).
Results
A total of 12,005 patients were triaged using the PAT. Of these patients, 1002 were selected for chart review (all 802 PAT-determined unstable patients and a sampling of 200 patients determined to be stable by PAT). We excluded from the analysis 474 patients who were missing exclusive patient and/or specific episode identifiers to ensure that the PAT card completed in triage corresponded to the exact ED episode; also excluded were children with repeat visits during the study period (Figure 2). The sample population is described in Table 2. Raw outcomes and sensitivity and specificity are reported in Table 3.
FIGURE 2.
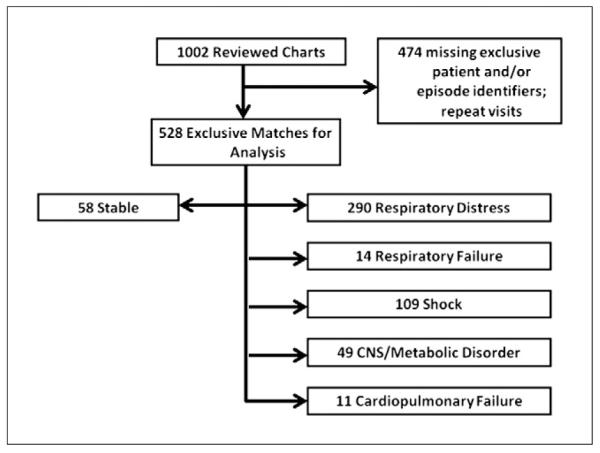
Patient eligibility and enrollment. CNS, Central nervous system.
TABLE 2.
Descriptive statistics of study patient population
| N | % | |
|---|---|---|
| Total | 528 | 100 |
| Gender | ||
| Male | 339 | 64 |
| Female | 189 | 36 |
| Age | ||
| 0 to 6 mo | 73 | 14 |
| 7 to 12 mo | 45 | 9 |
| 13 to 36 mo | 170 | 32 |
| 3 to 5 y | 70 | 13 |
| 6 to 10 y | 123 | 23 |
| 11 through 13 y | 47 | 9 |
| Emergency Severity Index triage levela | ||
| 1 | 89 | 17 |
| 2 | 284 | 54 |
| 3 | 140 | 27 |
| 4 | 14 | 3 |
| 5 | 0 | 0 |
| Ethnicity/race | ||
| African American | 88 | 17 |
| Asian | 23 | 4 |
| White | 20 | 4 |
| Hispanic | 392 | 74 |
| Other | 4 | 1 |
| Mode of arrival | ||
| Ambulance | 57 | 11 |
| Walk-in | 278 | 53 |
| Unknown | 193 | 37 |
| Assessed in | ||
| Triage | 297 | 56 |
| Room | 50 | 9 |
| Not specified | 181 | 34 |
| Disposition | ||
| Home | 410 | 78 |
| Ward | 59 | 11 |
| Step-down unit | 16 | 3 |
| Pediatric ICU | 40 | 8 |
| Transfer | 3 | 1 |
Triage level indicates 5-level Emergency Severity Index; 1 = highest (immediate life threat) and 5 = lowest (less urgent).
TABLE 3.
Test results, sensitivity, and specificity for Pediatric Assessment Triangle–defined category of illness
| N | TP | FP | TN | FN | Sensitivity % | 95% CI | Specificity % | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Instability | 58 | 292 | 178 | 50 | 8 | 97.3 | 94.6-98.8 | 22.9 | 17.0-30.0 |
| Respiratory distress | 290 | 224 | 66 | 216 | 22 | 91.1 | 86.6-94.2 | 76.6 | 71.1-81.3 |
| Respiratory failure | 14 | 3 | 11 | 505 | 9 | 25.0 | 6.7-57.2 | 97.9 | 96.1-98.9 |
| Shock | 109 | 20 | 89 | 412 | 7 | 74.1 | 53.4-88.1 | 82.2 | 78.5-85.4 |
| CNS/metabolic disturbance | 49 | 17 | 32 | 459 | 20 | 46.0 | 30.0-62.9 | 93.5 | 90.8-95.4 |
| Cardiopulmonary failure | 11 | 3 | 8 | 516 | 1 | 75.0 | 21.9-98.7 | 98.5 | 96.9-99.3 |
CI, Confidence interval; CNS, central nervous system; FN, false negatives; FP, false positives; N, number of subjects; TN, true negatives; TP, true positives.
Children found to be stable by PAT were 10 times more likely to be stable on final assessment (LR− 0.12, 95% confidence interval [CI] 0.06-0.25) (Table 4). The PAT predicted their category of pathophysiology: respiratory distress (LR+ 4, 95% CI 3.1-4.8), respiratory failure (LR+ 12, 95% CI 4.0-37), shock (LR+ 4.2, 95% CI 3.1-5.6), central nervous system/metabolic disorder (LR+ 7, 95% CI 4.3-11), and cardiopulmonary failure (LR+ 49, 95% CI 20-120).
TABLE 4.
Likelihood ratio performance for Pediatric Assessment Triangle–defined category of illness
| N | Positive LR (LR+) | 95% CI | Negative LR (LR−) | 95% CI | |
|---|---|---|---|---|---|
| Instability | 58 | 1.2 | 1.2-1.3 | 0.12b | 0.06-0.25 |
| Respiratory distress | 290 | 4.0a | 3.1-4.8 | 0.11b | 0.078-0.17 |
| Respiratory failure | 14 | 12.0¬*** | 3.7-36.7 | 0.80c | 0.55-1.06 |
| Shock | 109 | 4.2a | 3.1-5.6 | 0.32b | 0.17-0.60 |
| CNS/metabolic disturbance | 49 | 7.0a | 4.3-11.4 | 0.58 | 0.43-0.78 |
| Cardiopulmonary failure | 11 | 49.1c | 20.2-120.0 | 0.25c | 0.046-1.39 |
CI, Confidence interval; CNS, central nervous system; LR, likelihood ratio.
Meets LR+ 95% confidence threshold criterion (LR+ min ≥ 2.8).
Meets LR− 95% confidence threshold criterion (LR− max ≤ 0.4).
Does not meet sample size requirement.
The PAT performed better as a tool to identify pathophysiology than to exclude it entirely. The reliability of absence of findings to support absence of disease varied from reliable in respiratory distress (LR− 0.1, 95% CI 0.08-0.2) to unreliable in respiratory failure (LR− 0.8, 95% CI 0.6-1.1). That is, we found that a negative test for a specific PAT category did not reliably predict absence of an emergent condition (Table 4).
Inter-rater reliability (IRR) (Table 5) showed substantial agreement for stability (Fleiss’ κ = 0.7, P < .001). Specific categories of pathophysiology varied from fair agreement in shock (Fleiss’ κ = 0.32, P < .001) to substantial agreement in respiratory failure (Fleiss’ κ = 0.74, P < .001). IRR for respiratory distress was of borderline statistical significance (P = .08) in our sample; IRR for cardiopulmonary failure was not performed because of its rarity in the sample and the statistical limits of the calculation.
TABLE 5.
Inter-rater reliability of chart review for components of Pediatric Assessment Triangle and category of pathophysiology (N = 38; 3 raters)
| κ a | 95% CI | P value | |
|---|---|---|---|
| Component | |||
| Appearance | 0.70 | 0.51 to 0.88 | <.001 |
| Work of breathing | 0.24 | 0 to 0.48 | 0.01 |
| Circulation to skin | 0.32 | 0 to 0.49 | <.001 |
| Category of pathophysiology | |||
| Stable | 0.70 | 0.51 to 0.88 | <.001 |
| Respiratory distress | 0.16 | 0 to 0.49 | 0.08 |
| Respiratory failure | 0.74 | 0 to 1.00 | <.001 |
| Shock | 0.32 | 0 to 0.49 | <.001 |
| Central nervous system/metabolic disturbance | 0.68 | 0.51 to 0.88 | <.001 |
| Cardiopulmonary failure | N/Ab | N/A | N/A |
Fleiss’ κ coefficient: <0.00 poor; 0.00-0.20 slight; 0.21-0.40 fair; 0.41-0.60 moderate; 0.61-0.80 substantial; 0.81-1.00 almost perfect.4
N/A because of the rarity of the condition and limits of statistical calculation.
Discussion
In this prospective study, we found that the PAT accurately and reliably identifies acutely ill or injured infants and children in triage, as evidenced by a low negative LR for instability. Furthermore, the PAT reliably categorizes unstable children by pathophysiology as evidenced by high positive LRs for disease, thus aiding in identifying priorities of management. It therefore tends to “overtriage,” and it quickly identifies unstable children. Positive findings for a specific category of pathophysiology are helpful, but the absence of these findings for a given category does not rule out the condition. These performance characteristics are consistent with established triage scales.
The American College of Emergency Physicians and ENA published task-force recommendations (originally approved in 2003 and revised in 2010) to implement a “reliable, valid five-level triage scale such as the Emergency Severity Index (ESI)”.6,7 Other examples of 5-level triage scores include the Canadian Triage and Acuity Scale, the Manchester Triage Scale, and the Australasian (National) Triage Scale.8-10 These indices are algorithmic and take into account whether the patient is in extremis, the clinical context of presentation, the resources available, and vital signs.8-10 The aforementioned triage scales have been applied successfully to adults and children and are appropriate tools to apply to a broad population who present to the emergency department with a variety of signs and symptoms.11
These methods all have the dual strength and weakness of relying to some degree on symptomatology in triage. For example, eliciting a history in triage of a toxic ingestion would duly prompt a higher level of acuity for the “well-appearing ill” patient (over the “ill-appearing well” patient).12 Consonantly, a child may be unable to communicate his symptoms fully and clinicians may rely heavily on parents’ perceptions when assigning a triage category.13 History of present illness is important in triage but may not be complete or forthcoming initially.12 This factor may cause a delay or barrier in the proper understanding of the patient’s presentation and is problematic in the commonly used triage paradigms.
Haas14 outlined the ideal performance characteristics of a triage tool: It should be simple to use, accurate, rapid, reproducible, and discriminative to avoid potentially dangerous under-triage while appropriately assigning higher priority to patients with higher acuity. Moll11 reported that any commonly used triage system is based on expert opinion of physicians and ED nurses. This fact, in the high-acuity and high-uncertainty environment of the emergency department,12 underscores the importance of the proper use of any triage tool: to inform, not to decide.
In 2000, the American Academy of Pediatrics published Pediatric Education for Prehospital Providers, which introduced a new rapid assessment tool, called the Pediatric Assessment Triangle (PAT), to determine a child’s clinical status and category of illness.15 The use of the PAT in the emergency department was supported subsequently by the American College of Emergency Physicians and the American Academy of Pediatrics in the Advanced Pediatric Life Support course.16 The PAT is likewise included in the new version of the American Heart Association’s Pediatric Advanced Life Support course, as well as the ENA Emergency Nursing Pediatric Course.17,18 Although the PAT is widely taught, this study is the first to our knowledge to analyze the PAT quantitatively.
The PAT engages the clinician specifically in the visual14 and auditory (and therefore immediate) aspects of the initial evaluation. The PAT is not designed to be used as the sole independent triage tool; rather, it is meant to augment the full clinical impression. The main strength of the PAT is its ability to codify and communicate what would otherwise be deemed a “gut feeling.”
This last point deserves specific attention. History, when available, is often obtained through a third-party filter—the child’s caregiver. The child may be too young, frightened, or disabled to respond to questions.16 Vital signs—the cornerstones of adult assessment (and key to severity scores)—may be difficult to interpret because of age-based variation, lack of sensitivity (blood pressure), or poor specificity (heart rate, respiratory rate).1,2,19 This situation can complicate the goal of early recognition of and intervention in critical illness, especially in infants and children, who may compensate for their condition before a precipitous worsening in status.20-23 Furthermore, the PAT acts as a common language among providers and serves as a consistent metric in assessment and reassessment of the acutely ill or injured child.
LIMITATIONS
Due to missing exclusive patient and/or episode identifiers, as well as the goal to include one visit per patient, 474 patients were dropped from the analysis. Although the magnitude of excluded charts was not expected, this practice ensured certainty in matching the PAT triage cards with their corresponding ED visits. In addition, the decision to include one visit per patient avoids the possibility of confounding the dataset with repeated measures and intra-subject considerations in analysis.24,25
To evaluate the PAT in triage, we used the assessment closest in time to the triage PAT—the physician’s initial assessment. Although there is a potential lag time between triage assessment and initial physician assessment, the majority of our patients are triaged and sent to a room to be evaluated promptly by a physician or PNP. The triage and initial physician/PNP assessment, although not simultaneous, were as “clinically concurrent” as possible.
Since the sample of charts we reviewed was by design not representative of the population (all PAT-based unstable charts and a subset of the PAT-based stable charts were reviewed), we cannot report our findings in terms of positive predictive values or negative predictive values, which depend on the incidence of disease. Instead, we chose to report our results in LRs, which are a reflection of the performance of the test itself (calculated from sensitivity and specificity of the test). This procedure deemphasizes the population-based context (ie, positive predictive values and negative predictive values) and emphasizes the patient-based context (LR).
We did not meet our sample size requirement in the categories of respiratory failure and cardiopulmonary failure, because of excluded charts and the relative rarity of those conditions. Our study was not designed to evaluate children with congenital disorders or special health-care needs, because their appearance is abnormal at baseline.26
IMPLICATIONS FOR EMERGENCY NURSES
Emergency nurses can rely on the PAT as an objective early warning of children in or at high risk for clinical deterioration. It is especially helpful in cases when history and physical examination are limited. Furthermore, the PAT serves as a common vocabulary between health-care providers. A particularly powerful example of this benefit occurs in transfer of care, when the provider can replace subjective comments regarding clinical status with specific assessments of appearance, work of breathing, and circulation to the skin. The addition of the general impression (category of pathophysiology) serves as an adjunct in the communication of care and aids the receiving provider in determining reassessment and management priorities.
Conclusion
The PAT performed well in identifying stability in triage as evidenced by a significant negative likelihood ratio. Specific categories of pathophysiology varied in their strength of positive and negative LRs, limiting the use of the PAT alone to exclude an emergent condition. As a complement to established triage practices, the PAT can readily identify “red flags” for disease, especially when history is unavailable or limited.
Acknowledgments
We thank the nursing staff at Harbor–UCLA Medical Center for their cooperation in implementation of the study, Renee Sanchez-Durbin for her assistance in obtaining charts for review, and Heemun Kwok, MD, MS, for his assistance with inter-rater reliability calculations.
This project was supported in part by project 6H34MC08510 from the Maternal and Child Health Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services, entitled Evaluation of the Pediatric Assessment Triangle as an Assessment Tool for Children in the Prehospital Setting.
Contributor Information
Timothy Horeczko, Department of Emergency Medicine, Harbor-University of California, Los Angeles Medical Center, Torrance, CA; Investigator, Los Angeles Biomedical Research Institute, Torrance, CA; and Clinical Instructor of Medicine, Department of Medicine, David Geffen School of Medicine at the University of California, Los Angeles, CA..
Brianna Enriquez, Department of Emergency Medicine, Seattle Children’s Hospital, Seattle, WA..
Nancy E. McGrath, Department of Emergency Medicine, Harbor-University of California, Los Angeles Medical Center, Torrance, CA; Investigator, Los Angeles Biomedical Research Institute, Torrance, CA; and Lecturer, School of Nursing at the University of California, Los Angeles, CA..
Marianne Gausche-Hill, Division of Pediatric Emergency Medicine, and Director of Pediatric Emergency Medicine and EMS Fellowships, Department of Emergency Medicine, Harbor-University of California, Los Angeles Medical Center, Torrance, CA; Investigator, Los Angeles Biomedical Research Institute, Torrance, CA; and Professor of Clinical Medicine, Department of Medicine, David Geffen School of Medicine at the University of California, Los Angeles, CA..
Roger J. Lewis, Director of Research, and Research Fellowship Director, Department of Emergency Medicine, Harbor-University of California, Los Angeles Medical Center, Torrance, CA; Investigator, Los Angeles Biomedical Research Institute, Torrance, CA; and Professor of Medicine-in-Residence, Department of Medicine, David Geffen School of Medicine at the University of California, Los Angeles, CA..
REFERENCES
- 1.Dieckmann RD, Brownstein DR, Gausche-Hill M, Wiebe R, editors. Pediatric Education for Prehospital Professionals Instructor Toolkit. American Academy of Pediatrics and Jones & Bartlett Publishers; Sudbury, MA: 2005. [Google Scholar]
- 2.Dieckmann RA, Brownstein D, Gausche-Hill M. The Pediatric Assessment Triangle: a novel approach for the rapid evaluation of children. Pediatr Emerg Care. 2010;26:312–5. doi: 10.1097/PEC.0b013e3181d6db37. [DOI] [PubMed] [Google Scholar]
- 3.Ralston M, Hazinski MF, Zaritsky AL, Schexnayder SM, Kleinman ME, editors. PALS Course Guide. American Heart Association; Dallas, TX: 2007. [Google Scholar]
- 4.Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44(8):763–70. doi: 10.1016/0895-4356(91)90128-v. [DOI] [PubMed] [Google Scholar]
- 5.Reichenheim ME. Confidence intervals for the kappa statistic. Stata J. 2004;4(4):421–8. [Google Scholar]
- 6.Fernandes CMB, Tanabe P, Gilboy N, et al. Five-level triage: a report from the ACEP/ENA Five-Level Triage Task Force. J Emerg Nurs. 2005;31:39–50. doi: 10.1016/j.jen.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 7.American College of Emergency Physicians. Emergency Nurses Association . Joint Statement by the American College of Emergency Physicians (ACEP) and the Emergency Nurses Association (ENA): Triage Scale Standardization. American College of Emergency Physicians; Irving, TX: 2010. [Google Scholar]
- 8.Hohenhaus SM, Travers D, Mecham N. Pediatric triage: a review of emergency education literature. J Emerg Nurs. 2008;34:309–13. doi: 10.1016/j.jen.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 9.Considine J, LeVasseur SA, Charles A. Development of physiological discriminators for the Australasian Triage Scale. Accid Emerg Nurs. 2002;10:221–34. doi: 10.1016/s0965-2302(02)00156-x. [DOI] [PubMed] [Google Scholar]
- 10.van Veen M, Steyerberg EW, Ruige M, et al. Manchester triage system in paediatric emergency care: prospective observational study. BMJ. 2008;a1501:337. doi: 10.1136/bmj.a1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moll H. Challenges in the validation of triage systems at emergency departments. J Clin Epidemiol. 2010;63:384–8. doi: 10.1016/j.jclinepi.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Wolf L. Does your staff really “get” initial patient assessment? Assessing competency in triage using simulated patient encounters. J Emerg Nurs. 2010;36:370–4. doi: 10.1016/j.jen.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Baumann MR, Strout TD. Evaluation of the Emergency Severity Index (version 3) triage algorithm in pediatric patients. Acad Emerg Med. 2005;12:219–24. doi: 10.1197/j.aem.2004.09.023. [DOI] [PubMed] [Google Scholar]
- 14.Haas H. Outils de triage aux urgencies pédiatriques. Archives de Pédiatrie. 2005;12:703–5. doi: 10.1016/j.arcped.2005.04.048. [DOI] [PubMed] [Google Scholar]
- 15.Dieckmann RA, Brownstein D, Gausche-Hill M, editors. Pediatric Education for Prehospital Professionals: PEPP Textbook. Jones & Bartlett Publishers; Sudbury, MA: 2000. [Google Scholar]
- 16.Gausche-Hill M, Fuchs S, Yamamoto L, editors. Advanced Pediatric Life Support: The Pediatric Emergency Medicine Resource. American Academy of Pediatrics, American College of Emergency Physicians, and Jones & Bartlett Publishers; Sudbury, MA: 2003. [Google Scholar]
- 17.Ralston M, Hazinski MF, Zaritsky AL, Schexnayder SM, Kleinman ME, editors. PALS Provider Manual. American Heart Association; Dallas, TX: 2007. [Google Scholar]
- 18.Emergency Nurses Association [Accessed December 15, 2010];Emergency Nursing Pediatric Course. ENA Web site http://www.ena.org.
- 19.McCarthy PL, Lembo RM, Baron MA, Fink HD, Cicchetti DV. Predictive value of abnormal physical examination findings in ill-appearing and well-appearing febrile children. Pediatrics. 1985;76:167–71. [PubMed] [Google Scholar]
- 20.Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(suppl 3):S876–908. doi: 10.1161/CIRCULATIONAHA.110.971101. [DOI] [PubMed] [Google Scholar]
- 21.Hohenhaus S. Someone watching over me: observations in pediatric triage. J Emerg Nurs. 2006;32:398–403. doi: 10.1016/j.jen.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Center for Pediatric Emergency Medicine. New York University Langone Medical Center [Accessed December 15, 2010];Teaching Resource for Instructors in Prehospital Pediatrics. http://cpem.med.nyu.edu/teaching-materials.
- 23.Horeczko T, Gausche-Hill M. The Pediatric Assessment Triangle: a powerful tool for the prehospital provider. J Paramedic Pract. 2011;3(1) [Google Scholar]
- 24.Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 25.Obuchowski NA. Sample size calculations in studies of test accuracy. Stat Methods Med Res. 1998;7:371. doi: 10.1177/096228029800700405. [DOI] [PubMed] [Google Scholar]
- 26.Adirim T, Smith E, editors. Special Children’s Outreach and Prehospital Education (SCOPE) Jones & Bartlett Publishers; Sudbury, MA: 2007. [Google Scholar]


