Abstract
Objectives:
This study aimed to investigate trends in the estimated 10-year risk for developing cardiovascular disease (CVD) among adults with diagnosed diabetes in Oman. In addition, the effect of hypothetical risk reductions in this population was examined.
Methods:
Data from 1,077 Omani adults aged ≥40 years with diagnosed diabetes were collected and analysed from three national surveys conducted in 1991, 2000 and 2008 across all regions of Oman. The estimated 10-year CVD risk and hypothetical risk reductions were calculated using risk prediction algorithms from the Systematic COronary Risk Evaluation (SCORE), Diabetes Epidemiology Collaborative Analysis of Diagnostic Criteria in Europe (DECODE) and World Health Organization/International Society of Hypertension (WHO/ISH) risk tools.
Results:
Between 1991 and 2008, the estimated 10-year risk of CVD increased significantly in the total sample and among both genders, regardless of the risk prediction algorithm that was used. Hypothetical risk reduction models for three scenarios (eliminating smoking, controlling systolic blood pressure and reducing total cholesterol) identified that reducing systolic blood pressure to ≤130 mmHg would lead to the largest reduction in the 10-year risk of CVD in subjects with diabetes.
Conclusion:
The estimated 10-year risk for CVD among adults with diabetes increased significantly between 1991 and 2008 in Oman. Focused public health initiatives, involving recognised interventions to address behavioural and biological risks, should be a national priority. Improvements in the quality of care for diabetic patients, both at the individual and the healthcare system level, are required.
Keywords: Risk Assessment, Risk Reduction Behavior, Trends, Diabetes Mellitus, Cardiovascular Disease, Oman
Advances in Knowledge
- Utilising data from three large cross-sectional surveys conducted in Oman, this study shows that the nationwide population-based 10-year risk of cardiovascular disease (CVD) has increased over the last two decades among Omani diabetic patients who were reportedly free of CVD at the time they were surveyed.
Application to Patient Care
- This study demonstrates that controlling systolic hypertension among diabetic patients will lead to the greatest 10-year risk reduction of CVD among this group, in comparison to the elimination of smoking or the reduction of cholesterol.
- The results of this study may help to improve the evaluation and management of patients with diabetes within the Omani healthcare system.
Cardiovascular disease (CVD) is a major cause of morbidity and mortality in people with diabetes mellitus, accounting for at least 50% of all diabetes-related disabilities and fatalities in most populations.1,2 Strokes, all manifestations of acute coronary syndrome and sudden death are at least twofold more common in people with type 2 diabetes than in non-diabetic individuals.3 Furthermore, over 80% of diabetes-related deaths occur in low- and middle-income countries, thus posing a major threat to public health in most developing countries.4,5 In addition, the Arabian Peninsula has a higher percentage of excess deaths attributable to diabetes (9%) in comparison to North American (8.5%) or African countries (2.4%).6 The diabetes epidemic is sweeping across the Middle East; five of the top 10 globally ranked countries for diabetes prevalence in 2010 were countries in the Arabian Peninsula.7 Thus, a surge in mortality attributed to CVD is expected in such high-risk populations. Despite the gravity of this situation, only limited evidence is available regarding the trends in CVD risk factors among Arab populations in this region, including one review on nutrition-related non-communicable diseases.8
The aim of the current study was to investigate temporal trends in the estimated 10-year risk of developing CVD among adults with diagnosed diabetes in Oman over the past two decades. In addition, this study examined the effect of hypothetical risk reductions in this population.
Methods
This study used data from three population-based national surveys conducted in Oman in 1991, 2000 and 2008.9–11 Each survey was designed to include a nationally representative sample from all 11 administrative regions of Oman based on census enumeration strategies. Additionally, the surveys used multi-stage stratified cluster sampling techniques. In 1991, participants were interviewed at home and then asked to visit the nearest hospital or health centre within the following 72 hours after fasting overnight for at least eight hours. At the hospital/health centre, the participants then underwent various examinations and provided fasting venous blood samples. For the 2001 and 2008 surveys, a trained team collected early morning blood samples from survey participants following an interview at home.
Investigations were conducted as follows. For the 1991 and 2000 surveys, blood pressure (BP) was measured 10 minutes after the subject was seated using a mercury sphygmomanometer on the upper arm, while the 2008 survey used a digital sphygmomanometer applied to the wrist. In all three surveys, three readings were taken and the average recorded as the final reading. Blood samples for measuring glucose levels and cholesterol were collected in sodium fluoride oxalate anticoagulant and lithium heparin anticoagulant containers, respectively. In the 1991 survey, serum glucose and cholesterol were measured using a Synchron CX7 biochemistry analyser (Beckman Coulter, Inc., Brea, California, USA), while the 2000 and 2008 surveys used the Hitachi 911, 912 or 902 automated chemistry analysers (Boehringer Ingelheim GmbH, Ingelheim am Rhein, Germany). All machines were used as per their instructions and proprietary reagents were supplied by the manufacturers. In the 1991 survey, all samples were collected and transferred for analysis in a central tertiary hospital. In the 2000 and 2008 surveys, samples from each region were analysed in the local regional referral hospital. No attempt was made to assess the effect of methodology changes in the measured biochemical parameters between the three survey periods or between hospitals within the same survey. However, for the 2000 and 2008 surveys, all laboratories used the same methods and machines and applied the same internal and external quality control measures.
A diagnosis of diabetes among the participants was based on an oral glucose tolerance test (OGTT) in the 1991 survey and fasting plasma glucose (FPG) values in the 2000 and 2008 surveys using the 1999 diagnostic criteria recommended by the World Health Organization (WHO).12 Subjects were also classified as having diabetes if they reported a previous diagnosis of diabetes by a physician, regardless of their OGTT results or FPG values. Current smokers included participants smoking any type of tobacco at the time of the survey.
Total/absolute 10-year CVD risk estimates were calculated for diabetic subjects who reported that they had never been diagnosed with a heart condition or heart disease by a physician. These estimates were calculated using three gender-specific tools: the Systematic COronary Risk Evaluation (SCORE), the Diabetes Epidemiology Collaborative Analysis of Diagnostic Criteria in Europe (DECODE) and the joint WHO/International Society of Hypertension (ISH) risk prediction chart.13–15 These tools were selected because the risk calculation formulae used were readily available and because the variables required had been measured and collected during the three national surveys. Since two of the three tools (SCORE and WHO/ISH charts) were directed towards subjects aged ≥40 years, the risk estimates for this study were also calculated using a cohort of the same age.
All three tools incorporated age, gender, current smoking and diabetic status, systolic BP (SBP) and total cholesterol (TC) to estimate 10-year CVD risk (except SCORE which did not include diabetic status). SCORE and DECODE published equations; thus calculated estimates using these tools were presented as mean CVD risk over a 10-year period. Conversely, WHO/ISH risk prediction charts were published according to incremental risk categories and estimates were therefore presented as proportions of subjects with ≥30% risk over 10 years. Since WHO/ISH charts were developed to be region-, country- and income-specific, the Eastern Mediterranean Region charts in category B were utilised as Oman falls within this regional and income category.15
Tests for linear trends in CVD risk were conducted using logistic regression analyses, in which the survey period was used as a continuous independent variable and 10-year CVD risk as the dependent variable. Hypothetical estimates of 10-year risk reduction for adults with diabetes were calculated using all three risk tools and under the following scenarios: eliminating all current smoking; reducing systolic BP to <130 mmHg for subjects with a systolic BP of ≥130 mmHg, and reducing TC to <5.2 mmol/L for those with a TC concentration of ≥5.2 mmol/L. Statistical analyses were performed using Stata software, Version 11.1 (Stata Corp., College Station, Texas, USA).
Results
The overall response rate for the three surveys was 93%, 83% and 79% for the 1991, 2000 and 2008 surveys, respectively.9–11 A total of 1,900 subjects aged ≥40 years were diagnosed with diabetes in the three surveys. A total of 53% were female. Pregnant women (n = 24) and individuals missing data required to estimate 10-year CVD risk (n = 799) in the three surveys were excluded, giving a total sample of 1,077. Over two decades, the mean age of diabetic subjects significantly increased from 51.5 to 57.7 years (P <0.001). In contrast, the mean TC trend in the entire cohort showed a significant decline from 6.0 mmol/L in 1991 to 5.4 mmol/L in 2008 (P <0.001). This trend was observed in both men and women. In addition, the proportion of male current smokers doubled from 9.7% in 1991 to 19.6% in 2008 (P = 0.03). Mean SBP in men increased by more than 10 mmHg during the same time period (139.3 mmHg in 1991 to 149.9 mmHg in 2008; P = 0.002). No significant linear trends were noted with respect to the percentage of women (P = 0.379), current smokers (P = 0.163) or SBP (P = 0.135) in the entire sample [Table 1].
Table 1:
Characteristics of variables used to calculate the estimated 10-year risk of cardiovascular disease among Omani diabetic adults aged ≥40 years between 1991–2008* (N = 1,077)
| Variables | Survey year† | P value | ||
|---|---|---|---|---|
| 1991 | 2000 | 2008 | ||
| Total | ||||
| n | 379 | 470 | 228 | |
| Women in % | 54.6 (2.6) | 50.0 (2.3) | 56.3 (4.6) | 0.379 |
| Mean age in years | 51.5 (0.5) | 56.7 (0.5) | 57.7 (0.8) | <0.001 |
| Current smoker in % | 5.6 (1.2) | 6.8 (1.1) | 8.5 (2.1) | 0.163 |
| Mean SBP in mmHg | 142.1 (1.1) | 138.6 (0.9) | 146.4 (1.6) | 0.135 |
| Mean TC in mmol/L | 6.0 (0.1) | 5.8 (0.1) | 5.4 (0.1) | <0.001 |
| Men | ||||
| n | 172 | 235 | 100 | |
| Mean age in years | 51.8 (0.7) | 56.8 (0.8) | 58.4 (1.3) | <0.001 |
| Current smoker in % | 9.7 (2.3) | 12.0 (2.1) | 19.6 (4.7) | 0.030 |
| Mean SBP in mmHg | 139.3 (1.6) | 137.2 (1.2) | 149.9 (2.7) | 0.002 |
| Mean TC in mmol/L | 5.9 (0.1) | 5.7 (0.1) | 5.4 (0.1) | 0.002 |
| Women | ||||
| n | 207 | 235 | 128 | |
| Mean age in years | 51 (0.6) | 57 (0.6) | 57.2 (0.9) | <0.001 |
| Current smoker in % | 2.1 (1.1) | 1.7 (1.2) | 0 (-) | 0.157 |
| Mean SBP in mmHg | 144.3 (1.6) | 140.0 (1.3) | 143.6 (1.9) | 0.463 |
| Mean TC in mmol/L | 6.0 (0.9) | 5.9 (0.1) | 5.3 (0.1) | <0.001 |
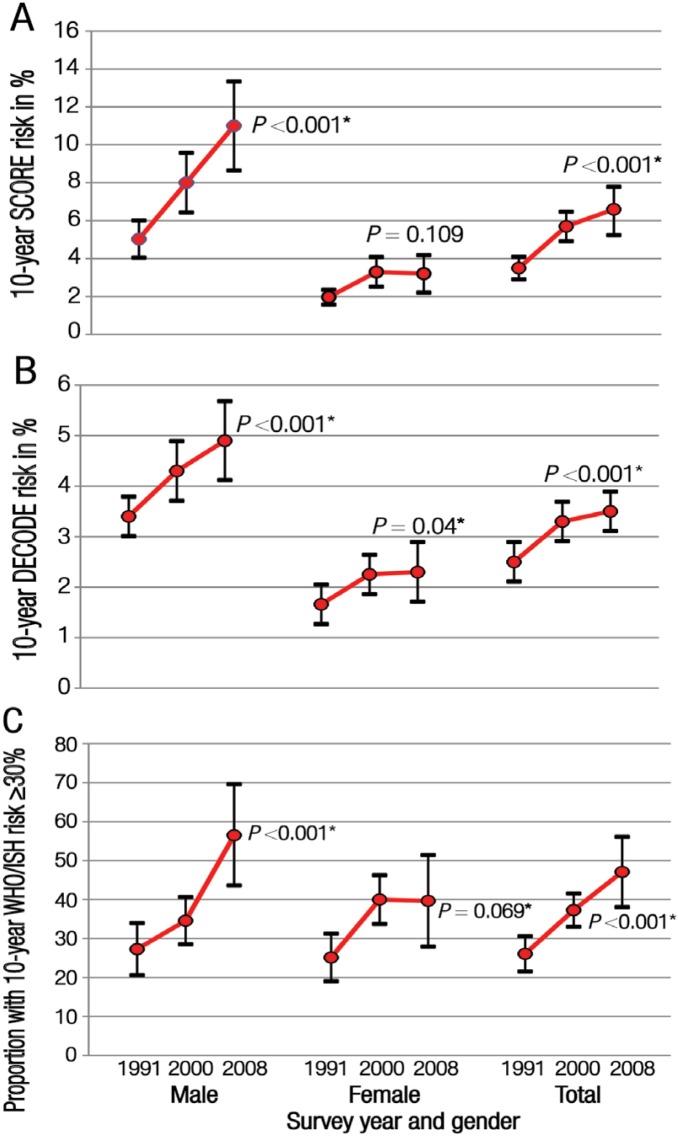
A consistent and significant increase in the 10-year risk of CVD in the entire diabetic cohort and between both genders was observed, regardless of the risk tool used [Figure 1]. The mean estimated 10-year risk for developing CVD using the SCORE tool increased significantly in the total sample (regression coefficient = 10.4%; standard error [SE] = 2.3; P <0.001) as well as among males (regression coefficient = 10.8%; SE = 2.5; P <0.001) and females (regression coefficient = 13.9%; SE = 5.7; P = 0.013). Although lower in magnitude, the DECODE risk tool also showed a similar pattern. Over the period of 1991–2008, men had the highest relative increase (120%) in the mean 10-year CVD risk using the SCORE tool (5% in 1991 to 11% in 2008). Although the relative increase in SCORE risk was less marked among women (60%), an increase was also noted (2% in 1991 to 3.2% in 2008).
Figure 1A–C:
Estimated trends of the 10-year risk for developing cardiovascular disease among adults with diabetes mellitus in Oman by gender and year using data from three population-based national surveys.9–11 Risk prediction was calculated using the (A) Systematic COronary Risk Evaluation (SCORE), (B) Diabetes Epidemiology Collaborative Analysis of Diagnostic Criteria in Europe (DECODE) and (C) World Health Organization (WHO)/International Society of Hypertension (ISH) tools.13–15 For SCORE and DECODE, each point on the graph represents the mean for 10-year risk and the bars represent the upper and lower limits of the 95% confidence intervals.
*Significance of linear trend test.
The proportion of subjects with a 10-year CVD risk of ≥30% increased from 26.1% in 1991 to over 47% in 2008 (P <0.001) using the WHO/ISH charts. Calculations of four hypothetical risk reduction scenarios (eliminating all current smoking, controlling SBP, attaining a favourable TC profile or all three combined) suggested that the largest reduction in the 10-year risk of developing CVD would be gained by improving SBP control compared to the other two interventions. This finding was consistently seen across risk tools and for all three periods studied. Simultaneous modifications of all three risk reduction techniques produced an additional yet modest reduction in the 10-year risk of CVD among people with diabetes [Table 2].
Table 2:
Estimated 10-year risk for cardiovascular disease among Omani diabetic adults aged ≥40 years according to different risk reduction scenarios and risk tools13–15 between 1991–2008* (N = 1,077)
| Survey year† | |||
|---|---|---|---|
| 1991 (n = 379) | 2000 (n = 470) | 2008 (n = 228) | |
| Current risk | |||
| Mean SCORE risk | 3.5 (0.3) | 5.7 (0.4) | 6.6 (0.7) |
| Mean DECODE risk | 2.5 (0.2) | 3.3 (0.2) | 3.5 (0.2) |
| WHO/ISH risk in % with risk ≥30% | 26.1 (2.3) | 37.3 (2.2) | 47.1 (4.6) |
| Smoking elimination scenario | |||
| Mean SCORE risk | 3.4 (0.3) | 5.3 (0.4) | 6.3 (0.7) |
| Mean DECODE risk | 2.4 (0.2) | 3.1 (0.2) | 3.2 (0.2) |
| WHO/ISH risk in % with risk ≥30% | 25.3 (2.3) | 36.2 (2.2) | 45.5 (4.6) |
| SBP <130 mmHg scenario | |||
| Mean SCORE risk | 2.2 (0.2) | 3.9 (0.3) | 3.9 (0.3) |
| Mean DECODE risk | 1.7 (0.1) | 2.4 (0.1) | 2.4 (0.2) |
| WHO/ISH charts in % with risk ≥30% | 15.3 (1.9) | 25.6 (2.1) | 32.5 (4.5) |
| TC level <5.2 mmol/L scenario | |||
| Mean SCORE risk | 2.9 (0.3) | 4.7 (0.4) | 5.8 (0.6) |
| Mean DECODE risk | 2.2 (0.1) | 3.0 (0.1) | 3.2 (0.2) |
| WHO/ISH risk in % with risk ≥30% | 26.1 (2.3) | 36.9 (2.2) | 47.1 (4.6) |
| Overall combined scenario | |||
| Mean SCORE risk | 1.7 (0.1) | 3.0 (0.2) | 3.2 (0.3) |
| Mean DECODE risk | 1.4 (0.1) | 2.0 (0.1) | 2.1 (0.1) |
| WHO/ISH risk in % with risk ≥30% | 14.7 (1.9) | 27.7 (2.1) | 31.8 (4.5) |
SCORE = Systematic COronary Risk Evaluation; DECODE = Diabetes Epidemiology Collaborative Analysis of Diagnostic Criteria in Europe; WHO/ISH = World Health Organization/International Society of Hypertension; SBP = systolic blood pressure; TC = total cholesterol.
Numbers in brackets signify standard error.
Discussion
Morbidity and mortality resulting from all forms of CVD are 2–8-fold higher among individuals with diabetes than in those without.16 Diabetes management should therefore include recommendations to prevent and control CVD risk. Using the SCORE, DECODE and WHO/ISH risk tools, this study found an increasing trend in the 10-year CVD risk among both men and women with diabetes in Oman between 1991–2008. In contrast, studies from industrialised nations have reported a declining trend in death rates and 10-year CVD risk among diabetic patients over the past two decades.17,18 This decline is largely attributed to improved management of CVD risk factors and hyperglycaemia through medication and behavioural changes.18,19
In Oman, a small number of community-based interventions focusing on both individual and community-wide behavioural change have been initiated at the provincial level. The largest of these was implemented in the Nizwa region in 2001.20 However, the 2010 Nizwa Healthy Lifestyle Project Evaluation Report indicated that the prevalence of diabetes in Nizwa had increased from 9.2% in 2001 to 9.7% in 2010 (P = 0.61).21 Similar increases were seen in the prevalence of CVD risk factors during the same time period, including pre-hypertension (8% to 13%; P = 0.0001), clinical hypertension (12% to 24%; P <0.001), being overweight (28% to 33%; P = 0.001) and obesity (13% to 17%; P = 0.001), although it is possible that these trends are not as dramatic as those observed nationally.21 For community-based interventions aiming to reduce CVD risk impact, policies and legislation related to tobacco control, salt reduction in foods and food taxes or subsidies to support healthy eating need to be developed in coordination with other sectors and implemented within communities in order for them to have the desired effect.4
In the present study, men were shown to have an absolute 10-year CVD risk that was 2–6 times higher than women. This may be a function of the observed increase among men of all the studied CVD risk factors; in comparison, only the risk factors of age and TC levels were found to increase among women. In a study of 2,551 people with diabetes, Al-Lawati et al. reported that men, on average, were older and had worse glycaemic and lipid profiles (glycated haemoglobin A1c ≥7% and TC ≥5.2 mmol/L) compared to women.22 Thus, the gender difference may be due at least partly to increased biological CVD risk levels in men,23 as well as a higher prevalence of behavioural risk factors among males (e.g. the prevalence of daily smoking in men is 14.8% compared to <0.5% in women).12 Furthermore, the mean age of the subjects increased by seven years over the span of two decades and this may also partially explain the increase in CVD risk in the total cohort. A small intervention study found that treatment plans were adhered to more closely among women than men; this may also partially explain the gender difference.24 It is also possible that the observed gender difference is a function of the equations used by the three risk tools to estimate 10-year CVD risk. Further research on ways to improve the implementation of diabetes management guidelines in Oman may prove useful in reducing gender disparities in CVD risk.
In the current study, the possible impact of hypothetical scenarios on 10-year CVD risk reduction was assessed. Among the risk factors studied (smoking, high cholesterol and hypertension), the analysis revealed that reducing SBP to ≤130 mmHg would result in the greatest reduction in 10-year CVD risk for the Omani population. In contrast, a similar analysis in the USA using the UK Prospective Diabetes Study (UKPDS) risk engine determined that reducing TC to <5.2 mmol/L and raising high-density lipoprotein levels to 1.05 mmol/L in men and 1.3 mmol/L in women were the factors that would most significantly reduce the 10-year coronary risk in their population.18 This difference is possibly due to decreasing TC levels and a simultaneous increase in hypertension among the general population of Oman.12,25 More intense population-based efforts to address risk factors for hypertension in Oman are warranted, particularly regarding behavioural risks such as high salt intake, unhealthy diets and physical inactivity. The WHO has identified the most cost-effective interventions to address CVD risk factors fueling the global epidemic of non-communicable diseases;4 these could be used to guide public health action in Oman.
Suboptimal management of glycaemia and cardiovascular risk factors among individuals with diabetes has been reported widely.26 Similar concerns have been raised regarding the quality of care provided for diabetic patients in Oman.22,27–29 Based on local evidence, strengthening patient education and self-management, training health workers in the primary care setting on behavioural change and redesigning delivery of care systems at the local level have been identified as key factors to improving quality of care.24,30 In addition, promoting more aggressive diabetes management may decrease the incidence of CVD.31–35
The strength of the current study lies in the utilisation of three population-based national surveys with similar methodologies to estimate the 10-year CVD risk among Omanis with diabetes. However, some uncertainty exists regarding the reported age of participants. All studied cohorts were born before or around 1968 when the entire country had only one hospital. At this time, birth registration was not a statutory requirement; even during the 1970s and 1980s, there was no emphasis on registering events such as deaths or births.36 It is possible, therefore, that the selected sample of adults does not include all those who were eligible for inclusion in this study due to inaccurate reporting among older adults. This may therefore have diluted the real mean estimates of the 10-year CVD risk. A second source of bias may have been introduced with missing variables, particularly with data obtained from the 2008 survey, as approximately 700 blood samples were not obtained. This missing data may indicate that certain subjects were excluded (for example, diabetic subjects who did not attend a scheduled blood test), thereby further diluting the measured effect on CVD trends. In addition, CVD-free status was self-reported by participants and not objectively verified. Given that illness-denial is not uncommon among survey subjects,37 this may have resulted in an overestimation of the 10-year CVD risk. A further limitation of this study was that two of the tools used to estimate 10-year CVD risk (SCORE and DECODE) were developed for European patients who are likely to differ from an Arab population in the Middle East. A study by Coleman et al. determined that these tools were not reliable across all patient populations.38 This factor may have biased risk estimates. Finally, the SCORE risk tool did not include any variable on glucose status as diabetes is often regarded as a coronary heart disease risk equivalent.39 Nonetheless, this tool was used in the current study to evaluate CVD risk in people with diabetes.
Conclusion
The increasing incidence of diabetes and associated risk factors for CVD is a serious public health concern in Oman. Using risk prediction tools, this study found an increasing trend in the 10-year CVD risk among both men and women with diabetes in Oman between 1991–2008. Focused community-based public health action based on recognised interventions to address behavioural risks for CVD should be a priority. Improving the quality of care, both at the individual and health system level, requires extra clinical emphasis in addition to personnel and financial resources. Further research on population- and individual-based interventions should be undertaken to guide specific public health actions to minimise the CVD risk among diabetic patients in Oman.
Acknowledgments
The authors thank the Department of Research & Studies, Ministry of Health, Oman, for sharing the dataset of the 2008 Oman World Health Survey. Additionally, the authors would also like to thank the Nizwa Healthy Lifestyle Project team for sharing selected results from their 2010 survey. The views expressed in this paper are those of the authors and do not necessarily reflect those of the WHO.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
References
- 1.International Diabetes Federation. Complications of Diabetes. From: www.idf.org/complications-diabetes Accessed: Oct 2013.
- 2.Barrett-Connor E, Pyörälä K. Long-term complications: Diabetes and coronary heart disease. In: Ekoé J-M, Zimmet P, Williams R, editors. The Epidemiology of Diabetes Mellitus: An International Perspective. West Sussex, UK: John Wiley & Sons Ltd; 2001. pp. 301–18. [Google Scholar]
- 3.Laakso M, Lehto S. Epidemiology of macrovascular disease in diabetes. Diabetes Rev. 1997;5:294–315. [Google Scholar]
- 4.World Health Organization. Global status report on noncommunicable diseases 2010: Description of the global burden of NCDs, their risk factors and determinants. From: www.who.int/nmh/publications/ncd_report2010/en/ Accessed: Mar 2014.
- 5.Pradeepa R, Prabhakaran D, Mohan V. Emerging economies and diabetes and cardiovascular disease. Diabetes Technol Ther. 2012;14:S59–67. doi: 10.1089/dia.2012.0065. [DOI] [PubMed] [Google Scholar]
- 6.Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, et al. The burden of mortality attributable to diabetes: Realistic estimates for the year 2000. Diabetes Care. 2005;28:2130–5. doi: 10.2337/diacare.28.9.2130. [DOI] [PubMed] [Google Scholar]
- 7.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Ng SW, Zaghloul S, Ali HI, Harrison G, Popkin BM. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf states. Obes Rev. 2011;12:1–13. doi: 10.1111/j.1467-789X.2010.00750.x. [DOI] [PubMed] [Google Scholar]
- 9.Asfour MG, Lambourne A, Soliman A, Al-Behlani S, Al-Asfoor D, Bold A, et al. High prevalence of diabetes mellitus and impaired glucose tolerance in the Sultanate of Oman: Results of the 1991 national survey. Diabet Med. 1995;12:1122–5. doi: 10.1111/j.1464-5491.1995.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 10.Al-Lawati JA, Al Riyami AM, Mohammed AJ, Jousilahti P. Increasing prevalence of diabetes mellitus in Oman. Diabet Med. 2002;19:954–7. doi: 10.1046/j.1464-5491.2002.00818.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Riyami A, Abdelaty MA, Jaju S, Morsi M, Al-Kharusi H, Al-Shekaili W. World Health Survey 2008. Muscat, Oman: Ministry of Health; 2012. [Google Scholar]
- 12.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus, provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 13.Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. SCORE project group Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/S0195-668X(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 14.Balkau B, Hu G, Qiao Q, Tuomilehto J, Borch-Johnsen K, Pyörälä K, DECODE Study Group; European Diabetes Epidemiology Group Prediction of the risk of cardiovascular mortality using a score that includes glucose as a risk factor: The DECODE study. Diabetologia. 2004;47:2118–28. doi: 10.1007/s00125-004-1574-5. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO/ISH Risk Prediction Charts for 14 WHO Epidemiological Sub-Regions. From: www.ish-world.com/downloads/activities/colour_charts_24_Aug_07.pdf Accessed: Jan 2012.
- 16.Grundy SM, Howard B, Smith S, Jr, Eckel R, Redberg R, Bonow RO. Prevention Conference VI: Diabetes and cardiovascular disease: Executive summary: Conference proceeding for healthcare professionals from a special writing group of the American Heart Association. Circulation. 2002;105:2231–9. doi: 10.1161/01.cir.0000013952.86046.dd. doi: 0.1161/01.CIR.0000013952.86046.DD. [DOI] [PubMed] [Google Scholar]
- 17.Gregg EW, Cheng YJ, Saydah S, Cowie C, Garfield S, Geiss L, et al. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: Findings from the National Health Interview Survey. Diabetes Care. 2012;35:1252–7. doi: 10.2337/dc11-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: Findings from the National Health and Nutrition Examination Survey, 1999– 2008. Diabetes Care. 2011;34:1337–43. doi: 10.2337/dc10-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 20.Al-Lawati JA, Mohammed AJ, Al-Hinai HQ, Jousilahti P. Prevalence of the metabolic syndrome among Omani adults. Diabetes Care. 2003;26:1781–5. doi: 10.2337/diacare.26.6.1781. [DOI] [PubMed] [Google Scholar]
- 21.Ministry of Health. Nizwa Healthy Lifestyle Project Evaluation Report 2010. Muscat, Oman: Ministry of Health; 2014. [Google Scholar]
- 22.Al-Lawati JA, N Barakat M, Al-Zakwani I, Elsayed MK, Al-Maskari M, M Al-Lawati N, et al. Control of risk factors for cardiovascular disease among adults with previously diagnosed type 2 diabetes mellitus: A descriptive study from a Middle Eastern Arab population. Open Cardiovasc Med J. 2012;6:133–40. doi: 10.2174/1874192401206010133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 24.Al-Sinani M, Min Y, Ghebremeskel K, Qazaq HS. Effectiveness of and adherence to dietary and lifestyle counselling: Effect on metabolic control in type 2 diabetic Omani patients. Sultan Qaboos Univ Med J. 2010;10:341–9. [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Riyami A, Afifi M, Al-Kharusi H, Morsi M. National health survey, study of lifestyle risk factors 2000. Muscat, Oman: Ministry of Health; 2003. [Google Scholar]
- 26.Gakidou E, Mallinger L, Abbott-Klafter J, Guerrero R, Villalpando S, Ridaura RL, et al. Management of diabetes and associated cardiovascular risk factors in seven countries: A comparison of data from national health examination surveys. Bull World Health Organ. 2011;89:172–83. doi: 10.2471/BLT.10.080820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdulhadi N, Al Shafaee M, Freudenthal S, Ostenson CG, Wahlström R. Patient-provider interaction from the perspectives of type 2 diabetes patients in Muscat, Oman: A qualitative study. BMC Health Serv Res. 2007;7:162. doi: 10.1186/1472-6963-7-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elliott JA, Abdulhadi NN, Al-Maniri AA, Al-Shafaee MA, Wahlström R. Diabetes self-management and education of people living with diabetes: A survey in primary health care in Muscat Oman. PloS One. 2013;8:e57400. doi: 10.1371/journal.pone.0057400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Mandhari A, Al-Zakwani I, El-Shafie O, Al-Shafaee M, Woodhouse N. Quality of diabetes care: A cross-sectional observational study in Oman. Sultan Qaboos Univ Med J. 2009;9:32–6. [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Shookri A, Khor GL, Chan YM, Loke SC, Al-Maskari M. Effectiveness of medical nutrition treatment delivered by dietitians on glycaemic outcomes and lipid profiles of Arab, Omani patients with type 2 diabetes. Diabet Med. 2012;29:236–44. doi: 10.1111/j.1464-5491.2011.03405.x. [DOI] [PubMed] [Google Scholar]
- 31.Kesteloot H, Sans S, Kromhout D. Dynamics of cardiovascular and all-cause mortality in Western and Eastern Europe between 1970 and 2000. Eur Heart J. 2006;27:107–13. doi: 10.1093/eurheartj/ehi511. [DOI] [PubMed] [Google Scholar]
- 32.Ferrannini E, Cushman WC. Diabetes and hypertension: The bad companions. Lancet. 2012;380:601–10. doi: 10.1016/S0140-6736(12)60987-8. [DOI] [PubMed] [Google Scholar]
- 33.Mannucci E, Monami M, Lamanna C, Gori F, Marchionni N. Prevention of cardiovascular disease through glycemic control in type 2 diabetes: A meta-analysis of randomized clinical trials. Nutr Metab Cardiovasc Dis. 2009;19:604–12. doi: 10.1016/j.numecd.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 34.Kelly TN, Bazzano LA, Fonseca VA, Thethi TK, Reynolds K, He J. Systematic review: Glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med. 2009;151:394–403. doi: 10.7326/0003-4819-151-6-200909150-00137. [DOI] [PubMed] [Google Scholar]
- 35.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 36.ElSayed MK. Civil Registration in the Sultanate of Oman: Its development and potential implications on vital statistics. Global Forum on Gender Statistics. From: www.en.istat.it/istat/eventi/2007/globalforum/martedimattina/CivilRegistrationOman.pdf Accessed: Jan 2014.
- 37.Covino JM, Stern TW, Stern TA. Denial of cardiac illness: Consequences and management. Prim Care Companion CNS Disord. 2011;13 doi: 10.4088/PCC.11f01166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coleman RL, Stevens RJ, Retnakaran R, Holman RR. Framingham, SCORE, and DECODE risk equations do not provide reliable cardiovascular risk estimates in type 2 diabetes. Diabetes Care. 2007;30:1292–3. doi: 10.2337/dc06-1358. [DOI] [PubMed] [Google Scholar]
- 39.Whiteley L, Padmanabhan S, Hole D, Isles C. Should diabetes be considered a coronary heart disease risk equivalent? Results from 25 years of follow-up in the Renfrew and Paisley survey. Diabetes Care. 2005;28:1588–93. doi: 10.2337/diacare.28.7.1588. [DOI] [PubMed] [Google Scholar]