Abstract
In most countries, the lack of explicit health workforce planning has resulted in imbalances that threaten the capacity of healthcare systems to attain their objectives. This has directed attention towards the prospect of developing healthcare systems that are more responsive to the needs and expectations of the population by providing health planners with a systematic method to effectively manage human resources in this sector. This review analyses various approaches to health workforce planning and presents the Six-Step Methodology to Integrated Workforce Planning which highlights essential elements in workforce planning to ensure the quality of services. The purpose, scope and ownership of the approach is defined. Furthermore, developing an action plan for managing a health workforce is emphasised and a reviewing and monitoring process to guide corrective actions is suggested.
Keywords: Health Workforce, organization and administration; Human Resources Development; Health Planning; Oman
According to a 2006 World Health Organization Report, health human resources (HHR), also known as human resources for health or the health workforce, are defined as “all people whose job is to protect and improve the health of their communities”.1 The term ‘workforce’, which aptly reflects the expanded roles and increased numbers of women in health professions, has replaced ‘manpower’ in order to denote the number of professionals available to provide services.2 These include the diverse clinical and non-clinical staff who implement individual and public health interventions.
The health workforce is an important component for the functioning and performance of labour-intensive healthcare systems.3 Workers are not just individuals, but integral parts of functioning healthcare teams in which each member contributes different skills and performs different functions.1 However, some countries facing health worker shortages have been reluctant to develop the detailed HHR policies or strategic plans that are necessary to guide and build the required human infrastructure of their health systems.4 For example, HHR planning has not succeeded in many African countries due to several factors, including insufficient balance between the plan and the planning process; lack of access to and use of planning methods and tools; lack of appropriate and accurate data; low stakeholder involvement in the planning process, and insufficient advocacy to attract resources for implementation.5 Such countries usually fail to adopt a planning method, depend essentially on introducing incremental changes in staffing on a year-to-year basis and use fixed standards combined with short-term adjustments to services and staffing in response to emerging health crises.6 In these cases, health systems usually operate without a targeted direction and the workforce is often unresponsive to the specific health needs and expectations of the community.
It is therefore important that national HHR policies and strategies are formulated using evidence-based planning in order to rationalise decisions regarding a country’s health workforce. Such plans can reduce workforce imbalances, strengthen the performance of staff and improve staff retention and adaptation to any major health sector reforms. In addition, they address the human resource development needs of priority health programmes and integrate them into a functional healthcare delivery system.6 A good example is the collaborative pan-Canadian Standards approach to HHR planning that was launched in 2004 and 2005 to support effective coordination and collaborative HHR planning across the country.7 In this approach, each jurisdiction in Canada determines the scope of their delivery system, their present and future needs and the type of service delivery models that would best meet their population’s needs. The jurisdictions are then able to more accurately determine their HHR requirements. However, this will occur within the context of a larger system that shares information and works collaboratively to develop the optimum combination and number of providers to meet all of the jurisdictions’ needs.7
This type of planning provides an opportunity to identify the services needed, innovative ways to deliver those services, the types of professionals required and how to deploy them and make the best use of their skills. This stands in contrast to a planning method based solely on how services are currently delivered and by whom.8 In addition, the health workforce planning model currently utilised in the Netherlands since 2002 has been successful in achieving equilibrium in the labour market, taking into account the qualitative fit between supply and demand. In this respect, both policymakers and stakeholders in the Netherlands have accepted the health workforce planning system and the model.3
The aim of this review is to highlight the importance of health workforce planning and to describe available models and methods. In addition, this review will examine the extent to which health workforce planning processes have been successful in reaching a balance between supply and demand, both internationally and in Oman. A selected collaborative approach for HHR planning and management that can be adapted to local circumstances, the Six-Step Methodology for Workforce Planning, is also presented. This approach can assist in the delivery of healthcare projects or programmes by considering both the number of workers needed and the characteristics desired in a workforce in order to improve access to and quality of healthcare services.9
Imbalances in Health Workforces
In contrast to effective workforce planning, imbalances in the health workforce represent a major challenge for health policymakers and hinder effective planning. Imbalances between available inputs and requirements characterise health systems in both developed and developing countries; however, they are often more visible in the latter, perhaps due to a lack of management and insufficient financial resources to attract qualified health professionals from other countries.6
Usually, all health workforce assessments begin with an estimation of the current number of physicians in the workforce. Indications of a shortage in this category depend on economic and demographic trends that impact the current supply of physicians, as well as estimates from databases of physicians and surgical organisations.10,11 Another approach to health workforce assessment involves the estimation of regional or national training needs and the competencies of local public health workers.12 However, many studies have revealed barriers to the success of workforce surveys and training initiatives. These limitations include a lack of organisational support; low response rates;13 the need for intensive follow-up to increase response rates; limited training time and resources,14 and non-representative or role-limited responses. Given these obstacles, very few comprehensive surveys of health workforces have been conducted at any level in order to assess the workforce.15
Geographical Imbalances
The unbalanced distribution of the health workforce within countries is a global problem that often results in great disparities in health outcomes between rural and urban populations. This imbalance may be explained economically, as a disequilibrium between labour supply and demand in a given geographic area, and normatively, as differences in staff density resulting from a given standard or social norm.16,17 A needs-based analysis alone does not consider the full labour market for health workers. From a demand perspective, three major sectors that utilise health workers also shape health worker labour markets: public, private and donor sectors. Government structures also influence the health worker market by setting rules and establishing the role of public policy in enabling the market to function.18 Other determinants that affect geographical distribution are the individual and organisational factors related to healthcare and educational systems, institutional structures and the broader sociocultural environment.
Role of the Government
Worldwide, governments continue to be the principal employers in the health sector, despite a tendency to give increasingly greater scope to the private sector in the provision of healthcare services.17 Many countries, however, lack the human resources needed to deliver essential health interventions for a number of reasons, including limited production capacity, migration of health workers within and across countries, poor combination of skills and demographic imbalances. The formulation of national policies and plans in pursuit of human resources for health development objectives requires sound information and evidence. Against the backdrop of an increasing demand for information, building knowledge and databases on the health workforce requires coordination across many sectors.19
Health Workforce Planning
Effective workforce planning has been defined as “the timely anticipation of potential future imbalances between the supply and demand of skills, enabling action”1 or as “the systematic assessment of future human resource needs and the determinations of the actions required to meet those needs”.20 These definitions reflect the challenge of translating an organisation’s plans and objectives into scheduling requirements; while human resources are considered to be the most valuable component of this process, they are nevertheless also the most volatile and potentially unpredictable.
Research has shown that it is the role of health planners to ensure that the right number of healthcare workers with the right knowledge, skills, attitudes and qualifications are performing the correct tasks in the right place at the appropriate time in order to achieve predetermined health targets.1,21 However, planning the health workforce is not only a technical process; demographic and epidemiological transitions drive changes in population-based health threats and the workforce must respond to these. Also, financing policies, technological advances and consumer expectations can dramatically shift demands of the workforce in health systems. Furthermore, workers usually seek opportunities and job security in dynamic health labour markets that are part of the global political economy.1 Such factors affect the ways in which workers are recruited, deployed, trained and made redundant.
Consequently, it has become a major challenge for policy makers to avoid these cyclic variations between shortages and surpluses of healthcare personnel.3 In this way, one of the roles of the HHR planning process is to seek a balance or to address the mismatches between available human resources and the actual requirements for delivering quality health services.21 Therefore, a basic workforce planning model consists of analyses in four key areas: supply, demand, gap and solution.
Supply analysis focuses on identifying organisational competencies, analysing staff demographics and determining employment trends.22 Demand analysis measures future activities and workloads, describes the required competencies of the future workforce and quantifies the impact of changes in work arising from technological or other sources.23 Gap analysis is an evaluation in which the supply and demand analyses are compared to understand differences between the current and future workforces. This likely results in one of two scenarios—the current number of workers or competencies in the workforce will not meet future needs (e.g. demand exceeds supply) or the current number of workers or competencies exceed future needs (e.g. supply exceeds demand).23 The solution analysis therefore strives to develop strategies to close the identified competency gaps and curtail surpluses.23
In order to estimate HHR supply and requirements, four types of approaches have been traditionally described: needs-based, utilisation or demand-based, health workforce to population ratio and target-setting.24,25 The difference between these approaches depends on the way that the required health services are identified. These may be based on the health needs of the population, while others are based on the current level of technology being utilised in health facilities. Moreover, methods may be based on a population’s demand for certain services and the various health services that are already provided, while others focus on meeting the population’s current health needs or work on projections of future requirements based on expected changes in population structure.24,26
Each of the above-described planning approaches have advantages and limitations. Problems in securing data are invariably encountered and some compromises have to be made with respect to the degree of precision with which the variables are specified.6 With the exception of the health workforce to population ratios approach, these methods seek to translate the required number and types of health services into time estimates. These estimates are then expressed as full-time equivalents of health personnel, using norms and standards on the actual productive time.21 It is also important for health system planners and managers to determine which variables are the dominant ones in any consideration of future requirements.6
Context in Oman
In Oman, human resources development in the area of healthcare has been a strategical priority for the past few decades.27 However, it was only in 1976 that the government of Oman began using health workforce planning to set staffing levels. Until 1990, this planning was erratic, locally based and poorly supported by a cohesive health information system. Periodically, the Ministry of Health (MOH) intervened with emergency measures in reaction to health workforce shortages, such as facilitating and accelerating administrative processes to recruit expatriate health workers already present in Oman, sponsoring partners of employed workers or attracting health workers from neighbouring countries.28 The MOH also implemented training and reorientation for existing healthcare staff to improve their skill levels, motivation and retention as well as increasing remuneration to encourage staff to work for extra hours or carry out additional tasks.29
In 1991, systematic health workforce planning began and the MOH adopted a rational staffing policy. This entailed staffing of healthcare institutions based on workload-cum-allocation considerations.28 Staffing norms were fixed in 1998 for most health centres and local hospitals in light of nationwide institutional surveys.30 The MOH also issued a set of guidelines for staffing primary healthcare institutions.31 Periodical reviews and adjustments of the staffing process in these institutions using computer-based hospital workforce planning models were conducted annually. In light of these reviews, planners came up with user-friendly staffing patterns for health centres and local hospitals. In 2006, they designed a simple classification of the health centres and local hospitals and proposed staffing norms for each type of facility.32 Planning for the recruitment and deployment of the health workforce in regional and referral hospitals was determined on a top-down basis using workload measurement tools or relying on professional judgments.
An alternative approach was to use research findings, where available, to develop the best doctor/nurse to patient ratios in particular services.28 Despite the validity of fixing certain optimum staff to patient ratios, it was often difficult to estimate the required numbers and allocate enough staff to each public hospital.33 In the light of the current situation in Oman, the methodology described below is suggested for implementation in the country.
The Six-Step Methodology for Workforce Planning
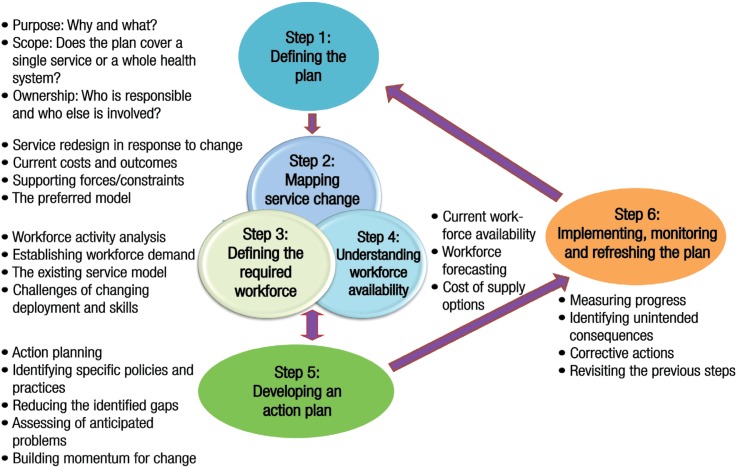
In the past, many countries have experienced limited success in planning and implementing HHR strategies.13–15 The risk of facing a potential HHR crisis has necessitated rethinking methods of health workforce planning. Accordingly, new service delivery models were suggested to encourage healthcare providers to work collaboratively and to the full scope of their practice. The Six-Step Methodology to Integrated Workforce Planning was developed by Skills for Health, a workforce projects team in the UK.34 It is a systematic practical approach that supports the delivery of quality patient care, productivity and efficiency, while ensuring that workforce planning decisions are sustainable and realistic.34 The methodology identifies the elements necessary for any workforce plan, taking into account the current and future demand for healthcare services, the local demographic situation and the impact on other services, while helping planners to cope with budgetary constraints [Figure 1]. Each of the six steps are described in more detail below.
Figure 1:
Health workforce planning cycle according to the Six-Step Methodology for Workforce Planning.34
Defining the Plan
In this step, planners identify why a workforce plan is needed and for whom it is intended by defining its purpose, scope and ownership.35 Workforce planners must be clear about the intended use of the plan and why it is required. The scope of the plan must be determined, including whether it will cover a single service area, a particular patient pathway or an entire nation-wide health system. Given this, it must also be apparent who will be responsible for ensuring the plan is delivered and who will be involved in the planning process.9
Mapping Service Change
This is the first of three interrelated steps. This second step involves the process of service redesign in response to patient choice, changes in modes of delivery, advances in care or financial constraints. Planners must be very clear about current costs and outcomes and should identify the intended benefits of any changes to healthcare services. Planners should also identify forces that may support or hamper each change. Additionally, there must be a clear statement about how the preferred model is more effective in delivering the desired benefits, given anticipated constraints.9
Defining the Required Workforce
Having established the foundations of the plan and the preferred programme model, planners must assess the workforce and appropriate skills that will be needed for delivery. This will require some consideration of both the key tasks undertaken by HHR and the skills needed to deliver these, along with an analysis of the levels of activity expected through the programme.36
Determining the types and number of workers needed is known as establishing the workforce demand. This must be performed as part of wider service and financial planning processes. Therefore, in order to estimate workforce demand, planners must consider their existing service model and the challenges of changing it with regards to deployment and required skills.37
Understanding Workforce Availability
This step involves describing the existing workforce in the areas under consideration and the existing skills and deployment, as well as assessing any problem areas arising from age profile or turnover. It may be the case that the ready availability or shortage of staff with particular skills contributes to the service redesign and that steps two and three will need to be revisited. Consideration should be given to the practicalities and cost of any retraining, redeployment and/or recruitment activities that could increase or change the workforce supply.9
Developing an Action Plan
With regard to the previous three steps and after determining the most effective way of ensuring the availability of staff to deliver the redesigned services, planners should develop a plan for delivering the appropriate number of staff with required skills.9 Planners should also identify specific policies and practices for acquiring, developing, assessing, rewarding and distributing the workforce as necessary to close any existing gaps in service. These policies and practices should be sufficiently specific to the required workforce and should enable the management of any future changes. At this stage, planners must also estimate the potential effects of the identified policies and practices in reducing identified gaps and any requirements for new or modified resources and authority procedures for their implementation.35,38 Planners should also include an assessment of anticipated problems and methods for overcoming these, including clinical engagement.9
Implementing, Monitoring and Refreshing the Plan
After the plan is launched, periodic review and adjustment are essential. To enable this, the plan should be explicit about how success will be measured. In addition, any unintended consequences of changes need to be identified so that corrective actions can be taken.9 Planners also need to put in place a reviewing and monitoring process so that they can update the plan according to the changing workforce needs of the project or programme.36
It is worthwhile to mention that, although the six steps presented above are in numerical order, the process of workforce planning is in itself cyclical and not linear.36 Accordingly, workforce planners may find themselves revisiting previous steps as they work through the methodology and when new information comes to light after the plan is implemented.
Conclusion
HHR planning occurs within a health system and is driven by the design and models of health service delivery. These are, in turn, based on a population’s health needs. For the success of any healthcare delivery system, workforce planners must continually assess the impact of service design decisions on human resources and make adjustments or corrections as required. Workforce planners must be clear about what they expect to achieve through collaborative HHR planning. Their objective should allow the development and maintenance of a health workforce with the skills to support the service delivery system and allow patients timely access to high-quality, effective and safe health services. Management decisions must be made regarding which HHR model is preferable. In order to ensure a greater capacity for influencing factors affecting HHR roles and work, the Six-Step Methodology to Integrated Workforce Planning is highly recommended for workforce planners in Oman and other developing countries.
References
- 1.World Health Organization. Working together for health: The World Health Report. 2006. From: www.who.int/whr/2006/whr06_en.pdf?ua=1 Accessed: May 2014. [Google Scholar]
- 2.Robiner WN. The mental health professions: Workforce supply and demand, issues, and challenges. Clin Psych Rev. 2006;26:600–25. doi: 10.1016/j.cpr.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Van Greuningen M, Batenburg RS, Van der Velden LF. Ten years of health workforce planning in the Netherlands: A tentative evaluation of GP planning as an example. Hum Resour Health. 2012;10:21. doi: 10.1186/1478-4491-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adano U. Collection and Analysis of Human Resources for Health (HRH) Strategic Plans. From: www.capacityproject.org/images/stories/files/resourcepaper_strategicplans.pdf Accessed: May 2014.
- 5.Nyoni J, Gbary A, Awases M, Ndecki P, Chatora R, World Health Organization Regional Office for Africa Policies and Plans for Human Resources for Health: Guidelines for countries in the WHO African region. From: www.who.int/workforcealliance/knowledge/toolkit/15.pdf Accessed: May 2014.
- 6.World Health Organization. Human Resources for Health Observer Issue no. 3: Models and tools for health workforce planning and projections. From: www.whqlibdoc.who.int/publications/2010/9789241599016_eng.pdf Accessed: May 2014.
- 7.Health Canada. Health Care System: Health human resource strategy (HHRS) From: www.hc-sc.gc.ca/hcs-sss/hhr-rhs/strateg/index-eng.php Accessed May 2014.
- 8.Federal/Provincial/Territorial Advisory Committee on Health Delivery and Human Resources (ACHDHR) A Framework for Collaborative Pan-Canadian Human Health Resources Planning. From: www.hc-sc.gc.ca/hcs-sss/alt_formats/hpb-dgps/pdf/pubs/hhr/2007-frame-cadre/2007-frame-cadre-eng.pdf Accessed: May 2014.
- 9.National Health Service. Step-by-step: A guide to planning a portfolio programme and project management team. From: www.systems.hscic.gov.uk/p3m/resource/development/example/planteam.pdf Accessed: May 2014.
- 10.Zurn P, Dal Poz MR, Stilwell B, Adams O. Imbalance in the health workforce. Hum Resour Health. 2004;2:13. doi: 10.1186/1478-4491-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper RA, Getzen TE, McKee HJ, Laud P. Economic and demographic trends signal an impending physician shortage. Health Aff (Millwood) 2002;21:140–54. doi: 10.1377/hlthaff.21.1.140. [DOI] [PubMed] [Google Scholar]
- 12.Alejos A, Weingartner A, Scharff DP, Ablah E, Frazier L, Hawley SR, et al. Ensuring the success of local public health workforce assessments: Using a participatory-based research approach with a rural population. Public Health. 2008;122:1447–55. doi: 10.1016/j.puhe.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Acquilla S, O’Brien M, Kernohan E. ‘Not too much, not too little, but just enough?’: Observations on continuing professional development in public health in the north of England. Public Health. 1998;112:211–25. doi: 10.1016/S0033-3506(98)00234-0. [DOI] [PubMed] [Google Scholar]
- 14.Freudenstein U, Yates B. Public health skills in primary care in South West England: A survey of training needs, obstacles and solutions. Public Health. 2001;115:407–11. doi: 10.1038/sj.ph.1900805. [DOI] [PubMed] [Google Scholar]
- 15.Lawlor DA, Morgan K, Frankel S. Caring for the health of the public: Cross sectional study of the activities of UK public health departments. Public Health. 2002;116:102–5. doi: 10.1038/sj.ph.1900820. [DOI] [PubMed] [Google Scholar]
- 16.Dussault G, Franceschini MC. Not enough there, too many here: Understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4:12. doi: 10.1186/1478-4491-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dussault G, Dubois CA. Human resources for health policies: A critical component in health policies. Hum Resour Health. 2003;1:1. doi: 10.1186/1478-4491-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soucat A, Scheffler R. The Labour Market for Health Workers in Africa: A new look at the crisis. From: www.openknowledge.worldbank.org/bitstream/handle/10986/13824/82557.pdf?sequence=5 Accessed: May 2014.
- 19.World Health Organization. Human Resources for Health: Toolkit on monitoring health systems strengthening. From: www.who.int/healthinfo/statistics/toolkit_hss/EN_PDF_Toolkit_HSS_HumanResources_oct08.pdf Accessed: May 2014.
- 20.Ripley DE. Workforce: How to determine future workforce needs. From: www.workforce.com/articles/how-to-determine-future-work-force-needs Accessed: May 2014.
- 21.Dreesch N, Dolea C, Dal Poz MR, Goubarev A, Adams O, Aregawi M, et al. An approach to estimating human resource requirements to achieve the Millennium Development Goals. Health Policy Plan. 2005;20:267–76. doi: 10.1093/heapol/czi036. [DOI] [PubMed] [Google Scholar]
- 22.Young M, Canadian Paediatric Society Human Resource Services, Center for Organizational Research The Aging and Retiring Government Workforce. From: www.accenture.com/SiteCollectionDocuments/PDF/CPS_AgeBubble_ExecutiveSummary.pdf Accessed: May 2014.
- 23.Rayner S. Business Blogs: Workforce planning - balancing demand and supply. From: www.businessblogshub.com/2012/10/workforce-planning-balancing-demand-and-supply/ Accessed: May 2014.
- 24.Hall TL, Mej’ia A, World Health Organization Health Manpower Planning: Principles, methods, issues. From: apps.who.int/iris/handle/10665/40341 Accessed: May 2014.
- 25.Markham B, Birch S. Back to the future: A framework for estimating health-care human resource requirements. Can J Nurs Adm. 1997;10:7–23. [PubMed] [Google Scholar]
- 26.Hornby P, Ray DK, Shipp PJ, Hall TL. Guidelines for Health Manpower Planning: A course book. From: www.whqlibdoc.who.int/publications/9241541563_%28p1-p188%29.pdf Accessed: May 2014.
- 27.Alshishtawy M. Medical specialties in Oman: Scaling up through national action. Oman Med J. 2009;24:279–87. doi: 10.5001/omj.2009.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alshishtawy MM. Nursing staffing in Oman: An approach for estimating the requirements of the 8th health system. Sultan Qaboos Univ Med J. 2012;12:258. [Google Scholar]
- 29.Ghosh B. Health workforce development planning in the Sultanate of Oman: A case study. Hum Resour Health. 2009;7:47. doi: 10.1186/1478-4491-7-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghosh B. Review of hospital bed capacity in Oman: An exploratory study. Muscat, Oman: Ministry of Health; 1999. pp. 1–56. [Google Scholar]
- 31.Oman Ministry of Health. Guidelines for Staffing Primary Health Care Institutions. Muscat, Oman: Ministry of Health; 1998. pp. 1–3. [Google Scholar]
- 32.Ghosh B. Staffing Norms Primary Health Care Institutions: A technical appendix to the 7th five-year human resources development plan. Muscat, Oman: Ministry of Health; 2006. pp. 1–21. [Google Scholar]
- 33.Oman Ministry of Health. The Human Resources Development Plan: 7th Five-year Health Development Plan (2006–2010) Muscat, Oman: Ministry of Health; 2006. pp. 20–4. [Google Scholar]
- 34.Skills for Health. Six Steps Methodology to Integrated Workforce Planning. From: www.clph.net/writedir/5ec5Six%20Steps%20Refresh.pdf Accessed: May 2014.
- 35.Po T. Getting it Right: A workforce planning approach. From: www.tepou.co.nz/library/tepou/getting-it-right-a-workforce-planning-approach Accessed: May 2014.
- 36.Health Service Journal. Six Steps to Integrated NHS Workforce Planning: Step three. From: www.hsj.co.uk/resource-centre/six-steps-to-integrated-nhs-workforce-planning-step-three/1921079.article#.U4xdZvmSxic Accessed: May 2014.
- 37.Brown JS, Learmonth A. Mind the gap: Developing the PH workforce in the North East and Yorkshire and Humber regions: A scoping stakeholder study. Public Health. 2005;119:32–8. doi: 10.1016/j.puhe.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 38.Emmerichs RM, Marcum CY, Robbert AA. An Operational Process for Working Force Planning. From: www.rand.org/content/dam/rand/pubs/monograph_reports/2005/MR1684.1.pdf Accessed: May 2014.