Abstract
Objective
To test the effectiveness of a trauma-specific psycho-educational intervention for pregnant women with a history of childhood maltreatment on six intrapartum and postpartum psychological outcomes.
Design
Quasi-experimental study comparing women from a single-group pretest-posttest pilot intervention study with women matched from a prospective observational study.
Setting
Rural and university-based prenatal clinics.
Participants
Pregnant women entered the study by responding to an advertisement or by referral from a maternity care provider. Women could take part whether or not they met posttraumatic stress disorder diagnostic criteria. Outcomes data exist for 17 pilot intervention study participants and 43 matched observational study participants.
Interventions
Participants in the observational study received usual care. Participants in the pilot intervention study received usual care plus the intervention, a fully manualized self-study program supported by weekly phone tutoring sessions with a health professional.
Main Outcome Measures
The National Women’s Study PTSD Module; The Peritraumatic Dissociation Experience Questionnaire); The Perception of Care Questionnaire; The Postpartum Depression Screening Scale; The Postpartum Bonding Questionnaire; and a semantic differential appraisal of the labor experience.
Results
Participants in the intervention study had better scores on all measures. Differences in means between participants in the intervention study and participants in the observational study equated to medium effect sized for dissociation during labor, rating of labor experience, and perception of care in labor, and small effect sizes for postpartum PTSD symptoms, postpartum depression symptoms, and mother-infant bonding.
Conclusion
This trauma-specific intervention reaches and benefits pregnant women with a history of childhood maltreatment.
Keywords: Primary mental health care, pregnancy, posttraumatic stress, psychoeducation, perinatal
Introduction
Post-traumatic stress disorder (PTSD) is an anxiety disorder that develops after an experience of a psychologically traumatic event. It is characterized by intrusive reminders of the event such as nightmares and flashbacks, avoidance of stimuli associated with the event, persistent negative cognitions and numbing of responses, and symptoms of anxiety, including hyper-vigilance, difficulty concentrating, irritability, and sleep disturbances. PTSD is associated with substantial distress and impairment in functioning (5th ed.; DSM-V; American Psychiatric Association, 2013). Epidemiological evidence consistently shows that, as for depressive disorders and other anxiety disorders, women are twice as likely as men to develop PTSD during their lifetimes (10.4% versus 5.0%) (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). The disparity is likely to be because of gender differences in the traumatic exposures, combined with psychological and biological differences in stress responses (Olff, Langeland, Draijer, & Gersons, 2007).
The lifetime prevalence of PTSD among US women generally is 12.3% and point prevalence is 4.6% (Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). A growing body of literature confirms that PTSD is twice as common during pregnancy. For example, the estimated prevalence of current (past month) PTSD in diverse samples of English-speaking pregnant women in the United States was 7.9% (Seng et al., 2010). In Australia it was 8.0% (Alcorn, O’Donovan, Patrick, Creedy, & Devilly, 2010). Demographic risk factors in the US sample included younger age, African American race, poverty, low levels of education, and high exposure to crime. Women who had experienced trauma were less likely to have current PTSD if they experienced fewer sociodemographic risks (Seng, Low, Sperlich, Ronis, & Liberzon, 2009).
PTSD during pregnancy is of clinical importance because it is associated with risk behaviors such as smoking, alcohol consumption, substance use, poor prenatal care, and excessive weight gain (Morland et al., 2007), as well as poor obstetric outcomes, including lower birth weight and shorter gestation (Rogal et al., 2007; Seng, Low, Sperlich, Ronis, & Liberzon, 2011). PTSD is frequently co-morbid with depression, panic disorder, and thoughts of self-harm during pregnancy (Smith, Poschman, Cavalier, Howell, & Yonkers, 2006), and is associated with postpartum depression and impaired mother-infant bonding (Seng et al., 2013).
Compared with other antecedent trauma exposures, childhood maltreatment, including sexual, physical, and emotional abuse or neglect, conveys the most increased risk (12-fold) of PTSD in pregnancy (Seng et al., 2009). Pregnant women with childhood abuse histories are more likely to be symptomatic than women with other kinds of trauma exposure because of the psychosexual nature of pregnancy and pregnancy care, including bodily changes, intrusive examinations, and the interpersonal difficulties exacerbated by power disparities between women and their health care providers (American College of Obstetricians and Gynecologists, 2001). Pregnant women with PTSD must manage their symptoms in the presence of triggers to arousal, such as fetal movement, vaginal and breast examinations, preparation for the demands of labor, birth, breastfeeding, and infant care. Together, these circumstances place great demands on a woman’s psychological resources (Simkin and Klaus 2004).
The range of psychological, behavioral, interpersonal, and physical aspects of childbearing suggest the need for additional support during prenatal care for women experiencing PTSD subsequent to childhood maltreatment. However, engaging women in evidence-based standard mental health treatments during pregnancy is challenging. Women experiencing anxiety or depressive symptoms during the perinatal period do not necessarily consider themselves mentally ill, and many find referral to specialist psychiatric services stigmatizing (Kelly, Zatzick, & Anders, 2001; Goodman and Tyler-Viola 2010). Most psychotherapy treatments for PTSD are trauma-focused and require emotional engagement (Foa, Keane, Friedman, & Cohen, 2008). The necessary psychological resources for successful treatment are likely to exceed those available in the context of elevated biopsychosocial stressors of childbearing (Kelly et al., 2001; Goodman and Tyler-Viola 2010).
Questions remain about the safety of exposure-based cognitive behavioral therapies during pregnancy (Arch, Dimidjian, & Chessick, 2012). Similarly, the use of medications to treat PTSD during pregnancy, including selective serotonin reuptake inhibitors, needs careful consideration of costs and benefits because of controversies about their potential impact on fetal development (Byatt, Deligiannidis, & Freeman, 2013; Ross et al., 2013). Women’s preferences for non-pharmaceutical treatments (Battle, Salisbury, Schofield, & Ortiz-Hernandez, 2013) and the known risk of untreated anxiety disorders to fetal and child development (O’Connor, Heron, & Glover, 2002) confirm the need for non-pharmacological resources for women with PTSD during pregnancy, particularly those that do not require exposure to traumatic reminders and are suitable for use in maternity care and social work settings.
There is limited evidence for PTSD treatment in pregnancy. However, Zlotnick, Capezza, and Parker (2011) developed a primary care treatment intervention to address depression and PTSD in low-income pregnant women with recent experience of intimate partner violence. The scripted intervention consists of five sixty-minute individual sessions during pregnancy, and up to two weeks postpartum, offered by trained, supervised staff. Principles of Interpersonal Psychotherapy are employed to assist women in improving interpersonal relationships, mobilizing social support, and adjusting to motherhood. Fifty-four women participated in a randomized controlled trial to test the intervention. The program was found to be feasible and acceptable. Participants who received the treatment experienced a reduction in symptoms of depression and PTSD compared with controls. Secondary analyses showed a moderate effect on reduction in depressive symptoms. However, there was a large effect on PTSD symptoms for women with histories of childhood sexual abuse and rape compared with women in the control condition. This effect suggests that interventions during pregnancy specifically targeting PTSD secondary to childhood sexual abuse rather than recent intimate partner violence may be beneficial.
Psychoeducation is a professionally delivered treatment modality for use in clinical and community settings. Psychoeducation has three components: condition-specific information, skills training for managing challenging circumstances, and emotional support. Structured psychoeducational programs, which usually emphasize health, collaboration, competency, and empowerment, are designed to be delivered by non-psychiatric clinicians who have been trained in program delivery. Programs are strengths-based and present-focused. There is evidence of effectiveness of psychoeducational programs in a range of applications in physical and mental health (Lukens & McFarlane, 2004), including for PTSD. For example, in a group of 58 women with PTSD subsequent to childhood maltreatment, those randomly assigned to a manualized eight-week program of skills training in affect and interpersonal regulation showed significant improvements in affect regulation, interpersonal deficits, and PTSD symptoms, compared with the minimal-attention wait-list control (Cloitre, Koenen, Cohen, & Han, 2002). The psychoeducational program included education about the rationale and goals of each session, skills acquisition, and application to current life circumstances, as well as between-session skills practice.
The Survivor Moms’ Companion (SMC) is a psychoeducational program for women survivors of childhood maltreatment who are pregnant, a time when pharmacological or exposure-based treatment may not be suitable. The SMC is a primary care, fully manualized, ten module, self-study and structured-listening program designed to be broadly available. It is congruent with the integrated primary mental health care (IPMHC) model which provides front-line, primary care interventions such as psychoeducation. It also provides case-finding for the estimated 10% to 15% of people who will also benefit from referral for treatment with medication or psychotherapy (Blount, 1998). The SMC follows extensive qualitative work, which investigated the experiences and needs of pregnant survivors of childhood maltreatment (Sperlich & Seng, 2008). It is based on psychoeducational components used in other evidence-based PTSD treatments (Cloitre et al., 2010). The SMC program is designed to be a 10-week self-study program structured with workbook modules that the woman works on to prepare for a 30-minute structured telephone consultation with a tutor—a trained perinatal nurse or social worker. Women are referred by a maternity care team member or can self-refer based on childhood maltreatment history, and the intervention is intended to assist women whether or not they meet PTSD diagnostic criteria. A full description of the program is published elsewhere (Seng et al., 2011; Sperlich et al., 2011).
Consistent with the IPMHC model, the goal of the SMC is to improve obstetric, postpartum, and early parenting experiences, as well as psychological functioning. Individual modules are designed to target three mechanisms: 1) Affect dysregulation, characterized by both emotional numbing (diminished intensity of sensations and emotions, low emotional awareness and mood) and irritability (low threshold to anger associated with chronic autonomic hyper-arousal); 2) Interpersonal reactivity, or difficulties interpreting other people’s intentions, leading to heightened offense from negative attribution, low trust, low self-esteem, problems establishing boundaries, and fears of intimacy; 3) PTSD symptom management in the presence of physical and psychological triggers and heightened dependency on others during pregnancy (Seng et al., 2011). Program content provides situation-specific skills practice to manage maternity care and promote positive infant relationships. In the pilot test of the SMC, the feasibility, safety and acceptability were confirmed (Sperlich et al., 2011), and scores on all three target mechanisms improved (Seng et al., 2011).
The purpose of this study was to conduct a preliminary quasi-experimental analysis of the influence of the SMC PTSD psychoeducational intervention on six outcomes. We hypothesized that compared with women matched from a prospective study who did not receive the SMC, women who participated in the pilot of the intervention will have better scores on six key outcomes, indicating less dissociation in labor, more favorable appraisal of their labor experience and the care they received from the physician or midwife, fewer PTSD and depression symptoms postpartum, and more optimal bonding with their infants. Results of these hypothesis tests will be used to generate effect size estimations to inform the power calculation for a protocol for future research.
Methods
We compared women from a single-arm open pilot study (BCBSMF Grant NR008767) who participated in the SMC psych-educational intervention with women who did not receive the program, matched from a prospective observational study, known as the STACY Project, conducted by the same team (NIH R01 NR006787, PI Seng). Eligible women in both studies were 18 or older, initiating prenatal care at less than 28 completed weeks gestation, and able to speak English without an interpreter. Institutional Ethics Review Boards approved both studies, and informed consent to participate was obtained from participants at enrollment.
Overview of the observational study
The observational study was a prospective cohort (n=1,049) investigation of the effects of PTSD on childbearing outcomes, including experience of labor, symptoms of postpartum depression and PTSD, and impaired mother-infant bonding (Seng et al., 2013). Three cohorts were enrolled: lifetime PTSD cases, trauma-exposed (resilient) controls, and non-exposed controls. Women were assigned to the lifetime PTSD case group based on trauma history and meeting the DSM-IV PTSD symptom cluster diagnostic criteria; this required having at least 6 symptoms, including at least 1 re-experiencing, 3 numbing and avoidance, and 2 arousal symptoms. Women were assigned to the trauma-exposed control group if they did not meet the PTSD cluster diagnostic criteria and had fewer than 5 total PTSD symptoms. They were assigned to the non-exposed control group if their trauma history did not meet DSM-IV criteria and they also had fewer than 5 PTSD symptoms. Women who did not fit any of these three cohort definitions were not enrolled. Structured psychiatric diagnostic interviews were conducted by telephone at three time points: early- to mid-pregnancy when the woman initiated prenatal care (baseline), late gestation, and six weeks postpartum (outcome). Five hundred and sixty six women (54% retention) completed the postpartum interview (Seng et al., 2013).
In the observational study, analysis of the postpartum data showed that women with PTSD scored statistically significantly worse on all outcomes of interest, except their global appraisal of their labor experience. The trauma-exposed but resilient control group scored better than the PTSD cases, but worse than the non-exposed control group. Thus, the SMC was developed as an intervention for childhood maltreatment survivors, whether or not they met PTSD diagnostic criteria.
Overview of the pilot SMC intervention study
The SMC intervention is a fully-manualized 10-module self-study psychoeducational program including a 30-minute telephone consultation with a trained health professional tutor as part of each module. The first 4 modules are regarded as “core,” and considered to be the minimum “dose”. Completion of modules is recorded by the tutor during the telephone tutoring session. Fidelity to the manual during the sessions is measured having both the tutor and the participant complete fidelity checklists which are returned to the research team and compared for their agreement as a means to motivate accurate reporting of session process and content (Bellg et al, 2004).
We conducted a single-group pretest-posttest pilot of the SMC. The Phase 1 (safety, feasibility, and acceptability) and Phase 2 (pre- to post-test change in mechanisms) reports have been published (Seng et al., 2011; Sperlich et al., 2011). We review those findings briefly here. Women with a history of childhood maltreatment were recruited between May 2008 and July 2010 from rural and university-area prenatal clinics via clinician- or self-referral. Consistent with norms for trials of PTSD interventions (Spinazzola, Blaustein, & van der Kolk, 2005), exclusion criteria addressed safety and included active psychotic disorders, untreated substance abuse, past year suicide attempts, intimate partner or parent abuse not addressed by social services, or high-risk pregnancy conditions requiring perinatologist care, psychotropic medication, and current engagement in long-term individual psychotherapy, but not completed therapy.
Participants were offered the SMC program conducted by a trained tutor. The same structured telephone interviews and assessment points used in the observational study were conducted at the time of recruitment during mid-pregnancy (baseline), and at 6 weeks postpartum (outcome). Thirty-two women were enrolled in the intervention.
Intention-to-treat analysis of the pretest-to-posttest change in scores indicated that improvements occurred on all of the targeted mechanisms except negative mood (affect) regulation (Seng et al., 2011). Results of the pilot intention-to-treat analysis indicate the intervention improved scores on PTSD symptom levels, interpersonal reactivity, and anger (affect) regulation. The next question was whether these “mechanism” improvements also improve outcomes.
Quasi-experimental study
Use of the same baseline and outcome measures in both the STACY study and the SMC pilot study provides an opportunity to estimate effect sizes of differences in outcomes that could be attributable to the intervention. This quasi-experiment tests the hypothesis that the intervention group will have better scores on six outcomes assessed postpartum than matched women who completed these measures as part of the STACY study, but did not participate in the SMC. The outcomes were three indicators of the labor experience (overall appraisal, dissociation, perception of care) and three indicators of postpartum status (PTSD symptoms, depression symptoms, impaired bonding).
Matching
Participants from the STACY study were selected for matching if they met the pilot SMC intervention study inclusion criterion of a history of childhood maltreatment. This was defined as physical, sexual, or emotional abuse or physical neglect prior to age 16 (n=261). Participants were matched on their number of sociodemographic risk factors for PTSD and on lifetime PTSD diagnostic status (yes versus no), based on the symptoms they reported in the diagnostic interview. The following sociodemographic (SES) factors increase risk for having PTSD: young age, low education, poverty, African American race, and living in a high crime area (Seng et al., 2009). For this quasi-experiment, we used a cumulative SES risk index (0–5) based on being pregnant as a teen, having high school education or less, having household income less than USD15,000, being African American, and living in a zip code with a crime rate higher than the U.S. average (SimplyMap, 2009). We matched women based on whether they had 0–1 versus 2 or more of these sociodemographic PTSD risk factors. Based on the relative proportions of observational and pilot study participants with the two matching criteria, and to maximize power for a quasi-experimental statistical analysis, matching was based on a 1:3 ratio, that is 1 SMC pilot (case) to 3 observational (control) women (Ming & Rosenbaum, 2000). We used a SAS macro from the Mayo Clinic Research Website called “vmatch,” choosing the “optimal” algorithm (Bergstralh & Kosanke, 2003). The 32 enrolled pilot intervention study participants were matched with 96 enrolled STACY study participants. The “as matched” enrolled samples are described in Table 1 in the left columns. A total of 65 women (43 in the STACY study and 22 in the pilot) completed the outcome interview. Five women from the pilot study with outcome data did not complete the first 4 (core) modules of the SMC. They were included in the open pilot intention-to-treat analyses. But they were excluded from these outcome analyses, leaving n=17 in the intervention group. Thus, the combined sample size for this quasi-experimental analysis “at outcome” is 60 women, described in Table 1 in the right columns.
Table 1.
Sample profiles of Observation Study and Open-pilot (Intervention) Study groups, as matched and at outcome.
| Comparison of groups AS MATCHED (n=128) | Comparison of groups AT OUTCOME (n=60) | |||||
|---|---|---|---|---|---|---|
| Observation Group, n=96 | Intervention Group, n=32 | p | Observation Group, n=43 | Intervention Group, n=17 | p | |
| Demographics | % (n) | % (n) | % (n) | % (n) | ||
| African American | 65.6% (63) | 25.0% (8) | <.001 | 48.8% (22) | 29.4% (5) | .127 |
| European American | 28.1% (27) | 65.6% (21) | <.001 | 41.9% (18) | 58.8% (10) | .235 |
| Hispanic/Latina | 2.1% (2) | 3.1% (1) | .801 | 0% (0) | 0% (0) | n/a |
| Asian/Pacific Islander | 3.1% (3) | 3.1% (1) | 1.00 | 2.3% (1) | 5.9% (1) | .489 |
| Native American/Alaskan | 3.1% (3) | 15.6% (5) | .011 | 2.3% (1) | 5.9% (1) | .489 |
| Poverty | 41.7% (40) | 53.6% (15) | .265 | 25.6% (11) | 42.9% (6) | .220 |
| Partnered | 38.5% (37) | 37.5% (12) | .916 | 55.8% (24) | 29.4% (5) | .065 |
| Low education | 68.8% (66) | 78.1% (25) | .311 | 53.5% (23) | 70.6% (12) | .226 |
| Trauma History | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Child Abuse | 2.01 (1.22) | 3.34 (1.33) | <.001 | 1.98 (1.22) | 3.00 (1.41) | .007 |
| Adult Abuse | 0.68 (0.86) | 1.16 (1.17) | .038 | 0.84 (0.92) | 1.45 (1.35) | .142 |
| Other Trauma | 6.50 (3.33) | 8.16 (3.35) | .016 | 5.98 (3.60) | 7.29 (2.57) | .175 |
| Diagnoses | % (n) | % (n) | % (n) | % (n) | ||
| Lifetime PTSD | 75.0% (72) | 75.0% (24) | 1.00 | 74.4% (32) | 76.5% (13) | .869 |
| Current PTSD | 35.4% (34) | 34.4% (11) | .915 | 30.2% (13) | 29.4% (5) | .950 |
| Past Year MDD | 34.4% (33) | 50.0% (16) | .115 | 39.5% (17) | 52.9% (9) | .345 |
| Symptoms | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Dissociation | 2.35 (3.61) | 4.34 (5.54) | .064 | 2.58 (4.00) | 3.45 (3.18) | .633 |
| Interpersonal sensitivity | 8.85 (7.30) | 13.53 (8.71) | .003 | 7.02 (5.97) | 12.76 (8.35) | .004 |
| Risk Behaviors | % (n) | % (n) | % (n) | % (n) | ||
| Pregnancy smoking | 26.0% (25) | 62.5% (20) | <.001 | 27.9% (12) | 64.7% (11) | .025 |
| Pregnancy drinking | 17.7% (17) | 37.5% (12) | .021 | 23.3% (10) | 47.1% (8) | .070 |
| Illicit drug use | 11.5% (11) | 12.5% (4) | .874 | 18.6% (8) | 11.8% (2) | .522 |
| Past year IPV | 8.3% (8) | 12.5% (4) | .484 | 9.3% (4) | 11.8% (2) | .774 |
| Treatment History | % (n) | % (n) | % (n) | % (n) | ||
| Prior therapy | 36.5% (35) | 78.1% (25) | <.001 | 44.2% (19) | 64.7% (11) | .152 |
| Prior medication | 21.9% (21) | 62.5% (20) | <.001 | 34.9% (15) | 52.9% (9) | .198 |
| Current therapy | 7.3% (7) | 23.3 (7) | .015 | 11.6% (5) | 40.0% (6) | .016 |
| Current medication | 5.2% (5) | 13.3% (4) | .131 | 11.6% (5) | 13.3% (23) | .861 |
Abbreviations: PTSD, Posttraumatic Stress Disorder MDD, Major Depressive Disorder; IPV Intimate Partner Violence.
Data collection
The six outcomes for the quasi-experimental comparisons are from the postpartum interview and include appraisal of labor experience and scales that measure dissociation in labor, appraisal of care received from the physician or midwife, postpartum PTSD symptoms, postpartum depression symptoms, and impaired mother-infant bonding. The baseline interview included established diagnostic interviews to assess trauma history, PTSD, depression, affect dysregulation, and interpersonal reactivity-associated features of PTSD, risk behaviors, and demographics. Study-specific items assessed treatment history, including use of individual psychotherapy or medication for mental health problems ever in the past and in the current pregnancy.
Measures
Background or baseline characteristics
The Life Stressor Checklist (LSC) (Wolfe & Kimerling, 1997) assesses 30 potentially traumatic events specific to women’s experiences. Formal validation of trauma history cannot occur without corroboration of actual events. There is however expert consensus criteria for item characteristics to elicit the most valid and reliable responses: behaviorally specific questions, non-legal language and a comprehensive list of traumatic events, tailored to the target population, which the LSC meets (Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). It has the highest sensitivity of the five most common trauma research instruments (Cusack, Falsetti, & de Arellano, 2002).
The Abuse Assessment Screen (McFarlane, Parker, Soeken, & Bullock, 1992) assessed past-year intimate personal violence. This measure is designed for use with pregnant women and its sensitivity is regarded as good because it yields higher prevalence estimates than other screening measures.
The National Women’s Study PTSD Module (NWS PTSD) assessed PTSD according to DSM-IV criteria. Assessment of past and current diagnoses has high sensitivity (0.99) and specificity (0.79) validated against face-to-face Structured Clinical Interview (Resnick et al., 1993; Kilpatrick et al, 1994). It measures all 17 symptoms of PTSD and assesses distress and impairment. In the STACY Project the internal consistency coefficient for the 17 items used as a scale was .88 (Kulkarni, Graham-Bermann, Rauch, & Seng, 2011), and in this sample was .72.
The Composite International Diagnostic Interview short form (CIDI) (Wittchen, 1994) was used to assess past year major depressive disorder. The CIDI is a structured psychiatric diagnostic tool designed to be used by trained interviewers who are not clinicians, and is supported by extensive field trial data on cross-national reliability and validity.
Perinatal Risk Assessment Monitoring Survey (PRAMS), an epidemiologic surveillance instrument created by the Centers for Disease Control and Prevention (Beck et al, 2002) assessed demographic indicators (income, education, race/ethnic identity), and health risk behaviors, including quantitative assessment of substance use during pregnancy.
Outcomes
Dissociation in labor
The Peritraumatic Dissociation Experience Questionnaire (PDEQ) (Marmar, Weiss, & Metzler, 1997) score assessed dissociative symptoms experienced during labor. This 10-item scale is widely used in prospective studies of risk for PTSD in the aftermath of potentially traumatic, overwhelming experiences (Birmes et al., 2005). It assesses experiences of distortion in sense of time and feeling disoriented, confused, or disconnected from the body on a five-point Likert scale (Marmar et al., 1997). Internal consistency reliability was .82 when used in relation to labor in the STACY Project (Seng et al., 2013) and .87 in this sample.
Labor experience
We used a single semantic differential item to ask the woman to appraise her experience of labor on a scale from 1 (horrible) to 10 (wonderful).
Perception of care
The Perception of Care Questionnaire (PCQ) (Creedy, 1999; Fisher, 1994) has 22 items assessing women’s perception of the quality professional care received during labor and birth. Higher score represents perception of better care. High internal reliability was reported (.90 and .96) for two phases of the instrument development study (Fisher, 1994). Internal consistency reliability was .91 when used in the STACY Project (Seng et al., 2013) and .89 in this sample.
PTSD Symptoms
The National Women’s Study PTSD Module (NWS PTSD) was described above.
Postpartum depression symptoms
The Postpartum Depression Screening Scale (PDSS) has 35 items assessing depression symptoms. It was validated on a normative sample. A cut-off score of 80 has a positive predictive value of 93% for major depressive disorder (Beck & Gable, 2002). In the STACY Project the Cronbach’s alpha coefficient was .95 (Seng et al., 2013).
Bonding impairment
The Postpartum Bonding Questionnaire (PBQ) (Brockington et al., 2001) is a 25-item clinical screening measure to assess impaired bonding. Higher score represents more impaired bonding. We omitted the 2 items querying incipient abuse of the infant (Scale 4) which appear too invariant and unreliable (Wittkowski, Wieck, & Mann, 2007). In the STACY Project the Cronbach’s alpha coefficient was .83 (Seng et al., 2013) and .76 in this sample.
Data management
Data were entered and analyzed in SPSS. All standardized measures yielded scores which were used as interval-level variables. Data reduction techniques were used to create trauma history variables (childhood maltreatment occurred, yes or no; sum of types of childhood maltreatment; adult victimization occurred, yes or no; sum of types of adult victimization). The total crime score was dichotomized to higher or lower crime area based on whether residential postal code’s crime rate was above or below the U.S. average using the Federal Bureau of Investigation crime report for ZIP code (Matching zip codes to FBI crime rates).
Analysis
Preliminary steps in data analysis included assessments of missing data, reliability of outcome measures, and assessment of descriptive statistics to verify that these variables met assumptions for parametric testing. Mean scores on outcome measures were compared using the STACY study group mean as the reference point. Effect sizes of the differences are reported as Cohen’s d and effect size r. We set the criterion for interpreting significance at p<.1, preferring to risk Type I error in this preliminary quasi-experimental analysis. The percentage difference in mean scores for intervention compared to observational group was calculated for each outcome.
Results
Descriptive analysis of the outcome variable scales indicated that all distributions approximated normal except for the PDEQ score, which was strongly skewed with a mode of reporting no symptoms. Assumptions for parametric testing of the PDEQ were verified by a normal distribution in the error variance, using standardized residuals in a linear regression with PTSD symptoms as a predictor.
Characteristics of the sample
The matching procedure obtained a 1:3 case-to-control ratio, resulting in a sample of 128 women with baseline data. Women who enrolled in the intervention study (n=32) were significantly less likely to be African American and more likely to be European American or Native American. They also had more trauma exposures, higher dissociation and interpersonal sensitivity scores, greater use of tobacco and alcohol in pregnancy, had more treatment and medication use in their history, and more use of psychotherapy during pregnancy (generally a therapy initiated by referral since the start of prenatal care) (Table 1, left columns). Retention was 45% in the observation group and 69% in the intervention group. The intervention group differed from the observation group only in that they were more likely to be unpartnered, to have a great number of types of childhood maltreatment trauma, greater interpersonal sensitivity scores, more smoking and alcohol use during pregnancy, and more current psychotherapy (Table 1, right columns).
Hypothesis tests
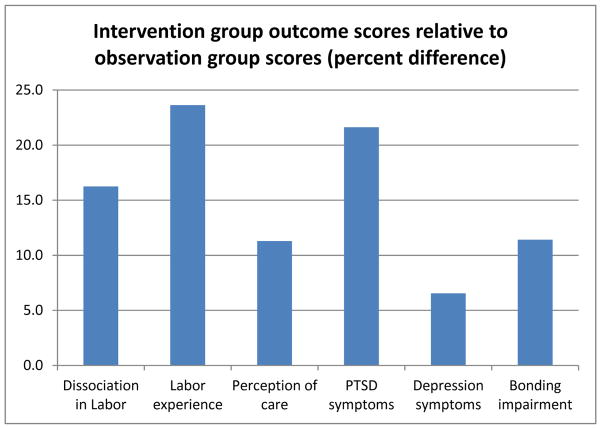
Mean scores on all six outcome measures favored the intervention group compared with the observation group (Table 2). This difference only reached statistical significance for two of the labor experience measures, dissociation in labor (PDEQ) (t = 1.86, df 55, p = .07) and the perception of care (PCQ) (t = −2.13, df 58, p = .04). Scores on dissociation in labor, overall labor experience, and postpartum PTSD each showed scores that were 15% better than the scores in the observation group. The smallest difference (7%) was in the postpartum depression score. Figure 2 depicts these differences by showing in a bar graph the intervention group’s outcome scores (percent higher or better as bars) relative to the observation group’s mean scores (as 0 on the Y axis).
Table 2.
Effect sizes of intervention participation (>=4 modules) on labor and postpartum outcomes
| Outcome | Observation group n=43
|
Intervention group n=17 | P | Cohen’s d | Effect size r | Variance explained | Effect size | ||
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | SEM | M (SD) | SEM | ||||||
| PDEQ score | 16.0 (7.1) | 1.1 | 13.4 (3.5) | 0.8 | .07 | .46 | .23 | 5% | medium |
| Labor rating | 5.5 (2.8) | 2.2 | 6.8 (2.8) | 0.7 | .14 | .47 | .23 | 5% | medium |
| PCQ score | 54.9 (9.3) | 1.4 | 61.1 (11.9) | 2.9 | .04 | .58 | .28 | 8% | medium |
| PTSD symptoms | 3.7 (2.9) | 0.4 | 2.9 (2.6) | 0.6 | .34 | .33 | .16 | 3% | small |
| PDSS score | 73.3 (19.7) | 3.0 | 68.5 (22.4) | 5.4 | .41 | .23 | .11 | 2% | small |
| PBQ score | 18.4 (6.5) | 1.0 | 16.3 (6.7) | 1.6 | .26 | .35 | .17 | 3% | small |
Abbreviations: PDEQ, Peritraumatic Dissociation Experiences Scale: PCQ, Perception of Care Questionnaire; PTSD, Posttraumatic Stress Disorder; PDSS, Postpartum Depression Screening Scale; PBQ, Postpartum Bonding Questionnaire.
Effect sizes
The final purpose of this quasi-experimental analysis was to estimate effect sizes of the group differences for future research (Table 2). The difference on PCQ scores had the largest effect size, with a Cohen’s d of .58, which is considered to be of a medium size (Cohen 1988), explaining 8% of variance. The difference in group scores on the PDSS had the smallest effect size, with a Cohen’s d of .23, which is considered small (Cohen, 1988), explaining 2% of variance.
Discussion
This study was a preliminary assessment of the novel, psychoeducational SMC program, which focuses on management of PTSD symptoms in pregnant women. We specifically examined the SMC program’s effect on the labor, birth, and postpartum experiences of participants. The quasi-experimental method employed a systematically-collected dataset to provide a matched comparison sample to assess effect sizes on standardized assessments of six outcomes of interest. The study has a number of strengths, including successful recruitment and retention of a group of vulnerable women to participate in a psychoeducational program and additional research interviews, the use of standardized measures, and the availability of a large comparison dataset collected by the same research group. There was, however, less than optimal retention to follow-up. This is likely to be because of the vulnerability of the women recruited to the studies, though may be due in part to burden of repeated research interviews. Drop-out from the intervention was consistent with that of other PTSD psychoeducation trials (e.g., Cloitre et al, 2002). The results should be interpreted with caution because of potential attrition bias, but they show that participation in the SMC program compared favorably with standard care on all outcomes, including experience of dissociation in labor; appraisal of labor experience and care received from the physician or midwife, postpartum PTSD and depression symptomatology, and mother-infant bonding. The results also yield important considerations for planned future intervention trials.
It is noteworthy that five of the women who had outcomes data did not complete the four core modules of the SMC and were excluded in the quasi-experimental analyses. These women experienced exacerbation of their PTSD symptoms at the assessment conducted after the second SMC module, suggesting that psychoeducation might need to take place in the context of specialty treatment for the approximately 20% of women more severely affected by PTSD symptoms. This finding has been addressed in a modification to the SMC protocol, which now includes a self-assessment and in-depth informed consent process to assist women in assessing whether the SMC by itself is a good “fit” for their needs, or if they would benefit from using it in the context of specialty care or at another time. This protocol prompts women to consider if they have the emotional support, time, and resources to participate in the program successfully.
It appears that the intervention is reaching women who need and can benefit from it. The characteristics of the women who did complete four or more of the SMC modules appear similar to those of the observation study sample, with the exception that the women in the SMC group seem to have more psychosocial needs, including being single, greater abuse history, and more affect dysregulation, interpersonal reactivity, and substance use. The SMC group’s greater likelihood of starting therapy during pregnancy should be adjusted for in statistical modeling in a future study.
The effect sizes were larger for the outcomes related to labor and delivery, including dissociation in labor, and appraisal of the labor experience and care during labor, than the postpartum outcomes. The smaller effect sizes for postpartum PTSD, depression and bonding outcomes suggests the need for continued psychoeducation after the birth in order to provide life stage-specific reinforcement of the material related to PTSD and depressive symptomatology. The effect size for the depression score was the smallest, which is consistent with the open pilot finding that participation in the SMC had little effect on the “Negative Mood Regulation” mechanism score from pre- to post-test periods (Seng et al., 2011). This may indicate the limit of this psychoeducational approach for managing depressive symptoms. The STACY study findings show that compromised maternal-infant bonding is most strongly associated with depression when it is comorbid with PTSD (Seng et al., 2013). Despite the small effect size of the impact on maternal postpartum depression in the intervention study, the mother-infant-bonding score was better for women who received the intervention, suggesting that anticipatory guidance about the relationship with the infant and the interpersonal reactivity “interpreting skills” in the SMC may have been helpful, even if the SMC’s impact on depression itself was small.
The effects of maternal PTSD exposure on offspring are well-documented (Yehuda, Halligan, & Bierer, 2001; Yehuda, Engel, Brand, Seckl, Marcus, & Berkowitz, 2005) and represent intergenerational transmission of abuse and psychiatric vulnerability. However, gene-by-environment research has demonstrated that it is possible to break this cycle, both biologically and behaviorally (Meaney, 2010). The SMC aims to help women manage pregnancy, labor and adjustment to motherhood more successfully, with the goal of interrupting intergenerational transmission of the effects of childhood maltreatment. This quasi-experimental analysis confirms that the SMC has the potential to assist vulnerable pregnant women with trauma-related posttraumatic stress. However, the efficacy of the SMC remains to be tested in a methodologically-robust trial. The effect size analysis reported here will inform the sample size protocol for a planned randomized trial.
Clinical implications
These preliminary findings have potential implications for nurses who provide care in obstetric settings. This trauma-specific prenatal intervention appeared to provide benefit in terms of improved labor experience, less postpartum PTSD, a slight attenuation of postpartum depression, and less bonding impairment. This represents a feasible intervention that is within the scope of practice of nurses in prenatal settings. The availability of an intervention to offer would enhance the utility of screening for trauma history and PTSD. Screening, offering psychoeducation, and cultivating referral resources for pregnant women with a maltreatment history would be an approach consistent with emerging models of trauma-informed care (“Trauma-Informed Care,” 2014). The relatively small effect sizes of the SMC on mood and parental bonding suggest, however, that women screening positive for depression should also be offered an evidence-based therapy for management of depressive symptoms (NICE Guidelines, 2007) and receive active anticipatory guidance and practical assistance to optimize the mother-infant relationship.
Figure 1.
Callouts.
Posttraumatic stress disorder (PTSD) affects 8% of pregnant women. The biggest risk factor for PTSD in pregnancy is a history of childhood maltreatment.
Front-line, evidence-based PTSD interventions for pregnant women that help navigate maternity care, labor, breastfeeding, and the early weeks of parenting are needed.
Women who used the Survivor Moms’ Companion intervention had better labor experience, postpartum mental health, and bonding. An adequately powered randomized controlled trial is warranted.
Acknowledgments
Financial support
Financial support for the studies was received from Blue Cross and Blue Shield Foundation of Michigan, and from the National Institutes of Health, National Institute for Nursing Research grant NR008767 (Seng, P.I.), “Psychobiology of PTSD & Adverse Outcomes of Childbearing.”
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Contributor Information
Heather Rowe, Jean Hailes Research Unit, School of Public Health & Preventive Medicine, Monash University, Melbourne, Victoria, Australia.
Mickey Sperlich, School of Social Work, Wayne State University, Detroit, Michigan.
Julia S. Seng, School of Nursing, Institute for Research on Women and Gender, Department of Obstetrics & Gynecology, and Department of Women’s Studies, University of Michigan, Ann Arbor, MI.
References
- Alcorn KL, O’Donovan A, Patrick JC, Creedy D, Devilly GJ. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychological Medicine. 2010;40(11):1849–1859. doi: 10.1017/S0033291709992224. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists. ACOG (American College of Obstetricians and Gynecologists) educational bulletin. Adult manifestation of childhood sexual abuse. Number 259, July 2000. Clinical management guidelines for obstetrician-gynecologists. International Journal of Gynaecology and Obstetrics. 2001;74:311–320. doi: 10.1016/s0020-7292(01)00491-x. [DOI] [PubMed] [Google Scholar]
- Arch J, Dimidjian S, Chessick C. Are exposure-based cognitive behavioral therapies safe during pregnancy? Archives of Women’s Mental Health. 2012;15:445–457. doi: 10.1007/s00737-012-0308-9. [DOI] [PubMed] [Google Scholar]
- Battle C, Salisbury AL, Schofield CA, Ortiz-Hernandez S. Perinatal antidepressant use: understanding women’s preferences and concerns. Journal of Psychiatric Practice. 2013;19(6):443–453. doi: 10.1097/01.pra.0000438183.74359.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck C, Gable R. Postpartum Depression Screening Scale. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- Beck L, Morrow B, Lipscomb L, Johnson C, Gaffield M, Rogers M, Gilbert B. MMWR. Surveillance Summaries : Morbidity and Mortality Weekly Report. CDC; 2002. Prevalence of selected maternal behaviors and experiences, pregnancy risk assessment monitoring system (PRAMS), 1999. [PubMed] [Google Scholar]
- Bellg A, Borrelli B, Resnick B, Hecht J, Minicucci D, Ory M, Czajkowski S. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- Bergstralh E, Kosanke J. VMATCH macro. 2003 Retrieved July 2012, from http://cancercenter.mayo.edu/mayo/research/biostat/sasmacros.cfm.
- Birmes P, Brunet A, Benoit M, Defer S, Hatton L, Sztulman H, Schmitt L. Validation of the Peritraumatic Dissociative Experiences Questionnaire self-report version in two samples of French-speaking individuals exposed to trauma. European Psychiatry. 2005;20(2):145–151. doi: 10.1016/j.eurpsy.2004.06.033. [DOI] [PubMed] [Google Scholar]
- Blount A. Integrated Primary Care: The Future of Medical and Mental Health Collaboration. New York, NY: Norton; 1998. [Google Scholar]
- Brockington I, Oates J, George S, Turner D, Vostanis P, Sullivan M, Murdoch C. A screening questionnaire for mother-infant bonding disorders. Archives of Women’s Mental Health. 2001;3(4):133–140. [Google Scholar]
- Byatt N, Deligiannidis K, Freeman MP. Antidepressant use in pregnancy: a critical review focused on risks and controversies. Acta Psychiatrica Scandinavica. 2013;127(2):94–114. doi: 10.1111/acps.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology. 2002;70(5):1067–1074. doi: 10.1037//0022-006x.70.5.1067. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson C, Petkova E. Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry. 2010;167(8):915–924. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- Cohen D. Statistical Power for the Behavioral Sciences. Hillside, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Creedy D. Birthing and the development of trauma symptoms: Incidence and predictors. Australian Digital Theses Database 1999 [Google Scholar]
- Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York, NY: Guilford Press; 2002. pp. 150–176. [Google Scholar]
- Fisher J. Unpublished doctoral dissertation. University of Melbourne; Melbourne, Victorial, Australia: 1994. Obstetric Intervention: Psychosocial Predictors and Psychological Consequences. [Google Scholar]
- Foa E, Keane T, Friedman M, Cohen J, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: Guilford Press; 2008. [Google Scholar]
- Goodman J, Tyler-Viola L. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. Journal of Women’s Health. 2010;19:477–490. doi: 10.1089/jwh.2008.1352. [DOI] [PubMed] [Google Scholar]
- Kelly R, Zatzick D, Anders T. The detection and treatment of psychiatric disorders and substance use among pregnant women cared for in obstetrics. American Journal of Psychiatry. 2001;158(2):213–219. doi: 10.1176/appi.ajp.158.2.213. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick D, Resnick H, Freedy J, Pelcovitz D, Resick P, Roth S, Van der Kolk B. DSM-IV Sourcebook. Washington, DC: American Psychiatric Press; 1994. The posttraumatic stress disorder field trial: emphasis on Criterion A and overall PTSD diagnosis. [Google Scholar]
- Kulkarni M, Graham-Bermann S, Rauch S, Seng J. Witnessing versus experiencing direct violence in childhood as correlates of adulthood PTSD. Journal of Interpersonal Violence. 2011;26(6):1264–81. doi: 10.1177/0886260510368159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukens EP, McFarlane WR. Psychoeducation as evidence-based practice: considerations for practice, research, and policy. Brief Treatment and Crisis Intervention. 2004;4(3):205–225. [Google Scholar]
- Marmar C, Weiss D, Metzler T. The Peritraumatic Dissociative Experiences Questionnaire. In: Wilson J, Keane T, editors. Assessing Psychological Trauma and PTSD: A Practitioner’s Handbook. New York, NY: Guilford Press; 1997. pp. 412–428. [Google Scholar]
- Methodology for matching zip codes and FBI crime rates. Retrieved July 29 2009, from http://www.easidemographics.com/also/methods.phtml.
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy: severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267:3176–3178. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- Meaney M. Epigenetics and the biological definition of gene x environment interactions. Child Development. 2010;81:41–79. doi: 10.1111/j.1467-8624.2009.01381.x. [DOI] [PubMed] [Google Scholar]
- Ming K, Rosenbaum P. Substantial gains in bias reduction from matching with a variable number of controls. Biometrics. 2000;56:118–124. doi: 10.1111/j.0006-341x.2000.00118.x. [DOI] [PubMed] [Google Scholar]
- Morland L, Goebert D, Onoye J, Frattarelli L, Derauf C, Herbst M, Friedman M. Posttraumatic stress disorder and pregnancy health: Preliminary update and Implications. Psychosomatics. 2007;48(4):304–308. doi: 10.1176/appi.psy.48.4.304. [DOI] [PubMed] [Google Scholar]
- NICE National Institute for Health and Clinical Excellence. Guidelines on Antenatal and Postnatal Mental Health. London: NICE; 2007. [Google Scholar]
- O’Connor T, Heron J, Glover V. Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. Journal of the American Adacemy of Child and Asolescent psychiatry. 2002;41(12):1470–1477. doi: 10.1097/00004583-200212000-00019. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychological Bulletin. 2007;133(2):183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Resnick H, Kilpatrick D, Dansky B, Saunders B, Best C. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, Yonkers KA. Effects of posttraumatic stress disorder on pregnancy outcomes. Journal of Affective Disorders. 2007;102(1–3):137–143. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Grigoriadis S, Mamisashvili L, Vonderporten EH, Roerecke M, Rehm J, Dennis CL, Koren G, Steiner M, Mousmanis P, Cheung A. Selected pregnancy and delivery outcomes after exposure to antidepressant medication: A systematic review and meta-analysis. JAMA. 2013;70(4):436–443. doi: 10.1001/jamapsychiatry.2013.684. [DOI] [PubMed] [Google Scholar]
- Seng J, Low LK, Sperlich M, Ronis D, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics & Gynecology. 2009;114(4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Low LK, Sperlich M, Ronis DL, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. BJOG: An International Journal of Obstetrics & Gynaecology. 2011;118(11):1329–1339. doi: 10.1111/j.1471-0528.2011.03071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Rauch SAM, Resnick H, Reed CD, King A, Low LK, Liberzon I. Exploring posttraumatic stress disorder symptom profile among pregnant women. Journal of Psychosomatic Obstetrics & Gynecology. 2010;31(3):176–187. doi: 10.3109/0167482X.2010.486453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Sperlich M, Kane Low L, Muzik M, Ronis D, Liberzon I. Posttraumatic stress disorder, child abuse history, postpartum mental health and bonding: A prospective cohort study. Journal of Midwifery and Women’s Health. 2013;58(1):57–68. doi: 10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Sperlich M, Rowe H, Cameron H, Harris A, Rauch SAM, Bell SA. The Survivor Moms’ Companion: Open pilot of a posttraumatic stress specific psychoeducation program for pregnant survivors of childhood maltreatment and sexual trauma. International Journal of Childbirth. 2011;1:111–121. [Google Scholar]
- Simkin P, Klaus P. When Survivors Give Birth: Understanding and Healing the Effects of Early Sexual Abuse on Childbearing Women. Seattle, WA: Classic Day Publishing; 2004. [Google Scholar]
- Smith M, Poschman K, Cavaler IM, Howell H, Yonkers K. Symptoms of posttraumatic stress disorder in a community sample of low-income pregnant women. American Journal of Psychiatry. 2006;163(5):881–884. doi: 10.1176/ajp.2006.163.5.881. [DOI] [PubMed] [Google Scholar]
- Sperlich M, Seng J. Survivor Moms: Women’s Stories of Birthing, Mothering, and Healing after Sexual Abuse. Eugene, OR: Motherbaby Press; 2008. [Google Scholar]
- Sperlich M, Seng J, Rowe H, Cameron H, Harris A, McCracken A, Bell SA. The Survivor Moms’ Companion: Feasibility, safety, and acceptability of a posttraumatic stress specific psychoeducation program for pregnant survivors of childhood maltreatment and sexual trauma. International Journal of Childbirth. 2011;1:122–135. [Google Scholar]
- Spinazzola J, Blaustein M, van der Kolk BA. Posttraumatic stress disorder treatment outcome research: The study of unrepresentative samples? Journal of Traumatic Stress. 2005;18(5):425–436. doi: 10.1002/jts.20050. [DOI] [PubMed] [Google Scholar]
- Trauma-Informed Care and Trauma Services. Substance Abuse and Mental Health Services Administration. Retrieved February 19m 2914 from http://www.samhsa.gov/nctic. [PubMed]
- Wittchen H. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wittkowski A, Wieck A, Mann S. An evaluation of two bonding questionnaires: a comparison of the Mother-to-Infant Bonding Scale with the Postpartum Bonding Questionnaire in a sample of primiparous mothers. Archives of Women’s Mental Health. 2007;10(4):171–175. doi: 10.1007/s00737-007-0191-y. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. New York, NY: Guilford Press; 1997. pp. 192–238. [Google Scholar]
- Yehuda R, Engel SM, Brand SR, Seckl J, Marcus SM, Berkowitz GS. Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. Journal of Clinical Endocrinology & Metabolism. 2005;90(7):4115–4118. doi: 10.1210/jc.2005-0550. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Halligan S, Bierer L. Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research. 2001;35(5):261–270. doi: 10.1016/s0022-3956(01)00032-2. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Capezza NM, Parker D. An interpersonally based intervention for low-income pregnant women with intimate partner violence: a pilot study. Archives of Women’s Mental Health. 2011;14(1):55–65. doi: 10.1007/s00737-010-0195-x. [DOI] [PMC free article] [PubMed] [Google Scholar]