Abstract
Objectives:
Sleep deprivation is common among medical residents of all specialties. This study aimed to determine the prevalence of sleep deprivation and depressive symptoms among medical residents in King Fahd University Hospital (KFUH) in Al Khobar, Saudi Arabia. Furthermore, the association between sleep deprivation, sleepiness and depressive symptoms was examined.
Methods:
This cross-sectional study took place between February and April 2012 and involved 171 KFUH medical residents of different specialties. Data were collected using a specifically designed questionnaire eliciting demographic information, working hours and number of hours of sleep. In addition, validated Arabic versions of the Epworth Sleepiness Scale and the Beck Depression Inventory-2 (BDI-2) were used.
Results:
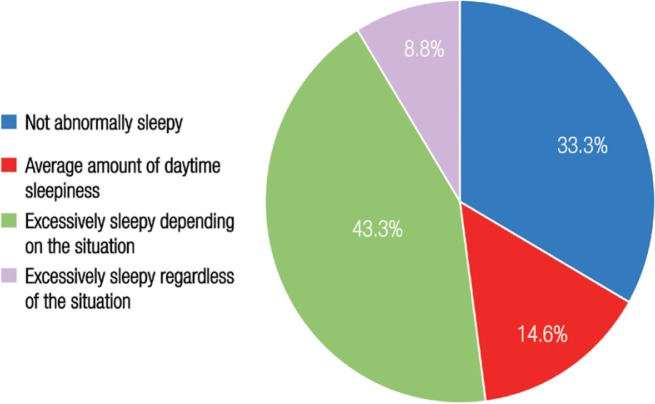
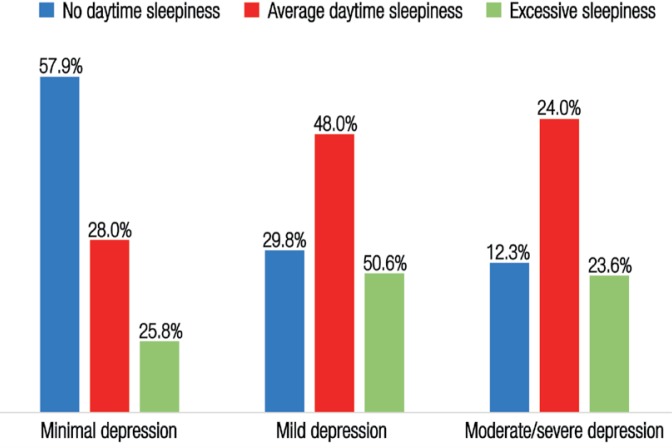
The prevalence of acute sleep deprivation and chronic sleep deprivation among residents in KFUH was 85.9% and 63.2%, respectively. The prevalence of overall sleepiness was 52%; 43.3% reported being excessively sleepy in certain situations while 8.8% reported being excessively sleepy regardless of the situation. Based on the BDI-2, the prevalence of mild, moderate and severe depressive symptoms was 43.3%, 15.2% and 4.7%, respectively. Significant associations were found between sleep deprivation and depressive symptoms; depressive symptoms and sleepiness, and depressive symptoms and being a female resident.
Conclusion:
The vast majority of medical residents had acute sleep deprivation, with more than half suffering from chronic sleep deprivation. The number of hours and quality of sleep among the residents were strongly associated with depressive symptoms. New regulations are recommended regarding the number of working hours and night duties for medical residents. Further studies should assess these new regulations on a regular basis.
Keywords: Sleep Deprivation, Depression, Drowsiness, Physicians, Saudi Arabia
Advances in Knowledge
- To the best of the authors’ knowledge, no study has yet been carried out in Saudi Arabia to examine the prevalence of sleep deprivation and its relation to depression among medical residents.
- The results of this study suggest that there is a strong association between depressive symptoms and acute sleep deprivation, working hours, sleepiness and gender among medical residents in a university hospital in Saudi Arabia.
Application to Patient Care
- Sleep deprivation among medical residents may affect the quality of their patient care. This study may improve awareness of sleep deprivation and depression in residents and contribute to new guidelines concerning the number of working hours and night duties assigned to residents.
The amount of sleep obtained by medical residents can have a significant impact on their work performance and, in turn, the safety of the patients they are interacting with. It is well known that residency training is very stressful, particularly as a result of the long working hours and heavy work load; these challenges often lead to sleep deprivation and limited personal time for residents.1,2 These conditions may be related to a high incidence of depression and anxiety among interns and residents.3,4 Sleep deprivation occurs when an individual has had insufficient sleep to function adequately in terms of their alertness, performance and health.5 The two main types of sleep deprivation are known as acute and chronic sleep deprivation. An individual will experience acute sleep deprivation if they have not slept over a period of one or two days while chronic sleep deprivation occurs as a result of sleeping less than 5–6 hours for several consecutive nights.5,6 Medical residents may experience acute sleep loss during night shifts when they are on-call. In addition, they may also experience chronic sleep loss as a long-term effect of regular night shifts.
Many studies have demonstrated the negative effects of acute and chronic sleep deprivation on the health of an individual.7,8 In addition, previous research has examined the association between sleep deprivation and depression among physicians. One such study found that chronic sleep deprivation increased the incidence of moderate depression by seven-fold.9 Balch et al. studied the relationship between working hours, night duties and surgeon distress. They found that depression was significantly associated with long working hours as well as an increased number of nights on-call.10
To the best of the authors’ knowledge, no studies have yet been carried out in Saudi Arabia to examine the prevalence of sleep deprivation and its relation to depression among residents. Therefore, the objective of this study was to determine the extent of sleep deprivation and depressive symptoms among medical residents of all specialties in King Fahd University Hospital (KFUH) in Al Khobar, Saudi Arabia. Furthermore, the association between sleep deprivation, sleepiness and depressive symptoms was examined.
Methods
This cross-sectional study was conducted from February to April 2012 among residents at KFUH in Al Khobar, Saudi Arabia. Medical residents of both genders working in all specialties and with night duties were included in the study population (N = 185). Both Saudi and non-Saudi participants were included. Residents who participated in the pilot study, those who did not respond and those who failed to complete the entire questionnaire were excluded from the study. Three instruments were used to collect data from the participants, including a specifically designed questionnaire and validated versions of the Epworth Sleepiness Scale (ESS) and the Beck Depression Inventory-2 (BDI-2).11,12
The first questionnaire was designed for the study and was composed of two sections. The first section collected demographic data including age, gender, nationality, marital status, number of family members/ children, pregnancy/nursing status for females, place of residence, living situation, income, specialty, level of residency and years of experience. The second section aimed to measure sleep deprivation, specifically the resident’s number of sleeping hours over their last night duty and in the previous seven days, number of working hours over one night duty and per week and the overall number of night duties per month. Following this, an Arabic version of the ESS was used.13 This self-administered eight-item questionnaire was translated by Riachy et al. from the original English version.11,13 The ESS has been shown to have good internal consistency with a Cronbach’s alpha value of 0.762.14 An overall score of 10 or more from the eight individual scores reflects above average daytime sleepiness and a need for further evaluation.11 The third instrument used was the BDI-2, a 21-item self-reported test translated into Arabic by Ghareeb in 2000.12,15 Alpha values for this instrument range from 0.82–0.93, indicating high reliability and internal consistency.16 A total score of 0–9 is considered to indicate minimal depression, while 10–19, 20–29 and 30–63 indicate mild, moderate and severe depression, respectively.15
A pilot study utilising the above instruments was carried out on 21 medical residents who were working in King Fahd Medical Military City and specialising in either obstetrics and gynaecology, family medicine or surgery. Three participants faced some difficulties in understanding a number of the sentences in the Arabic BDI-2 and therefore did not complete it. The overall response to the two scales (the Arabic versions of the BDI-2 and ESS) was that there was some ambiguity in the questions and participants had difficulties scoring themselves in the case of the Arabic BDI-2. Some alterations were made to both scales under the supervision of two consultants (one family physician and one psychologist) to resolve any ambiguity and clarify each question. The entire questionnaire (including the main questionnaire and the Arabic versions of the BDI-2 and EPSS) was then tested again on 30 participants with a positive response.
After data collection, all variables were processed using the Statistical Package for the Social Sciences (SPSS), Version 16.0 (IBM Corp., Chicago, Illinois, USA). A P value of ≤0.05 was considered statistically significant.
Ethical approval for this study was obtained from the Medical Director of KFUH. Verbal consent was taken from the participants after the purpose of the study was explained and confidentiality of the data was assured.
Results
Out of the 185 residents in the study population, 171 completed the questionnaire in its entirety, giving a response rate of 92.4%. Approximately 80% of the residents were between 25–30 years old while 16% were between 30 and 35. A total of 58% of the participants were female. The vast majority of the residents were Saudi Arabian (85%). More than half of the residents were married and less than 3% were divorced or separated. The majority of the residents (64%) were working in non-surgical specialties and 23% were working in family medicine. The residents were well distributed in terms of the different residency levels, with the exception of fifth-year (5%) and sixth-year residents (0%). More than 8% of the residents were service residents, i.e. residents who were working in a certain speciality department but were not part of the residency program for that speciality. About half of the participants had less than three years of experience and approximately 10% had more than five years of experience.
Table 1 shows the prevalence of sleep deprivation as indicated by direct indices (sleeping hours per night duty and sleeping hours per week). A total of 147 respondents (85.9%) reported that they had slept for less than six hours during their last night duty and thus were considered to be acutely sleep-deprived. Moreover, 63.2% of the residents were considered to be chronically sleep-deprived as they had slept for less than 42 hours in the previous seven days. Table 1 also shows the association between depressive symptoms and the direct indices of sleep deprivation. The association between acute sleep deprivation and depressive symptoms among residents was statistically significant (P = 0.009), with 45.9% of acutely sleep deprived residents showing mild depressive symptoms and 21.2% reporting moderate to severe depressive symptoms. There were no significant associations between chronic sleep deprivation and depressive symptoms among residents (P = 0.115).
Table 1:
Prevalence of sleep deprivation measured by direct indices and the association with depression among surveyed medical residents at King Fahd University Hospital (N = 171)
Table 2 shows the prevalence of sleep deprivation as indicated by indirect indices (working hours per week and the number of night duties per month). The lowest frequency was represented by residents working 8–18 hours (<3%) in one night shift, while the highest frequency was for those who worked 19–24 hours (≥40%). Residents who worked 40–76 hours a week were slightly more common than those who worked 77–90 hours. Approximately half of the residents had more than five night duties a month while only 9.4% had less than three night shifts. Furthermore, the association between the number of working hours per night duty and depressive symptoms was statistically significant (P = 0.003). As shown in Table 2, 54.8% of residents who worked more than 24 hours per one-night duty had mild depressive symptoms while 20.2% of those working more than 24 hours had moderate to severe symptoms. Depressive symptoms in residents were also shown to be significantly associated with the number of working hours per week (P = 0.047). Of the 74 residents who worked more than 76 hours per week, 28.4% reported symptoms of moderate to severe depression compared to 13.4% of those who worked less than 77 hours. No significant association was found between the number of night duties per month and depressive symptoms among residents (P = 0.780).
Table 2:
Prevalence of sleep deprivation measured by indirect indices and the association with depression among surveyed medical residents at King Fahd University Hospital (N = 171)
| Indirect index | n (%) | Percentage of residents | P value | ||
|---|---|---|---|---|---|
| Minimal depression† | Mild depression† | Moderate/severe depression† | |||
| Working hours per night duty | |||||
| ≤24 | 76 (44.4) | 48.7 | 30.3 | 21.1 | 0.003* |
| >24 | 84 (49.2) | 25 | 54.8 | 20.2 | |
| Working hours per week | |||||
| 40–76 | 97 (56.7) | 41.2 | 45.4 | 13.4 | 0.047* |
| 77–90 | 74 (43.3) | 31.1 | 40.5 | 28.4 | |
| Night duties per month | |||||
| 0 | 7 (4.1) | 42.9 | 42.9 | 14.3 | 0.780 |
| <3 | 9 (5.3) | 55.6 | 33.3 | 11.1 | |
| 3–5 | 66 (38.6) | 40.9 | 40.9 | 18.2 | |
| >5 | 89 (52) | 31.5 | 46.1 | 22.5 | |
The reported prevalence of sleepiness among the studied KFUH residents is depicted in Figure 1. A total of 89 residents (52%) experienced sleepiness; of those, 43.3% experienced excessive sleepiness in specific circumstances for which they might consider seeking medical attention, while 8.8% reported continuous excessive sleepiness requiring medical attention. Figure 2 shows the prevalence of depressive symptoms among the cohort. According to their responses to the BDI-2 instrument, 108 residents (63%) had depressive symptoms. The majority of those (43.3%) had mild symptoms, while 15.2% reported moderate symptoms and symptoms of severe depression. Moreover, 4.7% admitted to having suicidal thoughts. The relationship between depression and sleepiness among the residents can be seen in Figure 3. A significant association was found between sleepiness and depressive symptoms among the cohort (P = 0.003). Of the residents who reported excessive daytime sleepiness, 50.6% had mild depressive symptoms while 23.6% had symptoms of moderate to severe depression.
Figure 1:
Prevalence of sleepiness among surveyed medical residents at King Fahd University Hospital (N = 171). Sleepiness was scored using a validated Arabic version of the Epworth Sleepiness Scale.12,14
Figure 2:
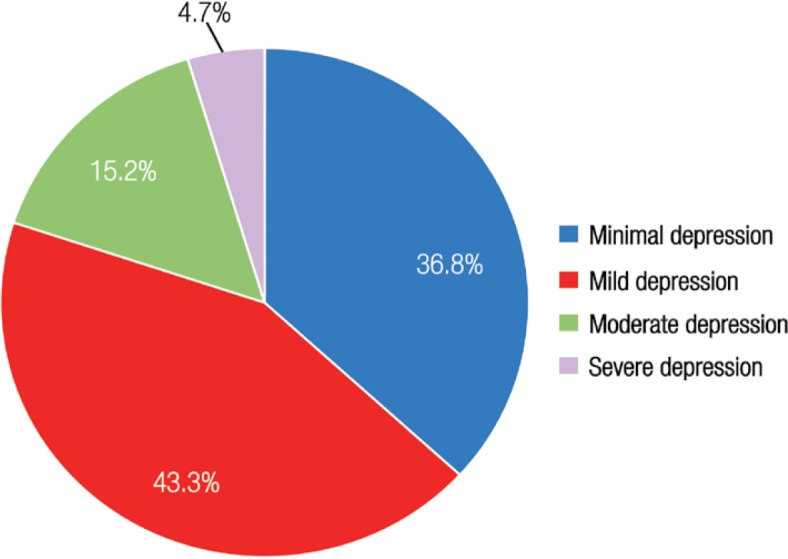
Prevalence of depression among surveyed medical residents at King Fahd University Hospital (N = 171). Depression was scored using a validated Arabic version of the Beck Depression Inventory-2.13,16 Critically, 4.7% of the cohort admitted to having suicidal thoughts.
Figure 3:
Prevalence of sleepiness among surveyed medical residents at King Fahd University Hospital (N = 171). Sleepiness was scored using a validated Arabic version of the Epworth Sleepiness Scale.12,14
There were no significant associations between depressive symptoms and sociodemographic factors, with the exception of gender (P = 0.033). A significant increase in the prevalence of depressive symptoms among female residents (68.7%) was noted in comparison to male residents (55.5%). Additionally, the percentage of female residents showing moderate to severe depressive symptoms was more than double that of the male residents. No significant relationship was found between the prevalence of depressive symptoms and choice of specialty; however, it was interesting to note that the prevalence of depressive symptoms was highest among general surgery, internal medicine, neurology and urology residents. Additionally, although no significant relationship was found between the prevalence of depressive symptoms and residency levels in general, the prevalence of depressive symptoms rose slightly among third-year residents and doubled among fourth-year residents in comparison to non-depressed residents at the same level. The results also revealed that the rates of depression among service residents were double that of non-service residents.
Discussion
Residency training is known to be a challenging and demanding period and many studies have investigated issues related to residents’ performance, mood changes, sleep deprivation and sleepiness. However, few studies have examined the possible relationship between sleep deprivation and depressive symptoms.9,10 The current study revealed that the majority of KFUH residents were acutely sleep-deprived (85.9%). This result was similar to those reported in both local and international studies. Sleep deprivation among medical residents in Chicago, USA, was reported to be extremely high (over 92%).17 Additionally, the prevalence of acute sleep deprivation among medical residents at KFUH was very similar to that observed among junior doctors in Jeddah, Saudi Arabia (87%).18 Chronic sleep deprivation among KFUH residents was also high (63.2%). A study conducted at the University of Pennsylvania in the USA found a much lower rate (43%).9 However, Wada et al. conducted a national survey on Japanese physicians which indicated a higher prevalence of total chronic sleep deprivation (85%).19
The frequency of night duties among KFUH residents did not differ from the norm when compared to similar studies around the world. Of the KFUH residents, 52% had an average of more than five night duties per month as compared to Japanese residents (58.9%) and German physicians (48.2%) with more than five and six night duties per month, respectively.19,20 However, the current study’s findings indicated a high number of working hours per week. At KFUH, 43.3% of the residents worked more than 76 hours per week; this is comparable to a study in Germany which reported 48.1% of physicians working over 70 hours per week.20 In contrast, less than 17% of the residents in the American College of Surgeons were reported to work more than 80 hours a week.10 The reason for this finding may be due to variations in working hours, night duty and on-call policies at individual institutions. Furthermore, the current study found a significant association between working hours and the prevalence of depression. However, the number of night duties worked by the residents did not affect the severity of their depressive symptoms. Balch et al. found a significant increase in the prevalence of depression with an increase in working hours among American surgeons.10
A significant association was observed between sleepiness and depressive symptoms among the residents in the current study. Excessive daytime sleepiness as a normal consequence of sleep loss was elevated (52%). This is higher than findings reported among Pennsylvania medical residents which ranged from 11% at the beginning of the academic year to 36% towards the end.9 In addition, the prevalence of depressive symptoms among the KFUH residents was particularly high (63%) in comparison to other studies. In Japan, the prevalence of depression among physicians was only 8.8%.19 Moreover, Goebert et al. examined depressive symptoms in medical students and residents in six different states in the USA; this study found that 11.9% of the medical residents were depressed, with 4.7% reporting mild to moderate depression and 7.2% with major depression, including 3.9% indicating suicidal ideation.21 The high prevalence of depressive symptoms among KFUH residents may potentially be explained by work-related stressors, such as difficulties with the nature of the work, patient care, career planning, poor interpersonal/interdisciplinary relationships, inadequate learning environments, a lack of adequate mentoring and information overload. A number of cultural factors or non-work-related stressors could also play a part, such as financial concerns or a lack of emotional support.
A strong association between sleep deprivation and depression was noted in the current study, akin to findings in the literature.10,22 However, while the significant relationship between depressive symptoms and acute sleep deprivation was confirmed, the relationship between depressive symptoms and chronic sleep deprivation was not significant. Wali et al. studied the effect of on-call-related sleep deprivation on junior physicians’ moods in Jeddah. In sleep-deprived physicians, mood status scores were high and were related to acute sleep deprivation and long on-call periods.18 Depression scores were significantly higher in the post-on-call period than in the pre-on-call period.18 In contrast to the current study, some research has shown a significant association between depressive symptoms and chronic sleep deprivation. Rosen et al. found a strong association between depression and chronic sleep deprivation among junior doctors in Pennsylvania.9 Among Japanese physicians, Wada et al. also found an association between depression and routinely sleeping less than five hours in a 24-hour period.19
Although the proportion of male to female participants differed, the results of the current study showed a significantly greater prevalence of depressive symptoms among female residents than their male counterparts. This finding could be due to several reasons. Women may be subject to additional stressors such as familial responsibilities (e.g. household tasks and child care), a lack of personal time, exhaustion and hormonal changes. Other studies have also observed that female physicians have a higher prevalence of depression. The prevalence of depression among physicians in primary healthcare settings in Jeddah was greater among women (53.3%) than men (28.6%).23 Wada et al. also found that depression among female Japanese physicians was more frequent than among men (10.5% and 8.3%, respectively).19
The outcome of this research may increase awareness about the need for sufficient sleep among medical professionals, as well as the need to regulate medical residents’ work hours. The number of working hours and night duties per month at KFUH is determined by the Saudi Arabian Ministry of Civil Services; however, it was observed that within many of the specialities these regulations were not being followed. Therefore, the authors of the current study recommend that a clear detailed guideline be set stating the number of working hours and night duties for residents. Specific guidelines for pregnant female residents should also be included. These new guidelines should be assessed on a regular basis by further studies. Additionally, the authors recommend that all medical residents be educated on the importance of sleep and its relationship to depression. Residents should be capable of predicting symptoms of sleep deprivation and depression and amend their sleeping patterns accordingly. Furthermore, a well-trained mentor for each resident is necessary to help minimise stress in the professional setting. Regular meetings should also be organised for all residents, including newly graduated specialists, in order for them to share their knowledge and experiences with one another.
The present study included some limitations. A few residents faced difficulties in answering the questions that depended on recalling their frequency of sleep. Furthermore, self-reported values may have been biased or inaccurate. Certain residents did not respond due to either a lack of time or interest and therefore were not included in the study. As the study was cross-sectional, it was difficult to determine causality. The simple random sampling technique was difficult to apply due to the limited time frame of the study and the number of residents in the study population. Finally, potential comorbidities and medications among the residents were not evaluated, which may have affected the results.
Conclusion
The vast majority of the studied KFUH residents were found to have acute sleep deprivation and more than half of them had chronic sleep deprivation. Daytime sleepiness was prevalent in almost half of the cohort. Approximately two-thirds of the participants reported mild or moderate to severe depressive symptoms. Strong associations were found between depressive symptoms and acute sleep deprivation, working hours (either per night duty or per week), sleepiness and gender. New regulations are recommended regarding the number of working hours and night duties for medical residents.
Acknowledgments
The authors would like to extend special thanks to Dr. Ammar Khamis, statistical advisor, for his constant guidance and support.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Shapiro SL, Shapiro DE, Schwartz GE. Stress management in medical education: A review of the literature. Acad Med. 2000;75:748–59. doi: 10.1097/00001888-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Public Citizen Foundation Petition Requesting Medical Residents Work Hour Limits. From: www.publiccitizen.org/publications/release.cfm?ID=6771 Accessed: Feb 2014.
- 3.Kirsling RA, Kochar MS, Chan CH. An evaluation of mood states among first-year residents. Psychol Rep. 1989;65:355–66. doi: 10.2466/pr0.1989.65.2.355. [DOI] [PubMed] [Google Scholar]
- 4.Girard DE, Elliot DL, Hickman DH, Sparr L, Clarke NG, Warren L, et al. The internship: A prospective investigation of emotions and attitudes. West J Med. 1986;144:93–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Cirelli C. Definition and consequences of sleep deprivation. From: www.uptodate.com/contents/definition-and-consequences-of-sleep-deprivation Accessed: Feb 2014. [DOI] [PubMed]
- 6.Carskadon MA, Dement WC. Cumulative effects of sleep restriction on daytime sleepiness. Psychophysiology. 1981;18:107–13. doi: 10.1111/j.1469-8986.1981.tb02921.x. [DOI] [PubMed] [Google Scholar]
- 7.Kramer M. Sleep loss in resident physicians: The cause of medical errors? Front Neurol. 2010;1:128. doi: 10.3389/fneur.2010.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Sleep Foundation White Paper: How much sleep do adults need? From: www.sleepfoundation.org/article/white-papers/how-much-sleep-do-adults-need Accessed: Apr 2012.
- 9.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81:82–5. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Balch CM, Shanafelt TD, Dyrbye L, Sloan JA, Russell TR, Bechamps GJ, et al. Surgeon distress as calibrated by hours worked and nights on call. J Am Coll Surg. 2010;211:609–19. doi: 10.1016/j.jamcollsurg.2010.06.393. [DOI] [PubMed] [Google Scholar]
- 11.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–97. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 13.Riachy M, Juvelikian G, Sleilaty G, Bazarbachi T, Khayat G, Mouradides C. [Validation of the Arabic version of the Epworth Sleepiness Scale: Multicenter study] Rev Mal Respir. 2012;29:697–704. doi: 10.1016/j.rmr.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 14.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–81. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 15.Ghareeb AG. Manual of Arabic BDI-II. Cairo, Egypt: Angle Press; 2000. [Google Scholar]
- 16.Alansari BM. Internal consistency of an Arabic adaptation of the Beck Depression Inventory-II with college students in eighteen Arab countries. Soc Behav Pers. 2006;34:425–30. doi: 10.2224/sbp.2006.34.4.425. [DOI] [Google Scholar]
- 17.Baldwin DC, Jr, Daugherty SR. Sleep deprivation and fatigue in residency training: Results of a national survey of first- and second-year residents. Sleep. 2004;27:217–23. doi: 10.1093/sleep/27.2.217. [DOI] [PubMed] [Google Scholar]
- 18.Wali S, Abushanab L, Quotah K, Krayem A. Effect of on-call related sleep deprivation on physicians’ mood and level of alertness. Chest. 2011;140:809A. doi: 10.1378/chest.1117573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wada K, Yoshikawa T, Goto T, Hirai A, Matsushima E, Nakashima Y, et al. National survey of the association of depressive symptoms with the number of off duty and on-call, and sleep hours among physicians working in Japanese hospitals: A cross sectional study. BMC Public Health. 2010;10:127. doi: 10.1186/1471-2458-10-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosta J, Gerber A. Excessive working hours and health complaints among hospital physicians: A study based on a national sample of hospital physicians in Germany. Ger Med Sci. 2007;5:Doc09. [PMC free article] [PubMed] [Google Scholar]
- 21.Goebert D, Thompson D, Takeshita J, Beach C, Bryson P, Ephgrave K, et al. Depressive symptom in medical students and residents: A multischool study. Acad Med. 2009;84:236–41. doi: 10.1097/ACM.0b013e31819391bb. [DOI] [PubMed] [Google Scholar]
- 22.Khuwaja AK, Qureshi R, Azam SI. Prevalence and factors associated with anxiety and depression among family practitioners in Karachi, Pakistan. J Pak Med Assoc. 2004;54:45–9. [PubMed] [Google Scholar]
- 23.Al-Harby NM. Prevalence of Depression and its Associated Factors among Physicians in the Primary Health Care Centers, Jeddah, Saudi Arabia. From: www.ssfcm.org/public/english/Artical/index/secid/867/artid/1748#1748 Accessed: Feb 2014.